Abstract
Background
The human immunodeficiency virus (HIV) epidemic has disproportionately affected African, Caribbean and Black (ACB) communities in Canada. We investigated the prevalence and factors associated with HIV infection among ACB people in Ontario.
Methods
A cross-sectional survey of first- and second-generation ACB people aged 15–64 years in Toronto and Ottawa (Ontario, Canada). We collected sociodemographic information, self-reported HIV status and offered dried blood spot (DBS) testing to determine the prevalence of HIV infection. Factors associated with HIV infection were investigated using regression models.
Results
A total of 1,380 people were interviewed and 834 (60.4%) tested for HIV. The HIV prevalence was 7.5% overall (95% confidence interval [CI] 7.1–8.0) and 6.6% (95% CI 6.1–7.1) in the adult population (15–49 years). Higher age (adjusted odds ratio [aOR] 2.8; 95% CI 2.77–2.82), birth outside of Canada (aOR 4.7; 95% CI 1.50–14.71), French language (aOR 9.83; 95% CI 5.19–18.61), unemployment (aOR 1.85; 95% CI 1.62–2.11), part-time employment (aOR 4.64; 95% CI 4.32–4.99), substance use during sex (aOR 1.66; 95% CI 1.47–1.88) and homosexual (aOR 19.68; 95% CI 7.64–50.71) and bisexual orientation (aOR 2.82; 95% CI 1.19–6.65) were associated with a positive HIV test. Those with a high school (aOR 0.01; 95% CI 0.01–0.02), college (aOR 0.00; 95% CI 0.00–0.01) or university education (aOR 0.00; 95% CI 0.00–0.01), more adequate housing (aOR 0.85; 95% CI 0.82–0.88), a higher social capital score (aOR 0.61; 95% CI 0.49–0.74) and a history of sexually transmitted infections (aOR 0.40; 95% CI 0.18–0.91) were less likely to have a positive HIV test.
Conclusion
Human immunodeficiency virus infection is linked to sociodemographic, socioeconomic, and behavioural factors among ACB people in Ontario.
Keywords: HIV, high-risk populations, African Caribbean and Black, healthcare resource use, Canada
Introduction
African, Caribbean and Black (ACB) people in Canada experience disproportionately high vulnerability to human immunodeficiency virus (HIV) due to intersecting social determinants that limit their ability to achieve optimal health outcomes ( ((1))). This is further aggravated by HIV-related stigma and discrimination towards communities affected by HIV ( ((2,3))). In Canada, ACB people constitute 2.5% of the population but 16% of people living with HIV ( ((4))). In the province of Ontario, ACB people constitute only 5% of the population but represent 25% of all new infections ( ((4))). Despite these figures, there is limited information on the HIV epidemic among ACB communities living in Canada, and there are currently no official estimates for HIV prevalence in ACB communities. Provincial surveillance data for HIV did not include ethnicity until recently ( ((5,6))), which may be a contributing factor. Despite being close to 40 years into the HIV epidemic, there are no racialized data on ACB people in Canada. As such, there is no agreed upon prevalence estimate for ACB people in Canada. Further, other systemic and structural factors may limit the capacity and resources to conduct research on ACB people, such as experiences of stigma and racial discrimination ( ((2,3))), alongside linguistic barriers ( ((7))) and migration-related issues ( ((8))).
Given that 52% of Canada’s ACB population (over half a million people) live in Ontario ( ((9))), investigations to better understand their vulnerability to HIV infection are beneficial at the national level, including for Canada’s planned response to reduce the burden and impact of sexually transmitted and blood-borne infections ( ((10))).
The purpose of this study (the A/C Study) is to inform policy and practice in Ontario, Canada regarding HIV care for ACB people by investigating the underlying factors that augment HIV risk and vulnerability of ACB people. In this paper, we report on the prevalence of HIV and factors associated with HIV infection.
Methods
We conducted a cross-sectional survey of ACB people in Toronto and Ottawa in Ontario, Canada from January to December 2019. The A/C Study was approved by the relevant Ethics Boards and the full protocol for the A/C Study is published elsewhere ( ((11))). Our study is reported according to the “Strengthening the Reporting of Observational Studies in Epidemiology” (STROBE) guidelines ( ((12))). Participants provided consent for the questionnaire, dried blood spot (DBS) and data linkage to administrative databases.
Eligibility
African, Caribbean and Black people were eligible to participate if they met the following criteria: were living in Toronto or Ottawa and their surrounding municipalities; were born in a Caribbean or Sub-Saharan African country or had a parent born in any of those countries; were 15 to 64 years old at the time of the survey; could communicate in English or French; and provided informed consent. The inclusion of youth as young as 15 years allowed us to capture their unique experiences and special safeguards were put in place, including counsellors and linkage to care ( ((11))).
