Abstract
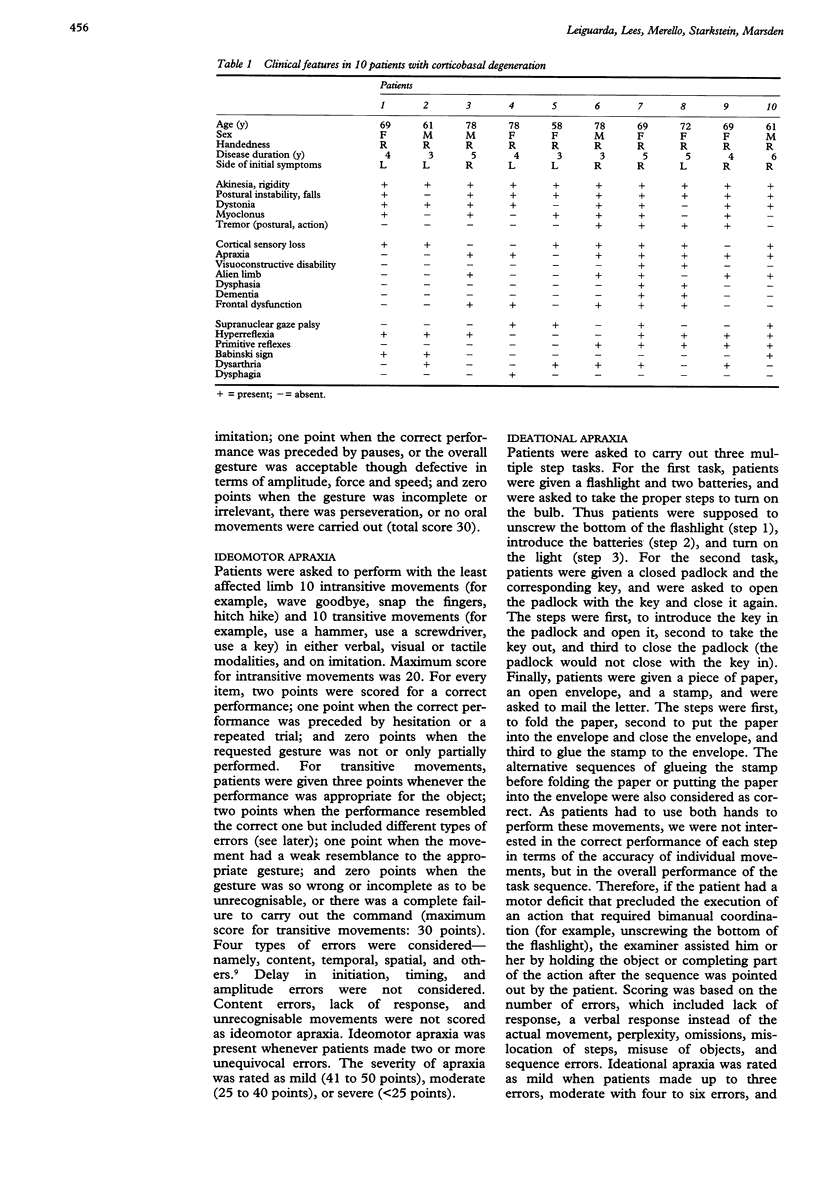
Although apraxia is one of the most frequent signs in corticobasal degeneration, the phenomenology of this disorder has not been formally examined. Hence 10 patients with corticobasal degeneration were studied with a standardised evaluation for different types of apraxia. To minimise the confounding effects of the primary motor disorder, apraxia was assessed in the least affected limb. Whereas none of the patients showed buccofacial apraxia, seven showed deficits on tests of ideomotor apraxia and movement imitation, four on tests of sequential arm movements (all of whom had ideomotor apraxia), and three on tests of ideational apraxia (all of whom had ideomotor apraxia). Ideomotor apraxia significantly correlated with deficit in both the mini mental state examination and in a task sensitive to frontal lobe dysfunction (picture arrangement). Two of the three patients with ideomotor apraxia and ideational apraxia showed severe cognitive impairments. The alien limb behaviour was present only in patients with ideomotor apraxia. In conclusion, ideomotor apraxia is the most frequent type of apraxia in corticobasal degeneration, and may be due to dysfunction of the supplementary motor area. There is a subgroup of patients with corticobasal degeneration who have a severe apraxia (ideomotor and ideational apraxia), which correlates with global cognitive impairment, and may result from additional parietal or diffuse cortical damage.
