Abstract
PURPOSE
Performance status (PS) is a crucial assessment for research and clinical practice in lung cancer (LC), including its usage for the assessment of the suitability and toxicity of treatment or eligibility for clinical trials of patients with LC. These PS assessments are subjective and lead to substantial discrepancies between observers. To improve the objectivity of PS assessments, Electronic Activity Monitoring devices (EAMs) are increasingly used in oncology, but how these devices are used for PS assessments in LC is an issue that remains unclear. The goal of this study is to address the challenges and opportunities of the use of digital tools to support PS assessments in patients with LC.
METHODS
The literature review followed PRISMA-ScR methodology. Searches were performed in the ScienceDirect, PsycInfo, ACM, IEEE Xplore, and PubMed databases. Furthermore, a panel discussion was performed to address the clinical use cases.
RESULTS
Thirty-two publications were found. Most of the studies used wrist accelerometry–based wearables (59%) and monitored sleep activity (SA; 28%) or physical activity (PA; 72%). Critical findings include positive usefulness of the use of wearables to categorize moderate-to-vigorous/light PA, which was associated with better sleep and health. In addition, steps and time awake immobile were found to be associated with risk of hospitalization and survival. Use cases identified included the health assessment of patients and clinical research.
CONCLUSION
There are positive experiences in the use of EAM to complement PS assessment in LC. However, there is a need for adapting thresholds to the particularities of patients with LC, for example, differentiating moderate-to-vigorous and light. Moreover, developing methodologies combining PS assessments and the use of EAM adapted to clinical and research practice is needed.
INTRODUCTION
Lung cancer (LC) is the leading cause of death by cancer,1 with a death rate of 18.4%. Moreover, approximately two million new cases were estimated worldwide every year, representing 11.6% of total cancer cases. The two most important types of LC are non–small-cell lung cancer (NSCLC) and small-cell lung cancer (SCLC), which represent 85% and 15% of new LC diagnoses, respectively.2,3 The predominant histologic type of NSCLC is adenocarcinoma, which accounts for around 40% of cases.4 Although there have been improvements in diagnostic and therapeutic approaches over the past few years, overall, 5-year survival rates remain low in NSCLC.5,6
CONTEXT
Key Objective
The study aims to understand the application and challenges of using Electronic Activity Monitoring devices (EAMs) in enhancing the objectivity of performance status (PS) assessments in patients with lung cancer (LC), a unique exploration in the oncology field.
Knowledge Generated
The study found that wearable EAMs are beneficial for categorizing physical activity levels and are associated with improved sleep and health outcomes. Furthermore, measures such as steps and immobile time awake could predict hospitalization risk and survival.
Relevance
These findings can potentially improve the PS assessments in LC, providing a more objective approach in evaluating patients' health and their eligibility for treatments or trials. However, adjustments to activity thresholds and further development of methodologies combining PS assessments and EAMs are needed for LC-specific contexts, offering opportunities for more individualized care and research in clinical practice.
Interestingly, many clinical decisions in LC (among other types of cancers) are based on health indicators that in most cases require subjective assessments. This is the case of performance status (PS), which is an indicator referring to the patients' daily life functionality (eg, walking, working, and self-caring) and is used to predict their health-related quality of life (HrQoL).7 To be more precise, the Eastern Cooperative Oncology Group performance status (ECOG PS)8 scale and the Karnofsky Performance Status Index (KPS)9 are two of the most used instruments to assess PS. These are psychometric tools taking the format of a list of ranked items representing different levels of daily physical functionalities. Scorings of the ECOG PS range from 0 (fully active) to 5 (dead). A level of 2 refers to people who can care and move by themselves more than 50% of time, excluding working activities. On the other hand, the KPS is an 11-point percentage scale ranging from 0 (dead) to 100 (no complaints or evidence of disease). A score of 50 indicates considerable assistance and frequent medical care.
The ECOG PS and KPS have advantages such as their low cost, simplicity, and usability in clinical settings. Nevertheless, biases in terms of discrepancies between observers' assessments have been reported. For example, there have been reports of10,11 interobserver agreement of only 50% between the patient and the oncologist regarding PS score assessments. Significant discrepancies in PS assessment between different health care professionals (eg, nurses v physician) have also been shown.7,12,13
Importantly, these instruments are used not only to predict patient HrQoL but also as guidance for suitability for treatment or eligibility for clinical trials.14 For example, improvements concerning first-line clinical treatments of patients with LC include immunotherapy or its combination with chemotherapy.15 However, patients with LC eligible for some of these types of therapies are mostly those scoring an ECOG PS of 0-1.2,16 Therefore, enhancing the accuracy of PS assessments appears to be critical when considering the abovementioned assessment discrepancies and the relevance of the assessments for clinical practice.
In the face of the foregoing, methodological approaches capable of increasing the objectivity of PS assessments are required to potentially yield more precise clinical decisions in oncology areas and especially in LC because of its lethality.
A promising approach to this issue comes from the hand of novel technological developments in terms of wearable devices. Among these, Electronic Activity Monitoring devices (EAM) are becoming popular because of their increasing availability in the market. EAMs are devices that can take the form of, for example, wrist watches that monitor functional activity (eg, steps count, sedentary behavior [SB], or sleep latencies) and also provide feedback via the screen display or in combination with mobile applications. In recent years, the use of these types of devices has increased exponentially in oncology fields as a mean of gathering more objective patient-generated health data (PGHD).7,17
However, to the best of our knowledge, no specific review has been reported regarding LC, which, considering its prevalence, deserves a special mention. Consequently, a comprehensive review of the current state of the use of EAMs in LC and their potential links to PS could provide further insights for future clinical research.
METHODS
Scoping Review—Eligibility Criteria
Eligible publications were those using wearable activity monitors to investigate their specific use in patients with LC. Study participants could be newly diagnosed, undergoing active treatment, or survivors. Wearable devices were considered eligible if they were worn (eg, on the wrist, arm, waist, or hip) and were used to track any form of physical activity (PA; eg, step count, activity count, sleep, or SB). Usability and acceptability studies were also of interest. The search was limited to publications written in English between January 2010 and August 2020.