Sampling
Our sample size estimation was informed by census and survey data on the distributions of ACB populations from the Caribbean and Africa in Toronto and Ottawa ( ((13,14))), a presumed 2% prevalence of HIV among first and second-generation ACB people and the Wilson confidence interval approach with continuity correction ( ((15))). This generated a sample size of 1,500, with 1,000 and 500 participants in Toronto and Ottawa, respectively.
Recruitment
Trained peer recruiters approached potentially eligible ACB people (social networks, events and venues populated by ACB people) to ask if they were interested in participating in the study.
Data collection
We obtained written informed consent for the interview and for collection of a DBS sample. Participants could consent for the interview alone or the interview and the DBS, but not the DBS alone.
The questionnaire was administered in French or English and included the following: socio-demographic information, sexual behaviour, substance use, blood donation, access to and use of health systems and services, and HIV testing, care and treatment. Further details on development and contents of the questionnaire can be found in the published protocol ( ((11))). A DBS sample was collected from all participants who consented to this part of the study; samples were tested by the Public Health Agency of Canada for antibodies against HIV. An honorarium of 40 CAD was offered to each participant. Participants were also offered a point-of-care HIV test.
Statistical analysis
The primary outcome was the result of a DBS HIV test (positive/negative). Participant characteristics analyzed were age group, city, language in which the survey was completed, sex, gender identity, sexual orientation, place of birth, level of education, employment, ability to meet basic needs, housing situation, ever tested for sexually transmitted infections (STIs), self-reported HIV status and social capital index score ( ((16))). The social capital index score was estimated from levels of agreement or disagreement on individuals’ perceptions about their neighbourhood ( ((16))).
We summarized continuous data with means and standard deviations, or medians (quartile 1; quartile 3). Categorical data was described using counts and percentages. We compared our sample to the 2016 Canadian Census profile ( ((17))), and weighted the data to match the age, sex, and city distribution of Black people in the Census. The prevalence of HIV was estimated as the proportion of people with a positive HIV test among those tested. We applied the coefficient of variation (CV)—as used by Statistics Canada—to determine which values were acceptable to report from small subgroups ( ((18))).
The factors associated with HIV infection were assessed using generalized linear models (GLM), adjusted for relevant covariates. Covariates were entered into separate models as blocks comprised of demographic (age [the six age groups were treated as ordinal], gender identity, level of education, place of birth, language, city), socioeconomic (employment status, ability to meet basic needs, housing situation, social capital index score) and sexual behaviour variables (age at first intercourse, substance use during sex, transactional sex, sexual orientation, ever had an STI test). We used robust standard errors to account for clustering within cities (Toronto and Ottawa). Only statistically significant covariates (p<0.05) were entered into the full model. Model fit was assessed using the Akaike Information Criterion (AIC) by comparing full models to partial models (a lower AIC indicates a better fit). Multicollinearity was assessed using the variance inflation factor (VIF) with a VIF>25 suggestive of multicollinearity. The type 1 error rate was set at 5%. Adjusted odds ratios (aOR) and 95% confidence intervals (CIs) are reported. Data were analyzed using Stata version 16.0.
Results
Participant characteristics
We included a total of 1,380 people 15–64 years of age. More people were recruited from Toronto (n=854/61.9%), took the survey in English (n=1,276/92.5%) and were female (n=853/63.4%). Most participants reported ever being tested for STIs (n=762/63.8%) and HIV (n=950/74.6%), with most self-reporting their HIV status as negative (n=848/91.9%). Only 834 (60.4%) participants agreed to take the DBS. A full sociodemographic profile of the participants is shown in Table 1.
Table 1. Sociodemographic characteristics of participants by dry blood spot test result for human immunodeficiency virus (unweighted).
