Abstract
Background
Remote patient monitoring (RPM), or telemonitoring, offers ways for health care practitioners to gather real-time information on the physiological conditions of patients. As telemedicine, and thus telemonitoring, is becoming increasingly relevant in today’s society, understanding the practitioners’ opinions is crucial. This systematic review evaluates the perspectives and experiences of health care practitioners with telemonitoring technologies.
Methods
A database search was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines for the selection of articles measuring health care practitioners’ perspectives and experiences with RPM technologies published between 2017 and 2021. Only articles written in English were included. No statistical analysis was performed and thus this is a qualitative review.
Results
A total of 1605 studies were identified after the initial search. After applying the inclusion and exclusion criteria of this review’s authors, 13 articles were included in this review. In all, 2351 practitioners’ perspectives and experience utilizing RPM technology in a variety of medical specialties were evaluated through close- and open-ended surveys. Recurring themes emerged for both the benefits and challenges. Common benefits included continuous monitoring of patients to provide prompt care, improvement of patient self-care, efficient communication, increased patient confidence, visualization of health trends, and greater patient education. Challenges comprised increased workload, higher patient anxiety, data inaccuracy, disorienting technology, financial issues, and privacy concerns.
Conclusion
Health care practitioners generally believe that RPM is feasible for application. Additionally, there is a consensus that telemonitoring strategies will become increasingly relevant. However, there are still drawbacks to the technology that need to be considered.
Introduction
Telemedicine was initially developed to care for astronauts during space missions and is now being applied to everyday patient care. 1 The application of telemedicine grew exponentially due to the COVID-19 pandemic, and this model of care will likely be integrated into the regular delivery of health care within the next years. 2 The importance of telemedicine for patients with nonurgent medical needs during these times has been emphasized. 3
Remote patient monitoring (RPM), or telemonitoring, is a strategy of telemedicine that offers a way for clinicians to observe patients’ physiological parameters remotely and to intervene if abnormalities appear (Figure 1). Telemonitoring is promising for use with patients diagnosed with chronic diseases, 4 and it can additionally be applied to temporary conditions, such as pregnancy. This technology offers cost-saving care to patients as they remain at home instead of staying in costly and limited-space nursing homes or hospitals. 5
Figure 1:
RPM allows health care practitioners to remotely observe the patient’s physiological parameters and intervene if abnormalities appear. RPM = remote patient monitoring. Created with BioRender.com.
One type of the most common technologies used are wearable devices, both consumer and medical grade, that monitor and record information on physiological conditions and activities. 6 More-invasive technologies include devices, such as pacemakers and implantable cardioverter-defibrillators, that are paired with a platform, such as a smartphone app, to gather patient data. 7
Regardless of the technology utilized, telemonitoring gathers real-time data from patients to allow health care practitioners to remotely evaluate their patients’ health status. Because this strategy is becoming increasingly relevant to patient care, the noted benefits and drawbacks of telemonitoring need to be evaluated to continue its improvement. Therefore, this systematic review aimed to find health care practitioners’ perceptions and experiences with RPM.
Methods
The search was performed in August 2021 and employed 4 electronic databases, including PubMed, Cumulative Index of Nursing and Allied Health Literature, Web of Science, and Google Scholar. The terms “healthcare provider experience,” “remote monitoring,” “remote patient monitoring,” and “medical technology” were used in combination in all the databases. The terms were arranged as follows: “healthcare provider experience AND remote monitoring OR remote patient monitoring AND medical technology.”
Studies were included if they 1) measured the health care practitioner experience or perspectives with 2) remote monitoring technology, 3) the technology was used at home, and 4) were in English. The search spanned the years 2017–2021. No particular specialty was chosen. Exclusion criteria included studies that solely focused on the patient’s experience with the technology and the use of this technology in clinical or hospital settings. The Preferred Reporting Items for Systematic Reviews and Meta-Analysis 8 was referenced for a description of the selection process (Figure 2).
