Abstract
Introduction
Many Canadians struggle to access the primary care they need while at the same time primary care providers report record levels of stress and overwork. There is an urgent need to understand factors contributing to the gap between a growing per-capita supply of primary care providers and declines in the availability of primary care services. The assumption of responsibility by primary care teams for services previously delivered on an in-patient basis, along with a rise in administrative responsibilities may be factors influencing reduced access to care.
Methods and analysis
In this mixed-methods study, our first objective is to determine how the volume of services requiring primary care coordination has changed over time in the Canadian provinces of Nova Scotia and New Brunswick. We will collect quantitative administrative data to investigate how services have shifted in ways that may impact administrative workload in primary care. Our second objective is to use qualitative interviews with family physicians, nurse practitioners and administrative team members providing primary care to understand how administrative workload has changed over time. We will then identify priority issues and practical response strategies using two deliberative dialogue events convened with primary care providers, clinical and system leaders, and policy-makers.
We will analyse changes in service use data between 2001/2002 and 2021/2022 using annual total counts, rates per capita, rates per primary care provider and per primary care service. We will conduct reflexive thematic analysis to develop themes and to compare and contrast participant responses reflecting differences across disciplines, payment and practice models, and practice settings. Areas of concern and potential solutions raised during interviews will inform deliberative dialogue events.
Ethics and dissemination
We received research ethics approval from Nova Scotia Health (#1028815). Knowledge translation will occur through dialogue events, academic papers and presentations at national and international conferences.
Keywords: primary care, health services administration & management, organisation of health services, human resource management
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This study will involve both quantitative and qualitative data complemented by deliberative dialogue events for robust description, analysis and actionable recommendations.
Trustworthiness of qualitative methods and analysis will be demonstrated through inclusion of three professional groups working in two provinces, the positionality and reflexivity of diverse research team members, the use of constant comparison throughout concurrent data collection, thick description and an audit trail.
A population-level analysis of factors shaping changing workload will inform trends for system-wide planning, but will not provide detailed clinician-level information.
Introduction
There are more primary care providers per person than ever before in Canada.1 At the same time, primary care is described as being in crisis,2–4 as Canadians struggle to access needed care5 and primary care providers report record levels of stress and overwork.6 There is an urgent need to understand factors contributing to the gap between a growing number of primary care providers per person and declines in the availability of primary care services.7 To some extent this gap may reflect declining hours worked8 or service volume9 per physician, but evidence also points to broader health system changes that may impact workload in primary care10 over and above visit volume. Neither the extent of these changes, nor their impact on provider experience and patient access have been carefully studied.6
Beyond patient visits, primary care providers (including family physicians (FPs) and nurse practitioners (NPs)) are responsible for indirect patient care activities such as arranging prescriptions, lab tests, imaging, specialist referrals and medical forms, as well as maintaining a longitudinal patient record.11 Over the past 20 years, we have seen a shift in care from hospitals to communities,12 a proliferation of guidelines and increased complexity in the management of common chronic conditions,13–16 and accelerating population ageing.12 17 18 The intersecting effects of these trends may mean that there is greater need than ever for care coordination or indirect patient care, contributing to expanding administrative workload in primary care. Navigating electronic medical records, complicated referral processes, and cumbersome forms, may be increasing the time needed to complete indirect patient related tasks. Patients may be referred by primary care providers to programmes or specialists as part of the overall care plan. These referrals, however, often result in additional administrative work and record-keeping responsibilities. Paperwork and tasks flow back to primary care from referral sources, further increasing workload. In addition to administrative responsibilities related to care coordination, primary care providers play varied roles in clinic administration, depending on service delivery model.
Administrative workload has been described as a source of burn-out and reduced access to care for patients, and may push FPs to choose options other than comprehensive community-based practice.19 This has been casually called ‘death by a thousand papercuts’ or more recently ‘death by a thousand clicks’.20 Under this view, time spent on a variety of administrative tasks is secondary to the ‘real’ work of primary care. Indeed administration has been broadly characterised as taking away from other patient care activities, thereby making health systems less efficient and also less equitable, as people who most need coordinated care may struggle to access it.10 21 At the same time, administrative work is central to delivering coordinated and integrated care to patients and to clinic operations.