| Variable | Positive test (n=67) |
Negative test (n=767) |
Not tested (n=546) |
Total (n=1,380) |
||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Age (years)a | ||||||||
| 15–19 | 3 | 4.6 | 93 | 12.3 | 61 | 11.7 | 157 | 11.7 |
| 20–29 | 4 | 6.2 | 263 | 34.7 | 159 | 30.5 | 426 | 31.7 |
| 30–39 | 18 | 27.7 | 193 | 25.4 | 127 | 24.4 | 338 | 25.1 |
| 40–49 | 22 | 33.8 | 148 | 19.5 | 116 | 22.3 | 286 | 21.3 |
| 50–59 | 16 | 24.6 | 49 | 6.5 | 43 | 8.3 | 108 | 8.0 |
| 60–64 | 2 | 3.1 | 13 | 1.7 | 15 | 2.9 | 30 | 2.2 |
| City | ||||||||
| Toronto | 38 | 56.7 | 457 | 59.6 | 359 | 65.8 | 854 | 61.9 |
| Ottawa | 29 | 43.3 | 310 | 40.4 | 187 | 34.2 | 526 | 38.1 |
| Language | ||||||||
| English | 51 | 76.1 | 729 | 95.0 | 496 | 90.8 | 1,276 | 92.5 |
| French | 16 | 23.9 | 38 | 5.0 | 50 | 9.2 | 104 | 7.5 |
| Sexa | ||||||||
| Male | 26 | 40.6 | 279 | 36.9 | 186 | 35.5 | 491 | 36.5 |
| Female | 38 | 59.4 | 477 | 63.0 | 338 | 64.5 | 853 | 63.4 |
| Intersex | 0 | 0.0 | 1 | 0.1 | 0 | 0.0 | 1 | 0.1 |
| Gender identitya | ||||||||
| Man | 22 | 34.9 | 276 | 36.5 | 183 | 34.9 | 481 | 35.8 |
| Woman | 39 | 61.9 | 468 | 61.8 | 335 | 63.9 | 842 | 62.6 |
| Trans persons | 0 | 0.0 | 2 | 0.3 | 4 | 0.8 | 6 | 0.4 |
| Non-binary persons | 2 | 3.2 | 11 | 1.5 | 2 | 0.4 | 15 | 1.1 |
| Sexual orientation | ||||||||
| Heterosexual | 44 | 74.6 | 619 | 85.4 | 421 | 87.7 | 1,084 | 85.8 |
| Homosexual | 9 | 15.3 | 26 | 3.6 | 24 | 5.0 | 59 | 4.7 |
| Bisexual | 4 | 6.8 | 56 | 7.7 | 27 | 5.6 | 87 | 6.9 |
| Other | 2 | 3.4 | 24 | 3.3 | 8 | 1.7 | 34 | 2.7 |
| Born in Canadaa | ||||||||
| Yes | 3 | 4.7 | 183 | 24.4 | 112 | 21.5 | 298 | 22.3 |
| Educationa | ||||||||
| University | 4 | 6.6 | 10 | 1.3 | 16 | 3.1 | 30 | 2.3 |
| College | 15 | 24.6 | 174 | 23.1 | 120 | 23.3 | 309 | 23.3 |
| High school | 14 | 23.0 | 136 | 18.1 | 99 | 19.3 | 249 | 18.8 |
| Less than high school | 28 | 45.9 | 432 | 57.4 | 279 | 54.3 | 739 | 55.7 |
| Employment | ||||||||
| Unemployed | 46 | 68.7 | 331 | 43.2 | 264 | 48.4 | 641 | 46.4 |
| Part-time | 12 | 17.9 | 147 | 19.2 | 103 | 18.9 | 262 | 19.0 |
| Full-time | 9 | 13.4 | 289 | 37.7 | 179 | 32.8 | 477 | 34.6 |
| Ability to meet basic needsb | ||||||||
| Not at all difficult | 8 | 12.7 | 201 | 28.4 | 106 | 21.9 | 315 | 25.1 |
| A little difficult | 18 | 28.6 | 221 | 31.2 | 155 | 32.0 | 394 | 31.4 |
| Fairly difficult | 19 | 30.2 | 152 | 21.5 | 122 | 25.2 | 293 | 23.3 |
| Very difficult | 18 | 28.6 | 134 | 18.9 | 102 | 21.0 | 254 | 20.2 |
| Housing situationb | ||||||||
| Not adequate | 15 | 25.4 | 120 | 16.7 | 95 | 19.8 | 230 | 18.3 |
| Barely adequate | 8 | 13.6 | 85 | 11.8 | 63 | 13.1 | 156 | 12.4 |
| Fairly adequate | 21 | 35.6 | 276 | 38.4 | 196 | 40.7 | 493 | 39.2 |
| Very adequate | 15 | 25.4 | 238 | 33.1 | 127 | 26.4 | 380 | 30.2 |
| Ever tested for STIa | ||||||||
| Yes | 43 | 72.9 | 443 | 63.6 | 276 | 62.9 | 762 | 63.8 |
| Self-reported HIV statusa | ||||||||
| HIV+ | 47 | 82.5 | 4 | 0.8 | 24 | 7.0 | 75 | 8.1 |
| HIV- | 10 | 17.5 | 520 | 99.2 | 318 | 93.0 | 848 | 91.9 |
Abbreviations: HIV, human immunodeficiency virus; STI, sexually transmitted infections
a Missing fewer than 5%
b Missing 5%–10%
Prevalence of HIV infection
After weighting the sample according to age, sex and city of residence of the ACB people in Ontario, the prevalence was 7.5% (95% CI 7.1–8.0). The prevalence of HIV in the adult population (15–49 years) was 6.6% (95% CI 6.1–7.1). The prevalence in selected subgroups is shown in Figure 1.
