ABSTRACT
Aim:
To study the masticatory efficacy and oral health-related quality of life (OHRQoL) of participants wearing a mandibular overdenture retained by an immediate loading single implant with different occlusal tooth forms.
Materials and Methods:
For this nonrandomized controlled trial study, 27 edentulous participants were selected and randomly divided into three groups (n = 9) based on occlusal tooth forms of the mandibular implant overdenture (MIOD). Group I: participants received an MIOD with an anatomical tooth form; Group II: participants received an MIOD with a semianatomical tooth form; and Group III: participants received an MIOD with a nonanatomical tooth form. For each participant, a single implant (screw root form) was inserted into the midline of the mandibular ridge to support the MIOD. For each group, the masticatory efficiency was evaluated after 3 months, and the OHRQoL of the participants was evaluated after 3 and 6 months. One-way ANOVA and post hoc Tukey’s test were used for data analysis (P < 0.05).
Results:
The masticatory efficiency of the anatomic and semianatomic tooth forms was higher than that of the nonanatomic (P < 0.05). Moreover, the improvement in the participants’ OHRQoL in the anatomic group was more significant than that of other groups (P < 0.05).
Conclusion:
There was a greater improvement in masticatory efficiency and participants’ OHRQoL when fitted with an anatomic tooth form mandibular overdenture retained by an immediate loading single implant than with a semianatomic or nonanatomic tooth form.
Keywords: Immediate loading, occlusal tooth forms, OHIP-EDENT questionnaire, oral health quality of life, overdenture, patient satisfaction, single implant
INTRODUCTION
Completely edentulous patients who wear complete dentures (CDs) frequently have problems with oral function issue due to mandibular prosthesis retention and stability. A well-established treatment for healthy edentulous patients is fitting a mandibular implant overdenture (MIOD) retained by an osseointegrated implant; this type of treatment improves the bite force compared with conventional CDs, suggesting that masticatory efficiency is improved. The inserting of 2-implants between two mental foramina to retain MIOD is considered the first treatment option for an edentulous mandible.[1] Evidence suggests that compared to conventional CD, this treatment considerably improves patient-reported outcomes, including patient satisfaction and oral health-related quality of life (OHRQoL).[2,3]
According to research, using only one implant to retain a mandibular overdenture is a more conservative approach.[1,4] Also, it was reported that wearing a single implant mandibular overdenture (SIMOD) improves oral health and OHRQoL.[5,6,7] A SIMOD is a conservative and cost-effective treatment for edentulous patients who are not comfortable with unstable CDs.[8] Moreover, a SIMOD is comparable to a standard 2-implant retained overdenture.[9,10,11,12,13,14,15] Using a SIMOD improved masticatory performance when measured at 1-,[10] 5-,[11] and 10-year[12] follow-ups. Furthermore, insignificant differences had been shown between the 2-groups in terms of survival rate, incidence of maintenance visits, and/or any prosthetic complications.[3,10] Two other clinical trials have measured the masticatory function of MIODs retained by 1-implant or 2-implants[13,14] and concluded that the participant’s chewing function in the SIMOD group was not inferior to the 2-implants overdenture group.
Hence, satisfaction with denture performance might impact the nutritional status of edentulous older adults, particularly those who use SIMOD systems.[16,17] Compared to the delayed healing protocol of traditional systems, immediate loading implants have significant advantages, such as fewer surgical steps, faster rehabilitation, and enhanced participant comfort. Furthermore, a streamlined management protocol is advantageous, particularly for edentulous patients with nonretentive mandibular CDs.[18,19]
In terms of teeth occlusal forms, anatomic teeth forms produced more lateral force than nonanatomic form teeth, according to studies on CDs.[20,21] The effects of different occlusal designs on force distribution in a simulated implant overdenture and its supporting bone revealed that cusped teeth produced 50% more initial breakage forces than flat teeth.[22] Evidence shows that one implant may be sufficient for adequate denture retention and function. Whether one or two implants are used to retain MIOD, the patient outcomes and OHRQoL are comparable. However, there is insufficient long-term evidence about a single implant with an immediate loading protocol.[18,19]
To achieve the same reduction in food particle size, subjects with MIOD require 1.5–3.6 times fewer chewing strokes than CD wearers.[23] Al-Ansari[24] compared various occlusal tooth forms of CD wearers and discovered that anatomic and lingualized posterior teeth forms were preferred over cuspless teeth forms. Similarly, Kaukinen et al.[21] reported that reducing cusp height and inclination limited lateral forces in implant-supported prostheses. Lowering lateral forces helps maintain and preserve osseointegration and is important in force transmission to bone.
