Abstract
Objective
On 20 July 2021, after the outbreak of COVID-19 at Nanjing Lukou International Airport, several universities started closed management and online teaching. This had a large impact on students’ daily life and study, which may lead to mental health problems. The purpose of this study is to study the effect of screen time on mental health status of university students and the possible mediating effect of sleep status.
Methods
This was a cross-sectional study. A web-based questionnaire survey was employed that included demographic characteristics, sleep status and mental health status (depression, anxiety and loneliness). The Pittsburgh Sleep Quality Index scale was used to assess sleep status, while the Centre for Epidemiologic Studies Depression (CES-D) scale, Generalised Anxiety Disorder-7 (GAD-7) scale and Emotional versus Social Loneliness Scale (ESLS) were used to assess depression, anxiety and loneliness, respectively. Linear and logistic regression models were developed and adjusted for confounding factors, and finally the mediating effects were tested using the Karlson-Holm-Breen method.
Results
Finally, 1070 valid questionnaires were included. Among these, 604 (56.45%) indicated depressive symptoms (CES-D score ≥16) and 902 (84.30%) indicated anxiety symptoms (GAD-7 score ≥10). The mean ESLS score (for loneliness) was 26.51±6.64. The relationship between screen time and depressive symptoms (OR 1.118, 95% CI 1.072 to 1.166) and anxiety symptoms (OR 1.079, 95% CI 1.023 to 1.138) remained significant after adjusting for confounding factors. Meanwhile, sleep status plays an intermediary role in screen time and mental health status (depression and anxiety) and accounts for 13.73% and 19.68% of the total effects, respectively. We did not find a significant association between screen time and loneliness.
Conclusion
During the outbreak of COVID-19, screen time is inevitably prolonged among university students. There is a relationship between mental health and screen time, and sleep status plays a mediating role.
Keywords: Depression & mood disorders, Anxiety disorders, Sleep medicine, MENTAL HEALTH
STRENGTHS AND LIMITATIONS OF THIS STUDY.
The first multiangle study of screen time, sleep status and mental health status of college students during the COVID-19 pandemic including mediation effects.
Internationally recognised scales were used to estimate mental health, so the results are comparable to those of other studies.
The potential confounding factors were adjusted for and multiple sensitivity analyses were conducted, so the results are robust.
This is a cross-sectional study, which is weak in causal inference and has the risk of reverse causality.
Due to the use of online questionnaire, there may be selection bias and information bias.
Introduction
On 20 July 2021, nine Nanjing Lukou International Airport staff tested positive for SARS-CoV-2.1 The government has sought to contain the spread of COVID-19 through lockdowns, limiting travel and restrict people to maintain distance. Many parts of Nanjing have been designated as risk or control areas, and several universities have implemented measures such as closed management and online teaching. In this context, COVID-19 also has a significant impact on mental health.2–4 University students are at an important transition stage in their lives and face a unique set of challenges. Therefore, there is a need to pay attention to the impact of the COVID-19 pandemic on the mental health of university students. Some studies have shown that the psychological pressure on college students caused by COVID-19 is particularly prominent in different age groups.5 6 During the pandemic, screen time is inevitably prolonged among students, and little is known about the exact impact of the COVID-19 pandemic on the mental health of university students.
When universities carry out closed management, the screen time of university students is bound to be extended. Screen time is divided into several areas, such as studying and working, browsing news and socialising. Excessive screen time can affect adolescents’ brain function and cognitive ability.7 The consequences of increased screen time in the wake of the pandemic have been analysed. A study from China concluded that screen time (specifically, time spent studying) is negatively associated with mood status,8 and another study concluded that screen time is correlated with the severity of depression and anxiety.9 Excessive screen time can also lead to increased feelings of loneliness.5 Some studies suggest that outdoor activity or exposure to nature (green time) may diminish the effects of increased screen time,10 11 but apparently, green time does not increase when university students are in closed management.
Lack of sleep affects the physical and mental health and psychosocial function of young people. Studies suggest that excessive screen time can lead to a lack of sleep in different ways: Screen time can replace sleep time12; the strong light emitted by electronic devices before going to bed can inhibit the production of melatonin and cause circadian rhythm disorder13; and teenagers using social media before going to bed not only shorten their sleep time,14 but are also awakened by notifications at night.15 Sleep problems are often accompanied by mental health problems such as depression and anxiety, and are even used as predictors of psychological problems.16 Therefore, we put forward the hypothesis that screen time can affect the mental health of university students, and sleep status plays an intermediary role.
