Abstract
We report flow characteristics of an in-situ internal thoracic artery (LITA) graft with angiographically competitive flow to the left anterior descending artery (LAD), based upon intraoperative transit-time flow measurement (TTFM) during coronary artery bypass grafting with aortic valve replacement (AVR) and during re-AVR seven years later. Although intraoperative TTFM of the graft showed lower mean flow and higher pulsatility index, suggesting inadequate anastomosis, fast Fourier transform (FFT) analysis of TTFM waveforms presented gradual waning of the amplitude, as shown in patent grafts. FFT analysis of the TTFM waveforms is helpful to judge the patency of LITA to LAD, even with competitive flow.
Learning objective
The internal thoracic artery (LITA) graft to left anterior descending artery (LAD) with angiographically competitive flow shows gradual waning of the amplitude on fast Fourier transform (FFT) analysis of the transit-time flow measurement (TTFM) waveforms, although lower mean graft flow, higher pulsatility index, and higher systolic reversal flow may suggest inadequate anastomosis. FFT analysis of the TTFM waveforms is useful to judge the patency of LITA to LAD, even with competitive flow.
Keywords: In-situ internal thoracic artery graft, Competitive flow, Transit-time flow measurement, Fractional flow reserve, Left anterior descending artery
Introduction
Transit-time flow measurement (TTFM) (Medi-Stim, Oslo, Norway) is increasingly used for intraoperative graft flow analysis during coronary artery bypass grafting (CABG) as a less invasive, more highly reproducible, and less time-consuming method [1]. A TTFM probe consists of an ultrasonic transmitter, reflection plate, and ultrasonic receiving device. Based on the theory of ultrasonic velocity measurement, it calculates the graft flow by measuring the time between the ultrasonic transmitting device and the ultrasonic receiving device. Previous studies have proposed the clear-cut values of TTFM to predict graft failure, using mean graft flow (Qm) < 15 ml/min, pulsatility index (PI) > 5.0, systolic reversal flow (SRF) > 4 %, and fast Fourier transform (FFT) ratio, the ratio of the first 2 harmonics > 1.0 [1].