Although several studies have investigated the stability and performance of SIMODs, there is less research on the impact on patient satisfaction of different occlusal forms of posterior teeth using a MIOD retained by an immediate loading single implant. The present study aimed to compare the effects of different occlusal tooth forms (anatomic, semianatomic, and nonanatomic) on patients’ masticatory efficiency and OHRQoL of a MIOD retained by immediate loading single implant. The null hypothesis of the present study was that the differences in either masticatory efficiency or OHRQoL for the effect of different occlusal tooth forms of MIOD retained by an immediate loading single implant would be insignificant.
MATERIALS AND METHODS
This nonrandomized controlled clinical study included patients who attended the outpatient department of a Faculty of Dental Medicine in Egypt. A nonrandomized sample of fully edentulous patients was recruited and screened for participation in this study. This study was approved by the Ethical Committee of the Faculty of Dental Medicine, Al-Azhar University Boys, Cairo, number (43/46/03-19).
INCLUSION CRITERIA
Participants were male and female, aged 40–60. They were completely maxillary and mandibular edentulous and required new denture construction. All participants were free from systemic diseases or temporomandibular disorders and had a minimum 4-mm diameter and 10-mm height of residual bone available without ridge augmentation.
EXCLUSION CRITERIA
The study excluded patients with severely atrophied ridges, those with class II and III skeletal relationships, those undergoing chemotherapy or radiotherapy, or those suffering from osteoporosis or hyperparathyroidism. Further, patients having mandibular ridge augmentation and participants who were satisfied with the retention and stability of their CDs were excluded.
STUDY POPULATION AND GROUPING
Twenty-seven participants were selected and subdivided into three nonrandomized groups (nine participants in each). The sample size was calculated based on the results of previous studies[25,26] with a power of 0.82 (1−β error probability) and an effect size of 0.74. The authors increased it to nine participants per group to find the difference in means. The participants were assigned and distributed into three groups according to the occlusal forms of the posterior teeth (Blueline DCL, Ivoclar, Liechtenstein) of the overdenture, namely, anatomic (Group I), semianatomic (Group II), and nonanatomic occlusal forms (Group III).
DENTURE FABRICATION
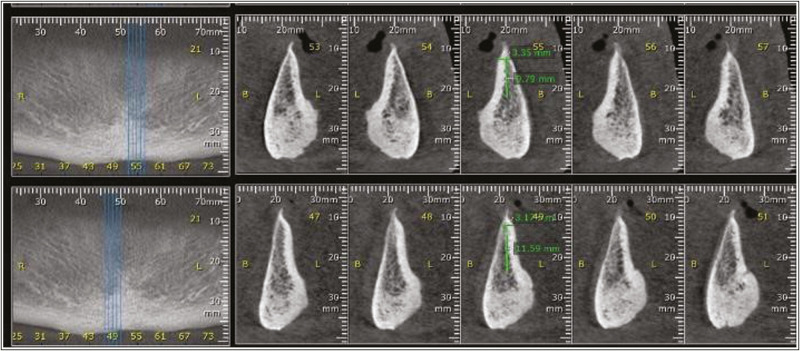
Intraoral examination and radiographic evaluation were carried out on each participant [Figure 1]. The CD was constructed with the specified occlusal tooth form using the standard insertion [26] and recall appointments were carried out [Figure 2]. During the follow-up appointments, necessary adjustments were made to manage problems that had occurred after fitting the prosthesis, such as pain in the oral tissue or ridges or problems with poor fit.
Figure 1.
Preoperative CBCT
Figure 2.
The complete dentures were constructed with a specified occlusal tooth form, (A) anatomic oclusal form, (B) semianatomic occlusal form, and (c) nonanatomic occlusal form
IMPLANT PLACEMENT
After 3 weeks, the participants were recalled for insertion of the implant. A flapless osteotomy was carried out at the midline of the mandibular ridge using a surgical stent [Figure 3], and an endosseous implant with a ball abutment (Multysystem Dental Implants, Italy) was inserted [Figure 4].
Figure 3.

Osteotomy at the midline of the mandibular ridge using a flapless technique
Figure 4.
