Tweetable abstract
Routine clinical application of thoracic ultrasound has greatly enhanced the process of diagnosing and treating patients with pneumothorax and infectious effusion by minimising radiation exposure and facilitating prompt diagnosis https://bit.ly/3FO6jBg
Introduction
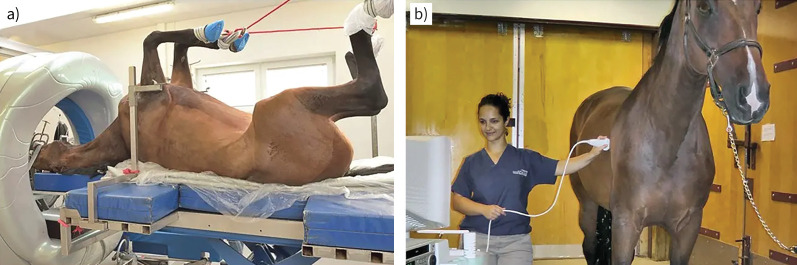
The origin of thoracic ultrasound (TUS) can be traced back to veterinary physician Norman Rantanen, who was driven by the challenges posed in obtaining computed tomography (CT) scans of horses (figure 1). This led him to explore novel methods for investigating conditions of the equine lungs. In the 1980s, Rantanen introduced the concept that TUS could effectively identify pneumothorax, effusion, and the distinctive reverberation artefacts that remain crucial aspects of image interpretation today [1].
FIGURE 1.
a) A horse is subjected to a computed tomography scan. Evidently, this is a resource- and time-consuming procedure requiring a broad array of veterinary competencies and staff. Image from IMV Imaging; reproduced with permission. b) A horse is examined using ultrasound. Note the calm body language of the horse, reflecting the modest discomfort experienced during the procedure. Image from Marion duPont Scott Equine Medical Center; reproduced with permission.
Over the subsequent decades, the supporting evidence for TUS has significantly strengthened, and ultrasound machines are now commonplace in clinical departments dedicated to diagnosing and treating patients with respiratory issues. Notably, emergent or semi-emergent conditions like pneumothorax and infectious effusions have undergone rigorous scientific scrutiny, which has led to substantial scientific advancements. This article will highlight a selection of these contributions.
Pneumothorax
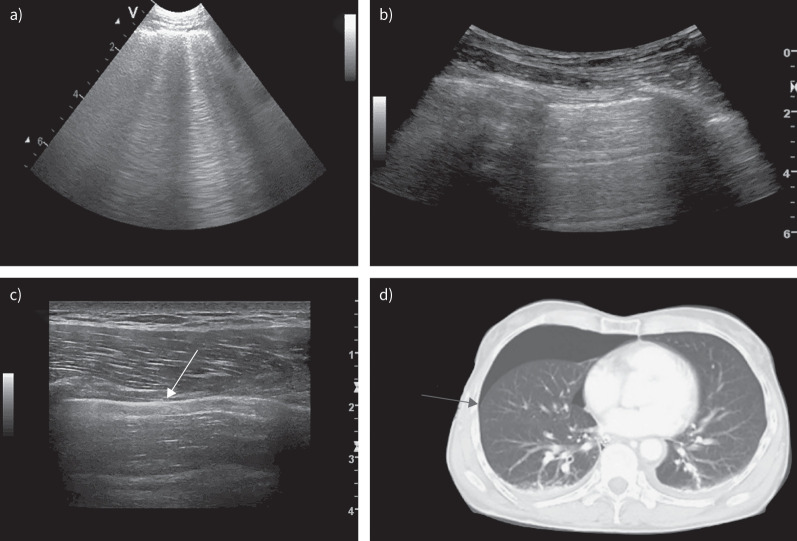
As outlined in a recent statement by the European Respiratory Society (ERS), there are three key ultrasonographic findings that allow clinicians to dismiss suspicion of a pneumothorax [2]. Among these, probably the most well-known is the presence of lung sliding, which manifests as a shimmering effect at the pleural line due to the visceral pleura's movement across the parietal pleura during breathing (figure 2). The second indicator, referred to as the lung pulse, involves subtle movements of the visceral pleura synchronised with the heart's contractions. This sign is particularly valuable when lung sliding is challenging or impossible to detect, such as during apnoea, severe emphysema or intubation in a main bronchus.
FIGURE 2.
a) Multiple B-lines, ruling out the presence of pneumothorax in the scanned zone. The B-lines are hyperechoic, go all the way to the bottom of the screen, erase horizontal A-lines and move with lung sliding. b) A normal standard view with lung sliding (unsurprisingly, this finding is not visible on a still image). c) A lung-point. Lung sliding is present at the left side of the image, whereas the pleural line is completely static on the right side. The white arrow indicates the lung point, which represents the junction where the lung ends and the pneumothorax starts. d) A computed tomography scan from the same patient as in c); the arrow corresponds to the lung point.