Outcomes of a survey conducted by Doctors Nova Scotia published in December 2021 revealed that administrative burdens were included among the top three challenges facing primary care physicians in that province.22 The magnitude of this problem led to the involvement of the Office of Regulatory Affairs and Service Effectiveness (ORASE) of the Nova Scotia government to investigate and implement concrete action plans to address unnecessary administrative burdens on physicians.23 With the support of Doctors Nova Scotia, a survey administered by ORASE found that 38% of physicians’ time was spent on unnecessary administrative tasks, and that 24% of that work could have been done by someone in a different role/profession.23 The survey also found that physicians believed that 14% of that work could be entirely eliminated.23 The report on the survey noted that the main contributors to unnecessary administrative tasks were: the completion of medical forms, doctor’s notes, business operations, billing, including shadow billing, licensing, privileging and tasks associated with requirements of government and oversight entities. Importantly, physicians indicated that administrative burdens significantly contributed to burn-out, and that reductions of time spent on these tasks would allow time for improved work/life balance and improved patient care.23 While administrative burden is a problem for all acute, specialist and primary care physicians in Nova Scotia, given the unique role primary care physicians play in coordinating care, we need detailed information about, and solutions for, this setting.
The impact of administrative burdens in primary care is complex. It is not simply a problem of too much paperwork. FPs and NPs are also increasingly responding to issues related to patients’ social determinants of health without adequate support and resources, often resulting in frustration, stress and emotional burden.23 Wait times for specialist referrals translate to lengthier periods of patient management, additional paperwork, follow-up on referrals and carrying the emotional burden of patients’ unmet needs. Added to these pressures are expectations to take on more ‘unattached’ patients, while not having the time or capacity to do so because of the complexity of care required by existing patients, coupled with heavy administrative burdens. While the emotional toll of administrative burden on primary care providers is not the focus of this study, it is important to recognise that there are many concerning ripple effects that accompany this problem.
A 2023 study24 built on the findings of the ORASE’s Physician Administrative Burden Survey conducted in Nova Scotia. Study outcomes demonstrated that a 10% reduction of unnecessary paperwork for primary care physicians in New Brunswick would equal an additional 119 726 patient visits annually.25 While increased recognition of this problem and attempts to address it are welcome, it comes with an implicit expectation that primary care providers will have the capacity to see new patients and/or increase the number of visits for existing patients. This expectation may add to primary care provider stress and emotional burden.
While there is some limited qualitative research with primary care physicians in the USA,26 none yet exists in Canada. We also need information drawing on the experience and expertise of NPs, clinic managers, medical office assistants and other primary care team members with administrative responsibilities. New information to understand the extent and drivers of administrative workload, as well as the strategies required to make this activity more efficient are urgently needed.
Study objectives
This project will address three objectives and nested research questions, with the overarching goal of adjusting administrative workload, while ensuring efficient, accountable and well-coordinated care:
-
Determine how the volume of services requiring primary care coordination has changed over time
How has service volume shifted from inpatient services to outpatient and community-based services requiring coordination through primary care?
How has the volume of outpatient services requiring primary care coordination and oversight (ie, prescriptions, testing, imaging and specialist consultations) changed over time?
-
Use interviews with primary care providers (FPs and NPs) and administrative team members to understand how administrative workload has changed:
What are current experiences of administrative workload, including work related to patient care and clinic administration?
How has administrative workload changed over time? What factors have shaped changes?
What are areas of particular concern and how might these be addressed?
-
Drawing on the findings of objectives 1 and 2, with primary care providers and service planners, coidentify priority issues and codevelop practical response strategies to make administrative work more efficient:
Which areas of concern are addressable in the short, medium and long term?
What actions would be needed, who is in a position to act, and what resources would be involved?
Methods
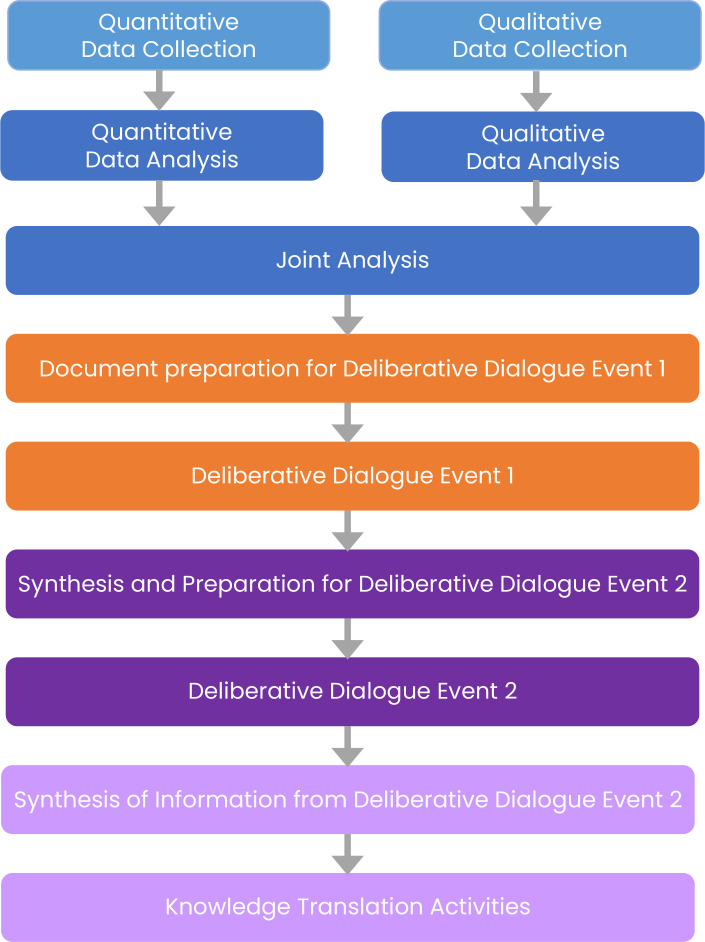
This 2-year study (June 2023–May 2025) will use different data sources and methodologies to address each project objective within two study provinces, Nova Scotia and New Brunswick (figure 1). Findings of descriptive quantitative analysis under objective 1 and in-depth qualitative interviews under objective 2 will inform deliberative dialogues used to address objective 3.