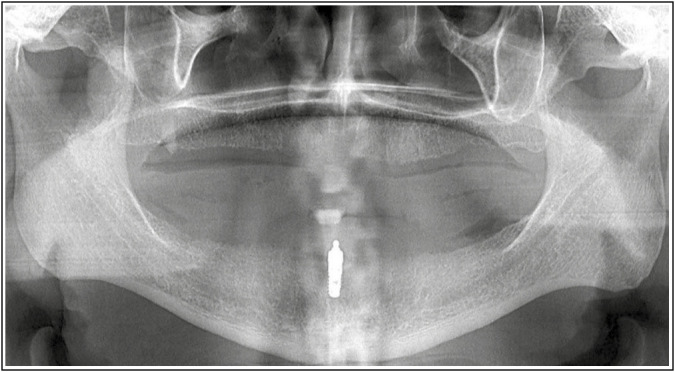
Panoramic X-ray of the endosseous implant with ball abutment
A space in the metal housing was created in the fitting surface of the lower Cd opposite the implant with a round stone burr. The denture was tried in the participant’s mouth to ensure no interference between the attachment and the denture. A small amount of self-cured acrylic resin was placed into the space created in the lower CD, and small increments were applied over the metal housing. The upper and lower CDs were inserted into the participant’s mouth, and the participant was instructed to close the mouth to occlusion. Following polymerization, metal housing and an O ring was picked up in the denture, and excess resin was removed. Pressure-indicating paste was used until uniform contact of the intaglio surface of the denture over the ridge was obtained [Figure 5]. Subsequently, the MIOD was immediately inserted and delivered to the participant after the surgery. Postinsertion instructions were given, and recall visits were carried out.
Figure 5.

O ring was picked up in the denture
MASTICATORY EFFICIENCY
Masticatory efficiency was evaluated for each group after 3 months as follows[25,26,27]: 1-cm cubes of a grain of peanut, a carrot, and a banana were chewed and swallowed normally. The number of chew strokes, the time until the first swallow, the total number of swallows, and the time until the mouth was clean were all recorded. The number of chew strokes and the time elapsed until the 1st swallow, the number of swallows, and the time elapsed until the mouth was free of food were measured. Five items of each test food were chewed, and the means of the five measurements were used as a measure of masticatory efficiency.[28,29]
OHRQOL
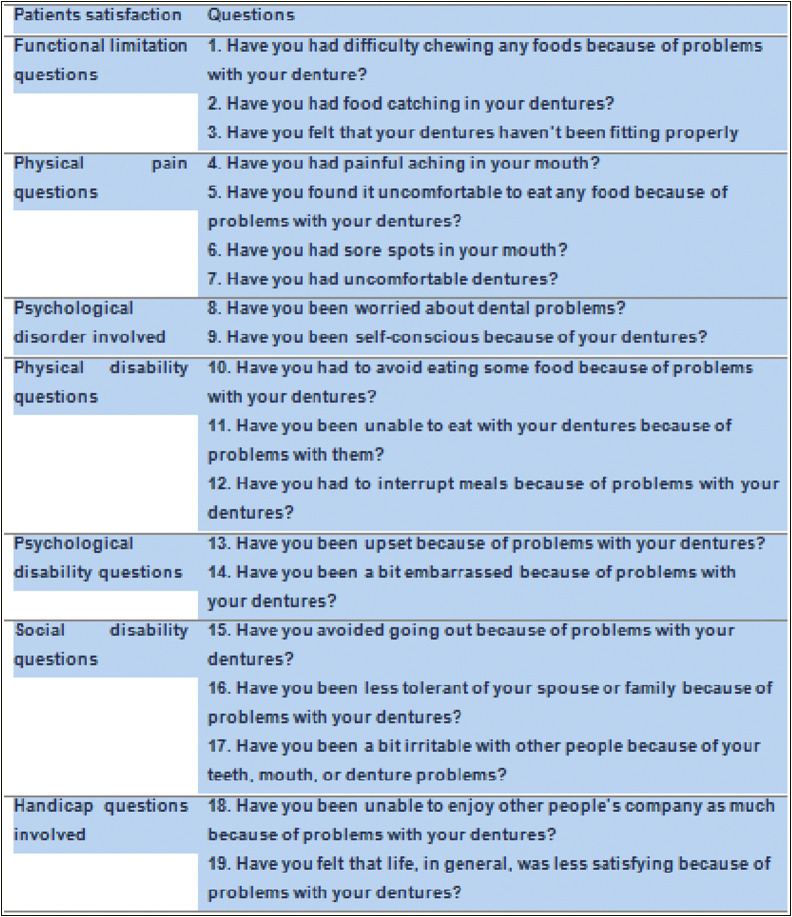
The OHRQoL was evaluated for each group after 3 and 6 months using the Arabic version of the oral health impact profile for edentulous (OHIP-EDENT) questionnaire.[30] The questionnaire was completed by the participants using a Likert-type self-rating scale scored as 0 = never, 1 = hardly ever, 2 = occasionally, 3 = fairly often, and 4 = very often. The sum of the seven measures of the OHIP-EDENT questionnaire was calculated; the lesser the mean scores were considered, the better the quality of life [Figure 6].