Figure 2:
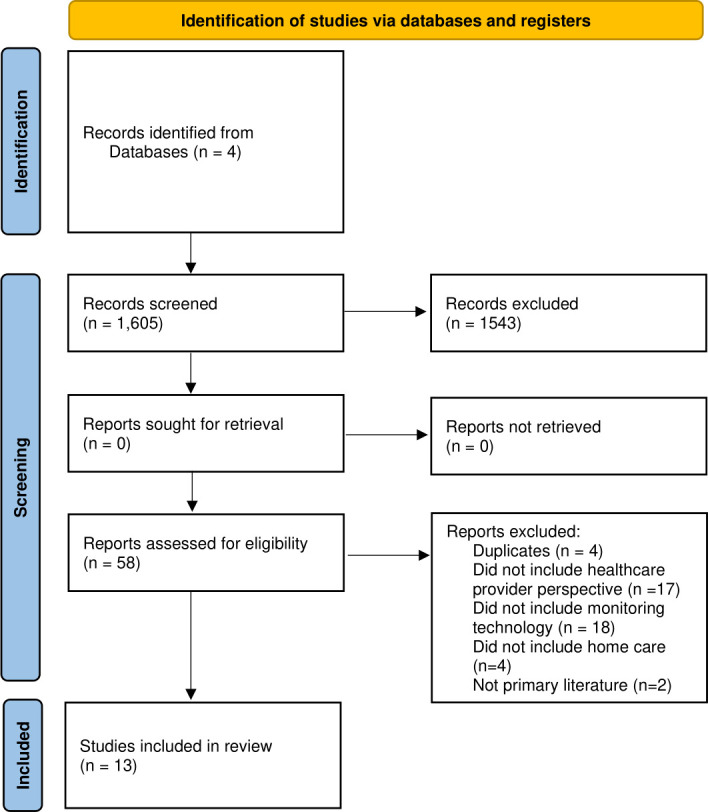
Preferred Reporting Items for Systematic Reviews and Meta-Analyses Flow Diagram. Included and excluded studies. Flowchart created using PRISMA design from Page MJ, McKenzie JE, Bossuyt PM et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi:10.1136/bmj.n71. 36 Creative Commons Attribution (CC BY 4.0) license (https://creativecommons.org/licenses/by/4.0/legalcode).
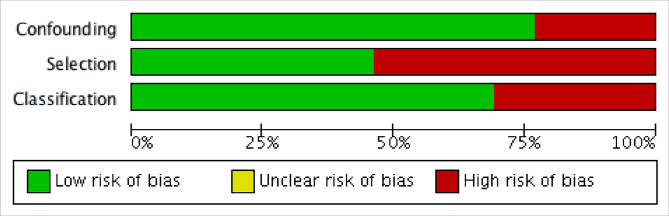
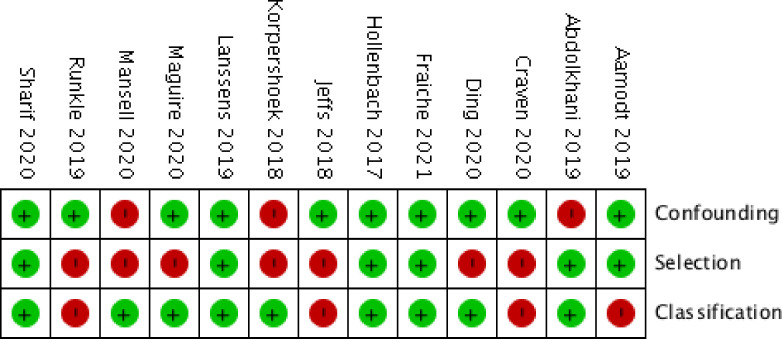
Risk of bias
The Cochrane Library Risk Of Bias In Non-randomized Studies of Interventions tool was used to assess the risk of bias. 9 Descriptions of individualized bias and cross-sectional studies bias are shown in Figures 3 and 4, respectively.
Figure 3:
Individualized risk of bias. The green color represents low risk of bias, and the red color represents a high risk.
Figure 4:
Summary of risk of bias all included studies. (+) indicates absence, and (-) indicates the presence of bias.
Results
The initial search resulted in 1605 studies. After an initial title screening and duplicate removal, 54 titles underwent abstract and full-text screening. This selection resulted in 13 articles eligible for inclusion in the review (Table 1). The studies gathered data through the employment of different types of surveys which are summarized in Table 2. All the studies inquired about the health care practitioners’ benefits and challenges of RPM.