Scoping Review—Search Approach
The scoping review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) methodological framework.18 Search terms regarding the population and devices were combined to compose search queries in ScienceDirect, PsycInfo, ACM Library (Association for Computing Machinery), IEEE Xplore, and PubMed databases (Table 1). Screening and selection of eligible records was performed via the Rayyan QCRI web platform, which has been developed to perform literature reviews.19 Two independent reviewers (L.F.-L. and S.C.-T.) screened titles and abstracts. Discrepancies were discussed, and a third reviewer (F.J.N.-B.) was consulted when necessary. Full-text review was performed after that screening.
TABLE 1.
Databases and Search Queries Used in the Review
Data Extraction
Details of the study design (eg, cross-sectional or prospective), details about the type of device used (eg, placement), and patient-reported outcomes (PROs, eg, quality of life [QoL], PA, behavioral/cognitive, PS) were extracted (Table 2).
TABLE 2.
Informative Summary of the Articles Included in the Review
Discussion of Results in the Virtual Panel
The results from the scoping review were designed to also inform a panel discussion designed to gather oncologists' perspectives on how to discover the principal factors that influence the PS scoring in clinical practice and to understand how data-enriched PS should be represented to clinicians to be useful and trusted.
Online panel discussion was conducted on September 28, 2021, with the participation of three clinical oncologists, one clinician specialized in pharmacologic treatment, and two facilitators who specialized in medical informatics. The panel discussion was divided into two parts, each related to one study objective:
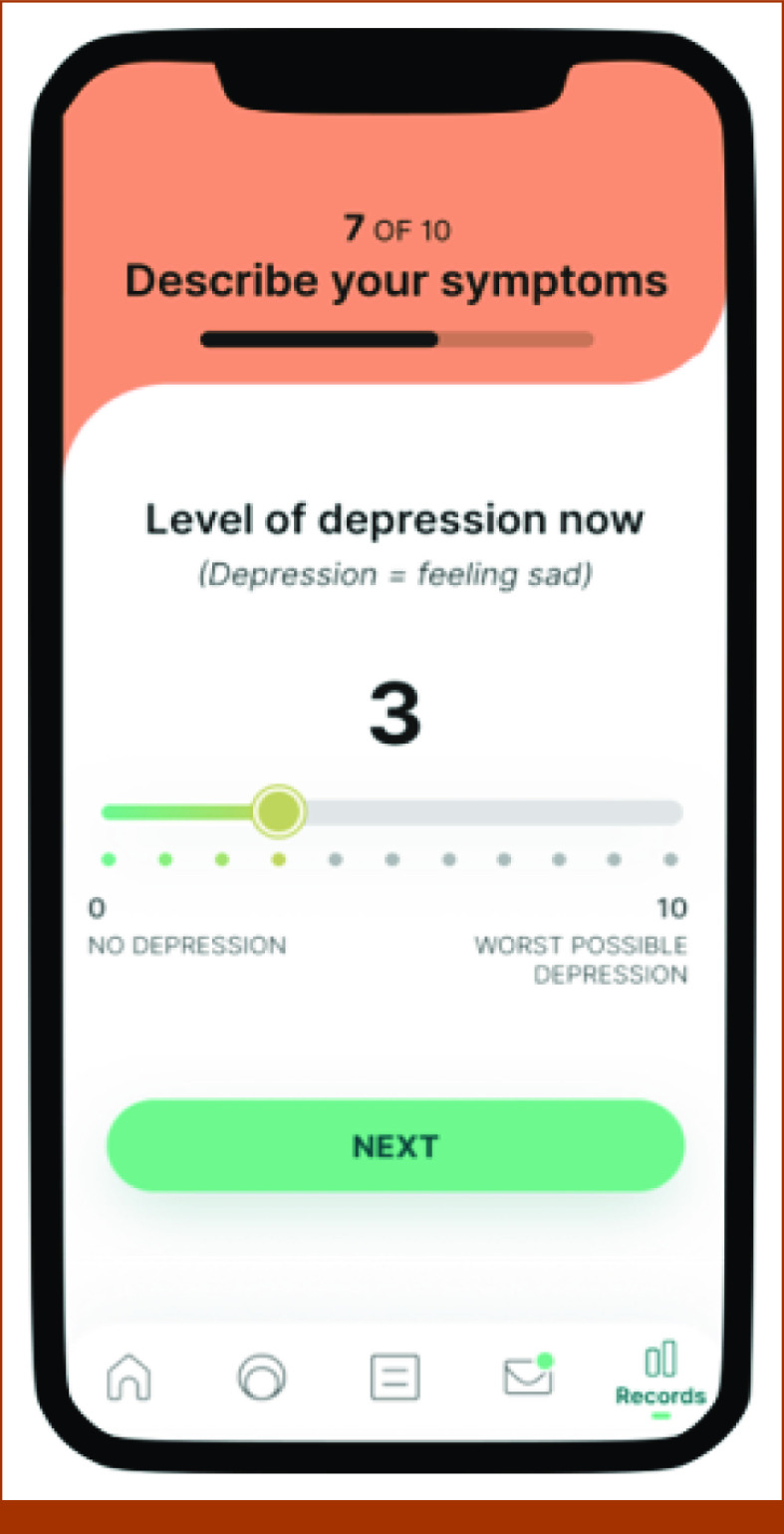
1. A set of hypothetical patient cases (n = 15) were prepared on the basis of real data from the Phase I LUPA study in patients with LC (ClinicalTrials.gov identifier: NCT04751162). The cases included the following personal health data and data on the basis of wearables and mobile psychometrics (eg, sleep quality, psychical activity, perceived symptom burden; Fig 1). Each one of the hypothetical cases was presented to the participating clinicians, and they were asked to individually assess their PS score on the basis of the provided data, using an adaptation of the card-sorting methodology. The scores were collected for all the cases, and the results were discussed.