Figure 6.
The oral health impact profile for edentulous questionnaire
STATISTICAL ANALYSIS
The data were analyzed using IBM SPSS Statistics Version 20.0 (Armonk, NY: IBM Corp). Statistical analysis was done using a 1-way-ANOVA and a post hoc Tukey test for pair-wise comparisons. The results were analyzed using the means and standard deviations of seven aspects of the outcome measures of participants’ OHRQoL; the lesser the mean scores are, the better the quality of life.
RESULTS
Table 1 shows the mean, standard deviation, and significance between groups. One-way ANOVA showed significant differences between groups with different tooth forms in terms of all tested parameters for masticatory efficiency (P < 0.001) except the number of swallows to empty the mouth of a banana (P = 0.397). A lower number of strokes and shorter times were recorded for the anatomic teeth form group, followed by semianatomic (P < 0.001) except for peanut with the following parameters: number of strokes to mouth emptying (P = 0.347), number of swallows to mouth emptying (P = 0.304), time to first swallow (P = 0.162), and time to mouth emptying (P = 0.182). In comparison to anatomic and semianatomic teeth forms, the nonanatomic form showed a significantly higher number of strokes and time needed for swallows and mouth emptying (P < 0.001), considering all tested parameters. There was a significant increase in time elapsed until the first swallow and until the mouth was empty in the nonanatomic group than other groups when chewing carrots, bananas, and peanuts (P < 0.001).
Table 1.
Comparison between the masticatory efficiency of different groups after 3 months
| Masticatory efficiency test | Group I | Group II | Group III | F | P | |
|---|---|---|---|---|---|---|
| No. of strokes to the first swallow | Raw carrots | 8.88 ± 0.52 | 13.32 ± 0.86 | 16.64 ± 0.17 | 220.333 | <0.001* |
| Banana | 3.14 ± 0.13 | 4.12 ± 0.23 | 5.0 ± 0.28 | 86.573* | <0.001* | |
| Peanut | 8.54 ± 0.26 | 9.82 ± 0.33 | 12.48 ± 0.23 | 261.181* | <0.001* | |
| No. of strokes to mouth empty | Raw carrots | 13.36 ± 0.17 | 18.04 ± 0.26 | 23.56 ± 0.17 | 3153.484 | <0.001* |
| Banana | 3.14 ± 0.13 | 4.12 ± 0.23 | 5.0 ± 0.28 | 86.573* | <0.001* | |
| Peanut | 9.92 ± 0.61a | 10.34 ± 0.48a | 14.64 ± 0.17 | 162.997* | <0.001* | |
| No. of swallows to mouth empty | Raw carrots | 2.08 ± 0.11 | 2.28 ± 0.11 | 2.68 ± 0.11 | 38.889 | <0.001* |
| Banana | 1.0 ± 0.0a | 1.0 ± 0.0a | 1.20 ± 0.45a | 1.000 | 0.397 | |
| Peanut | 2.04 ± 0.09a | 2.20 ± 0.24a | 2.68 ± 0.11 | 20.800* | <0.001* | |
| Time to first swallow (s) | Raw carrots | 5.14 ± 0.15 | 8.02 ± 0.36 | 11.12 ± 0.26 | 618.258 | <0.001* |
| Banana | 2.82 ± 0.19 | 3.76 ± 0.17 | 4.42 ± 0.20 | 90.636* | <0.001* | |
| Peanut | 4.0 ± 0.12a | 5.0 ± 1.38a | 8.40 ± 0.16 | 41.240* | <0.001* | |
| Time to mouth empty (s) | Raw carrots | 8.60 ± 0.27 | 12.64 ± 0.28 | 18.12 ± 0.23 | 1670.517 | <0.001* |
| Banana | 2.82 ± 0.19 | 3.76 ± 0.17 | 4.42 ± 0.20 | 90.636* | <0.001* | |
| Peanut | 8.86 ± 0.15a | 10.48 ± 2.33a | 16.10 ± 0.16 | 39.592* | <0.001* |
*: Statistically significant at P ≤ 0.05. Same letter per raw indicating no significant differences in pairwise comparison between groups
Table 2 presents the variations between OHIP domains. There were significant differences between different groups for all domains at 3 months and 6 months, with different occlusal forms (P < 0.05). Group III scored significantly higher compared to Groups I and II in all domains except Group II vs. Group III in functional limitations after three months (P = 0.649) and physical pain after three months (P = 0.297). Concerning overall patient satisfaction, Group III scored higher than Groups I and II, and there was no significant difference between Groups I and II, which indicated better OHRQoL (P < 0.001).