Figure 1.
Objective 1: quantitative administrative data
To address objective 1, we will seek out and combine administrative data from multiple sources to create a more complete picture of shifts in service use over time, accessing data from 2001/2002 (or earliest available, depending on dataset) and 2023/2024 (or most recent available). This time frame will allow us to explore long-term trends, as well as changes since March 2020 due to the pandemic. We do not need access to individual, record-level data to meet study objectives and plan only population-level analysis, using population-based data that captures service delivery for all insured residents of the study provinces (approximately 1 million residents in NS and 800 000 in NB). To address question 1a, we will combine publicly available data accessible through the Canadian Institutes of Health Information at the provincial level to examine trends in hospital services use as well as services delivered on an outpatient basis or in the community. To examine trends in hospitalisations, we will count the number of discharges recorded in the Discharge Abstract Database (DAD) and the number of days patients spent in hospital.27 The DAD captures administrative, clinical and demographic information on all hospital discharges (including deaths, sign-outs and transfers). To capture outpatient physician service use, we will use the National Physician Database (NPD) to track number of visits with primary care physicians, as well as with medical specialists and surgical specialists. The NPD contains information on both the demographic characteristics, and their payments and activities within the healthcare system. We will use the DAD to count the number of day surgery procedures. Finally, we will use the National Health Expenditures Database to triangulate findings about service volume, examining shifts in spending between hospitals and other categories of healthcare over time.28
To address question 1b, we will track total laboratory tests and imaging services completed for outpatients, as FP/NPs have a role in reviewing and coordinating these even when ordered by other physicians. Public prescription data for seniors will be used to count the number of different drugs dispensed per year, at the level of the first five digits of the Anatomical Therapeutic Chemical classification code.29 We will exclude vaccines (J07), vitamins (A11), mineral supplements (A12), tonics (A13) and various (V) categories. As with lab tests, as FP/NPs have a role in managing all prescriptions, we will report the total. We will use NPD to track specialist physician visit data, focusing on those seen as outpatients, as reports would go back to NPs/FPs for patient follow-up.
Quantitative analysis
Our approach is primarily descriptive and it is not necessary to link datasets at the individual level. We will present service use data as annual total counts (to capture how total workload has changed), as rates per capita (to capture how patient-level care has changed), as well as rates per primary care provider, and per primary care service (to capture how changes in workload map onto primary care workforce supply and practice volume). Following visual inspection of trends over time, we will use segmented regression to quantify changes in level or trend of service use over time, including in the context of the COVID-19 pandemic.30
Objective 2: in-depth video interviews
Our approach most closely resembles a mixed-methods multilevel plan in which quantitative and qualitative data will be concurrently collected and analysed, each with equal weight. The research questions we are attempting to answer through the use and analysis of quantitative data while complementary, are distinct from the research questions we are exploring though qualitative interviews and analysis. Findings from both methods will contribute to knowledge generation and may enhance each other; however, it is impossible to know in advance of data collection and analysis precisely how this will evolve. We anticipate that findings from quantitative data on changes in service volume requiring primary care coordination will be better understood when complemented by narratives from the interviews that add important contextual information
Interviews
We will use interviews with primary care providers (FPs, NPs and other team members involved in administration (clinic managers and/or medical office assistants) to understand their current administrative workload (including care coordination and other administrative activities), how this has changed over time, and what opportunities exist to manage this differently. See online supplemental material for interview guides. We will be interviewing primary care providers and administrative staff in New Brunswick as well as Nova Scotia to compare narratives between the two provinces, and to inform a planned Pan-Canadian study on this topic in the future.
bmjopen-2023-076917supp001.pdf (546.7KB, pdf)
We will conduct interviews via a secure online video platform. Interviews will last approximately 1 hour and will be scheduled at a time that is convenient and acceptable to study participants. This will allow us to reach a geographically varied set of participants at a lower cost than conducting in-person interviews. Video interviews have been shown to produce similar data richness when compared with in-person interviews.31 32 Interviews will be conducted by Master’s or PhD trained qualitative research staff. Interview data will be digitally recorded, professionally transcribed, quality checked for accuracy and deidentified prior to analysis. Each interviewer will complete field notes shortly after interviews take place. Field notes will be reviewed prior to and during analysis. The research associate will document all analytic decisions for the audit trail.