2. A semistructured panel discussion was conducted focused on how to make PS more actionable and integrated into the clinical workflow. In this session, participants were asked to discuss the integration of mobile- and wearable-based data into clinical practice. This was performed with the use of examples from the literature. The dimensions addressed in this discussion included follow-up of patients, clinical decision support, quality monitoring, and integration with clinical guidelines.
FIG 1.
Mobile Solution (Adhera Health Inc) that can be used to capture ePROs in combination with wearable devices. ePROS, electronic patient-related outcomes.
RESULTS
The initial search identified 419 studies, 21 of which were detected as duplicates. The resulting 398 records were further screened by titles and abstract, yielding 36 records to be included for full-text review. After the full-text review, 32 records involving wearable EAMs in LC populations resulted as eligible for the scoping review (Fig 2). Inter-rater reliability by Cohen's kappa (k = 0.65) indicated a moderate agreement between the two reviewers.52
FIG 2.
CONSORT diagram. LC, lung cancer.
Population
Most of the publications targeted a group of patients with NSCLC exclusively (n = 19; 59.4%) or, in addition, a less proportion of patients with SCLC (n = 2; 6.2%). The rest did not specify the type of LC investigated. It is important to note that among the reviewed publications, several belonged to the same study, leading to a total of N = 25 studies. Together, the number of participants was approximately 1,900 (Mage = 65.47). Moreover, approximately half of the publications measured PS directly via either the ECOG PS (n = 13; 53%) or the KPS (n = 6; 18.7%). The other half did not report the use of these PS assessment instruments. In most cases, the assessment of PS was only used as an inclusion criterion and was not linked to the patient-generated data through the used wearables. Generally, participants with an ECOG PS of 0-2 or a KPS of ≥70% were eligible for participation in studies.
Monitored Activity
The studies used EAMs to monitor mainly sleep activity (SA; n = 8; 25%) or PA (n = 23; 72%). One publication investigated associations between SA and PA. The device placement included mostly the wrist/arm (n = 19, 59%), waist (n = 8; 25%), or hip (n = 5, 12%). Moreover, three studies (9%) paired the wearable device with a mobile app, which was used to deliver feedback and also electronic patient-reported outcomes (ePROs, eg, psychometric questionnaires). Two of these studies were also focused on technology acceptance and usability.
In general, the devices included accelerometry, which records activity counts per minute (an epoch). Then, such activity (or its absence) was translated into different parameters such as step counts, total time spent active, peak activity, time awake spent immobile, time spent in moderate-to-vigorous activity, sleep duration, sleep efficiency (SE), total sleep time (TST)/sleep duration, sleep-onset latency (SOL), wake after sleep onset, wakes number and duration, or in-bed/out-of-bed index ratio (I < O). In the following paragraphs, we summarize the most important reported findings in terms of PGHD by the wearables as associated with SA and PA.
SA
As abovementioned, eight publications focused on the use of wearables to investigate SA of patients with LC. In general, all studies report that wearables are reliable to detect and record sleep patterns of patients with LC, which, in many cases, are characterized by symptoms of insomnia (difficulty to fall asleep, staying asleep, waking up during sleep time, or inadequate sleep durations, eg, <7 hours/night). Furthermore, the studies investigated associations mostly between wearable gathered sleep data and PROs in terms of sleep quality, mental health, and QoL psychometric questionnaires.
Reported outcomes concerning patients' sleep quality were measured in most cases using the Pittsburgh Sleep Quality Index (PSQI).53 This is a 19-item questionnaire comprising seven sleep components (subjective sleep quality, sleep latency, sleep duration, habitual SE, sleep disturbances, use of sleep medication, and daytime dysfunction). Together, these components lead to a global sleep quality score ranging from 0 to 27. Scores >5 are considered as poor sleep, but among patients with cancer, scores >8 are also considered.
Grutsch et al22 showed, for example, that lower mean activity during wake time and wake number of episodes during sleep time measured by a wearable, was associated with poor sleep quality, and higher levels of anxiety and depression, particularly regarding outpatients.21 Moreover, the study also reported a link between PS and sleep quality so that poor PS (assessed by the ECOG) correlated with poor sleep quality, and specifically daytime dysfunction.
Taking into consideration the fact that age can affect the circadian rhythms, one of the studies showed that groups of patients both younger and older than 65 years, showing worse I < O ratios, reported not only poorer sleep quality but also earlier mortality risk.33 Poor sleep parameters were also associated with worsened QoL, including symptoms of fatigue, pain, and loss of appetite.23
On the other hand, six studies used a sleep diary/log (eg, Wang et al,20 TST “last night I slept a total of [n hours],” waking episodes “I woke up during the night [number of times],” “My sleep quality was [0-10; from very bad to very good]”) or a more elaborated interview to contextualize objective information concerning the sleep experiences.44 In general, the sleep diary/interview and the wearable-gathered information correlated satisfactorily. Nevertheless, wearables tend to objectively detect poorer sleep experiences than subjective instruments, probably because of recall biases.20,44
PA
As for SA, the reviewed studies reported that, in general, objectively measured PA by the wearables is feasible and useful in LC settings. Among the monitored information, step counts was one of the most representative outcomes (n = 15; 65.5%).
On the one hand, two studies specifically addressed the usability and acceptability of commercial wearable devices that monitored step counts and, in addition, are required to synchronize the device with a mobile app.49,51 This is an important issue since actual device-wearing time is not usually reported in detail. It was shown, for example, that a great number of participants are capable of performing such synchronization (approximately 70%), which in turn, seems to be associated with adherence to wearing the device.49
On the other hand, step counts were observed as an indicator of differential activity levels depending on exogenous variables such as season weather.48 In other cases, step counts were used to examine differential activity levels between patients (eg, higher vs lower levels of cachexia;39) or as a primary outcome to measure the effects of nutritional and PA intervention programs.24,38,41 Furthermore, Ohri et al31 were able to show that continuous activity monitoring in patients receiving radiotherapy predicted hospitalization risk. Concretely, the study reported a 38% reduction of hospitalization risk for every 1,000 steps taken each day (before radiotherapy until few weeks afterward).