Full text
PDF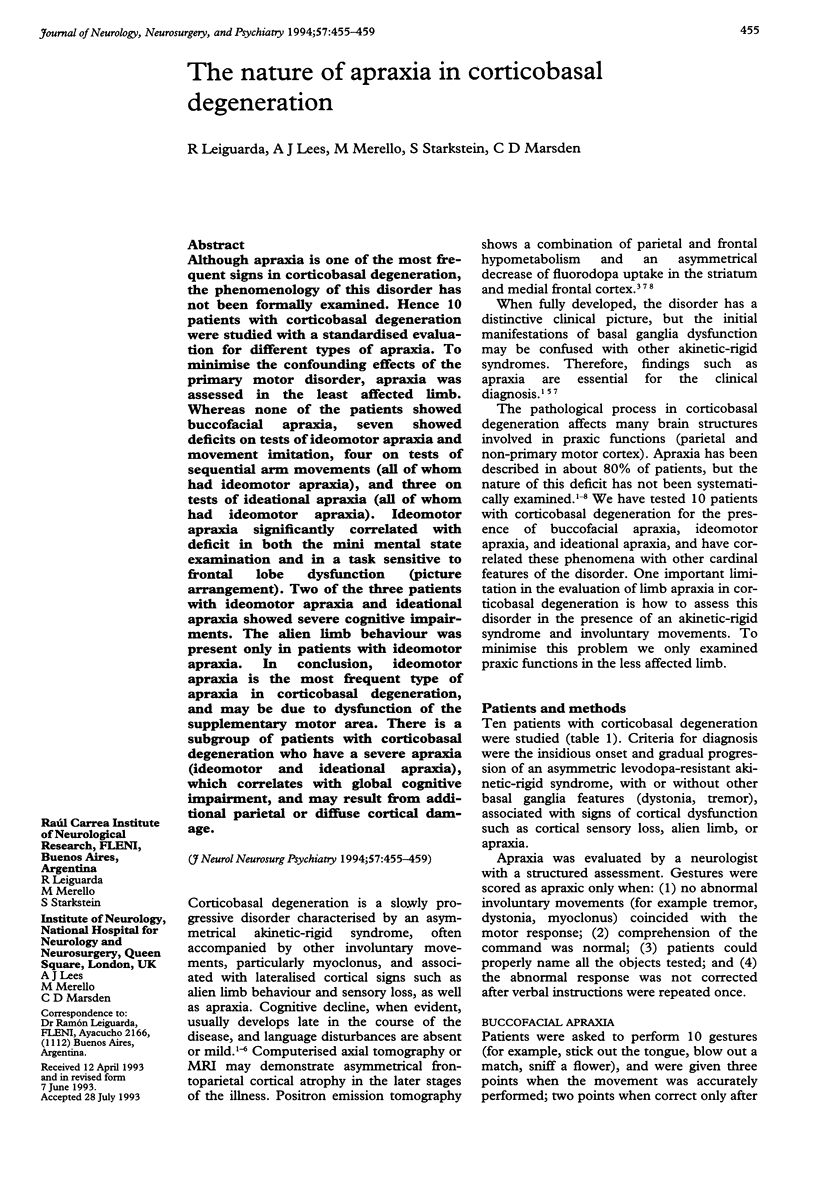
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brinkman C., Porter R. Supplementary motor area in the monkey: activity of neurons during performance of a learned motor task. J Neurophysiol. 1979 May;42(3):681–709. doi: 10.1152/jn.1979.42.3.681. [DOI] [PubMed] [Google Scholar]
- Clark A. W., Manz H. J., White C. L., 3rd, Lehmann J., Miller D., Coyle J. T. Cortical degeneration with swollen chromatolytic neurons: its relationship to Pick's disease. J Neuropathol Exp Neurol. 1986 May;45(3):268–284. doi: 10.1097/00005072-198605000-00011. [DOI] [PubMed] [Google Scholar]
- DENNY-BROWN D. The nature of apraxia. J Nerv Ment Dis. 1958 Jan;126(1):9–32. doi: 10.1097/00005053-195801000-00003. [DOI] [PubMed] [Google Scholar]
- De Renzi E., Lucchelli F. Ideational apraxia. Brain. 1988 Oct;111(Pt 5):1173–1185. doi: 10.1093/brain/111.5.1173. [DOI] [PubMed] [Google Scholar]
- Douglass A. B., Harris L., Pazderka F. Monozygotic twins concordant for the narcoleptic syndrome. Neurology. 1989 Jan;39(1):140–141. doi: 10.1212/wnl.39.1.140. [DOI] [PubMed] [Google Scholar]
- Fried I., Katz A., McCarthy G., Sass K. J., Williamson P., Spencer S. S., Spencer D. D. Functional organization of human supplementary motor cortex studied by electrical stimulation. J Neurosci. 1991 Nov;11(11):3656–3666. doi: 10.1523/JNEUROSCI.11-11-03656.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibb W. R., Luthert P. J., Marsden C. D. Corticobasal degeneration. Brain. 1989 Oct;112(Pt 5):1171–1192. doi: 10.1093/brain/112.5.1171. [DOI] [PubMed] [Google Scholar]
- Ikeda A., Lüders H. O., Burgess R. C., Shibasaki H. Movement-related potentials recorded from supplementary motor area and primary motor area. Role of supplementary motor area in voluntary movements. Brain. 1992 Aug;115(Pt 4):1017–1043. doi: 10.1093/brain/115.4.1017. [DOI] [PubMed] [Google Scholar]
- Lippa C. F., Cohen R., Smith T. W., Drachman D. A. Primary progressive aphasia with focal neuronal achromasia. Neurology. 1991 Jun;41(6):882–886. doi: 10.1212/wnl.41.6.882. [DOI] [PubMed] [Google Scholar]