Table 1:
Summary of articles included in this systematic review
| Author, date | Focus | Technology | Health care practitioners’ demographics | Monitors | |||||
|---|---|---|---|---|---|---|---|---|---|
| Type | Gender | Age | |||||||
| Cardiovascular System | |||||||||
| Aamodt et al, 2019 10 | Heart failure | Internet-based personal devices | Nor | Lith | Nor | Lith | Nor | Lith | Body weight, blood pressure, heart rate, dyspnea, and other vitals |
| P = 63 N = 163 |
P = 137 N = 173 |
M = 58 F = 167 |
M = 32 F = 278 |
P = 48 (SD 11) N = 45 (SD 11) |
P = 51 (SD 12) N = 46 (SD 9) |
||||
| Abdolkhani et al, 2019 11 | Cardiac arrhythmia | Medical wearables | HCPs = 9 HI = 4 RPMS = 7 |
NR | NR | Cardiac rhythm | |||
| Ding et al, 2020 12 | Atrial fibrillation | FDA-approved consumer digital health devices | P = 1104 APP = 186 Nurse = 122 |
NR | NR | Electrocardiographic data | |||
| Fraiche et al, 2021 7 | Cardiology | Pacemakers, implantable cardioverter-defibrillators | P = 8 N = 3 DT = 2 |
NR | 61 (range 27−84 years) | Cardiac rhythm | |||
| Respiratory System | |||||||||
| Hollenbach et al, 2017 13 | Asthma | Inhaler sensor, mobile health application, FDA-approved spirometer | P = 17 PA = 7 APRN = 6 RN, BSN, LPN = 7 Unknown = 4 |
M = 9 F = 32 |
49 (±13.7) years) | Medication use, lung function | |||
| Korpershoek et al, 2018 14 | Chronic obstructive pulmonary disease | mHealth through smartphone or tablet | P = 2 N = 3 PT = 1 |
M = 4 F = 2 |
20–59 years | Self-management of exacerbations | |||
| Maguire et al, 2020 15 | Malignant pleural mesothelioma | Advanced Symptom Management System through a smartphone | P = 2 N = 9 |
NR | NR | Symptoms | |||
| Mansell et al, 2020 16 | Chronic hypercapnic respiratory failure | NIV with modem technology | HCPs = 12 | M = 7 F = 5 |
25−34 (n = 4) or 35−44 (n = 6) | Tidal volume, leak, respiratory rate, minute ventilation, patient-triggered breaths, achieved pressure, patient compliance | |||
| Prenatal Care | |||||||||
| Lanssens et al, 2019 17 | Pregnancy | Blood pressure monitor, activity tracker, weight scale | P = 13 MW = 52 |
NR | NR | Blood pressure, activity, weight | |||
| Runkle et al, 2019 18 | Pregnancy | Smartphone applications, wearables | P = 28 | M = 21 F = 7 |
21–30 (n = 10) 31–40 (n = 11) 41–50 (n = 7) |
Blood glucose, blood pressure, chronic conditions | |||
| Other Medical Fields | |||||||||
| Abdolkhani et al, 2019 11 | Diabetes, sleep disorders | Consumer (diabetes) and medical (sleep disorder) wearables | HCPs = 9 HI = 4 RPMS = 7 |
NR | NR | Blood glucose, insulin pumps, sleep disorder data | |||
| Craven et al, 2020 19 | Epilepsy, multiple sclerosis, depression | Wearables and mobile phone applications | HSR = 3 HTR = 2 C = 16 PAB = 7 |
NR | NR | Activity, location, user-supplied data from questionnaires | |||
| Jeffs et al, 2018 20 | Chronic kidney disease | eQConnect software | P = 1 N = 2 PC = 3 CC = 1 PD = 1 |
M = 3 F = 5 |
NR | Peritoneal dialysis treatment progress, health status, supply usage | |||
| Sharif et al, 2020 21 | Orthopedics | RPM as part of Virtual Health Technology | HCPs = 16 | NR | NR | Blood pressure, blood glucose, weight, physical fitness, heart rate, heart rhythm, respiratory rate | |||
APP, advance practice practitioner; APRN, advance practice registered nurse; BSN, bachelor of science in nursing; C, clinician; CC, clinical coordinator; DT, Device Technicians; F, female; FDA, US Food and Drug Administration; HCPs, health care practitioners; HI, health information; HSR, health service researcher; HTR, health technology researcher; Lith, Lithuania; LPN, licensed practical nurse; M, male; MW, midwife; N, nurse; NIV, noninvasive ventilation; Nor, Norway; NR, not reported; P, physician; PA, physician assistant; PAB, patient advisory board; PC, project coordinator; PD, product development; PT, physiotherapist; RN, registered nurse; RPM, remote patient monitoring; RPMS, patient remote monitoring solution; SD, standard deviation.