Importantly, a greater number of steps have also been associated with improved QoL, physical and emotional functioning, dyspnea, and pain.37,40 On the contrary, time awake spent immobile was found to be negatively correlated with QoL.45
Interestingly, beyond step counts, the intensity levels of PA seem to also play a major role in health of patients with LC. Thresholds of wearable-based activity counts per minute (cpm) have been proposed to determine sedentary time (<100 cpm), light-intensity physical activity (LIPA; 100-1,951 cpm), and moderate-to-vigorous physical activity (MVPA; ≥1,952 cpm).54 In this regard, it has been observed that LIPA rather than, MVPA, is associated with improved fatigue, lower symptoms of depression, and higher satisfaction with life.34
In fact, a study investigating associations between physical and SA showed that LIPA was associated with greater total wearable-measured sleep time and efficiency.28 Together, these findings point to the idea of promoting training programs for patients with LC that address PA goals of light intensity rather than moderate intensity.
Finally, it is noteworthy that only two of the reviewed studies explicitly addressed links between PS and patient-generated health data through the wearables. Specifically, Ohri et al46 explored correspondences between ECOG PS levels and clusters of inactive, moderately active, and highly active, on the basis of step counts. Fujisawa et al45 reported associations, with higher time awake spent immobile correlating with higher ECOG PS levels (0-2). Interestingly, among patients with an ECOG PS of 0-1, a 10% increase in immobility was associated with worse survival of patients with LC, whereas the PS assessment itself did not predict survival.
Integration Into the Clinical Practice—Panel Discussion
During the panel discussion described in the Methods section, the clinicians agreed that symptomatology and PA self-reported data need to be integrated with other personal factors that can only be gathered in the clinical visit (eg, unawareness, lack of understanding, fear, etc) that influence the story that patients tell their oncologists, which is crucial to assess the overall performance of patients in their daily lives. In terms of PA, a crucial element to understand is the intensity and duration of the PA.
During the panel discussion, clinicians provided insight on how PS enriched with wearable- and mobile-based psychometrics can help better stratify patients for clinical trials and also personalize the care during the clinical practice. This should not be considered only at one point (start of oncologic treatment) but supports a continuous follow-up including different time points to detect patient-level trends and variation across the patient journey. Using mobile and wearable data across the treatment regimens of LC can support a better understanding of the evolving needs of patients.
The integration into the clinical practice also requires presenting these new data insights in a visual way that facilitates clinician understanding of the health status without requiring complex and time-consuming analysis. For example, participants highlighted the importance of plotting wearable data (PA and SA) along the day hours and the activity intensity was marked with colors. These data insights can complement PS scoring together with symptoms and other health data.
The panelist also discussed potential barriers for the use of wearable- and mobile-based patient-reported symptoms to complement PS into the clinical practice. First, the trustworthiness of any tool will be of crucial importance, including validation studies in real clinical settings. Second, oncologists will require training on the use of new data-driven approaches to complement PS assessment, especially if these require the use of artificial intelligence techniques.
DISCUSSION
The goal of this scoping review was to address the use of EAM devices in monitoring PGHD as a means to objectivize activity levels of patients with LC.
A key element to consider across the studies reviewed was that there is high acceptability, but we should be cautious about that finding since in most cases, the patients used the devices for short periods of times and not as part of routine clinical practice. Regarding the adherence for long periods of time, there is an ongoing research study55 that will study the use of EAM during 10 weeks combined with mobile-based PROs.
Sleep plays a major role in overall health status of patients with LC.56 Regarding sleep, although polysomnography (PSG) is still considered the gold standard to investigate sleep and circadian patterns,57 data monitored through EAMs, which have the advantage of being used in more ecologic patient settings (eg, home), have been shown to positively correlate with PSG reports.58 In this regard, the studies reviewed here support the fact that patients with cancer present high levels of sleep-related burdens, including insomnia, fatigue, restlessness, and sleepiness, on the basis of objective wearable-based information complementing sleep diaries and psychometric instruments such as PSQI. That is an important point because subjective sleep assessments serve to contextualize objective measured data. At the same time, however, these assessments are subject to recall bias. For example, in some cases, participants tended to overestimate the sleep duration or underestimate wake episodes as compared with the data gathered through the wearables.20,25
The review also highlights the idea of investigating several aspects referring to PA of patients with LC, in more detail.
First, LIPA seems to be very helpful to improve mental and physical health of patients with LC, even more than MVPA standard recommendations for patients with cancer (eg, ≥150 minutes per week).59 Thresholds to categorize wearable-based activity counts per minute into inactivity (<100 cpm), LIPA (100-1,951 cpm), or (MVPA ≥1,952 cpm) have been proposed elsewhere.54 However, it might be well the case that these thresholds do not account for the particular health characteristics of people living with a chronic condition or, more specifically, LC,60 hence requiring further adaptation to specific populations.61
Second, another aspect addressed refers to specific wearable-based indicators, which have shown promising associations with health aspects of patients with LC. Concretely, step count measurement seems to be useful to predict risk of hospitalization46 and time awake spent immobile (TAI) was associated with worse survival.45
Furthermore, third, a critical question related to step counts and TAI is that they are objective indicators, which have been explicitly linked to conventional PS assessment via ECOG PS.45 However, as abovementioned, only two publications tackled this question. This is highly relevant because such links may serve to yield more comprehensive and informative clinical assessments in oncology settings. Consequently, developing further methodologies that help to stablish more robust links between PS assessments and wearable-based PGHD are required.