Materials and methods
Study design and sample
This cross-sectional study was conducted from 1 August 2021 to 31 September 2021. The participants were university students studying in China, aged 18–30 years, with no requirements on gender and major. The questionnaire was distributed online and widely disseminated after the pre-experiment, the questionnaires were created and posted on forums and social media through WenJuanxing software (https://www.wjx.cn/). The process of estimating the sample size for this study is described in online supplemental material. A total of 1200 questionnaires were distributed and 1070 valid questionnaires were finally included, with a validity rate of 89.2%, the detailed questionnaire selection process is shown in online supplemental figure S1.
bmjopen-2023-073347supp001.pdf (2.8MB, pdf)
The survey was completely anonymous. The purpose of the study was detailed in the questionnaire guidelines. Informed consent was provided by all participants. Permissions for the questionnaire were set (every IP address can only be used once) to prevent duplication. All questions in the questionnaire were set as required fields to ensure data integrity.
Measures
Screen time
Screen time is defined as the total time spent per day in front of a screen of any electronic device, including mobile phones, tablets and e-books. Screen time is divided into four parts according to the purpose of the screen time: work and study, social activities, audio-visual entertainment and shopping and takeaway, we defined the different screen times categorisations in detail in the questionnaire to avoid bias. These classifications are reported by the respondents themselves. In this study, 18 questionnaires reporting a total of more than 24 hours of screen time per day were excluded (online supplemental figure S1).
Sleep status
Sleep status was assessed using the Pittsburgh Sleep Quality Index (PSQI), a 19-item scale subdivided into seven parts, that is, (1) sleep duration, (2) sleep disturbance, (3) sleep latency, (4) daytime dysfunction due to sleepiness, (5) sleep efficiency, (6) overall sleep quality and (7) sleep medication use,17 with a score of 0–3 for each section and thus a maximum total score of 21. A total score of 5 is often used as the critical value to judge sleep status,18–20 where PSQI<5 is considered good sleep quality and PSQI≥5 is considered bad sleep quality.
Mental health status
In this study, mental health status was assessed based on depression, anxiety and loneliness.
Depression was assessed using the Centre for Epidemiologic Studies Depression (CES-D) scale,21 which is a brief self-report scale containing 20 items with a maximum total score of 60. CES-D≥16 is generally considered to indicate depressive symptoms.22–24
Anxiety was assessed with the Generalised Anxiety Disorder-7 (GAD-7) scale,25 which is also a self-rating scale. The scale has seven items, each with a score of 0–3 points, reaching a maximum total score of 21 points. A GAD-7 score of ≥10 is generally considered to indicate anxiety symptoms.
The Emotional versus Social Loneliness Scale (ESLS)26 was used to evaluate loneliness. The ESLS uses 10 items to evaluate emotional and social loneliness on a scale of 0–5 for each question, with higher scores indicating more intense loneliness.
Covariates
General demographic characteristics and exercise status were included as covariates. General demographic characteristics included: gender, region (Nanjing, non-Nanjing), education (bachelor candidate, master candidate, PhD candidate), type of major (engineering, medicine, liberal arts, other), cost of living (<¥1000, ¥1000–¥2000, ¥2000–¥3000, >¥3000) and change in sports time (decrease, no change, increase) between before and after the COVID-19 outbreak.
Statistical analysis
A database with all collected questionnaire data was created. The total scores were calculated and invalid data were eliminated. Continuous variables are presented as mean and SD after passing the normality test, and categorical variables are presented as absolute values and proportions. The t-test, χ2 test or Spearman’s coefficient test was selected for correlation analysis between variables. The relationships between independent and dependent variables and between independent and mediating variables were examined using logistic regression models (results for dichotomous variables) or linear regression models (results for continuous variables). Two models were developed to account for possible confounders: a crude model without adjusting for any confounders and an adjusted model controlling for differences in gender, region, education level, type of profession, cost of living and time spent doing exercise. After controlling for confounding factors, we also further tested whether the relationship between screen time and mental health status changed when the mediating variable (sleep status) was included. Finally, because the mediating variable was dichotomous and the dependent variable had dichotomous and continuous variables, we used the Karlson-Holm-Breen method27 to calculate the model’s total, direct and indirect effects. We considered a profile effect significant if its CI did not include zero. All statistical analyses were conducted by STATA V.17.0 (StataCorp).
Patient and public involvement
The study participants were not involved in the design of this study.