Figure 1.
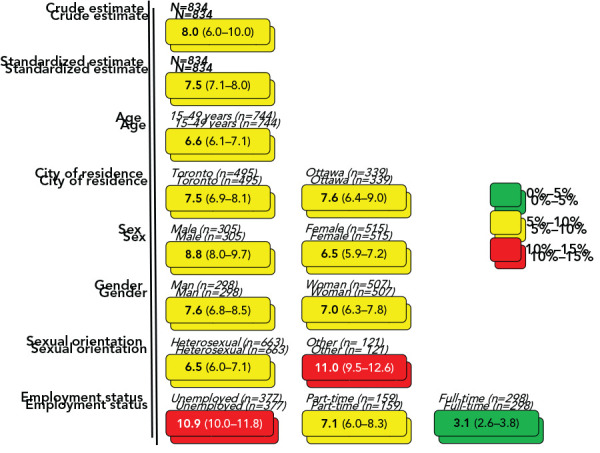
Prevalence of human immunodeficiency virus in subgroups of African, Caribbean and Black people in Toronto and Ottawa, Ontario
Factors associated with HIV infection
In the demographic model, older people (aOR 1.86; 95% CI 1.58–2.18), people with non-binary gender identities (aOR 5.20; 95% CI 1.18–7.28; compared to men), people born outside of Canada (aOR 3.19; 95% CI 1.88–5.40) and people who completed the survey in French (aOR 8.11; 95% CI 2.34–28.14) were more likely to have a positive HIV test. Women (aOR 0.58; 95% CI 0.58–0.59) compared to men, and people with a high school education (aOR 0.15; 95% CI 0.05–0.46), college (aOR 0.08; 95% CI 0.07–0.08) or university (aOR 0.05; 95% CI 0.04–0.07) compared to people with less than high school education were less likely to have a positive test.
In the socioeconomic model, people who were unemployed (aOR 2.38; 95% CI 2.17–2.62) or only part-time employed (aOR 1.35; 95% CI 1.04–1.76) were more likely to have a positive HIV test. People with better housing situations (aOR 0.71; 95% CI 0.69–0.74) and with a higher social capital index score (aOR 0.55; 95% CI 0.51–0.60) were less likely to have a positive test.
In the behavioural model, people who identified as homosexual (aOR 8.63; 95% CI 5.86–12.72) and bisexual (aOR 2.45; 95% CI 1.25–4.8) were more likely to have a positive HIV test than those who identified as heterosexual. People with a higher age at first intercourse (aOR 0.91; 95% CI 0.88–0.95), people who reported substance use during sex (aOR 0.51; 95% CI 0.39–0.66), people who reported more sexual partners (aOR 0.78; 95% 0.74–0.82), and people who had ever had an STI test (aOR 0.51; 95% CI 0.27–0.94) were less likely to have a positive test.
In the full model (including demographic, socioeconomic and behavioural factors), older people (aOR 2.8; 95% CI 2.77–2.82), people born outside of Canada (aOR 4.7; 95% CI 1.5–14.71), people who completed the survey in French (aOR 9.83; 95% CI 5.19–18.61), people who were unemployed (aOR 1.85; 95% CI 1.62–2.11) or part-time employed (aOR 4.64; 95% CI 4.32–4.99), people who reported substance use during sex (aOR 1.66; 95% CI 1.47–1.88) and people who identified as homosexual (aOR 19.68; 95% CI 7.64–50.71) or bisexual (aOR 2.82; 95% CI 1.19–6.65) were more likely to have a positive HIV test. In contrast, people with a high school (aOR 0.01; 95% CI 0.01–0.02), college (aOR 0.00; 95% CI 0.00–0.01) or university education (aOR 0.00; 95% CI 0.00–0.01), compared to people with less than high school education, people who reported a more adequate housing situation (aOR 0.85; 95% CI 0.82–0.88), people with a higher social capital index score (aOR 0.61; 95% CI 0.49–0.74) and people who reported ever having an STI test (aOR 0.40; 95% CI 0.18–0.91) were less likely to have a positive test. The results of the models are shown in Table 2.