Lastly, the existence of the B-line artefact also serves to rule out the presence of pneumothorax. This artefact arises from and corresponds with physical changes in the superficial lung tissue; thus, as ultrasound waves cannot travel through air, presence of B-lines necessitates contact between the visceral and parietal pleura [3].
The utilisation of B-lines in suspected pneumothorax was initially documented by Lichtenstein et al. [4] in 1999, who termed it the “comet-tail artefact”. This phenomenon was defined as “a roughly vertical narrow-based, laser ray-like hyperechogenic reverberation artefact arising from the pleural line and spreading up to the edge of the screen” [4]. In their examination of 190 hemithoraces, the researchers found that the comet-tail artefact was conspicuously absent in all 42 cases of pneumothorax.
Unsurprisingly, these promising findings spurred subsequent studies that corroborated the initial results. In 2004, the term “comet-tail artefact” was replaced with “B-line”, while adding the requirements for this artefact to move in concert with lung sliding and eliminate the horizontal reverberation artefacts of the pleura, commonly known as A-lines [5, 6].
In addition to its ability to rule out pneumothorax, TUS can also provide confirmation of the diagnosis through the identification of a lung point. This finding indicates the region where the visceral and parietal pleura alternate between making direct contact and disengaging from each other during the breathing cycle. From an ultrasound perspective, this manifestation is observed as a stationary pleural line on one side of the screen that is partially replaced by lung sliding upon inhalation. As mentioned in the recent statement article from the ERS, presence or absence of lung sliding may also be appreciated by means of M-mode, which would reveal the characteristic seashore sign or barcode sign, respectively [2]. It is important to note that recognising a lung point necessitates a point of connection between the visceral and parietal pleura, which is not present if the lung is completely collapsed.
In 2013, a systematic review and meta-analysis conducted by Alrajab et al. [7] reported the sensitivity of TUS at 78.6% (95% CI 68.1–98.1%) and specificity at 98.4% (95% CI 97.3–99.5%) in cases of suspected pneumothorax. Despite a diagnostic accuracy superior to that of chest radiography, the ensuing academic discourse revealed notable controversy regarding the actual specificity of the lung point. A prominent example is the 2021 review by Skulec et al. [8], highlighting several ultrasonographic findings that can mimic a lung point. One of these is the physiological lung point sign, which can be observed by aligning the probe longitudinally at the fourth to fifth intercostal space parasternally. Consequently, it is possible to display a tissue interface including both mediastinal tissue with the absence of pleural sliding and a normally aerated lung with pleural sliding. Another example is the aptly named bleb point sign, which is observable in patients with bullous degeneration of the pulmonary parenchyma. The sign may be encountered at the boundary between the bulla and preserved aerated lung tissue. However, despite these concerns, research consistently demonstrated impressive diagnostic accuracies, exemplified in a recent Cochrane review by Chan et al. [9], which reported a sensitivity of 0.91 (95% CI 0.85–0.94) and a specificity of 0.99 (95% CI 0.97–1.00) for pneumothorax in trauma patients. Seemingly, as stated by Santos-Silva et al. [10] in a thorough manuscript on why the above-mentioned situations do not produce a true lung point, “lung point is still a sign specific to pneumothorax”. Lastly, when using TUS to confirm pneumothorax, it is important to recognise that measuring the distance between the parietal and visceral pleura is not possible and that lung sliding may be absent despite pleural contact in the presence of pleural adhesions or bullous emphysema [2]. This raises the question of whether chest radiography remains indispensable for quantification of pneumothorax size. Volpicelli et al. [11] addressed this question in 2014. In a study of 124 patients with pneumothorax scanned in a supine position, the authors reported that the location of the lung point was a useful predictor of pneumothorax volume: the more posteriorly located, the larger the size. Notably, TUS performs well for quantification of the percentage of lung collapse. However, the data in the current literature do not allow us to rely solely on ultrasound to assess the abundance of a pneumothorax.
Infectious effusion
Chest radiography is often the initial imaging modality in emergency departments for patients with respiratory symptoms. However, TUS has demonstrated greater sensitivity and specificity than chest radiography for various common causes of dyspnoea or respiratory symptoms such as pulmonary oedema. TUS also has the capability to confirm or rule out other pathologies, e.g. to distinguish between atelectasis and pneumonia [2, 12].
Approximately 20% of patients with pneumonia are reported to also exhibit pleural effusion; however, utilising TUS this percentage increases to around 50% [13, 14]. Often, effusions seen in the radiograph give an insight into the volume, but the chest radiograph does not add much more information. TUS provides valuable details and information about the fluid and allows probing into characteristics of the effusion in terms of echogenicity, location and whether the effusion contains septations or loculation as a sign of complicated parapneumonic effusion (CPPE) (figure 3).