- Ochipa C., Rothi L. J., Heilman K. M. Conceptual apraxia in Alzheimer's disease. Brain. 1992 Aug;115(Pt 4):1061–1071. doi: 10.1093/brain/115.4.1061. [DOI] [PubMed] [Google Scholar]
- Orgogozo J. M., Larsen B. Activation of the supplementary motor area during voluntary movement in man suggests it works as a supramotor area. Science. 1979 Nov 16;206(4420):847–850. doi: 10.1126/science.493986. [DOI] [PubMed] [Google Scholar]
- PENFIELD W., WELCH K. The supplementary motor area of the cerebral cortex; a clinical and experimental study. AMA Arch Neurol Psychiatry. 1951 Sep;66(3):289–317. doi: 10.1001/archneurpsyc.1951.02320090038004. [DOI] [PubMed] [Google Scholar]
- Raade A. S., Rothi L. J., Heilman K. M. The relationship between buccofacial and limb apraxia. Brain Cogn. 1991 Jul;16(2):130–146. doi: 10.1016/0278-2626(91)90002-p. [DOI] [PubMed] [Google Scholar]
- Rebeiz J. J., Kolodny E. H., Richardson E. P., Jr Corticodentatonigral degeneration with neuronal achromasia. Arch Neurol. 1968 Jan;18(1):20–33. doi: 10.1001/archneur.1968.00470310034003. [DOI] [PubMed] [Google Scholar]
- Riley D. E., Lang A. E., Lewis A., Resch L., Ashby P., Hornykiewicz O., Black S. Cortical-basal ganglionic degeneration. Neurology. 1990 Aug;40(8):1203–1212. doi: 10.1212/wnl.40.8.1203. [DOI] [PubMed] [Google Scholar]
- Sawle G. V., Brooks D. J., Marsden C. D., Frackowiak R. S. Corticobasal degeneration. A unique pattern of regional cortical oxygen hypometabolism and striatal fluorodopa uptake demonstrated by positron emission tomography. Brain. 1991 Feb;114(Pt 1B):541–556. doi: 10.1093/brain/114.1.541. [DOI] [PubMed] [Google Scholar]
- Tognola G., Vignolo L. A. Brain lesions associated with oral apraxia in stroke patients: a clinico-neuroradiological investigation with the CT scan. Neuropsychologia. 1980;18(3):257–272. doi: 10.1016/0028-3932(80)90122-0. [DOI] [PubMed] [Google Scholar]
- Watson R. T., Fleet W. S., Gonzalez-Rothi L., Heilman K. M. Apraxia and the supplementary motor area. Arch Neurol. 1986 Aug;43(8):787–792. doi: 10.1001/archneur.1986.00520080035016. [DOI] [PubMed] [Google Scholar]