Table 2.
Comparison between the three studied groups in concern OHIP score
| OHIP domains | Time point | Group I | Group II | Group III | F | P |
|---|---|---|---|---|---|---|
| Functional limitation questions | After 3 months | 3.20 ± 0.84 | 4.78 ± 0.71a | 5.21 ± 0.71a | 9.884* | 0.003* |
| After 6 months | 2.83 ± 0.71a | 3.50 ± 0.71a | 4.78 ± 0.71 | 9.816* | 0.003* | |
| Physical pain | After 3 months | 2.71 ± 0.71a | 3.44 ± 0.71a,b | 4.14 ± 0.71b | 5.113* | 0.025* |
| After 6 months | 2.0 ± 0.71a | 2.20 ± 0.71a | 3.44 ± 0.71 | 6.085* | 0.015* | |
| Psychological disorder involved | After 3 months | 0.75 ± 0.35a | 0.78 ± 0.07a | 1.50 ± 0.14 | 18.030* | <0.001* |
| After 6 months | 0.56 ± 0.09 | 0.30 ± 0.07 | 1.20 ± 0.14 | 97.515* | <0.001* | |
| Physical disability | After 3 months | 2.14 ± 0.71a | 2.78 ± 0.07a | 4.57 ± 0.07 | 46.660* | <0.001* |
| After 6 months | 1.83 ± 0.07 | 2.50 ± 0.07 | 3.78 ± 0.14 | 490.817* | <0.001* | |
| Psychological disability | After 3 months | 1.15 ± 0.22 | 0.87 ± 0.08 | 1.79 ± 0.14 | 43.325* | <0.001* |
| After 6 months | 0.63 ± 0.07 | 0.40 ± 0.07 | 0.87 ± 0.11 | 37.659* | <0.001* | |
| Social disability questions | After 3 months | 0.08 ± 0.01a | 0.11 ± 0.01a | 0.38 ± 0.11 | 49.959* | <0.001* |
| After 6 months | 0.07 ± 0.01a | 0.09 ± 0.02a | 0.25 ± 0.14 | 12.351* | 0.001* | |
| Handicap questions involved | After 3 months | 0.36 ± 0.07 | 0.22 ± 0.07 | 0.50 ± 0.07 | 19.600* | <0.001* |
| After 6 months | 0.17 ± 0.02 | 0.22 ± 0.04 | 0.49 ± 0.03 | 462.250* | <0.001* | |
| Total patient satisfaction | After 3 months | 1.48 ± 0.09a | 1.84 ± 0.24a | 2.58 ± 0.28 | 33.564* | <0.001* |
| After 6 months | 1.16 ± 0.22a | 1.27 ± 0.23a | 2.05 ± 0.28 | 19.455* | <0.001* |
*Statistically significant at P ≤ 0.05. Same letter per raw indicating no significant differences in pairwise comparison between groups
DISCUSSION
The study evaluated masticatory efficiency and participants’ OHRQoL for different occlusal tooth forms of MIOD retained by an immediate loading single implant. Anatomic and semianatomic teeth forms showed better chewing efficiency than nonanatomic teeth forms. Furthermore, the results indicated that the anatomic teeth form group showed better OHRQoL scores. All participants preferred the anatomic and semianatomic to nonanatomic teeth forms. Therefore, the null hypothesis was rejected.