Recruitment
We will purposively recruit primary care providers who are funded through a range of payment models (fee-for-service and alternate payment plans), who work in a range of clinic models (independent, health authority partnered, turn-key health authority operated) and who work in a range of geographical locations (urban and rural locations throughout each province). Specifically, we will recruit from Nova Scotia Health Primary Care Clinics, Dalhousie Family Medicine teaching sites, Doctors Nova Scotia and NPs of New Brunswick. Potential participants will complete a brief on-line screening survey (see online supplemental information). We plan sample sizes of 20 FP/NP and 20 administrative team member interviews to investigate differences by models and locations. The total sample size is 40. This sample size is consistent with recommendations for similar study designs.33–35 Previous research we conducted concerning primary care practice was received with strong interest36; we anticipate similarly strong interest in this topic.
bmjopen-2023-076917supp002.pdf (602KB, pdf)
The project research associate will contact key individuals at recruitment organisations to explain the study and coordinate outreach. Key individuals at each site will distribute introductory emails along with a study poster. There will be a link from the poster to the screening survey. Our aim is to interview participants from various geographical settings, practice types, remuneration models, discipline (NP, FP, administration) and with varying lengths of practice experience and roles in primary care clinic settings. Sampling from the results of the screening survey will involve selection of interview participants with the greatest number of diverse characteristics. Sampling will depend on the number and diversity of survey responses. Additional recruitment will take place until sampling goals have been reached.
Gender is of central importance in this project. A substantial body of evidence shows that physician practice patterns are gendered, as are expectations with respect to care provision, including potentially administrative workload.37–39 We will be attentive to gender in both interview recruitment and qualitative analysis. As an increasing proportion of FPs are women, and 92% of NPs in Canada40 are female we will actively recruit men and ensure there are no barriers to participation for people with other genders. We will ask participants about how they perceive relationships between gender and administrative workload, and our analysis will explore how responses and experiences vary by gender.
Informed consent
Consent is implied by completion of the online survey. This is clearly articulated in the introductory text to the survey and has been approved by the local research ethics board. Potential participants selected for interviews will be contacted by the research associate. A participant information sheet covering all the topics typically included in consent forms will be provided at that time, and participants will have an opportunity to ask any questions they have before interviews are scheduled. At the beginning of each interview, the research associate will review study aims, participant rights and obtain verbal consent. The consent process will be audiotaped for documentation purposes.
Each participant will be assigned an identification number in place of their name. All interview transcripts will bear the identification number. Participant quotes will be included in presentations and publications emanating from this study; however, there will not be any personal identifiers. Quotes will be attributed to the type of professional, gender and province in which the person is practicing, with attention to any contextual details of practice that could be identified.
Data management
Quantitative and qualitative data and consent forms will be securely stored on encrypted password-protected computers. Files are backed up monthly on an external drive. Both quantitative and qualitative data will be stored for a period of 7 years after which it will be permanently destroyed in accordance with the policies of Dalhousie University.
Qualitative analysis
We will employ Braun and Clarke’s reflexive thematic analysis,41 which fits well with our critical qualitative approach42 43 and relativist epistemology.44 Our analysis will also be guided by social constructivism.45 This blended approach reflects our positionality as active participants in the research process, our understanding that meaning is socially constructed, and the key role of reflexivity throughout the research process. There are six fluid phases involved when conducting reflexive thematic analysis. The first phase is becoming familiar with the interview data by reading through transcripts on several occasions. The next phase involves initial coding of data related to the research question. We plan to employ an inductive approach to analysis at that stage. This will be followed by the generation of preliminary themes. We will then return to the data, further develop and revise themes. Depending on the analysis in progress, we may continue with the inductive analysis or we may decide to conduct a deductive analysis based on a concept or framework that we determine at that point may provide greater depth to the findings. In the latter case, we will return to the data and commence a new phase of coding deductively. This is what is meant by the fluidity of analytic phases. Once that phase has been completed, we will further refine and name themes and develop definitions for the themes. The final stage involves written preparation of the results including a discussion of their relevance to the existing literature.