Grafting of the in-situ internal thoracic artery (LITA) to the left anterior descending artery (LAD) can be compromised by competitive flow when the stenosis of LAD is less severe, leading to a string phenomenon [2]. We report flow characteristics on TTFM of a LITA graft to LAD with angiographically competitive flow based upon two findings of TTFM during the first CABG and during the redo cardiac surgery with 7-year interval. We obtained oral informed consent from the patient for publication of this case report. Institutional review board approval for this report was not required by our institution.
Case report
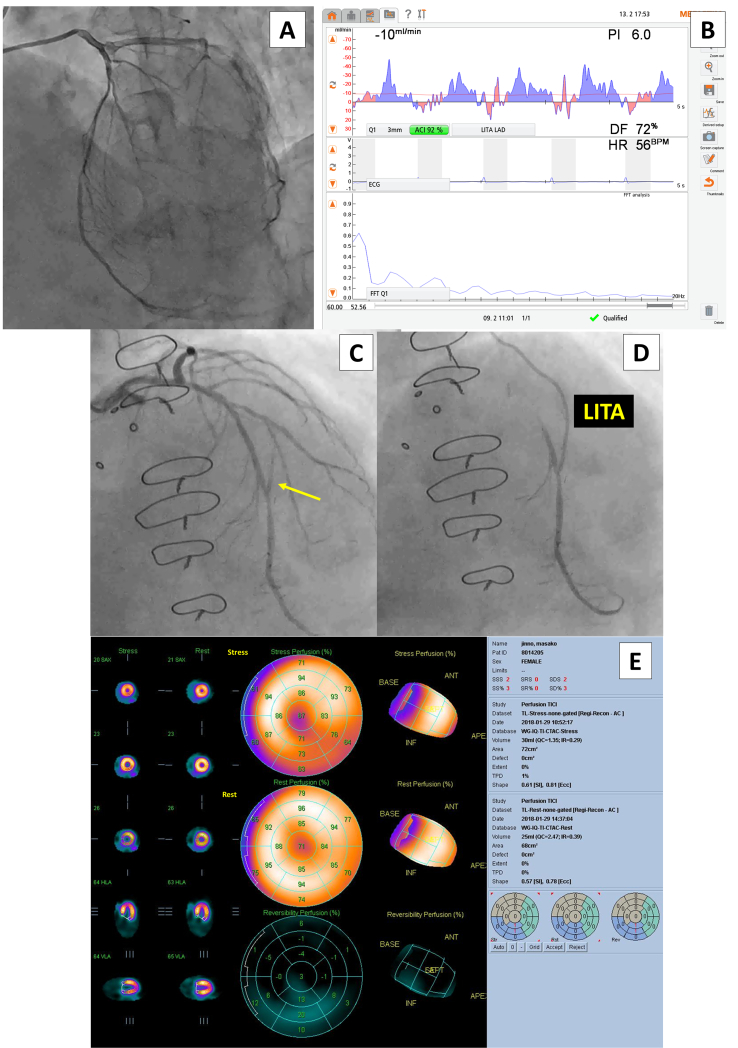
In 2016, a 71-year-old female patient with hypertension, dyslipidemia, and diabetes mellitus presented syncope and was diagnosed with aortic valve stenosis and 3-vessel coronary disease on coronary angiography, including LAD with a fractional flow reserve (FFR) of 0.74 (Fig. 1A). She underwent aortic valve replacement (AVR) with a 19-mm bioprothesis (Mosaic Ultra; Medtronic, Minneapolis, MN, USA) and triple CABG: in-situ LITA graft to LAD, sequential saphenous vein graft (SVG) to left circumflex artery and right coronary artery. Intraoperative TTFM of the LITA showed Qm of 10 ml/min, PI of 6.0, and SRF of 14 %. FFT analysis of the TTFM waveforms showed gradual waning of the amplitude with a FFT ratio of 2.5 (Fig. 1B). Postoperative angiography two months after surgery showed patent SVG and LITA graft with competitive flow of the LAD but without a string sign (Fig. 1C and D). Postoperative stress myocardial perfusion scintigraphy using thallium-201 also showed no ischemia of the LAD area (Fig. 1E).
Fig. 1.
(A) Preoperative coronary angiography of the left anterior descending artery (LAD) with a fractional flow reserve of 0.74. (B) Results of transit-time flow measurement of in-situ internal thoracic artery (LITA) graft to the LAD during the first cardiac surgery. The fast Fourier transform (FFT) analysis waveform shows a gradually attenuating waveform with a FFT ratio of 2.5. (C) Postoperative coronary angiography of the LAD, showing reversal blood flow from the native LAD to the LITA graft (yellow arrow). (D) Postoperative angiography of the LITA graft. (E) Postoperative stress myocardial scintigraphy, showing no ischemia.