In addition, from an interventional point of view, tailored PA programs that include personalized motivational messages through the app have also been shown to be associated with device-wearing adherence and less missing reported information.38 Reported drawbacks with regard to device adherence (particularly of the wrist type) are related to skin irritation or bad ergonomics.51,62
A major limitation of the studies here reviewed is that they are not clearly describing the use of wearables for health status monitoring in patients with LC as part of the routine clinical practice. We should be aware of wronging concerns about the implementation challenges of new data-driven solution in oncologic clinical practice.63 Therefore, it seems that further research specifically addressing the prospective collection of wearable-based activity data is needed to undergo an actionable assessment of PA and PS in patients with LC. There are many potential aspects that can hinder the application of those devices into the clinical practice, from concerns about trustworthiness to usability.64 Although the use of wearables to monitor sleep quality is already a clinical gold standard in sleep medicine (ie, PSG), they are not meant to be used for longer periods of time (typically 1 week). Another major limitation of current research, which was highlighted in the panel, was the need to consider well the context of the patients, including socioeconomical aspects, which is also related to the known barrier digital health literacy and accessibility.65
We should consider that there is a growing usage of mobile applications in oncology, many of which include the use of psychometrics.66 This eventually might raise the need to consider how to combine different heterogenous sources of patient-generated data, including mobile and wearable data.67-69 Furthermore, there is ongoing research to include new sensors to better understand aspects of relevance to understand the health status of patients with LC, including breathing sensors and electrocardiograms, among others.70-74 The incorporation of those devices might also rise concerns in terms of equity and accessibility for such technology. In this review, we did not address implementation and economic implications of the use of reviewed technologies. This is a matter of great importance for future research as the sustainability of health care systems across the globe is being challenged by the increasing prevalence of cancer.
Future research should investigate the utility and feasibility of incorporating those in the clinical practice and research, considering specific use cases such as the creation of patient registries or integration in clinical guidelines,75,76 including research that helps defining quality thresholds for specific clinical and research use cases. For example, the quality threshold of potential sensor-derived predictions will be different if they are designed to simply complement the available information from the clinician about overall well-being of a patient or even suggest a PS concrete level.
Another important aspect not covered in this review, which merits further research, is the impact of regulation with regard to software as a medical device. In particular, there are emerging concerns about safety issues of software and hardware technologies that might be used to support clinical decision-making such as cancer risk assessment.77 This is of special importance in the context of artificial intelligence solutions where the quality of the data is a crucial element for the output of such systems in oncology,78,79 and it is also linked to regulatory and governance issues.80 In these potential future applications on the basis of extensive data collection and artificial intelligence–based outputs, we should always be careful about the acceptability by end users (eg, clinicians and patients) to avoid potential safety concerns (eg, not understanding the reliability of artificial intelligence–based algorithms) or end-user fatigue (eg, complex and confusing interfaces that generate user fatigue).
In conclusion, the reviewed literature showed that wearable EAM devices provide oncologists with a new opportunity to potentially assess in an objective and unobtrusive manner their patients' daily PA performance in real-world settings and to better understand the personal determinants leading to optimal health outcomes. This fact has the possibility to provide them with enhanced tools in clinical routine toward a more personalized health care delivery although further validation in prospective studies is needed. The panel of experts highlighted the need to further investigate the application of such technologies in clearly defined implementation use cases such as enhancing research activities or routine clinical practice.
ACKNOWLEDGMENT
The authors acknowledge the support from the Adhera Health, Inc. team for providing their expertise and insights.
Santiago Ponce Aix
Consulting or Advisory Role: Roche, Bristol Myers Squibb
Speakers' Bureau: Bristol Myers Squibb, Roche, AstraZeneca
Travel, Accommodations, Expenses: AstraZeneca, Roche
Francisco J. Núñez-Benjumea
Research Funding: Vifor Pharma (Inst), GlaxoSmithKline (Inst), Astellas Pharma (Inst), Janssen (Inst)
Pablo Arnáiz
Employment: Roche
Stock and Other Ownership Interests: Roche
Luis Fernández-Luque
Employment: Adhera Health
Stock and Other Ownership Interests: Adhera Health
Patents, Royalties, Other Intellectual Property: Two patents pending
Uncompensated Relationships: Adhera Health (Inst)
No other potential conflicts of interest were reported.
PRIOR PRESENTATION
Presented in part at the ASCO Annual Meeting, virtual, June 4-8, 2021.
SUPPORT
Supported by Roche Farma S.A.
DATA SHARING STATEMENT
Qualified researchers may request access to individual patient-level data through the clinical study data request platform (https://vivli.org/). Further details on Roche's criteria for eligible studies are available at https://vivli.org/members/ourmembers/. For further details on Roche's Global Policy on the Sharing of Clinical Information and how to request access to related clinical study documents, see (https://www.roche.com/research_and_development/who_we_are_how_we_work/clinical_trials/our_commitment_to_data_sharing.htm).
AUTHOR CONTRIBUTIONS
Conception and design: Francisco J. Núñez-Benjumea, Pablo Arnáiz, Luis Fernández-Luque
Administrative support: Andrés Flores
Provision of study materials or patients: Santiago Ponce Aix
Collection and assembly of data: Luis Fernández-Luque
Data analysis and interpretation: Santiago Ponce Aix, Sergio Cervera-Torres, Andrés Flores, Luis Fernández-Luque
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/cci/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Santiago Ponce Aix
Consulting or Advisory Role: Roche, Bristol Myers Squibb
Speakers' Bureau: Bristol Myers Squibb, Roche, AstraZeneca
Travel, Accommodations, Expenses: AstraZeneca, Roche
Francisco J. Núñez-Benjumea
Research Funding: Vifor Pharma (Inst), GlaxoSmithKline (Inst), Astellas Pharma (Inst), Janssen (Inst)
Pablo Arnáiz
Employment: Roche
Stock and Other Ownership Interests: Roche
Luis Fernández-Luque
Employment: Adhera Health
Stock and Other Ownership Interests: Adhera Health
Patents, Royalties, Other Intellectual Property: Two patents pending
Uncompensated Relationships: Adhera Health (Inst)
No other potential conflicts of interest were reported.