Table 2:
Summary of the surveys employed in each study
| Study | Survey | Participants | Location |
|---|---|---|---|
| Aamodt et al 10 | Close- and open-ended questionnaires | 536 | Norway, Lithuania |
| Abdolkhani et al 11 | In-depth interviews | 9 | Australia |
| Craven et al 19 | Open-ended questionnaire | 28 | Europe |
| Ding et al 12 | Close-ended questionnaire | 1601 | 77 countries |
| Fraiche et al 7 | Semi-structured interviews | 13 | United States |
| Hollenbach et al 13 | Focus groups | 41 | United States |
| Jeffs et al 20 | Semi-structured interviews | 6 | Canada |
| Korpershoek et al 14 | Focus groups | 6 | Netherlands |
| Lanssens et al 17 | Close-ended questionnaire | 44 | Belgium |
| Maguire et al 15 | Semi-structured interviews | 11 | England, Scotland |
| Mansell et al 16 | Focus groups | 12 | United Kingdom |
| Runkle et al 18 | Close- and open-ended questionnaire | 28 | United States |
| Sharif et al 21 | Semi-structured interviews | 16 | United Kingdom |
Cardiovascular system
Aamodt et al 10 conducted a nationwide cross-sectional survey in Norway and Lithuania to evaluate the perspectives of both nurses and physicians that were nonusers of noninvasive telemonitoring technologies. They found that approximately half of the health care practitioners (58.0% in Norway and 55.5% in Lithuania) perceived telemonitoring to be beneficial for follow-up of heart failure patients. On the other hand, a few concerns were raised when health care practitioners with experience working with medical wearables on patients with cardiac arrhythmia and patients were asked about the management and quality of telemonitoring patient-generated data. These included digital health literacy, the accuracy of wearable devices, and the complexity of data analysis. Additionally, it was highlighted that the lack of integration with existing electronic medical record systems posed a problem. Consequently, the authors suggested that the accuracy of data collected by wearables can be improved by creating quality guidelines with all stakeholders, including patients, health care practitioners, and manufacturers. 11
A large study done by Ding et al 12 that assessed 1601 health care practitioners with a range of experience using US Food and Drug Administration (FDA)-approved consumer digital health devices to measure cardiac rhythm found that 62.3% would recommend the use of the device for atrial fibrillation detection. Consistent with this method, Fraiche et al 7 interviewed 13 physicians, nurses, nurse practitioners, and device clinic technicians with varying levels of experience with pacemakers and implantable cardioverter-defibrillators that gather cardiac rhythm data from patients. Interviewees in general had high levels of trust in the telemonitoring practice.
Respiratory system
In 2017, 41 health workers, including pulmonologists, pediatricians, physician assistants, nurse practitioners, nurses, and medical assistants participated in a group interview to discuss the relevancy of utilizing inhaler sensors, mobile health applications, and an FDA-approved spirometer to monitor lung function and medication compliance in patients with asthma. This study done by Hollenbach et al 13 reported that health care practitioners viewed the implementation of this technology favorably.
Korpershoek et al 14 —through a focus group with 3 nurses, a pulmonology resident, a general practitioner, and a respiratory physiotherapist discussing the use of an mHealth platform to support self-management of exacerbations of chronic obstructive pulmonary disease in patients—found that the practitioners considered the platform valuable.
Moreover, Maguire et al 15 implemented a new system, the Advanced Symptom Management System, to monitor malignant pleural mesothelioma. The study interviewed 2 respiratory consultants and 9 nurses on their experience. Clinicians mostly believed the system was attainable and acceptable, with topics such as early symptom management and the connection between patients and clinicians being featured. Additionally, patients reported experiencing the feeling of being listened to and receiving timely assurance about their symptoms. These results show a need for further trials of remote symptom monitoring to support patients with malignant pleural mesothelioma at home.