Initially, each member of the qualitative working group will review 2–3 transcripts each. Working group members will meet weekly to discuss the transcripts and potential codes. The research associate will use NVivo software to begin the inductive coding process based on those discussions. We will begin by generating a detailed description of administrative workload (research question 2a). Analysis will occur concurrently with data collection and the interview guide will be iteratively adjusted if needed as our understanding of experiences of administrative workload develops. We will then expand analysis to explore changes over time (question 2b) and to make comparisons between FP/NP and administrative team member interviews, as well as to explore variation across payment model, practice model and practice setting. To address research question 2c, and in preparation for Objective 3, we will group and compile areas of concern and potential solutions raised by participants.
The qualitative working group will continue to meet biweekly or as needed throughout the analytic process. The diverse perspectives and expertise of group members will ensure a robust and meticulous analysis of qualitative data. We will have representation from family medicine, nursing, health administration and health policy, as well as expertise in qualitative research methods, ethnography and medical anthropology. Each interviewer will prepare field notes shortly after interviews take place. This may result in modifications to the interview guides. Field notes will be reviewed prior to and during analysis. The research associate will document all analytic decisions as part of the audit trail.
Time frame: We expect the recruitment period and interviews to begin in September and be complete by the end December 2023. Qualitative analysis will also commence in September 2023 and is expected to continue through to June 2024.
Objective 3: integration of findings and knowledge exchange
We will work with partners on the team to identify relevant participants for a final two-phase dialogue event, designed to integrate and interpret both scientific and contextual data for the purpose of informing policy development,46 in this case, strategies to address administrative workload. We will include (1) a subset of interview participants (primary care providers and administrative team members) working in varied contexts, (2) clinical leaders who can make changes within primary care service delivery environments and (3) system administrators and policy-maker leaders who can change processes that involve both primary care and other parts of the health system or sectors. We anticipate 12–15 participants will be involved in both the first and second stages of dialogue events.
Prior to the first meeting, the study team will review quantitative findings and the initial list of areas of concern identified through qualitative interviews. These will be integrated into a background document circulated in advance of the dialogue process. Quantitative findings will inform changing administrative workload over time, and qualitative findings will provide context for areas of concern and potential solutions that will be explored during dialogue events. Dialogues will be conducted via video-conference in two stages. In the first stage, nominal group technique (NGT)47 48 will be used to guide discussion and prioritisation of issues and solutions. Nominal group technique has been used since the 1960s for the identification of problems, priority ranking of issues, action items or questions in small group in-person sessions. One of the technique’s key strengths is it is designed for equal representation among participants and is non-hierarchical in nature. In this study, areas of concern generated and recorded in qualitative interviews will serve as a starting point for discussion, with participants invited to add topics not yet mentioned. In a ranking exercise, participants will be invited to consider which tasks are time-consuming and/or offer lower value to patients and the system. Then participants will be asked to discuss and explain the reasons for their ranking.
The second stage will focus on feasibility and actions needed to address high-priority areas of concern identified in the first event. Prior to the second stage, we will identify any additional participants with knowledge specific to areas of concern. Participants will be asked to consider which could be addressable in the short term (<3 months), medium term (3–12 months) and long term (1 year or more). In breakout groups focusing on individual areas of concern, participants will be asked to consider what action would be needed and who would need to be involved. Each breakout group will be led by a facilitator briefed and prepared by the research team. After the breakout group discussions, there will be a debriefing with the full group of participants. The dialogue process will provide concrete and actionable strategies tailored to the primary care setting, which complement other ongoing work within Nova Scotia and New Brunswick health systems.
Impact on equity in recruitment and retention of healthcare professionals
Administrative workload directly impacts recruitment and retention of healthcare professionals, at times influencing FPs to choose options other than community-based primary care as a strategy to circumvent burn-out.19 Expectations for coordination may vary by how primary care providers are gendered and racialised49; women form a growing proportion of the primary care workforce.50 Addressing coordination workload can, therefore, play a role in supporting equity in recruitment and retention of healthcare professionals. Understanding and supporting coordination of care is central to people-centred, flexible, quality healthcare. Identifying practical strategies to make coordination more efficient can support innovative healthcare models, and more seamless integration of virtual care into patients’ journeys.
Patient and public involvement
Patients or members of the public were not involved in the design of this study and will not be involved during implementation. While our research questions respond to topics of patient and public interest, research approaches focus on routinely collected health system data and research participants are primary care providers and administrative staff. We, therefore, focus on including a range of policy and provider expertise and experience within the research team. Inclusion of patients in the deliberative dialogue events is not currently planned.
Study limitations
Available quantitative data sources capture variables labelled ‘sex’, but there is no measure of gender, and administrative or legal sex may not correspond to sex assigned at birth. This is a limitation of secondary analysis of these data. Where possible, we will distinguish between patterns plausibly shaped by sex or gender in interpretation.