The findings of the current study supported those of Khamis et al.,[31] who compared different anatomic teeth forms (0-, 30-degrees, and lingualized occlusion) of overdenture supported by four root form implants connected with a Hader bar and concluded that patients prefer 30-degree and lingualized occlusal tooth forms over 0-degree forms. The masticatory efficiency method used in this study was recommended since it has been shown to be a reliable measure of masticatory efficiency. ADditionally, it allows users to chew and swallow food normally and is practical for all sorts of food when compared to other techniques.[27]
Most of the participants explained their preference for the anatomic form by their improved ability to chew bananas, followed by peanuts and then raw carrots. Anatomic forms provided better chewing efficiency than semianatomic and nonanatomic forms. This supported the findings of Al-Ansari,[24] who found that participants who received CDs with anatomic posterior occlusal forms were more satisfied with their chewing function than those who received dentures with 0-degree posterior occlusal forms lingualized teeth.
The current study results indicated that the anatomic tooth forms group showed a better OHRQoL. All participants preferred the anatomic and semianatomic forms over the nonanatomic form. Explaining the whole procedure to every patient led to full awareness, which increased patients’ realistic expectations and promoted satisfaction with the overdenture received.[32] Because there is little research on MIODs and occlusal forms, it is difficult to directly compare our findings to those of other studies. This is mainly due to the variations in research design, outcome measures, clinical and technical methods, number of implants, and overdenture attachment systems. Irrespective of the degree of residual ridge resorption, participants who get implant overdentures have reported increased stability, bite force, and predictable masticatory performance.[27,29,31]
Although the use of a single central implant is a cost-effective solution in completely edentulous subjects, avoidance of immediate loading via retention part was recommended, as well as ball and socket type.[33] Therefore, further investigation and evaluation of different occlusal tooth forms on the longevity of MIODs retained by an immediate loading single implant using new attachment systems are recommended for future study. A limitation of this study was that it did not consider psychological factors, such as the relationship of the patient with the dentist and the past experience of the participants with dentures. ADditionally, the quality of the denture foundation area was not considered and should be addressed in future studies.
CONCLUSION
There was a greater improvement in masticatory efficiency and participants’ OHRQoL after being fitted with a mandibular overdenture retained by an immediate loading single implant with an anatomic or semianatomic form.
FINANCIAL SUPPORT AND SPONSORSHIP
This research received no external funding.
CONFLICTS OF INTEREST
The authors declare no conflict of interest.
AUTHORS CONTRIBUTIONS
Not applicable.
ETHICAL POLICY AND INSTITUTIONAL REVIEW BOARD STATEMENT
This clinical study included patients who attended the outpatient at the Faculty of Dental Medicine, Boys, Cairo, Al-Azhar University. All data were kept confidential at the Ethical Committee at Faculty of Dental Medicine, Boys, Cairo, Al-Azhar University under ref no. 43/46/03-19.
PATIENT DECLARATION OF CONSENT
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
DATA AVAILABILITY STATEMENT
Not applicable.
ACKNOWLEDGEMENT
Not available.
REFERENCES
- 1.Feine JS, Carlsson GE, Awad MA, Chehade A, Duncan WJ, Giani S, et al. The McGill consensus statement on overdentures. Montreal, Quebec, Canada. May 24–25, 2002. Int J Prosthodont. 2002;15:413–4. [PubMed] [Google Scholar]
- 2.Aldhohrah T, Mashrah MA, Wang Y. Effect of 2-implant mandibular overdenture with different attachments and loading protocols on peri-implant health and prosthetic complications: A systematic review and network meta-analysis. J Prosthet Dent. 2022;127:832–44. doi: 10.1016/j.prosdent.2020.12.016. [DOI] [PubMed] [Google Scholar]