Table 2. Summary of generalized linear models for factors associated with a positive human immunodeficiency virus test.
| Partial models | Full model (n=348) AIC 4.105 |
||||||
|---|---|---|---|---|---|---|---|
| Block | Variable | aOR | p-value | aOR | p-value | ||
| n | 95% CI | n | 95% CI | ||||
| Demographic (n=797) AIC 4.787 |
Age | 1.86 | 1.58–2.18 | <0.001 | 2.8 | 2.77–2.82 | <0.001 |
| Gender identity | |||||||
| Man | 1 | 1 | N/A | 1 | 1 | N/A | |
| Woman | 0.58 | 0.58–0.59 | <0.001 | 1.16 | 0.83–1.62 | 0.393 | |
| Other | 5.20 | 1.18–7.28 | <0.001 | Omitteda | N/A | ||
| Level of education | |||||||
| Less than high school | 1 | 1 | N/A | 1 | 1 | N/A | |
| High school | 0.15 | 0.05–0.46 | 0.001 | 0.01 | 0.01–0.02 | <0.001 | |
| College | 0.08 | 0.07–0.08 | <0.001 | 0.00 | 0.00–0.01 | <0.001 | |
| University | 0.05 | 0.04–0.07 | <0.001 | 0.00 | 0.00–0.00 | <0.001 | |
| Place of birth | |||||||
| Canada | 1 | 1 | N/A | 1 | 1 | N/A | |
| Other | 3.19 | 1.88–5.4 | <0.001 | 4.7 | 1.5–14.71 | 0.008 | |
| Language | |||||||
| English | 1 | 1 | N/A | 1 | 1 | N/A | |
| French | 8.11 | 2.34–28.14 | 0.001 | 9.83 | 5.19–18.61 | <0.001 | |
| City | |||||||
| Toronto | 1 | 1 | N/A | Not included in model | |||
| Ottawa | 0.79 | 0.62–1.01 | 0.064 | Not included in model | |||
| Economic (n=731) AIC 6.175 |
Employment | ||||||
| Unemployed | 2.38 | 2.17–2.62 | <0.001 | 1.85 | 1.62–2.11 | <0.001 | |
| Part-time | 1.35 | 1.04–1.76 | 0.024 | 4.64 | 4.32–4.99 | <0.001 | |
| Full-time | 1 | 1 | N/A | 1 | 1 | N/A | |
| Ability to meet basic needs | 0.89 | 0.73–1.08 | 0.223 | Not included in model | |||
| Housing situation | 0.71 | 0.69–0.74 | <0.001 | 0.85 | 0.82–0.88 | <0.001 | |
| Social capital score | 0.55 | 0.51–0.60 | <0.001 | 0.61 | 0.49–0.74 | <0.001 | |
| Behavioural (n=369) AIC 5.435 |
Age at first intercourse | 0.91 | 0.88–0.95 | <0.001 | 0.99 | 0.92–1.07 | 0.797 |
| Substance use during sex | |||||||
| No | 1 | 1 | N/A | 1 | 1 | N/A | |
| Yes | 0.51 | 0.39–0.66 | <0.001 | 1.66 | 1.47–1.88 | <0.001 | |
| Number of sexual partners | 0.78 | 0.74–0.82 | <0.001 | 0.80 | 0.69–0.93 | 0.004 | |
| Transactional sex encounters | 1.17 | 0.47–2.91 | 0.741 | Not included in model | |||
| Sexual orientation | |||||||
| Heterosexual | 1 | 1 | N/A | 1 | 1 | N/A | |
| Homosexual | 8.63 | 5.86–12.72 | <0.001 | 19.68 | 7.64–50.71 | <0.001 | |
| Bisexual | 2.45 | 1.25–4.8 | 0.009 | 2.82 | 1.19–6.65 | 0.018 | |
| Other | 1.02 | 0.03–32.11 | 0.992 | 6.92 | 0.53–89.73 | 0.139 | |
| Ever had an STI test | |||||||
| No | 1 | 1 | N/A | 1 | 1 | N/A | |
| Yes | 0.51 | 0.27–0.94 | 0.032 | 0.40 | 0.18–0.91 | 0.030 | |
Abbreviations: AIC, Akaike information criterion; aOR, adjusted odds ratio; CI, confidence interval; N/A, not applicable; STI, sexually transmitted infections
a Omitted due to insufficient data
Discussion
In this study the overall adult prevalence of HIV infection was 6.6% (95% CI 6.1–7.1) and varied among subgroups; thus confirming the role of sociodemographic, socioeconomic and behavioural factors in HIV vulnerability. These findings were further highlighted in the multivariable analysis in which we identified age, education, place of birth, language, employment, housing, social capital, sexual orientation and STI testing behaviours to be associated with HIV infection.
This work highlights several key issues. First, 82.5% of people with a positive test self reported their positive HIV status; i.e., they were aware of their status. Awareness of HIV-positive status is the first of the UNAIDS 95-95-95 targets for 2030 ( ((19))), and this work confirms concerns that even if countries meet these targets on the national level, vulnerable sub populations may not. African, Caribbean and Black people in Ontario are 12.5% shy of the 2030 target. However, individuals may underreport their HIV-positive status for fear of stigma and discrimination, as shown in other studies ( ((20))).