Result
Participant characteristics
In total, 1070 participants were included. The demographic characteristics of the study population are shown in table 1. Males accounted for 43.08%, the number of undergraduate students was the largest (826, 77.20%), engineering students accounted for 38.60%, most people’s cost of living was in the range of ¥1000–¥2000, accounting for 58.04%, and after the emergence of the pandemic, 76.92% of university students had the same or reduced exercise time. The distribution of screen time and sleep status across mental health conditions is given in table 2. Worse psychological conditions such as depressive symptoms and anxiety symptoms were associated with longer screen time (depression: 7.79 hour vs 8.83 hours, p<0.001; anxiety: 7.98 hours vs 8.85 hours, p=0.001), but similar results were not observed for loneliness symptoms. Poor sleep status tended to be associated with poor mental health status, as did loneliness symptoms. The proportions of people with good sleep and bad sleep are different across mental health conditions (without depression: 47.4% vs 52.6%; with depression: 14.7% vs 85.3%; without anxiety: 41.6% vs 58.4%; with anxiety: 13.7% vs 86.3%). The loneliness score was also lower among people with good sleep than among people with bad sleep (24.98 vs 27.42, p<0.001).
Table 1.
Baseline data
| Characteristics | N | % |
| Gender | ||
| Male | 461 | 43.08 |
| Female | 609 | 56.92 |
| Area | ||
| Nanjing | 711 | 66.45 |
| Non-Nanjing | 359 | 33.55 |
| Education | ||
| Freshman | 226 | 21.12 |
| Sophomore | 207 | 19.35 |
| Junior | 215 | 20.09 |
| Senior | 178 | 16.64 |
| Master candidate | 185 | 17.29 |
| PhD candidate | 59 | 5.51 |
| Type of major | ||
| Engineering | 413 | 38.60 |
| Medicine | 236 | 22.06 |
| Liberal arts* | 361 | 33.74 |
| Other† | 60 | 5.61 |
| Cost of living (Chinese yuan) | ||
| <¥1000 | 194 | 18.13 |
| ¥1000–¥2000 | 621 | 58.04 |
| ¥2000–¥3000 | 203 | 18.97 |
| >¥3000 | 52 | 4.86 |
| Sports time change | ||
| Decrease | 444 | 41.50 |
| No change | 379 | 35.42 |
| Increase | 247 | 23.08 |
*Liberal arts include literature, law and philosophy.
†Other includes science, agriculture, management, economics, art, education, history, military.
Table 2.
Distribution of screen time and sleep status among different mental health status conditions (depression, anxiety and loneliness)
| Characteristics | Depression* | Anxiety† | Loneliness | |||||
| No (N=604) | Yes (N=466) | P value | No (N=902) | Yes (N=168) | P value | P value | ||
| Screen time, hour, mean (SD) | 7.79 (3.14) | 8.83 (3.31) | <0.001 | 7.98 (3.18) | 8.85 (3.40) | 0.001 | 0.0334‡ | 0.2755 |
| Sleep status, n (%)§ | ||||||||
| Good (N=398) | 349 (47.4) | 49 (14.7) | <0.001 | 375 (41.6) | 23 (13.7) | <0.001 | 24.98 (6.40) | <0.001 |
| Bad (N=672) | 388 (52.6) | 284 (85.3) | 527 (58.4) | 145 (86.3) | 27.42 (6.62) | |||
*CES-D score ≥16 indicates depressive symptoms.
†GAD-7 score ≥10 indicates anxiety symptoms.
‡Spearman’s correlation coefficient.
§PSQI score ≥5 indicates bad sleep status.
CES-D, Centre for Epidemiologic Studies Depression; GAD-7, Generalised Anxiety Disorder-7; PSQI, Pittsburgh Sleep Quality Index.
Association of screen time with sleep status and mental health status
Table 3 shows the relationship between screen time and mental health status. In the crude model without adjusting for any confounder, longer screen time was significantly associated with depressive symptoms and anxiety symptoms (depression: OR 1.107, 95% CI 1.065 to 1.151; anxiety: OR 1.084, 95% CI 1.032 to 1.139), but not with loneliness status (β=0.032, 95% CI −0.091 to 0.156). After adjusting for potential confounding factors such as cost of living and changes in exercise time, the relationship between screen time and depressive symptoms (OR 1.118, 95% CI 1.072 to 1.166) and anxiety symptoms (OR 1.079, 95% CI 1.023 to 1.138) remained significant, while the relationship between screen time and loneliness symptoms remained not statistically significant (β=0.106, 95% CI −0.023 to 0.237). Table 3 also shows that increased screen time is a risk factor for sleep status in both the unadjusted crude model (OR 1.069, 95% CI 1.027 to 1.112) and the model after adjusting for confounding factors (OR 1.049, 95% CI 1.005 to 1.095).