REFERENCES
- 1.Bray F, Ferlay J, Soerjomataram I, et al. : Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394-424, 2018 [DOI] [PubMed] [Google Scholar]
- 2.Friedlaender A, Liu SV, Passaro A, et al. : The role of performance status in small-cell lung cancer in the era of immune checkpoint inhibitors. Clin Lung Cancer 21:e539-e543, 2020 [DOI] [PubMed] [Google Scholar]
- 3.Molina JR, Yang P, Cassivi SD, et al. : Non-small cell lung cancer: Epidemiology, risk factors, treatment, and survivorship. Mayo Clinic Proc 83:584-594, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Travis WD, Brambilla E, Nicholson AG, et al. : The 2015 World Health Organization Classification of Lung Tumors: Impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol 10:1243-1260, 2015 [DOI] [PubMed] [Google Scholar]
- 5.Cetin K, Ettinger DS, Hei YJ, et al. : Survival by histologic subtype in stage IV nonsmall cell lung cancer based on data from the Surveillance, Epidemiology and End Results Program. Clin Epidemiol 3:139-148, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ferlay J, Colombet M, Soerjomataram I, et al. : Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer 144:1941-1953, 2019 [DOI] [PubMed] [Google Scholar]
- 7.Kelly CM, Shahrokni A: Moving beyond Karnofsky and ECOG performance status assessments with new technologies. J Oncol 2016:e6186543, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oken MM, Creech RH, Tormey DC, et al. : Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5:649-656, 1982 [PubMed] [Google Scholar]
- 9.Karnofsky D, Burchenal J: The clinical evaluation of Chemotherapeutic agents in cancer, in MacLeod CM. (ed): Evaluation of Chemotherapeutic Agents, Volume 196. New York, NY, Columbia University Press, 1949 [Google Scholar]
- 10.Blagden SP, Charman SC, Sharples LD, et al. : Performance status score: Do patients and their oncologists agree? Br J Cancer 89:1022-1027, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Azam F, Latif MF, Farooq A, et al. : Performance status assessment by using ECOG (Eastern Cooperative Oncology Group) score for cancer patients by oncology healthcare professionals. Case Rep Oncol 12:728-736, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chow R, Chiu N, Bruera E, et al. : Inter-rater reliability in performance status assessment among health care professionals: A systematic review. Ann Palliat Med 5:83-92, 2016 [DOI] [PubMed] [Google Scholar]
- 13.Neeman E, Gresham G, Ovasapians N, et al. : Comparing physician and nurse Eastern Cooperative Oncology Group Performance Status (ECOG‐PS) ratings as predictors of clinical outcomes in patients with cancer. Oncologist 24:e1460-e1466, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dajczman E, Kasymjanova G, Kreisman H, et al. : Should patient-rated performance status affect treatment decisions in advanced lung cancer? J Thorac Oncol 3:1133-1136, 2008 [DOI] [PubMed] [Google Scholar]
- 15.Duma N, Santana-Davila R, Molina JR: Non–small cell lung cancer: Epidemiology, screening, diagnosis, and treatment. Mayo Clin Proc 94:1623-1640, 2019 [DOI] [PubMed] [Google Scholar]
- 16.Petrillo LA, El-Jawahri A, Nipp RD, et al. : Performance status and end-of-life care among adults with non–small cell lung cancer receiving immune checkpoint inhibitors. Cancer 126:2288-2295, 2020 [DOI] [PubMed] [Google Scholar]
- 17.Kuhn P, Nieva JJ: Physicist vs. physician: Digitizing clinical assessment and using it for evidence-based prediction of outcomes. Bioinformatics, Convergence Science, and Systems Biology. American Association for Cancer Research, 2019 (abstr PL01-01)
- 18.Tricco AC, Lillie E, Zarin W, et al. : PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med 169:467-473, 2018 [DOI] [PubMed] [Google Scholar]
- 19.Ouzzani M, Hammady H, Fedorowicz Z, et al. : Rayyan—A web and mobile app for systematic reviews. Syst Rev 5:210, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang SY, Chang HJ, Lin CC: Sleep disturbances among patients with non-small cell lung cancer in Taiwan: Congruence between sleep log and actigraphy. Cancer Nurs 33:E11, 2010 [DOI] [PubMed] [Google Scholar]
- 21.Du-Quiton J, Wood PA, Burch JB, et al. : Actigraphic assessment of daily sleep–activity pattern abnormalities reflects self-assessed depression and anxiety in outpatients with advanced non-small cell lung cancer. Psychooncology 19:180-189, 2010 [DOI] [PubMed] [Google Scholar]
- 22.Grutsch JF, Wood PA, Du-Quiton J, et al. : Validation of actigraphy to assess circadian organization and sleep quality in patients with advanced lung cancer. J Circadian Rhythms 9:4, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grutsch JF, Ferrans C, Wood PA, et al. : The association of quality of life with potentially remediable disruptions of circadian sleep/activity rhythms in patients with advanced lung cancer. BMC Cancer 11:193, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van der Meij BS, Langius JAE, Spreeuwenberg MD, et al. : Oral nutritional supplements containing n-3 polyunsaturated fatty acids affect quality of life and functional status in lung cancer patients during multimodality treatment: An RCT. Eur J Clin Nutr 66:399-404, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dean GE, Redeker NS, Wang YJ, et al. : Sleep, mood, and quality of life in patients receiving treatment for lung cancer. Oncol Nurs Forum 40:441-451, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Granger CL, McDonald CF, Irving L, et al. : Low physical activity levels and functional decline in individuals with lung cancer. Lung Cancer 83:292-299, 2014 [DOI] [PubMed] [Google Scholar]
- 27.Dean GE, Abu Sabbah E, Yingrengreung S, et al. : Sleeping with the enemy: Sleep and quality of life in patients with lung cancer. Cancer Nurs 38:60-70, 2015 [DOI] [PubMed] [Google Scholar]
- 28.Chen HM, Wu YC, Tsai CM, et al. : Relationships of circadian rhythms and physical activity with objective sleep parameters in lung cancer patients. Cancer Nurs 38:215-223, 2015 [DOI] [PubMed] [Google Scholar]