FIGURE 3.
a) A simple pleural effusion. The fluid is homogeneous, hypoechoic and devoid of septation. To the right of the image, the diaphragm is seen; beneath it, the liver. b) A simple parapneumonic effusion. The pneumonic tissue is hypoechoic compared to adjacent structures and contains air bronchograms, small hyperechoic areas, representing air in the bronchi. c) A complicated parapneumonic effusion (Eff) with septation spanning from the diaphragm above the liver (Lvr) to the pneumonic lung (Pnm). d) Pleural effusion characterised by comprehensive fibrinous material, highly suggestive of empyema.
Minor, simple and uncomplicated parapneumonic effusion (UPPE) is often seen in pneumonia patients without comorbidities, no pleuritic chest pain, and without significant clinical distress. Depending on the patient's clinical presentation, UPPE does not always require intervention. On the contrary, CPPE is associated with significantly higher morbidity and mortality, demanding comprehensive treatment like drainage, and for instance thoracoscopy, intrapleural therapy or surgical intervention [15].
Simple UPPE displays as anechoic effusions with little or no septation and a free-floating, more or less consolidated lung. Despite the scarcity of larger, comparative studies, TUS has demonstrated a robust discriminative yield [16]. The study by Svigals et al. [16] compared ultrasonographic findings with CT findings. They divided the ultrasonographic findings into four categories (anechoic, complex non-septate, complex septate, and homogeneous complex effusions) and used pleural fluid analyses as gold standard. The study found that TUS demonstrated a sensitivity and specificity of 69.2% and 90.0%, respectively, compared to chest CT with sensitivity of 76.9% and specificity of 65.0%. TUS then outperformed chest CT in ruling out CPPE, and the positive likelihood ratio was significantly higher for TUS than for both chest CT and chest radiography. Thus, TUS could play a significant role in the management, monitoring and clinical decision-making for patients with CPPE, although chest CT remains relevant. The time and indications warrant discussion, but chest CT remains essential for cases with limited treatment effectiveness or suspected of clinical worsening (e.g. developing pulmonary abscess or bronchopleural fistula or suspected incorrect placement of the drainage). Furthermore, if the effusion is hyperechoic collections representing pus, it can be difficult to distinguish the complex effusion from the consolidated lung; in this case, contrast-enhanced CT could guide the assessment and subsequent decision-making [17].
Timely pleural fluid evacuation and analyses form fundamental pillars in CPPE treatment. Given the aetiological differences between pleural and pulmonary infections, fluid analyses could guide the microbial therapy. Ultrasound guidance for pleural aspiration or drainage insertion is considered the contemporary gold standard and is in many institutions most often handled by physicians and not radiologists [18]. Adequate training is imperative for both point-of-care TUS and ultrasound-guided procedures. Various training recommendations have been published emphasising, especially for the ultrasound-guided procedures, simulation-based training prior to performing the ultrasound-guided aspiration or drainage on patients [2].
Contrast-enhanced ultrasound, as a supplement to conventional B-mode ultrasound, has been gaining notable attention within the past couple of years and in the aspect of infectious pleural effusion it has been proved useful in the assessment of catheter placement [19]. Also, it is to be noted that the septation and/or lobulation can lead to differences in echogenicity and pH in the different effusion pockets. Using contrast through the drain, it is possible to visualise which pockets are connected and which are isolated and perhaps need another drain or other intervention like interpleural enzyme therapy.
Summary
In summary, the diligent scientific exploration of TUS has produced significant breakthroughs. These findings have greatly enhanced the process of diagnosing and treating patients with pneumothorax and infectious effusion. Through its ability to minimise radiation exposure and facilitate prompt diagnosis, routine clinical application of TUS has the potential to positively impact patient outcomes and overall quality of life.
Footnotes
Conflicts of interest: C. Falster reports personal fees from Bristol-Myers Squibb, outside the submitted work. T. Gille reports personal fees from Roche S.A.S., and other support from Oxyvie (oxygen provider), Vivisol France (oxygen provider) and Menarini France, outside the submitted work; T. Gille is a current member of the Breathe editorial board. The remaining authors have nothing to disclose.