Table 3.
Association of screen time with depression, anxiety, loneliness and sleep status
| Depression, OR (95% CI) |
Anxiety, OR (95% CI) |
Loneliness, β (95% CI) |
Sleep status, OR (95% CI) |
|
| Crude model | ||||
| Screen time, hour | 1.107 (1.065 to 1.151)** | 1.084 (1.032 to 1.139)*** | 0.032 (−0.091 to 0.156) | 1.069 (1.027 to 1.112)** |
| Adjusted model | ||||
| Screen time, hour | 1.118 (1.072 to 1.166)*** | 1.079 (1.023 to 1.138)** | 0.107 (−0.023 to 0.237) | 1.049 (1.005 to 1.095)* |
*p<0.05, **p<0.01, ***p<0.001.
Mediating effect of sleep status on the association between screen time and mental health status
The mediation effect of sleep status between screen time and mental health status (depression and anxiety) is shown in table 4. After controlling for screen time (p<0.05) and other covariates, poor sleep status was a risk factor for depressive symptoms (OR 5.044, 95% CI 3.746 to 6.793) and anxiety symptoms (OR 4.449, 95% CI 2.781 to 7.117). The relationship between increased screen time and depressive symptoms (OR 1.115, 95% CI 1.066 to 1.166) and anxiety symptoms (OR 1.067, 95% CI 1.010 to 1.128) remained significant after the inclusion of mediating variables in the model.
Table 4.
Mediating effect of sleep status on the association between screen time and mental health status (depression, anxiety and loneliness)
| Depression, OR (95% CI) | Anxiety, OR (95% CI) | |||||||
| X→Y | X+M→Y | Indirect effect (95% CI) | Proportion of mediation (%) | X→Y | X+M→Y | Indirect Effect (95% CI) |
Proportion of mediation (%) | |
| Screen time, hour | 1.118 (1.072 to1.166)*** |
1.115 (1.066 to 1.166)*** |
0.017 (0.016 to 0.033)* |
13.73% | 1.079 (1.023 to 0.138)** |
1.067 (1.010 to 1.128)* |
0.016 (0.001 to 0.031)* |
19.68% |
| Sleep status, bad versus good | 5.044 (3.746 to 6.793)*** |
4.449 (2.781 to 7.117)*** |
||||||
*p<0.05, **p<0.01, ***p<0.001.
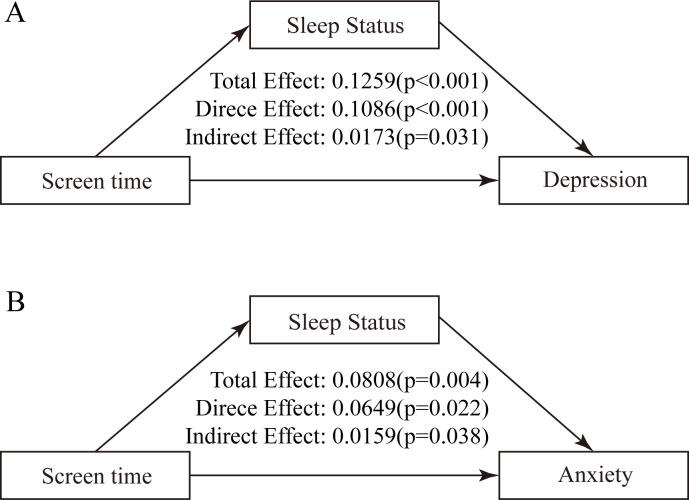
The analysis of mediation effects showed that screen time had a significant indirect effect on both depressive symptoms (indirect effect=0.0173, p<0.05) (figure 1A) and anxiety symptoms (indirect effect=0.0076, p<0.05) (figure 1B) through sleep status after controlling for all covariates. As demonstrated in table 4, the relative proportions of intermediaries are 13.73% and 19.68%, respectively.
Figure 1.
The intermediary model. (A) Screen time+sleep status→ depression. (B) Screen time+sleep status→ anxiety.
Sensitivity analysis
To ensure robustness of the results, we repeated the above analysis after transformation of variables. The results are presented in online supplemental material. As shown in online supplemental tables S1–S6 and figures S2 and S3, when we used the PSQI score as a continuous variable to indicate sleep status, the mediating effect of sleep status between screen time and depressive symptoms and between screen time and anxiety symptoms was increased (depression: indirect effect=0.044, 95% CI 0.022 to 0.066, proportion of mediation=32.89%; anxiety: indirect effect=0.046, 95% CI 0.023 to 0.068, proportion of mediation=57.48%). As shown in online supplemental tables S7–S9 and figure S4, no association was found between screen time and loneliness symptoms, either using the ESLS score as a continuous variable to represent loneliness symptoms or using loneliness symptoms as a dichotomous variable according to the median ESLS score (median=26).