Mansell et al 16 recruited 12 health care practitioners to participate in being interviewed on the use of noninvasive ventilation (NIV) with a modem technology to monitor tidal volume, leak, respiratory rate, minute ventilation, patient-triggered breaths, achieved pressure, and compliance of patients diagnosed with chronic hypercapnic respiratory failure. The study found that modern technology was generally considered a feasible addition in managing home NIV that increases the patient’s access to care.
Prenatal care
Lanssens et al 17 surveyed 35 midwives and 9 obstetricians who participated in a yearlong study called the Pregnancy REmote MOnitoring study, 22 where they gained experience using a blood pressure monitor, activity tracker, and weight scale that gathered data during prenatal care. Seventy-seven percent of the midwives and 67% of the obstetricians felt that remote monitoring benefited their patients, especially the patients at high risk.
On the other hand, Runkle et al 18 administered an electronic survey to 28 family medicine and OB/GYN practitioners regarding their perceptions of using applications and wearables. Only approximately half of the practitioners believed this technology will be further implemented in the future and could be useful for their patients.
Other medical fields
Abdolkhani et al 11 conducted an interview with 9 health care practitioners to gain insight into their experiences with consumer and medical wearables for monitoring patients with diabetes and sleep disorders. The study focused on 2 topics related to personalized health care data management and quality. The authors reported that the lack of support and advice for patients and the lack of guidelines in health care settings may have caused unreliable data collection. For instance, an endocrinologist noted the limited staff available to advise. Furthermore, the way data is presented via wearable components, such as a receiver or a mobile app, may influence the patient’s understanding of their data and, consequently, their self-care decisions.
Jeffs et al 20 found that health care practitioners believe that the eQConnect software, 23 which monitors peritoneal dialysis treatment and health status in patients with chronic kidney disease, can increase efficiency and safety for their patients, although with certain drawbacks. Through an open-ended survey, Craven et al 19 gathered information on the potential of remote monitoring in patients with epilepsy, multiple sclerosis, and depression. The survey results present a promising application of a technology system, the Remote Assessment of Disease and Relapse–Central Nervous System. Additionally, benefits and challenges were determined in an interview conducted by Sharif et al 21 on the general perception of RPM as part of the larger virtual health technology platform.
Discussion
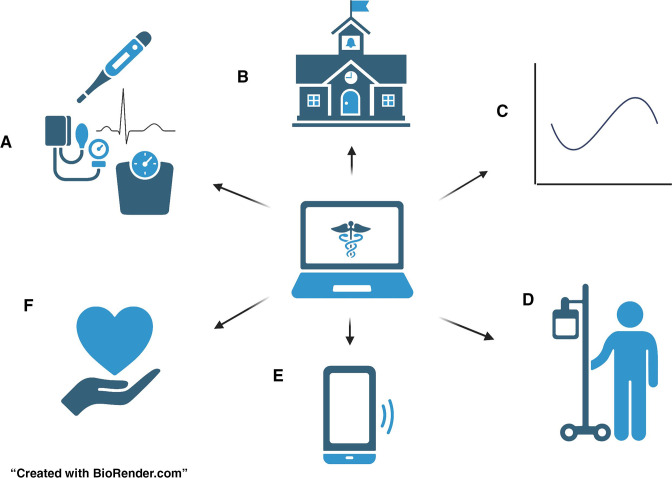
Although the studies gathered for this review covered several specialties and diverse technologies, recurrent themes emerged during discussions of both the benefits and the challenges of telemonitoring. The results show that a majority of the health care practitioners do believe that application of remote monitoring tools will become increasingly relevant in the future and is advantageous for their practice. Figure 5 shows a summary of the major themes regarding the perceived benefits of telemonitoring.
Figure 5:
Benefits of RPM as perceived by health care practitioners. A) the continuos monitoring of vital signs allows for a more realistic view of the patient and early detection of deterioration. B) Improved patient education due to the patient's ability to view their health status that can establish perceived control of the disease. C) The storage of patient data supports visualization of long-term health trends and helps determine ideal treatment plans. D) Monitoring can increase patient confidence. E) Prompt and efficient communication due to alerts. F) Telemonitoring can assist patients that are expected to self-manage. RPM = remote patient monitoring.