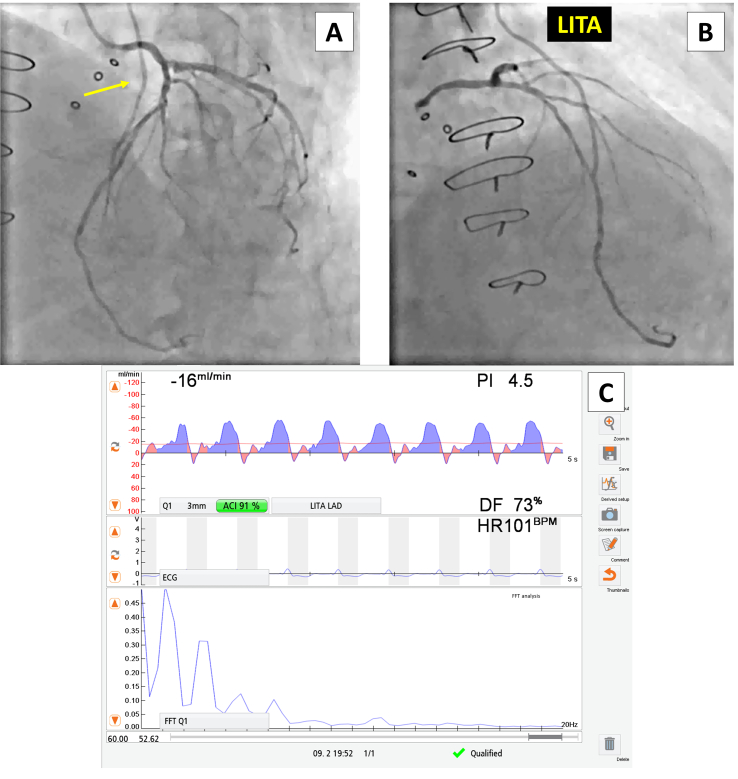
At the age of 78 years in 2022, she developed exertional dyspnea and syncope again. Echocardiography revealed aortic bioprosthetic stenosis with max velocity of 3.9 m/s, mean pressure gradient of 31 mmHg, and estimated valve area of 0.6 cm2. A coronary angiography redone for re-AVR showed patent SVG and LITA graft with more competitive flow of the LAD but without a string sign (Fig. 2A and B). During re-AVR with a 17-mm mechanical valve (SJM Regent; St Jude Medical, St Paul, MN, USA), intraoperative TTFM of the LITA showed Qm of 16 ml/min, PI of 4.5, and SRF of 8 %. FFT analysis of the TTFM waveforms showed gradual waning of the amplitude with a FFT ratio of 1.7 (Fig. 2C).
Fig. 2.
(A) Coronary angiography of the left anterior descending artery (LAD) before the second cardiac surgery, showing reversal blood flow from the native LAD to the internal thoracic artery (LITA) graft (yellow arrow). (B) Angiography of the LITA graft before the second surgery. (C) Results of transit-time flow measurement of the LITA graft to the LAD during the second surgery. The fast Fourier transform (FFT) analysis shows a gradually attenuating waveform with a FFT ratio of 1.7.
Discussion
In this report, the patent LITA graft to LAD with angiographically competitive flow showed gradual waning of the amplitude on FFT analysis of the TTFM waveforms, despite lower Qm, higher PI, higher SFR, suggesting inadequate anastomosis, in a patient undergoing redo cardiac surgery. It may suggest that FFT analysis of the TTFM waveforms is useful to judge the patency of LITA to LAD, even with competitive flow.
The main indicators of intraoperative TTFM to assess anastomosis quality of the LITA graft to LAD, Qm, PI, and SRF, are strongly affected by preoperative FFR value of the LAD, which reflects the physiologic degree of stenosis or myocardial ischemia [3]. In particular, PI should be noted, because the formula for it is (maximal flow-minimal flow)/Qm. High sharp waves and negative blood flow can increase the difference between the maximum and minimum blood flow. These features are more alarming to surgeons than Qm, as Quin et al. reported that the re-anastomosis rate increased with an increase in PI [4]. Therefore, the combination of TTFM indicators and FFT improve the accuracy to evaluate graft quality in clinical settings.
FFT analysis is based upon the principal that all periodic waveforms can be broken down into a series of pure sine waves or harmonics. Harmonics exist at frequencies that are multiples of the frequency of the original waveform (“the fundamental frequency”) and are described in terms of an amplitude and phase [[5], [6], [7], [8]]. The greatest value of FFT is that it quantifies TTFM waveforms by transforming the waveforms into the frequency domain. The harmonics reflected the complexity of the TTFM waveform. For example, the sine wave has only 1 harmonic, and the more harmonics, the more complex the wave. The frequency of harmonics also reflected waveform complexity.