Discussion
In this study, we investigated the relationship between screen time, sleep status and mental health status among university students. The study was conducted shortly after the COVID-19 outbreak at Nanjing Lukou International Airport. We focused on the effects of university closure on students. Our study showed that among university students, screen time was associated with depression and anxiety. No significant relationship between screen time and loneliness was observed. Sleep status partially mediated the effects of screen time on depression and anxiety. This survey was conducted among university students during a COVID-19 outbreak to provide suggestions for healthy care measures at universities during outbreaks.
Logistic regression analysis showed that after adjusting for confounding effects, the proportions of students with depressive symptoms and with anxiety symptoms were higher among university students with long screen time. Several studies conducted in China and abroad have shown that excessive screen time is positively associated with mental health status among university students.28–32 As for the reason for this correlation, some researchers believe that during COVID-19 outbreaks, we get a lot of negative information through electronic media, but the quality of such information is uncontrollable. In addition, fragmented information is prevalent, which leads to an increase in our negative emotions and possibly also to symptoms of depression and anxiety.33–36 In public health emergencies, negative information can be amplified with the influx of information, resulting in more serious consequences.37 Organised sports are one of the most common forms of physical activity for teens, but they are also eliminated during COVID-19, and using a screen to connect with friends and family is the only option.38 In addition, studies have found that longer screen time in adolescents is associated with a decreased attention span,39 violent tendencies40 and low self-esteem,41 all of which are proven risk factors for mental health conditions.42
The results also showed that screen time and sleep status were negatively correlated, and sleep status partially mediated the relationship between screen time and both depression and anxiety, accounting for 13.73% and 19.68% of the total effects, respectively. Excessive screen time may affect melatonin secretion13 and sleep is also affected by nighttime notifications.15 In addition, video games may lead to mental arousal and thus affect sleep,43 and the violent content of video games has a particularly pronounced effect on sleep conditions.44 University students are often surrounded by a large number of electronic devices, especially in places such as dormitories where the division of areas is not clear, and the hindrance to their sleep is very obvious.45 In addition, even if the screen is turned off, electromagnetic radiation may still be perceived as light by the pineal gland, thus affecting the secretion of melatonin and causing sleep difficulties.46 Sleep status was included in this study because sleep status affects physical and psychological functions in young people, including anxiety and depression,47 which may be related to poor sleep, dysfunction of the cholinergic neurotransmitter system and the prefrontal cortex, and increased limbic system activity.48 Moreover, sleep disorders can cause abnormal hormone secretion by interfering with the function of the hypothalamus–pituitary–adrenal axis, which may make the body more sensitive to stress factors in the environment and may induce psychological problems.49 Screen time also has adverse effects on early childhood neurodevelopment. For example, children with longer screen time have significantly lower communication and daily living skill scores.50
This study has several strengths. First, this study is the first multiangle study of screen time, sleep status and mental health status of college students during the COVID-19 pandemic including mediation effects. This is of great significance for the formulation of epidemic prevention and control strategies. Second, we used internationally recognised scales to estimate the mental health status, so the results are comparable with those of other studies. Third, the potential confounding factors were adjusted for and multiple sensitivity analyses were conducted, so the results are robust.
However, there were still some limitations in this study that need to be carefully considered. First, this is a cross-sectional study, which is weak in causal inference and has the risk of reverse causality. Second, the online questionnaire survey may result in selection bias and information bias. Third, the evaluation of some covariates is not accurate, such as the change in sports time. More accurate indicators to evaluate exercise should be considered, such as the International Physical Activity questionnaire.51 Fourth, there is the possibility of bias due to unmeasured confounding factors, such as the study subjects’ living habits and personality. Finally, insomnia may also lead to increased screen time, with potential reverse causality needing to be explored in further longitudinal studies.
In the context of COVID-19 prevention and control, the prolonged use of electronic devices by university students is unavoidable, while the impact of increased screen time on mental health status can be mitigated by improving sleep quality, but how to improve sleep conditions is a question worthy of attention, reducing alcohol and caffeine intake, following a regular bedtime and engaging in meditation practices are more effective ways to improve sleeping conditions.52 Schools and universities should also provide healthcare measures to ensure the physical and mental health of students. A longitudinal study should be conducted in the future to further investigate the association between screen time and mental health status.