Care coordination activities are not recorded in administrative billing data. It is not possible to directly capture time spent on care coordination or other administrative work. Instead, we focus broadly on shifts in care delivery between hospital and community, as well as changes in services that require coordination, review and/or administration on the part of primary care providers. It is beyond the scope and budget of this project to obtain access to linked, record-level data or to collect detailed time use data. Study objectives can be addressed through aggregate data that can be shared with no risk of identification. This project will form the groundwork for a future grant proposal that will use record-level data from the same sources to analyse changes over time by population age and generate projections of future primary care capacity.
Ethics and dissemination
Research ethics approval for this protocol was received from Nova Scotia Health (REB # 1028815) for research activities in both Nova Scotia and New Brunswick. This study conforms to the Declaration of Helsinki (June 1962; amended October 2013) and the Belmont Report (1979).
We are taking an integrated knowledge translation approach51 and have assembled a team that includes varied perspectives. Primary care provider coinvestigators and policy partners affirm the urgent need to address administrative workload. We will present findings and seek feedback from the groups represented by partners and team members following completion of objectives 1 and 2. Deliberative dialogues under objective 3 are themselves a method for knowledge translation, designed to integrate and interpret data to inform strategies addressing administrative workload. This project will also yield traditional academic outputs crossing multiple disciplines and results will be disseminated to a range of audiences.
Results will inform healthcare delivery excellence that addresses opportunities for team-based care and the ability of healthcare providers to work to their full scope of practice. New or expanded roles for administrative and other primary care team members are being piloted in Nova Scotia. This pilot research will enrich the understanding of our research outcomes and also support ongoing innovation. Finally, a robust system of primary care is fundamental to addressing health inequalities in access to care. There is evidence of declining equity in access to primary care in Canada.7 Limited primary care capacity and inadequate systems of coordination impact patients with more complex health and social needs most severely. High-performing systems of primary care can connect healthcare with other community resources. This coordination is needed to support collaborative approaches to address the social determinants of health.
Supplementary Material
Footnotes
Twitter: @DrEmilyMarshall, @MisenerRuth
Contributors: MRL originally conceived the study, wrote the first draft of the introduction and objective 1 methods. CM wrote the first draft of objective 2 methods. FB, RB, JE, AG, LH, ML, MM, EGM, RM-M, MM, EP and JT provided feedback for revisions to the interview guides, screening questionnaire and the draft protocol, and approved the final version for submission.
Funding: This study is supported by Research Nova Scotia. Dr. Ruth Lavergne is a Tier 2 Canada Research Chair in Primary Care.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Canadian Institute for Health Information . Supply, Distribution and Migration of Physicians in Canada, 2020- Data Tables. CIHI, 2021. [Google Scholar]
- 2.Walsh M, Pearson H. Nova Scotia Doctor Calls Family Doctor Shortage a “Crisis” Available: http://globalnews.ca/news/3270444/nova-scotia-doctor-calls-family-doctor-shortage-a-crisis/ [Accessed 6 Jun 2017].
- 3.British Columbia Medical Journal . The evolving crisis in primary care. Available: https://bcmj.org/editorials/evolving-crisis-primary-care [Accessed 16 Aug 2022].
- 4.The Globe and Mail . Opinion: Canada has a primary-care crisis. Here are three steps we must take to solve this problem. Available: https://www.theglobeandmail.com/opinion/article-canada-has-a-primary-care-crisis-here-are-three-steps-we-must-take-to/ [Accessed 16 Aug 2022].