- 29.Maeda K, Higashimoto Y, Honda N, et al. : Effect of a postoperative outpatient pulmonary rehabilitation program on physical activity in patients who underwent pulmonary resection for lung cancer. Geriatr Gerontol Int 16:550-555, 2016 [DOI] [PubMed] [Google Scholar]
- 30.Dhillon HM, Bell ML, van der Ploeg HP, et al. : Impact of physical activity on fatigue and quality of life in people with advanced lung cancer: A randomized controlled trial. Ann Oncol 28:1889-1897, 2017 [DOI] [PubMed] [Google Scholar]
- 31.Ohri N, Kabarriti R, Bodner WR, et al. : Continuous activity monitoring during concurrent chemoradiotherapy. Int J Radiat Oncol Biol Phys 97:1061-1065, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Timmerman JGJ, Dekker-van Weering MGHM, Wouters MWJM, et al. : Physical behavior and associations with health outcomes in operable NSCLC patients: A prospective study. Lung Cancer 119:91-98, 2018 [DOI] [PubMed] [Google Scholar]
- 33.Chang WP, Smith R, Lin CC: Age and rest-activity rhythm as predictors of survival in patients with newly diagnosed lung cancer. Chronobiol Int 35:188-197, 2018 [DOI] [PubMed] [Google Scholar]
- 34.Vallance JK, Bebb GD, Boyle T, et al. : Psychosocial health is associated with objectively assessed sedentary time and light intensity physical activity among lung cancer survivors. Ment Health Phys Activity 14:61-65, 2018 [Google Scholar]
- 35.D’Silva A, Bebb G, Boyle T, et al. : Demographic and clinical correlates of accelerometer assessed physical activity and sedentary time in lung cancer survivors. Psychooncology 27:1042-1049, 2018 [DOI] [PubMed] [Google Scholar]
- 36.D’Silva A, Gardiner PA, Boyle T, et al. : Associations of objectively assessed physical activity and sedentary time with health-related quality of life among lung cancer survivors: A quantile regression approach. Lung Cancer 119:78-84, 2018 [DOI] [PubMed] [Google Scholar]
- 37.Bade BC, Brooks MC, Nietert SB, et al. : Assessing the correlation between physical activity and quality of life in advanced lung cancer. Integr Cancer Ther 17:73-79, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bade BC, Hyer JM, Bevill BT, et al. : A patient-centered activity regimen improves participation in physical activity interventions in advanced-stage lung cancer. Integr Cancer Ther 17:921-927, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Morikawa A, Naito T, Sugiyama M, et al. : Impact of cancer cachexia on hospitalization-associated physical inactivity in elderly patients with advanced non-small-cell lung cancer. Asia Pac J Oncol Nurs 5:377-382, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mouri T, Naito T, Morikawa A, et al. : Promotion of behavioral change and the impact on quality of life in elderly patients with advanced cancer: A physical activity intervention of the multimodal nutrition and exercise treatment for advanced cancer program. Asia Pac J Oncol Nurs 5:383-390, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Naito T, Mitsunaga S, Miura S, et al. : Feasibility of early multimodal interventions for elderly patients with advanced pancreatic and non-small-cell lung cancer. J Cachexia, Sarcopenia Muscle 10:73-83, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jonsson M, Ahlsson A, Hurtig-Wennlöf A, et al. : In-hospital physiotherapy and physical recovery 3 months after lung cancer surgery: A randomized controlled trial. Integr Cancer Ther 18:1534735419876346, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jonsson M, Ahlsson A, Hurtig-Wennlöf A, et al. In-hospital physiotherapy and physical recovery three months after lung cancer surgery: A randomized controlled trial. 2019. http://urn.kb.se/resolve?urn=urn:nbn:se:oru:diva-73625 [DOI] [PMC free article] [PubMed]
- 44.Dean GE, Ziegler P, Chen H, et al. : Trajectory of insomnia symptoms in older adults with lung cancer: Using mixed methods. Support Care Cancer 27:2255-2263, 2019 [DOI] [PubMed] [Google Scholar]
- 45.Fujisawa D, Temel JS, Greer JA, et al. : Actigraphy as an assessment of performance status in patients with advanced lung cancer. Pall Supp Care 17:574-578, 2019 [DOI] [PubMed] [Google Scholar]
- 46.Ohri N, Halmos B, Bodner WR, et al. : Daily step counts: A new prognostic factor in locally advanced non-small cell lung cancer? Int J Radiat Oncol Biol Phys 105:745-751, 2019 [DOI] [PubMed] [Google Scholar]
- 47.Paul S, Bodner WR, Garg M, et al. : Cardiac irradiation predicts activity decline in patients receiving concurrent chemoradiation for locally advanced lung cancer. Int J Radiat Oncol Biol Phys 108:597-601, 2020 [DOI] [PubMed] [Google Scholar]
- 48.Kong S, Park HY, Kang D, et al. : Seasonal variation in physical activity among preoperative patients with lung cancer determined using a wearable device. J Clin Med 9:349, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Miyaji T, Kawaguchi T, Azuma K, et al. : Patient-generated health data collection using a wearable activity tracker in cancer patients—A feasibility study. Support Care Cancer 28:5953-5961, 2020 [DOI] [PubMed] [Google Scholar]
- 50.Cavalheri V, Jenkins S, Cecins N, et al. : Patterns of sedentary behaviour and physical activity in people following curative intent treatment for non-small cell lung cancer. Chron Respir Dis 13:82-85, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Finley DJ, Fay KA, Batsis JA, et al. : A feasibility study of an unsupervised, pre-operative exercise program for adults with lung cancer. Eur J Cancer Care 29:e13254, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McHugh ML: Interrater reliability: The kappa statistic. Biochemia Med 22:276-282, 2012 [PMC free article] [PubMed] [Google Scholar]
- 53.Buysse DJ, Reynolds CF, Monk TH, et al. : The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res 28:193-213, 1989 [DOI] [PubMed] [Google Scholar]
- 54.Freedson PS, Melanson E, Sirard J: Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc 30:777-781, 1998 [DOI] [PubMed] [Google Scholar]
- 55.Aix SP, Lopez M, Núñez-Benjumea F, et al. : P43. 03 LUPA-01: An observational study to monitor lung cancer patients’ activity and assess performance status through a wearable device in Spain. J Thorac Oncol 16:S1083, 2021 [Google Scholar]