Conclusion
At the time of the short-term outbreak of COVID-19, our findings suggest that the after controlling for confounding factors, increased screen time among university students was found to be positively associated with depressive symptoms and anxiety symptoms. Sleep status plays a partially mediating role. Although the COVID-19 pandemic is over, this finding remains potentially valuable and informative in the event of a similar widespread public health event.
Supplementary Material
Acknowledgments
Thanks to the 1251 participants who supported this study, and the language of this article has been polished up by International Science Editing to make it more readable.
Footnotes
Contributors: XH: conceptualisation, funding acquisition, methodology and supervision; WW and JJ: data curation, software, formal analysis and writing–original draft; LQ, FZ, JW and XZ: investigation and validation; BW: project administration and writing–review and editing. XH is the study guarantor.
Funding: This research was supported by National Natural Science Foundation of China (No. 82204057); Basic research program of Jiangsu province (BK20220827); China Postdoctoral Science Foundation funded project (2022M720713).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request from the corresponding author.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Ethics Committee of Zhongda Hospital, Southeast University(2022ZDKYSB013). Participants gave informed consent to participate in the study before taking part.
References
- 1.Liu Y, Yang B, Liu L, et al. Occupational characteristics in the outbreak of the COVID-19 Delta variant in Nanjing, China: rethinking the occupational health and safety vulnerability of essential workers. IJERPH 2021;18:10734. 10.3390/ijerph182010734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Campion J, Javed A, Sartorius N, et al. Addressing the public mental health challenge of COVID-19. Lancet Psychiatry 2020;7:657–9. 10.1016/S2215-0366(20)30240-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Serafini G, Parmigiani B, Amerio A, et al. The psychological impact of COVID-19 on the mental health in the general population. QJM 2020;113:531–7. 10.1093/qjmed/hcaa201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garfin DR, Silver RC, Holman EA. The novel coronavirus (COVID-2019) outbreak: amplification of public health consequences by media exposure. Health Psychol 2020;39:355–7. 10.1037/hea0000875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lisitsa E, Benjamin KS, Chun SK, et al. Loneliness among young adults during COVID-19 pandemic: the mediational roles of social media use and social support seeking. J Soc Clin Psychol 2020;39:708–26. 10.1521/jscp.2020.39.8.708 [DOI] [Google Scholar]
- 6.Browning M, Larson LR, Sharaievska I, et al. Psychological impacts from COVID-19 among university students: risk factors across seven States in the United States. PLoS One 2021;16:e0245327. 10.1371/journal.pone.0245327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yu L, Zhou X. Emotional competence as a mediator of the relationship between Internet addiction and negative emotion in young adolescents in Hong Kong. Appl Res Qual Life 2021;16:2419–38. 10.1007/s11482-021-09912-y [DOI] [Google Scholar]
- 8.Xiao S, Yan Z, Zhao L. Physical activity, screen time, and mood disturbance among Chinese adolescents during COVID-19. J Psychosoc Nurs Ment Health Serv 2021;59:14–20. 10.3928/02793695-20201104-04 [DOI] [PubMed] [Google Scholar]
- 9.Maras D, Flament MF, Murray M, et al. Screen time is associated with depression and anxiety in Canadian youth. Prev Med 2015;73:133–8. 10.1016/j.ypmed.2015.01.029 [DOI] [PubMed] [Google Scholar]
- 10.Wu X, Tao S, Zhang Y, et al. Low physical activity and high screen time can increase the risks of mental health problems and poor sleep quality among Chinese college students. PLoS ONE 2015;10:e0119607. 10.1371/journal.pone.0119607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oswald TK, Rumbold AR, Kedzior SGE, et al. Mental health of young Australians during the COVID-19 pandemic: exploring the roles of employment precarity, screen time, and contact with nature. Int J Environ Res Public Health 2021;18:5630. 10.3390/ijerph18115630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cheung CHM, Bedford R, Saez De Urabain IR, et al. Daily touchscreen use in infants and toddlers is associated with reduced sleep and delayed sleep onset. Sci Rep 2017;7:46104. 10.1038/srep46104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Figueiro M, Overington D. Self-luminous devices and melatonin suppression in adolescents. Light Res Technol 2016;48:966–75. 10.1177/1477153515584979 [DOI] [Google Scholar]