In addition to factors that have been described in the literature, we found additional factors that may explain ACB people’s vulnerability to HIV or the nefarious consequences of HIV infection. We found that people who reported a lower social capital were more likely to have HIV, suggesting that family and community supports can play a role in enhancing resilience among ACB people. These mechanisms may work by buffering systemic disadvantages that predispose individuals to HIV ( ((21))), but also by promoting preventive behaviours.
African, Caribbean and Black people who were not born in Canada were more likely to have a positive HIV test. It is possible that those who were not born in Canada immigrated from countries with a high underlying prevalence of HIV. Also, we must consider that Black immigrants, irrespective of baseline risk, have other vulnerabilities related to income and employment that increase their risk of HIV, including culture shock, socioeconomic and racial disadvantage of immigrants ( ((22))).
People who completed the survey in French were also more likely to have a positive test. These individuals constitute an ethnic and linguistic minority in Ontario, and as a result may face additional socioeconomic barriers due to their language and migrant status. A scoping review on access to HIV care for Francophones in majority English-speaking provinces highlighted difficulties faced by healthcare professionals in providing care to French-speaking clients ( ((7))).
Increasing age was associated with a higher likelihood of a positive test. This finding is similar to national trends, which show an increasing prevalence in HIV from 15–19 years age group up to the 30–39 years age group, and then a steady decline ( ((23))). In our study, the 50–59 years age group had the highest HIV prevalence. It is possible that the older people have been living with HIV for longer, and have experienced other factors (e.g. advances in understanding about prevention and public health efforts in recent decades) that may increase longevity in people with HIV.
Previous STI testing was associated with lower HIV risk. We postulate that people who have a history of an STI test may have a better appreciation of their risk for STIs including HIV. Moreover, having an STI increases the risk of HIV infection ( ((24))); therefore, testing for and treating STIs would be expected to reduce HIV risk.
Overall, our findings corroborate previous research highlighting the need for information, testing and treatment services for ACB people ( ((25))), and a disconnect between perceived and actual risk for HIV infection ( ((26))). Even though we have discussed these factors separately, they do not exist in a vacuum and likely interact in complex ways to create vulnerability to HIV. While this study was conducted among ACB people, the findings may be true for other racialized or equity-seeking groups of people in Canada and serve to further our understanding of vulnerability to HIV.
Study limitations
This study is not without limitations. First, the planned sample size of 1,500 was not met; however, the sample size of 1,500 was based on an assumed prevalence of HIV of 2%. Given that the prevalence was higher, a smaller sample size would suffice. Second, this is a cross-sectional study, which precludes inferences about causality or the temporal nature of the associations reported here. Third, inaccuracies and non-response to certain questions were inevitable, leading to potential recall bias and social desirability bias. More so, despite weighting, the people who opted to take a DBS test may not be representative of the ACB population, and selection bias may be present. Fourth, the language in which participants chose to complete the questionnaire might not be a true reflection of their primary language of communication.
Study strengths
This study was led by ACB researchers, in line with the principles of autonomy and self-determination in community-led research, and ensured that those participants, recruiters and other community members were treated respectfully in a culturally appropriate manner. Our approach to knowledge translation prioritized the community and has been implemented so far through community presentations and a community report in French and English ( ((27,28))). This is the largest study of ACB people in Canada, with estimates of HIV prevalence by subgroups. Further details on the A/C Study can be accessed online.
Conclusion
African, Caribbean and Black people in Ontario are at a high risk of HIV infection and this risk is linked to sociodemographic, socioeconomic, and behavioural factors. Interventions to improve the social and economic wellbeing of ACB people by removing structural barriers to information, HIV testing, pre and post-exposure prophylaxis and other resources that curb transmission of HIV are needed. An ACB cohort study or linkage to administrative databases would be an ideal way to measure long-term trends in HIV risk, access to health services and health outcomes.
Acknowledgements
We acknowledge the support of the Public Health Agency of Canada’s National HIV and Retrovirology Laboratories for performing the dried blood spot testing; the community members, interviewers, study coordinators, community organizations (Women’s Health in Women’s Hands, Black Creek Community Health Centre, Somerset West Community Health Centre, Canadians of African Descent Health Organization, AIDS committee of Ottawa, African Canadian Association of Ottawa, TAIBU Community Health Centre, Africans in Partnership Against AIDS, African and Black Diaspora Global Network, Black Health Alliance, Bruce House, Regent Park Community Health Centre), partner institutions and participants who contributed their valuable time to this research. Also, we thank the numerous collaborators, colleagues and partners who were involved in earlier stages of this project.
Competing interests
None.
Funding
This work is supported by an award/grant from The Ontario HIV Treatment Network (OHTN).
This study was supported by the Canadian Institutes of Health Research through an Operating Grant in the HIV/AIDS Community Based Research (CBR) Program.