- 3.Coutinho PC, Nogueira TE, Leles CR. Single-implant mandibular overdentures: Clinical, radiographic, and patient-reported outcomes after a 5-year follow-up. J Prosthet Dent. 2022;128:949–55. doi: 10.1016/j.prosdent.2021.01.007. [DOI] [PubMed] [Google Scholar]
- 4.Emami E, Heydecke G, Rompré PH, de Grandmont P, Feine JS. Impact of implant support for mandibular dentures on satisfaction, oral and general health-related quality of life: A meta-analysis of randomized-controlled trials. Clin Oral Implants Res. 2009;20:533–44. doi: 10.1111/j.1600-0501.2008.01693.x. [DOI] [PubMed] [Google Scholar]
- 5.Fouda K, Fahmy A, Aziz K, Aal MA, Naguib A, Nabi NA. Implant stability changes for a single implant mandibular overdenture. Eur J Dent. 2022;16:619–26. doi: 10.1055/s-0041-1736416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Passia N, Ali S, Behrendt C, Fritzer E, Kohal RJ, Luthardt RG, et al. Single mandibular implant study – chewing efficiency – 5-year results from a randomized clinical trial using two different implant loading protocols. J Prosthodont Res. 2022;66:610–7. doi: 10.2186/jpr.JPR_D_21_00216. [DOI] [PubMed] [Google Scholar]
- 7.Meira IA, Pinheiro MA, CáceresBarreno AH, de Moraes M, Rodrigues Garcia RCM. Speaking space, chewing rotational denture movement, OHRQoL, and patient expectations for single-implant mandibular overdentures. Int J Prosthodont. 2022;35:711–7. doi: 10.11607/ijp.7901. [DOI] [PubMed] [Google Scholar]
- 8.Nogueira TE, Dias DR, Leles CR. Mandibular complete denture versus single-implant overdenture: A systematic review of patient-reported outcomes. J Oral Rehabil. 2017;44:1004–16. doi: 10.1111/joor.12550. [DOI] [PubMed] [Google Scholar]
- 9.Alqutaibi AY, Esposito M, Algabri R, Alfahad A, Kaddah A, Farouk M, et al. Single vs two implant-retained overdentures for edentulous mandibles: A systematic review. Eur J Oral Implantol. 2017;10:243–61. [PubMed] [Google Scholar]
- 10.Nogueira TE, Aguiar FMO, Esfandiari S, Leles CR. Effectiveness of immediately loaded single-implant mandibular overdentures versus mandibular complete dentures: A 1-year follow-up of a randomized clinical trial. J Dent. 2018;77:43–50. doi: 10.1016/j.jdent.2018.07.006. [DOI] [PubMed] [Google Scholar]
- 11.Kronstrom M, Davis B, Loney R, Gerrow J, Hollender L. Satisfaction and clinical outcomes among patients with immediately loaded mandibular overdentures supported by one or two dental implants: Results of a 5-year prospective randomized clinical trial. Int J Oral Maxillofac Implants. 2017;32:128–36. doi: 10.11607/jomi.4824. [DOI] [PubMed] [Google Scholar]
- 12.Passia N, Wolfart S, Kern M. Ten-year clinical outcome of single implant-retained mandibular overdentures—A prospective pilot study. J Dent. 2019;82:63–5. doi: 10.1016/j.jdent.2019.01.006. [DOI] [PubMed] [Google Scholar]
- 13.Resende GP, Jordão LMR, Souza JAC, Schimmel M, Leles CR. Single versus two-implant mandibular overdentures using early-loaded titanium-zirconium implants with hydrophilic surface and ball attachments: 1-year randomized clinical trial. Clin Oral Implants Res. 2021;32:359–68. doi: 10.1111/clr.13707. [DOI] [PubMed] [Google Scholar]
- 14.Paleari AG, Oliveira Junior NM, Marin DOM, Rodriguez LS, ArioliFilho JN, Pero AC, et al. One-year prospective clinical study comparing patient satisfaction and masticatory performance of mandibular overdentures supported by one versus two implants. J Appl Oral Sci. 2018;26:e20160628. doi: 10.1590/1678-7757-2016-0628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nogueira TE, Schimmel M, Leles CR. Changes in masticatory performance of edentulous patients treated with single-implant mandibular overdentures and conventional complete dentures. J Oral Rehabil. 2019;46:268–73. doi: 10.1111/joor.12744. [DOI] [PubMed] [Google Scholar]
- 16.Nogueira TE, Aguiar FMO, de Barcelo’s BA, et al. A 2-year prospective study of single-implant mandibular overdentures: Patient-reported outcomes and prosthodontic events. Clin Oral Implants Res. 2018;29:541–50. doi: 10.1111/clr.13151. [DOI] [PubMed] [Google Scholar]