Health care practitioners considered telemonitoring applications to be valuable due to their ability to monitor patients’ conditions continuously between clinic visits. 10,18,20 This continuous monitoring allows clinicians to identify deterioration earlier and provide prompt care. 10,11,14,15,18,20 Prompt care of patients, especially the ones with chronic conditions, allows for better outcomes and habit changes for more preventative care. Additionally, remote monitoring can decrease unnecessary clinic visits if the patient is recovering well 16,19 or, if visits do occur, the health care practitioners will be more efficient due to the supplied data. 16 For example, in a patient with a common diagnosis, such as chronic heart failure, who is monitored remotely through telemonitoring applications, clinicians are able to observe any changes in their condition throughout the week. If the patient’s condition starts to deteriorate, the clinicians are able to identify it earlier and provide prompt care. By providing prompt care, the patient is able to make necessary lifestyle changes to prevent further health complications. Additionally, the patient can avoid unnecessary clinic visits if the data from the telemonitoring application shows that their condition is improving.
With RPM technology, health care practitioners were able to view valuable symptom or patient condition information that patients did not necessarily report during in-person clinic visits. 15,19 Furthermore, telemonitoring allowed for a more realistic view of certain vitals, such as blood pressure, that might be elevated only during a clinic or hospital visit due to “white coat syndrome.” 21 This more realistic view of the patient’s health status results in more relevant treatment to further benefit the patient.
Maguire et al 15 reported that health care practitioners could determine which treatments better alleviated symptoms or access information on patient compliance to prescribed treatments. 13,16 Along with that, these technologies have the ability to store long-term data that provide an overview of patient’s health status 11 and determine health trends. 13,20 Together, those aspects of the technology create a more personalized care for the patient, which, as the health care practitioners noted, is what is the most helpful for the specific patient.
Additionally, patients who have access to that data can become more educated on their disease, 10,14,19,21 leading to a perceived control of the disease. 14 Other RPM studies support these findings, stating that patients able to access their data engage better in their health management. 24
Moreover, self-care is crucial to maintaining a higher quality of life, especially for patients with chronic diseases. 25 Health care practitioners found that these technologies can greatly benefit patients who are expected to self-manage at home by increasing their awareness and thus their confidence. 10,14,15,20,21 Patient studies echo the practitioner perceptions, showing that telemedicine does establish confidence in patients 26–29 and reduce emergency or unnecessary in-person visits. 30 Jeffs et al 20 noted that health care practitioners were able to see the supply usage data of patients with chronic kidney disease and address deficiencies in their self-management, further improving the patient’s ability to self-manage.
Of importance, these technologies empower patients to contact their health care practitioners, thus decreasing patient insecurity 14 and improving overall patient communication. 18 Additionally, these technologies can also provide alerts prompting patients to contact the clinic if there are any abnormalities with their health status. 20 The technologies also alert health changes on the practitioner end to create an appointment or prompt a phone call from a clinician. 19
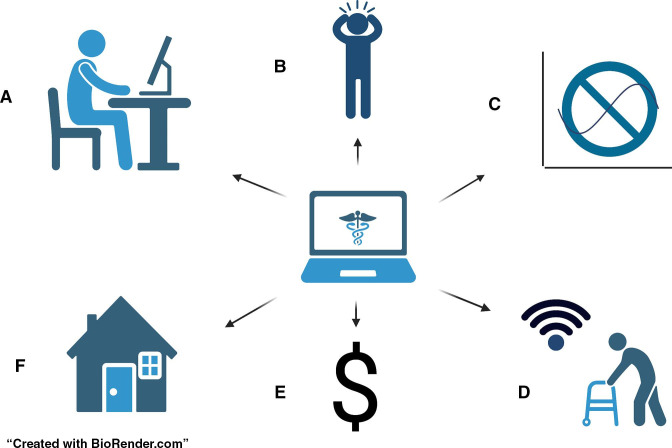
Although there were many positive perceptions and experiences of RPM technologies, health care practitioners also mentioned challenges in this practice. Figure 6 demonstrates the health care practitioners’ major problems with the technology. One of the main challenges seen in several included studies was the concern that RPM would lead to an increase in the practitioner’s workload, 12–16,18,19 although some health care practitioners did believe it would decrease their workload in the outpatient setting. 10 The health care practitioners in the study by Lanssens et al 17 found no actual increase in their workload when utilizing the technology.