References
- 1.Rantanen NW. Diseases of the thorax. Vet Clin North Am Equine Pract 1986; 2: 49–66. doi: 10.1016/s0749-0739(17)30732-0 [DOI] [PubMed] [Google Scholar]
- 2.Laursen CB, Clive A, Hallifax R, et al. . European Respiratory Society statement on thoracic ultrasound. Eur Respir J 2021; 57: 2001519. doi: 10.1183/13993003.01519-2020 [DOI] [PubMed] [Google Scholar]
- 3.Soldati G, Demi M, Inchingolo R, et al. . On the physical basis of pulmonary sonographic interstitial syndrome. J Ultrasound Med 2016; 35: 2075–2086. doi: 10.7863/ultra.15.08023 [DOI] [PubMed] [Google Scholar]
- 4.Lichtenstein D, Mezière G, Biderman P, et al. . The comet-tail artifact: an ultrasound sign ruling out pneumothorax. Intensive Care Med 1999; 25: 383–388. doi: 10.1007/s001340050862 [DOI] [PubMed] [Google Scholar]
- 5.Lichtenstein D. Lung ultrasound in the critically ill. In: Vincent JL, ed. Yearbook of Intensive Care and Emergency Medicine. Heidelberg, Springer, 2004; pp. 625–644. [Google Scholar]
- 6.Lichtenstein DA, Mezière G, Lascols N, et al. . Ultrasound diagnosis of occult pneumothorax. Crit Care Med 2005; 33: 1231–1238. doi: 10.1097/01.CCM.0000164542.86954.B4 [DOI] [PubMed] [Google Scholar]
- 7.Alrajab S, Youssef AM, Akkus NI, et al. . Pleural ultrasonography versus chest radiography for the diagnosis of pneumothorax: review of the literature and meta-analysis. Crit Care 2013; 17: R208. doi: 10.1186/cc13016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Skulec R, Parizek T, David M, et al. . Lung point sign in ultrasound diagnostics of pneumothorax: imitations and variants. Emerg Med Int 2021; 2021: 6897946. doi: 10.1155/2021/6897946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chan KK, Joo DA, McRae AD, et al. . Chest ultrasonography versus supine chest radiography for diagnosis of pneumothorax in trauma patients in the emergency department. Cochrane Database Syst Rev 2020; 7: CD013031. doi: 10.1002/14651858.CD013031.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Santos-Silva J, Lichtenstein D, Tuinman PR, et al. . The lung point, still a sign specific to pneumothorax. Intensive Care Med 2019; 45: 1327–1328. doi: 10.1007/s00134-019-05677-z [DOI] [PubMed] [Google Scholar]
- 11.Volpicelli G, Boero E, Sverzellati N, et al. . Semi-quantification of pneumothorax volume by lung ultrasound. Intensive Care Med 2014; 40: 1460–1467. doi: 10.1007/s00134-014-3402-9 [DOI] [PubMed] [Google Scholar]
- 12.Alzahrani SA, Al-Salamah MA, Al-Madani WH, et al. . Systematic review and meta-analysis for the use of ultrasound versus radiology in diagnosing of pneumonia. Crit Ultrasound J 2017; 9: 6. doi: 10.1186/s13089-017-0059-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reissig A, Copetti R, Mathis G, et al. . Lung ultrasound in the diagnosis and follow-up of community-acquired pneumonia: a prospective, multicenter, diagnostic accuracy study. Chest 2012; 142: 965–972. doi: 10.1378/chest.12-0364 [DOI] [PubMed] [Google Scholar]
- 14.Garoute C, Rault I, Gosset-Woimant M, et al. . Pleural ultrasonography, new standard for para pneumonic effusion? French multicentric prospective study. Preliminary report. Eur Respir J 2017; 50: Suppl. 61, PA2116. doi: 10.1183/1393003.congress-2017.PA2116 [DOI] [Google Scholar]
- 15.Bedawi EO, Ricciardi S, Hassan M, et al. . ERS/ESTS statement on the management of pleural infection in adults. Eur Respir J 2023; 61: 2201062. doi: 10.1183/13993003.01062-2022 [DOI] [PubMed] [Google Scholar]
- 16.Svigals PZ, Chopra A, Ravenel JG, et al. . The accuracy of pleural ultrasonography in diagnosing complicated parapneumonic pleural effusions. Thorax 2017; 72: 94–95. doi: 10.1136/thoraxjnl-2016-208904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hassan M, Mercer RM, Rahman NM. Thoracic ultrasound in the modern management of pleural disease. Eur Respir Rev 2020; 29: 190136. doi: 10.1183/16000617.0136-2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Havelock T, Teoh R, Laws D, et al. . Pleural procedures and thoracic ultrasound: British Thoracic Society pleural disease guideline 2010. Thorax 2010; 65: Suppl. 2, i61–i76. doi: 10.1136/thx.2010.137026 [DOI] [PubMed] [Google Scholar]
- 19.Bi K, Wang B, Zhang Y, et al. . Contrast-enhanced ultrasound of the pleural cavity: a method to locate pleural catheters and identify fibrous septa. Ultrasound Med Biol 2021; 47: 1261–1268. doi: 10.1016/j.ultrasmedbio.2021.01.011 [DOI] [PubMed] [Google Scholar]