- 14.Grover K, Pecor K, Malkowski M, et al. Effects of instant messaging on school performance in adolescents. J Child Neurol 2016;31:850–7. 10.1177/0883073815624758 [DOI] [PubMed] [Google Scholar]
- 15.Falbe J, Davison KK, Franckle RL, et al. Sleep duration, restfulness, and screens in the sleep environment. Pediatrics 2015;135:e367–75. 10.1542/peds.2014-2306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marinelli M, Sunyer J, Alvarez-Pedrerol M, et al. Hours of television viewing and sleep duration in children: a multicenter birth cohort study. JAMA Pediatr 2014;168:458–64. 10.1001/jamapediatrics.2013.3861 [DOI] [PubMed] [Google Scholar]
- 17.Buysse DJ, Reynolds CF, Monk TH, et al. The pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193–213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 18.Bertolazi AN, Fagondes SC, Hoff LS, et al. Validation of the Brazilian Portuguese version of the pittsburgh sleep quality index. Sleep Med 2011;12:70–5. 10.1016/j.sleep.2010.04.020 [DOI] [PubMed] [Google Scholar]
- 19.Barazzetti L, Garcez A, Freitas Sant’Anna PC, et al. Does sleep quality modify the relationship between common mental disorders and chronic low back pain in adult women. Sleep Med 2022;96:132–9. 10.1016/j.sleep.2022.05.006 [DOI] [PubMed] [Google Scholar]
- 20.Halson SL, Johnston RD, Appaneal RN, et al. Sleep quality in elite athletes: normative values, reliability and understanding contributors to poor sleep. Sports Med 2022;52:417–26. 10.1007/s40279-021-01555-1 [DOI] [PubMed] [Google Scholar]
- 21.RADLOFF LSJAPM . The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement 1977;1:385–401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- 22.Costantine MM, Smith K, Thom EA, et al. Effect of thyroxine therapy on depressive symptoms among women with subclinical hypothyroidism. Obstet Gynecol 2020;135:812–20. 10.1097/AOG.0000000000003724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li Z, Hicks MH-R. The CES-D in Chinese American women: construct validity, diagnostic validity for major depression, and cultural response bias. Psychiatry Research 2010;175:227–32. 10.1016/j.psychres.2009.03.007 [DOI] [PubMed] [Google Scholar]
- 24.Vilagut G, Forero CG, Barbaglia G, et al. Screening for depression in the general population with the center for epidemiologic studies depression (CES-D): a systematic review with meta-analysis. PLoS One 2016;11:e0155431. 10.1371/journal.pone.0155431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Spitzer RL, Kroenke K, Williams JBW, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166:1092–7. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 26.Shaver PR, Brennan K. Measures of depression and loneliness. In: Measures of personality and social psychological attitudes. Academic Press, 1991: 195–289. 10.1016/B978-0-12-590241-0.50010-1 [DOI] [Google Scholar]
- 27.Kohler U, Karlson KB, Holm A. Comparing coefficients of nested nonlinear probability models. Stata J 2011;11:420–38. 10.1177/1536867X1101100306 [DOI] [Google Scholar]
- 28.Feng Q, Zhang Q, Du Y, et al. Associations of physical activity, screen time with depression, anxiety and sleep quality among Chinese college freshmen. PLoS One 2014;9:e100914. 10.1371/journal.pone.0100914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li X, Vanderloo LM, Keown-Stoneman CDG, et al. Screen use and mental health symptoms in Canadian children and youth during the COVID-19 pandemic. JAMA Netw Open 2021;4:e2140875. 10.1001/jamanetworkopen.2021.40875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu M, Wu L, Yao S. Dose-response association of screen time-based sedentary behaviour in children and adolescents and depression: a meta-analysis of observational studies. Br J Sports Med 2016;50:1252–8. 10.1136/bjsports-2015-095084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang W, Du X, Guo Y, et al. Associations among screen time, sleep duration and depressive symptoms among Chinese adolescents. J Affect Disord 2021;284:69–74. 10.1016/j.jad.2021.01.082 [DOI] [PubMed] [Google Scholar]