Figure 6:
Challenges of RPM as perceived by health care practitioners. A) Increased workload due to the large amount of patient data. B) Constant disease reminders that can increase patient anxiety. C) Data inaccuracy and limited trust of technology. D) A majority of the patients are elderly, and technology can ocassionally be disorienting. E) No consensus on finantial responsabilities. F) Privacy and security concerns. RPM = remote patient monitoring.
The main concern for the health care practitioners who believe these new technologies will increase their work is the large amount of data gathered that leads to the laborious requirement of determining which information is valuable and which is extraneous. 11,13,16,18,19 Along with the sheer amount of data, Abdolkhani et al 11 noted that the acquired data is not always integrated into the patient’s electronic medical record. This becomes increasingly complicated with the diversity in manufacturers, making it difficult to normalize the data.
Studies have been done to increase the interoperability of the technology, including one by Gay et al, 31 where they created a mobile application to store all health data in a singular platform. However, connecting the information to the patient’s actual electronic medical record remains complicated, with systems not allowing access to third-party developers to protect legal patient data. 32
Access to legal patient data is included in the privacy concern theme mentioned by the health care practitioners in several surveys. Health care practitioners were concerned over security issues when using the device 10 given that patient information is added to a third-party software. Moreover, health care practitioners mention that patients may feel they are constantly being watched, 13,18 with one study noting that this can potentially impact the patient–clinician relationship. 16 On the other hand, the health care practitioners in the study by Korpershoek et al 14 believed constant monitoring would enhance the relationship because patients will feel heard and supported by their health care practitioners through individualized care, which is in agreement with the patients’ reported perceptions. 33,34
Additionally, concerns about data accuracy was frequently mentioned whether the concern was due to lack of trust of the technology, 11,12 invalid patient measures, 13,14 or concerns of false positives. 18,19 In the study by Ding et al, 12 the health care practitioners were less comfortable diagnosing atrial fibrillation based on pulse data gathered from the wearables rather than medical electrocardiogram devices. This concern for inaccuracy of data is relevant as studies that evaluate and state that wearables provide accurate results have been conducted only in controlled settings. 35
Another major concern for the health care practitioners is the potential problem with patients relying heavily on RPM. 7,14,16 Patients may believe that their health care practitioners are continuously monitoring the data and may postpone contact. Other studies have demonstrated that RPM should not replace all in-person contact, 36,37 and self-efficacy was found to decrease in some telemonitored patients. 38 Sharif et al 21 stated that generation of error messages and abnormal data visible to patients leads to increased patient anxiety. Health care practitioners are not constantly assessing patient data and might not contact the patient immediately after data collection, further increasing patient anxiety and frustration.
Furthermore, a majority of the patient population is in an older age group for whom technology can be disorienting 15,21 or even the diversity of the equipment from different manufacturers can become complex. 7,11 However, finding a way to normalize data 12 or provide educational training 7,10,17 can reduce levels of concern.
Financial concerns were another prominent theme throughout the studies. Many health care practitioners indicated that access to these technologies can be difficult for low-income patient populations, 13,17 especially when there is no consensus on how to finance the devices. 10 In a survey done by Engler et al, 39 they found the main reason patients did not use monitoring technology was due to their high cost. However, Jeffs et al 20 found that RPM can result in overall cost savings for the patient due to consistent tracking of self-management supplies, minimizing overuse, and reducing the need for clinic visits. Additionally, the decreased need for emergency in-person visits will also be cost saving. 40 It can be used as an argument in favor of reimbursement through insurance for the use of telemonitoring technology. 41
Overall, health care practitioners found that RPM technology is beneficial due to the ability to monitor patients’ conditions continuously, decrease unnecessary clinic visits, and create personalized care. Patients are also able to access data to become more educated on their disease and increase their confidence in self-management. Although there were many positive perceptions and experiences, there were challenges, such as increased workload, privacy concerns, data accuracy, and financial burdens. Finding ways to overcome these challenges will be of utmost importance to ensure the successful implementation of these technologies, ultimately leading to improved patient outcomes.