- 5.Canadian Institute for Health Information . How Canada Compares: Results from the Commonwealth Fund’s 2020 International Health Policy Survey of the General Population in 11 Countries. CIHI, 2021. [Google Scholar]
- 6.Sovran V, Ytsma A, Husak L, et al. Coordination of care could improve: Canadian results from the Commonwealth fund International health policy survey of primary care physicians. Healthc Q 2020;23:6–8. 10.12927/hcq.2020.26283 [DOI] [PubMed] [Google Scholar]
- 7.Lavergne MR, Bodner A, Peterson S, et al. Do changes in primary care service use over time differ by neighbourhood income? population-based longitudinal study in British Columbia, Canada. Int J Equity Health 2022;21:80. 10.1186/s12939-022-01679-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Islam R, Kralj B, Sweetman A. Physician workforce planning in Canada: the importance of accounting for population aging and changing physician hours of work. CMAJ 2023;195:E335–40. 10.1503/cmaj.221239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rudoler D, Peterson S, Stock D, et al. Changes over time in patient visits and continuity of care among graduating cohorts of family physicians in four Canadian provinces. CMAJ 2022;194:E1639–46. 10.1503/cmaj.220439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lavergne R, Peterson S, Rudoler D, et al. Productivity decline or administrative avalanche? examining factors that shape changing workloads in primary care. Healthc Policy 2023;19:114–29. 10.12927/hcpol.2023.27152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.College of Family Physicians of Canada . Family Medicine Professional Profile. College of Family Physicians of Canada, 2018. [Google Scholar]
- 12.Chappell NL, Hollander MJ. An evidence-based policy prescription for an aging population. Healthc Pap 2011;11:8–18. 10.12927/hcpap.2011.22246 [DOI] [PubMed] [Google Scholar]
- 13.Adams WL, McIlvain HE, Lacy NL, et al. Primary care for elderly people: Why do doctors find it so hard Gerontologist 2002;42:835–42. 10.1093/geront/42.6.835 [DOI] [PubMed] [Google Scholar]
- 14.Mangin D, Sweeney K, Heath I. Preventive health care in elderly people needs Rethinking. BMJ 2007;335:285–7. 10.1136/bmj.39241.630741.BE1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Korownyk C, McCormack J, Kolber MR, et al. Competing demands and opportunities in primary care. Can Fam Physician 2017;63:664–8. [PMC free article] [PubMed] [Google Scholar]
- 16.Millar E, Stanley J, Gurney J, et al. Effect of Multimorbidity on health service utilisation and health care experiences. J Prim Health Care 2018;10:44–53. 10.1071/HC17074 [DOI] [PubMed] [Google Scholar]
- 17.Barer ML, Evans RG, Hertzman C. Avalanche or glacier?: health care and the demographic rhetoric. Can J Aging 1995;14:193–224. 10.1017/S0714980800011818 [DOI] [Google Scholar]
- 18.Canadian Institute for Health Information . Health care in Canada, 2011: A focus on seniors and aging. 2012. Available: https://www.deslibris.ca/ID/230734 [Accessed 20 Apr 2022].
- 19.Kabir M, Randall E, Mitra G, et al. Resident and early-career family physicians’ focused practice choices in Canada: a qualitative study. Br J Gen Pract 2022;72:e334–41. 10.3399/BJGP.2021.0512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fortune FS Erika Fry . Death by 1,000 clicks: where electronic health records went wrong. Kaiser health news. 2019. Available: https://khn.org/news/death-by-a-thousand-clicks/ [Accessed 17 Jun 2023].
- 21.Starfield B. The hidden inequity in health care. Int J Equity Health 2011;10:15. 10.1186/1475-9276-10-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McKay M. The future of family medicine: Nova Scotia family physicians’ visions and priorities. Final research report. Doctors Nova Scotia, 2023. [Google Scholar]
- 23.Government of Nova Scotia . Office of regulatory affairs and service effectiveness. physician administrative burden survey – final report. 2020. Available: https://doctorsns.com/sites/default/files/2020-11/admin-burden-survey-results.pdf
- 24.Alegbeh A. Patients before paperwork. Nova Scotia’s approach to improving patient care by reducing physician red tape. Canadian Federation of Independent Business, 2023. Available: https://www.cfib-fcei.ca/en/research-economic-analysis/patients-before-paperwork-nova-scotias-approach-to-improving-patient-care-by-reducing-physician-red-tape https://20336445.fs1.hubspotusercontent-na1.net/hubfs/20336445/research/reports/2023/Patients_Before_Paperwork_Report_2023.pdf [Google Scholar]
- 25.CBC News . Fredericton family doctor calls on province to help cut paperwork, free up time for patients. n.d. Available: https://www.cbc.ca/news/canada/new-brunswick/family-doctors-paperwork-new-brunswick-will-stymiest-medical-society-1.6734457
- 26.Apaydin E. Administrative work and job role beliefs in primary care physicians: an analysis of semi-structured interviews. SAGE Open 2020;10:215824401989909. 10.1177/2158244019899092 [DOI] [Google Scholar]
- 27.Canadian Institute for Health Information . Discharge Abstract Database (DAD) metadata. 2023. [Google Scholar]
- 28.Canadian Institute for Health Information . National Health Expenditure Trends 2020—Methodology Notes. Ottawa, ON: CIHI, 2022. [Google Scholar]
- 29.WHO Collaborating Centre for Drug Statistics Methodology . International language for drug utilization research. Available: https://www.whocc.no [Accessed 10 Apr 2023].