References
- 1.Ontario Advisory Committee on HIB+V/AIDS. Focusing our efforts. HIV/AIDS Strategy to 2026. Toronto, ON: OAN; 2016. https://bit.ly/2lPrA7E
- 2.Ontario HIV Treatment Network. African, Caribbean and Black Communities. Toronto, ON: OHTN; 2018. http://www.ohtn.on.ca/research-portals/priority-populations/african-caribbean-and-black-communities/
- 3.Kerr J, Northington T, Sockdjou T, Maticka-Tyndale E. Perceived Neighborhood Quality and HIV-related Stigma among African Diasporic Youth; Results from the African, Caribbean, and Black Youth (ACBY) Study. J Health Care Poor Underserved 2018;29(2):651–63. 10.1353/hpu.2018.0049 [DOI] [PubMed] [Google Scholar]
- 4.Canadian H. IV/AIDS Black, African and Caribbean Network. CHABAC Awareness Day. CHABAC; 2018. http://www.blackhivday.ca/awareness_day_fact_sheet_2018_EN_final.pdf
- 5.Bourgeois AC, Edmunds M, Awan A, Jonah L, Varsaneux O, Siu W. HIV in Canada-Surveillance Report, 2016. Can Commun Dis Rep 2017. Dec;43(12):248–56. 10.14745/ccdr.v43i12a01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haddad N, Li JS, Totten S, McGuire M. HIV in Canada-Surveillance Report, 2017. Can Commun Dis Rep 2018. Dec;44(12):348–56. 10.14745/ccdr.v44i12a03 [DOI] [PubMed] [Google Scholar]
- 7.Djiadeu P, Yusuf A, Ongolo-Zogo C, Nguemo J, Odhiambo AJ, Mukandoli C, Lightfoot D, Mbuagbaw L, Nelson LE. Barriers in accessing HIV care for Francophone African, Caribbean and Black people living with HIV in Canada: a scoping review. BMJ Open 2020. Aug;10(8):e036885. 10.1136/bmjopen-2020-036885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bekele T, Collins EJ, Maunder RG, Gardner S, Rueda S, Globerman J, Le TL, Hunter J, Benoit A, Rourke SB, Ohtn Cohort Study Team T. Childhood Adversities and Physical and Mental Health Outcomes in Adults Living with HIV: Findings from the Ontario HIV Treatment Network Cohort Study. Aids Res Treat 2018. Mar;2018:2187232. 10.1155/2018/2187232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Statistics Canada. Diversity of the Black population in Canada: An overview. Ottawa, ON: StatCan; 2019. https://www150.statcan.gc.ca/n1/pub/89-657-x/89-657-x2019002-eng.htm
- 10.Public Health Agency of Canada. Accelerating our response: Government of Canada five-year action plan on sexually transmitted and blood-borne infections. Ottawa, ON: PHAC; 2020. https://www.canada.ca/en/public-health/services/reports-publications/accelerating-our-response-five-year-action-plan-sexually-transmitted-blood-borne-infections.html [DOI] [PMC free article] [PubMed]
- 11.Mbuagbaw L, Tharao W, Husbands W, Nelson LE, Aden M, Arnold K, Baidoobonso S, Dabone C, Dryden O, Etowa E, Hamid J, Jackson-Best F, Kohoun B, Lawson DO, Lofters AK, Luyombya H, Mbulaheni T, Mkandawire P, Ndungu M, Nyambi A, Obiorah S, Ongoiba F, Ongolo-Zogo C, Oraka C, Shahin R, Yaya S, Hendricks A, Gebremeskel A, Inoua H, Etowa J. A/C study protocol: a cross-sectional study of HIV epidemiology among African, Caribbean and Black people in Ontario. BMJ Open 2020. Jul;10(7):e036259. 10.1136/bmjopen-2019-036259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007. Oct;370(9596):1453–7. 10.1016/S0140-6736(07)61602-X [DOI] [PubMed] [Google Scholar]
- 13.Statistics Canada. Census Profile, 2016 Census. Ottawa, ON: StatCan; 2018. https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/details/Page.cfm?Lang=E&Geo1=PR&Code1=01&Geo2=&Code2=&Data=Count&SearchText=Canada&SearchType=Begins&SearchPR=01&B1=All&GeoLevel=PR&GeoCode=01
- 14.Statistics Canada. Census Program: Census of Population. Ottawa, ON: StatCan; 2016. https://www12.statcan.gc.ca/census-recensement/index-eng.cfm
- 15.Newcombe RG. Two-sided confidence intervals for the single proportion: comparison of seven methods. Stat Med 1998. Apr;17(8):857–72. [DOI] [PubMed] [Google Scholar]