- 17.Hyland R, Ellis J, Thomason M, El-Feky A, Moynihan P. A qualitative study on patient perspectives of how conventional and implant-supported dentures affect eating. J Dent. 2009;37:718–23. doi: 10.1016/j.jdent.2009.05.028. [DOI] [PubMed] [Google Scholar]
- 18.Walton JN, Glick N, Macentee MI. A randomized clinical trial comparing patient oral health quality of life and prosthetic outcomes with mandibular overdentures retained by one or two implants. Int J Prosthodont. 2009;22:331–9. [PubMed] [Google Scholar]
- 19.Kronstrom M, Davis B, Loney R, Gerrow J, Hollender L. A prospective randomized study on the immediate loading of mandibular overdentures supported by one or two implants: A 12-month follow-up report. Int J Oral Maxillofac Implants. 2010;25:181–8. [PubMed] [Google Scholar]
- 20.Kugimiya Y, Watanabe Y, Igarashi K, Hoshino D, Motokawa K, Edahiro A, et al. Factors associated with masticatory performance in community-dwelling older adults: A cross-sectional study. J Am Dent Assoc. 2020;151:118–26. doi: 10.1016/j.adaj.2019.10.003. [DOI] [PubMed] [Google Scholar]
- 21.Abduo J. Occlusal schemes for complete dentures: A systematic review. Int J Prosthodont. 2013;26:26–33. doi: 10.11607/ijp.3168. [DOI] [PubMed] [Google Scholar]
- 22.kaukinen JA, Edge MJ, Lang BR. The influence of occlusal design on simulated masticatory forces transferred to implant-retained prostheses and supporting bone. J Prosthet Dent. 1996;76:50–5. doi: 10.1016/s0022-3913(96)90346-7. [DOI] [PubMed] [Google Scholar]
- 23.Geertman ME, Slagter AP, van Waas MA, Kalk W. Comminution of food with mandibular implant-retained overdentures. J Dent Res. 1994;73:1858–64. doi: 10.1177/00220345940730121101. [DOI] [PubMed] [Google Scholar]
- 24.Al-Ansari A. Edentulous people prefer lingualized or anatomic posterior occlusal tooth forms. What is the best posterior tooth form for complete dentures? Evid Based Dent. 2007;8:113. doi: 10.1038/sj.ebd.6400530. [DOI] [PubMed] [Google Scholar]
- 25.Ettinger RL, Lindquist TJ. A systematic approach to problem solving for elderly patients wearing complete dentures. Austin J Dent. 2018;5:1102. [Google Scholar]
- 26.Alsayed HAA, Helal MAM, Saker HM, Alkholy MRZ, Baraka OA. Comparison between bilateral balanced occlusion and canine guidance occlusion in mandibular implant overdentures. Al-Azhar J Dent Sci. 2009;12:272–8. [Google Scholar]
- 27.Pebe P, Barbot R, Trinided J, Pesquera A, Lusente J. Nishimura R and Nasr H: Contertorque testing and A histomorphometric analysis of various implant surfaces in canines: A pilot study. Implant Dent. 1997;6:259–65. doi: 10.1097/00008505-199700640-00002. [DOI] [PubMed] [Google Scholar]
- 28.Mericske-Stern RD. Treatment outcomes with implant-supported overdentures: Clinical considerations. J Prosthet Dent. 1998;79:66–73. doi: 10.1016/s0022-3913(98)70196-9. [DOI] [PubMed] [Google Scholar]
- 29.Kimoto K, Garrett NR. Effect of mandibular ridge height on masticatory performance with mandibular conventional and implant-assisted overdentures. Int J Oral Maxillofac Implants. 2003;18:523–30. [PubMed] [Google Scholar]
- 30.Albaker AM. The oral health-related quality of life in edentulous patients treated with conventional complete dentures. Gerodontology. 2013;30:61–6. doi: 10.1111/j.1741-2358.2012.00645.x. [DOI] [PubMed] [Google Scholar]
- 31.Khamis MM, Zaki HS, Rudy TE. A comparison of the effect of different occlusal forms in mandibular implant overdentures. J Prosthet Dent. 1998;79:422–9. doi: 10.1016/s0022-3913(98)70156-8. [DOI] [PubMed] [Google Scholar]
- 32.Aarts JM, Payne AG, Thomson WM. Patients’ evaluation of two occlusal schemes for implant overdentures. Clin Implant Dent Relat Res. 2008;10:140–56. doi: 10.1111/j.1708-8208.2007.00070.x. [DOI] [PubMed] [Google Scholar]
- 33.Kern M, Passia N. The single implant as a minimal restoration in the edentulous mandible Does it work long term? Implantologie. 2021;29:25–35. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.