- 30.Wagner AK, Soumerai SB, Zhang F, et al. Segmented regression analysis of interrupted time series in medication use research. J Clin Pharm Ther 2002;27:299–309. 10.1046/j.1365-2710.2002.00430.x [DOI] [PubMed] [Google Scholar]
- 31.Archibald MM, Ambagtsheer RC, Casey MG, et al. Using zoom Videoconferencing for qualitative data collection: perceptions and experiences of researchers and participants. International Journal of Qualitative Methods 2019;18:160940691987459. 10.1177/1609406919874596 [DOI] [Google Scholar]
- 32.Gruber M, Eberl JM, Lind F, et al. Qualitative interviews with irregular migrants in times of COVID-19: recourse to remote interview techniques as a possible methodological adjustment. Forum Qualitative Sozialforschung / Forum: Qualitative Social Research 2021;22. 10.17169/fqs-22.1.3563 [DOI] [Google Scholar]
- 33.Sandelowski M. Sample size in qualitative research. Res Nurs Health 1995;18:179–83. 10.1002/nur.4770180211 [DOI] [PubMed] [Google Scholar]
- 34.Morse JM. Analytic strategies and sample size. Qual Health Res 2015;25:1317–8. 10.1177/1049732315602867 [DOI] [PubMed] [Google Scholar]
- 35.Morse JM. Designing funded qualitative research. In: Handbook of Qualitative Research. Sage Publications, Inc, 1994: 220–35. [Google Scholar]
- 36.Lavergne MR, Goldsmith LJ, Grudniewicz A, et al. Practice patterns among early-career primary care (ECPC) physicians and workforce planning implications: protocol for a mixed methods study. BMJ Open 2019;9:e030477. 10.1136/bmjopen-2019-030477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hedden L. Beyond Full-Time Equivalents: Gender Differences in Activity and Practice Patterns for BC’s Primary Care Physicians. University of British Columbia, 2015. [Google Scholar]
- 38.Buddeberg-Fischer B, Stamm M, Buddeberg C, et al. The impact of gender and parenthood on physicians’ careers - professional and personal situation seven years after graduation. BMC Health Serv Res 2010;10:40. 10.1186/1472-6963-10-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jolly S, Griffith KA, DeCastro R, et al. Gender differences in time spent on parenting and domestic responsibilities by high-achieving young physician-researchers. Ann Intern Med 2014;160:344–53. 10.7326/M13-0974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Canadian Institute for Health Information . Nurse practitioners. 2022. Available: https://www.cihi.ca/en/nurse-practitioners
- 41.Maggino F. Encyclopedia of quality of life and well-being research. In: Thematic Analysis: A Practical Guide. Cham: Sage Publications Ltd, 2020. 10.1007/978-3-319-69909-7 [DOI] [Google Scholar]
- 42.Flick U. Challenges for a new critical qualitative inquiry: introduction to the special issue. Qual Inq 2017;23:3–7. 10.1177/1077800416655829 [DOI] [Google Scholar]
- 43.Denzin NK. Critical qualitative inquiry. Qual Inq 2017;12. 10.4324/9781315421292 [DOI] [Google Scholar]
- 44.Lincoln YS, Lynham SA, Guba EG. Paradigmatic controversies, contradictions, and emerging Confluences, Revisited. In: Denzin NK, Lincoln YS, eds. The Sage handbook of qualitative research. 5th ed. Thousand Oaks, CA: Sage, 2018: 108–50. [Google Scholar]
- 45.Boyland J. A social Constructivist approach to the gathering of empirical data. Australian Counselling Research Journal 2019:30–4. [Google Scholar]
- 46.Boyko JA, Lavis JN, Abelson J, et al. Deliberative dialogues as a mechanism for knowledge translation and Exchange in health systems decision-making. Social Science & Medicine 2012;75:1938–45. 10.1016/j.socscimed.2012.06.016 [DOI] [PubMed] [Google Scholar]
- 47.Harvey N, Holmes CA. Nominal group technique: an effective method for obtaining group consensus. Int J Nurs Pract 2012;18:188–94. 10.1111/j.1440-172X.2012.02017.x [DOI] [PubMed] [Google Scholar]
- 48.Potter M, Gordon S, Hamer P. The nominal group technique: a useful consensus methodology in Physiotherapy research. New Zealand Journal of Physiotherapy 2004;3:70–4. [Google Scholar]
- 49.Guerra CE, McDonald VJ, Ravenell KL, et al. Effect of race on patient expectations regarding their primary care physicians. Family Practice 2007;25:49–55. 10.1093/fampra/cmn005 [DOI] [PubMed] [Google Scholar]
- 50.Hedden L, Barer ML, Cardiff K, et al. The implications of the Feminization of the primary care physician workforce on service supply: a systematic review. Hum Resour Health 2014;12:32. 10.1186/1478-4491-12-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bowen S, Graham I. Integrated knowledge translation. In: Knowledge Translation in Health Care. John Wiley & Sons, Ltd, 2013: 14–23. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-076917supp001.pdf (546.7KB, pdf)
bmjopen-2023-076917supp002.pdf (602KB, pdf)