- 32.Zhang Y, Wu X, Tao S, et al. Associations between screen time, physical activity, and depressive symptoms during the 2019 Coronavirus disease (COVID-19) outbreak among Chinese college students. Environ Health Prev Med 2021;26:107. 10.1186/s12199-021-01025-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chao M, Xue D, Liu T, et al. Media use and acute psychological outcomes during COVID-19 outbreak in China. J Anxiety Disord 2020;74:102248. 10.1016/j.janxdis.2020.102248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dubey S, Biswas P, Ghosh R, et al. Psychosocial impact of COVID-19. Diabetes Metab Syndr 2020;14:779–88. 10.1016/j.dsx.2020.05.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Holman EA, Garfin DR, Silver RC. Media’s role in broadcasting acute stress following the Boston Marathon bombings. Proc Natl Acad Sci U S A 2014;111:93–8. 10.1073/pnas.1316265110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Resnyansky L. Disaster studies, and human communication. IEEE Technol Soc Mag 2014;33:54–65. 10.1109/MTS.2014.2301857 [DOI] [Google Scholar]
- 37.Qin F, Song Y, Nassis GP, et al. Prevalence of insufficient physical activity, sedentary screen time and emotional well-being during the early days of the 2019 novel Coronavirus (COVID-19) outbreak in China: a national cross-sectional study. SSRN Journal 2020. 10.2139/ssrn.3566176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Champion KE, Newton NC, Gardner LA, et al. Health4Life eHealth intervention to modify multiple lifestyle risk behaviours among adolescent students in Australia: a cluster-randomised controlled trial. Lancet Digit Health 2023;5:e276–87. 10.1016/S2589-7500(23)00028-6 [DOI] [PubMed] [Google Scholar]
- 39.Tamana SK, Ezeugwu V, Chikuma J, et al. Screen-time is associated with inattention problems in preschoolers: results from the CHILD birth cohort study. PLoS One 2019;14:e0213995. 10.1371/journal.pone.0213995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Keikha M, Qorbani M, Kazemi Tabaee MS, et al. Screen time activities and aggressive behaviors among children and adolescents: a systematic review. Int J Prev Med 2020;11:59. 10.4103/ijpvm.IJPVM_71_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Braig S, Genuneit J, Walter V, et al. Screen time, physical activity and self-esteem in children: the Ulm birth cohort study. Int J Environ Res Public Health 2018;15:1275. 10.3390/ijerph15061275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Grøntved A, Singhammer J, Froberg K, et al. A prospective study of screen time in adolescence and depression symptoms in young adulthood. Prev Med 2015;81:108–13. 10.1016/j.ypmed.2015.08.009 [DOI] [PubMed] [Google Scholar]
- 43.King DL, Delfabbro PH, Zwaans T, et al. Sleep interference effects of pathological electronic media use during adolescence. Int J Ment Health Addiction 2014;12:21–35. 10.1007/s11469-013-9461-2 [DOI] [Google Scholar]
- 44.Oshima N, Nishida A, Shimodera S, et al. The suicidal feelings, self-injury, and mobile phone use after lights out in adolescents. J Pediatr Psychol 2012;37:1023–30. 10.1093/jpepsy/jss072 [DOI] [PubMed] [Google Scholar]
- 45.Hysing M, Pallesen S, Stormark KM, et al. Sleep and use of electronic devices in adolescence: results from a large population-based study. BMJ Open 2015;5:e006748. 10.1136/bmjopen-2014-006748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Halgamuge MN. Pineal melatonin level disruption in humans due to electromagnetic fields and ICNIRP limits. Radiat Prot Dosimetry 2013;154:405–16. 10.1093/rpd/ncs255 [DOI] [PubMed] [Google Scholar]
- 47.O’Brien LM. The Neurocognitive effects of sleep disruption in children and adolescents. Sleep Med Clin 2011;6:109–16. 10.1016/j.jsmc.2010.12.007 [DOI] [Google Scholar]
- 48.Raniti MB, Allen NB, Schwartz O, et al. Sleep duration and sleep quality: associations with depressive symptoms across adolescence. Behav Sleep Med 2017;15:198–215. 10.1080/15402002.2015.1120198 [DOI] [PubMed] [Google Scholar]
- 49.van Dalfsen JH, Markus CR. The influence of sleep on human hypothalamic–pituitary–adrenal (HPA) axis reactivity: a systematic review. Sleep Med Rev 2018;39:187–94. 10.1016/j.smrv.2017.10.002 [DOI] [PubMed] [Google Scholar]
- 50.Miura M, Tanimoto T. Study inclusions in the association between screen time and neurodevelopment in early childhood. JAMA Pediatr 2023;177:738–9. 10.1001/jamapediatrics.2023.1185 [DOI] [PubMed] [Google Scholar]
- 51.Doane LD, Gress-Smith JL, Breitenstein RS. Multi-method assessments of sleep over the transition to college and the associations with depression and anxiety symptoms. J Youth Adolesc 2015;44:389–404. 10.1007/s10964-014-0150-7 [DOI] [PubMed] [Google Scholar]
- 52.Baranwal N, Yu PK, Siegel NS. Sleep physiology, pathophysiology, and sleep hygiene. Prog Cardiovasc Dis 2023;77:59–69. 10.1016/j.pcad.2023.02.005 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-073347supp001.pdf (2.8MB, pdf)
Data Availability Statement
Data are available upon reasonable request from the corresponding author.