- 56.Nishiura M, Tamura A, Nagai H, et al. : Assessment of sleep disturbance in lung cancer patients: Relationship between sleep disturbance and pain, fatigue, quality of life, and psychological distress. Pall Supp Care 13:575-581, 2015 [DOI] [PubMed] [Google Scholar]
- 57.Lim DC, Mazzotti DR, Sutherland K, et al. : Reinventing polysomnography in the age of precision medicine. Sleep Med Rev 52:101313, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Scott H, Lack L, Lovato N: A systematic review of the accuracy of sleep wearable devices for estimating sleep onset. Sleep Med Rev 49:101227, 2020 [DOI] [PubMed] [Google Scholar]
- 59.Schmitz KH, Courneya KS, Matthews C, et al. : American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Med Sci Sports Exerc 42:1409-1426, 2010 [DOI] [PubMed] [Google Scholar]
- 60.Peddle-Mcintyre CJ, Cavalheri V, Boyle T, et al. : A review of accelerometer-based activity monitoring in cancer survivorship research. Med Sci Sports Exerc 50:1790-1801, 2018 [DOI] [PubMed] [Google Scholar]
- 61.Wijndaele K, Westgate K, Stephens SK, et al. : Utilization and harmonization of adult accelerometry data: Review and expert consensus. Med Sci Sports Exerc 47:2129-2139, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Crane TE, Skiba MB, Miller A, et al. : Development and evaluation of an accelerometer-based protocol for measuring physical activity levels in cancer survivors: Development and usability study. JMIR Mhealth Uhealth 8:e18491, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Patel S, Goldsack JC, Cordovano G, et al. : Advancing digital health innovation in oncology: Priorities for high-value digital transformation in cancer care. J Med Internet Res 25:e43404, 2023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pavic M, Klaas V, Theile G, et al. : Feasibility and usability aspects of continuous remote monitoring of health status in palliative cancer patients using wearables. Oncology 98:386-395, 2020 [DOI] [PubMed] [Google Scholar]
- 65.Verma R, Saldanha C, Ellis U, et al. : eHealth literacy among older adults living with cancer and their caregivers: A scoping review. J Geriatr Oncol 13:555-562, 2022 [DOI] [PubMed] [Google Scholar]
- 66.Upadhyay VA, Landman AB, Hassett MJ: Landscape analysis of oncology mobile health applications. JCO Clin Cancer Inform 10.1200/CCI.20.00156 [DOI] [PubMed] [Google Scholar]
- 67.Cox SM, Lane A, Volchenboum SL: Use of wearable, mobile, and sensor technology in cancer clinical trials. JCO Clin Cancer Inform 10.1200/CCI.17.00147 [DOI] [PubMed] [Google Scholar]
- 68.Nilanon T, Nocera LP, Martin AS, et al. : Use of wearable activity tracker in patients with cancer undergoing chemotherapy: Toward evaluating risk of unplanned health care encounters. JCO Clin Cancer Inform 10.1200/CCI.20.00023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gupta A, Stewart T, Bhulani N, et al. : Feasibility of wearable physical activity monitors in patients with cancer. JCO Clin Cancer Inform 10.1200/CCI.17.00152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Davies HJ, Bachtiger P, Williams I, et al. : Wearable in-ear PPG: Detailed respiratory variations enable classification of COPD. IEEE Trans Biomed Eng 69:2390-2400, 2022 [DOI] [PubMed] [Google Scholar]
- 71.Marland JRK, Gray ME, Dunare C, et al. : Real-time measurement of tumour hypoxia using an implantable microfabricated oxygen sensor. Sens Biosensing Res 30:100375, 2020 [Google Scholar]
- 72.Yu Q, Chen J, Fu W, et al. : Smartphone-based platforms for clinical detections in lung-cancer-related exhaled breath biomarkers: A review. Biosensors (Basel) 12:223, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zhai T, Li Y, Brown R, et al. : Spirometry at diagnosis and overall survival in non-small cell lung cancer patients. Cancer Med 11:4796-4805, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zhan X, Long H, Gou F, et al. : A convolutional neural network-based intelligent medical system with sensors for assistive diagnosis and decision-making in non-small cell lung cancer. Sensors (Basel) 21:7996, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Basch E, Stover AM, Schrag D, et al. : Clinical utility and user perceptions of a digital system for electronic patient-reported symptom monitoring during routine cancer care: Findings from the PRO-TECT trial. JCO Clin Cancer Inform 10.1200/CCI.20.00081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Maruszczyk K, Aiyegbusi OL, Torlinska B, et al. : Systematic review of guidance for the collection and use of patient-reported outcomes in real-world evidence generation to support regulation, reimbursement and health policy. J Patient Rep Outcomes 6:57, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.McInerney CD, Scott BC, Johnson OA: Are regulations safe? Reflections from developing a digital cancer decision-support tool. JCO Clin Cancer Inform 10.1200/CCI.20.00148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bertsimas D, Wiberg H: Machine learning in oncology: Methods, applications, and challenges. JCO Clin Cancer Inform 10.1200/CCI.20.00072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Nagy M, Radakovich N, Nazha A: Machine learning in oncology: What should clinicians know? JCO Clin Cancer Inform 10.1200/CCI.20.00049 [DOI] [PubMed] [Google Scholar]
- 80.Reddy S, Allan S, Coghlan S, et al. : A governance model for the application of AI in health care. J Am Med Inform Assoc 27:491-497, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Qualified researchers may request access to individual patient-level data through the clinical study data request platform (https://vivli.org/). Further details on Roche's criteria for eligible studies are available at https://vivli.org/members/ourmembers/. For further details on Roche's Global Policy on the Sharing of Clinical Information and how to request access to related clinical study documents, see (https://www.roche.com/research_and_development/who_we_are_how_we_work/clinical_trials/our_commitment_to_data_sharing.htm).