Mao et al. demonstrated that the FFT analysis can be applied to evaluate CABG graft flow using multi-scale models of a 3D LITA-LAD graft of different stenosis in LAD to get different magnitude of competitive flows [5,6]. Their in vitro results showed that the FFT ratio > 1.0 is preserved for the patent LITA-LAD graft with any degree of stenosis, as demonstrated in this report. When the TTFM indices are not good, such as Qm < 15 ml/min, PI > 5.0, or SFR > 4 %, FFT analysis should be recommended. When the FFT ratio is 1.0 or higher, the graft anastomosis is adequate and the surgical indication for revascularization of the LAD is not adequate. When the FFT ratio is <1.0, there may be a problem with the anastomosis, and therefore, graft revision should be considered [3]. Alternatively, Jia et al. reported that main wave (H0), the amplitude of the first harmonic (H1), and the frequency of the first harmonic are predictive parameters for graft failure, although they concluded that FFT of TTFM waveforms can be used to evaluate graft quality [8].
In conclusion, the patent LITA graft to LAD with angiographically competitive flow showed gradual waning of the amplitude with the FFT ratio > 1.0 on FFT analysis of the TTFM waveforms, despite lower Qm, higher PI, higher SFR. FFT analysis of the TTFM waveforms is useful to judge the patency of LITA to LAD, even with competitive flow.
The following are the supplementary data related to this article.
Clinical course of the patient, including coronary angiography, stress myocardial scintigraphy, and intraoperative transit-time flow measurement of the in-situ internal thoracic artery graft to the left anterior descending artery.
Patient permission/consent statement
We obtained oral informed consent from the patient for publication of this case report. Institutional review board approval for this report was not required by our institution.
Funding
None.
Declaration of competing interest
The authors have no conflicts of interest to declare.
Acknowledgements
None.
References
- 1.Takami Y., Takagi Y. Roles of transit-time flow measurement for coronary artery bypass surgery. Thorac Cardiovasc Surg. 2018;66:426–433. doi: 10.1055/s-0037-1618575. [DOI] [PubMed] [Google Scholar]
- 2.Villareal R.P., Mathur V.S. The string phenomenon: an important cause of internal mammary artery graft failure. Tex Heart Inst J. 2000;27:346–349. [PMC free article] [PubMed] [Google Scholar]
- 3.Noda M., Takami Y., Amano K., Sakurai Y., Akita K., Maekawa A., et al. Relation of fractional flow reserve with transit time coronary artery bypass graft flow measurement. Ann Thorac Surg. 2021;111:134–140. doi: 10.1016/j.athoracsur.2020.04.100. [DOI] [PubMed] [Google Scholar]
- 4.Quin J., Lucke J., Hattler B., Gupta S., Baltz J., Bishawi M., et al. Surgeon judgment and utility of transit time flow probes in coronary artery bypass grafting surgery. JAMA Surg. 2014;149:1182–1187. doi: 10.1001/jamasurg.2014.1891. [DOI] [PubMed] [Google Scholar]
- 5.Takami Y., Ina H. Relation of intra-operative flow measurement with post-operative quantitative angiographic assessment of coronary artery bypass grafting. Ann Thorac Surg. 2001;72:1270–1274. doi: 10.1016/s0003-4975(01)02933-2. [DOI] [PubMed] [Google Scholar]
- 6.Mao B., Wang W., Zhao Z., Zhao X., Li L., Zhang H., et al. On the relationship between competitive flow and FFT analysis of the flow waves in the left internal mammary artery graft in the process of CABG. Biomed Eng Online. 2016;15(Suppl. 2):129. doi: 10.1186/s12938-016-0260-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mao B., Feng Y., Duan M., Dong Y., Li G., Li B., et al. A novel method to determine the cause of left internal mammary artery instant non-patency based on transit time flow measurement. Front Physiol. 2022;13:901280. doi: 10.3389/fphys.2022.901280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jia Y., Xu H., Su P., Gao J., Gu S., Liu Y., et al. Predictive value of graft patency and major adverse cardiac and cerebrovascular events (MACCEs) in coronary artery bypass grafting (CABG) based on Fourier transform (FFT) J Thorac Dis. 2021;13:2705–2715. doi: 10.21037/jtd-21-178. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Clinical course of the patient, including coronary angiography, stress myocardial scintigraphy, and intraoperative transit-time flow measurement of the in-situ internal thoracic artery graft to the left anterior descending artery.