- 16.Vemuri AW, Grove JM, Wilson MA, Burch WR Jr. A tale of two scales: evaluating the relationship among life satisfaction, social capital, income, and the natural environment at individual and neighborhood levels in metropolitan Baltimore. Environ Behav 2011;43(1):3–25. 10.1177/0013916509338551 [DOI] [Google Scholar]
- 17.Statistics Canada. Data products, 2016 Census. Ottawa, ON: StatCan; 2017; (accessed 2020-12-07). https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/index-eng.cfm
- 18.Statistics Canada. 5.0 Data accuracy and quality. Ottawa, ON: StatCan; 2009. https://www150.statcan.gc.ca/n1/pub/13f0026m/2007001/ch5-eng.htm
- 19.Joint United Nations Programme on HIV/AIDS. Understanding fast-track: accelerating action to end the AIDS epidemic by 2030. Geneva, CH: UNAIDS; 2015. https://www.unaids.org/sites/default/files/media_asset/201506_JC2743_Understanding_FastTrack_en.pdf
- 20.Soni N, Giguère K, Boily MC, Fogel JM, Maheu-Giroux M, Dimitrov D, Eshleman SH, Mitchell KM. Under-Reporting of Known HIV-Positive Status Among People Living with HIV: A Systematic Review and Meta-analysis. AIDS Behav 2021. Dec;25(12):3858–70. 10.1007/s10461-021-03310-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Antabe R, Miller D, Kohoun B, Okonufua O, Husbands W. Black Resilience: A Strategic Asset for Engaging Heterosexual Black Canadian Men in Community Responses to HIV. J Racial Ethn Health Disparities 2022. Jun;9(3):756–66. 10.1007/s40615-021-01011-w [DOI] [PubMed] [Google Scholar]
- 22.Blot S, Godbout C, Liu J, Bullock S, Tharao W, Iveniuk J, Tharao W, Iveniuk JD, Godoy S, Frans D, Allen A, Lee A, Gyamfowa A, Oyelowo O, Yehdego, Arnold MK, Maitland D, Soomarie D, Odhiambo J, Ndungu M, Habanyama M, Chigugudhlo D. MSAFIRI Post-Migration Health Project: Findings and HIV prevention strategy development for Ontario ACB people below the radar. Knowledge Translation and Exchange (KTE) Forum Summary Report. 2018.
- 23.Haddad N, Weeks A, Robert A, Totten S. HIV in Canada—surveillance report, 2019. Can comun Dis Rep 2021;47(1):77–86. 10.14745/ccdr.v47i01a11 10.14745/ccdr.v47i01a11 [DOI] [PMC free article] [PubMed]
- 24.Gray RH, Wawer MJ, Brookmeyer R, Sewankambo NK, Serwadda D, Wabwire-Mangen F, Lutalo T, Li X, vanCott T, Quinn TC; Rakai Project Team . Probability of HIV-1 transmission per coital act in monogamous, heterosexual, HIV-1-discordant couples in Rakai, Uganda. Lancet 2001. Apr;357(9263):1149–53. 10.1016/S0140-6736(00)04331-2 [DOI] [PubMed] [Google Scholar]
- 25.Antabe R, Konkor I, McIntosh M, Lawson E, Husbands W, Wong J, Arku G, Luginaah I. “I went in there, had a bit of an issue with those folks”: everyday challenges of heterosexual African, Caribbean and black (ACB) men in accessing HIV/AIDS services in London, Ontario. BMC Public Health 2021. Feb;21(1):315. 10.1186/s12889-021-10321-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baidoobonso S, Bauer GR, Speechley KN, Lawson E; BLACCH Study Team . HIV risk perception and distribution of HIV risk among African, Caribbean and other Black people in a Canadian city: mixed methods results from the BLACCH study. BMC Public Health 2013. Mar;13:184. 10.1186/1471-2458-13-184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baidoobonso S, Kihembo M, Nare H, Mbuagbaw L, Husbands W, Etowa J, Tharao W, Djiadeu P, Daboné C, Etowa E, Lawson D, Obiorah S, Ndung’u M, Ongoiba F, Inoua H, Odongo JK, Owino M, Nelson L, Gebremeskel A. A/C study community report: HIV among African, Caribbean, and Black people in Ontario. 2020. https://acstudy.ca/wp-content/uploads/2021/02/A_C_report2020.pdf
- 28.Baidoobonso S, Kihembo M, Nare H, Mbuagbaw L, Husbands W, Etowa J, Tharao W, Djiadeu P, Daboné C, Etowa E, Lawson D, Obiorah S, Ndung’u M, Ongoiba F, Inoua H, Odongo JK, Owino M, Nelson L, Gebremeskel A. Rapport Communautaire de l’étude A/C: Le VIH chez les Africains, Caribéennes et Noirs (ACN) en Ontario. 2020. https://acstudy.ca/wp-content/uploads/2021/02/E%CC%81TUDE_AC.pdf