Conclusion
This review shows that health care practitioners recognize telemonitoring as an increasingly relevant tool for patient care, and many find it acceptable for their practice. Recurring themes discussed the value of various technologies in treating various patients, and health care practitioners noted several ways telemonitoring can personalize care and enhance patient outcomes. Although there are many positive perceptions and experiences with telemonitoring, health care practitioners still have concerns regarding certain aspects of RPM. Finding ways to address these drawbacks will help improve this platform as it continues to become an important strategy in today’s medical care.
Limitations
This review has several limitations. There are limited data on health care workers’ experience with remote technology and gathering more information on the opinion of such practitioners can benefit the further development of telemonitoring. The studies included in this review varied on the type of technology used, the specialty, and what vitals were monitored, which could be a limitation for comparison. Additionally, there is the potential for misinterpretation of results due to the majority of the surveys being open-ended.
Footnotes
Funding: This study was supported in part by the Mayo Clinic Clinical Research Operations Group and Mayo Clinic Center for Regenerative Medicine.
Conflicts of Interest: None declared
Author Contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission. Luiza Palmieri Serrano, MS, designed the study, and Francisco R Avila, MD, Ricardo A Torres-Guzman, MD, John P Garcia, MD, conducted the data collection and selection. Luiza Palmieri Serrano, MS, Karla C Maita, MD, Abdullah S Eldaly, MD, analyzed the results and drafted the article. Clifton R Haider, PhD, Christopher L Felton, MS, and Margaret R Paulson, DO, performed a critical revision of the manuscript. Finally, Michael J Maniaci, MD, and Antonio J Forte, MD, PhD, approved the last version for publication.
References
- 1. Freiburger G, Holcomb M, Piper D . The STARPAHC collection: Part of an archive of the history of telemedicine . J Telemed Telecare . 2007; 13 ( 5 ): 221 – 223 . 10.1258/135763307781458949 [DOI] [PubMed] [Google Scholar]
- 2. Temesgen ZM, DeSimone DC, Mahmood M, Libertin CR, Varatharaj Palraj BR, Berbari EF . Health care after the COVID-19 pandemic and the influence of telemedicine . Mayo Clin Proc . 2020; 95 ( 9S ): S66 – S68 . 10.1016/j.mayocp.2020.06.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lakkireddy DR, Chung MK, Deering TF, et al . Guidance for rebooting electrophysiology through the COVID-19 pandemic from the Heart Rhythm Society and the American Heart Association Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology: Endorsed by the American College of Cardiology . Heart Rhythm . 2020; 17 ( 9 ): e242 – e254 . 10.1016/j.hrthm.2020.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wootton R . Twenty years of telemedicine in chronic disease management-an evidence synthesis . J Telemed Telecare . 2012; 18 ( 4 ): 211 – 220 . 10.1258/jtt.2012.120219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Deen MJ . Information and communications technologies for elderly ubiquitous healthcare in a smart home . Pers Ubiquit Comput . 2015; 19 ( 3–4 ): 573 – 599 . 10.1007/s00779-015-0856-x [DOI] [Google Scholar]
- 6. Majumder S, Mondal T, Deen MJ . Wearable sensors for remote health monitoring . Sensors (Basel) . 2017; 17 ( 1 ). 10.3390/s17010130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fraiche AM, Matlock DD, Gabriel W, Rapley F-A, Kramer DB . Patient and provider perspectives on remote monitoring of pacemakers and implantable cardioverter-defibrillators . Am J Cardiol . 2021; 149 : 42 – 46 . 10.1016/j.amjcard.2021.03.023 [DOI] [PubMed] [Google Scholar]
- 8. Page MJ, McKenzie JE, Bossuyt PM, et al . The PRISMA 2020 statement: An updated guideline for reporting systematic reviews . BMJ . 2021; 372 : 71 . 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sterne JA, Hernán MA, Reeves BC, et al . ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions . BMJ . 2016; 355 : e4919 . 10.1136/bmj.i4919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Aamodt IT, Lycholip E, Celutkiene J, et al . Health care professionals’ perceptions of home telemonitoring in heart failure care: Cross-sectional survey . J Med Internet Res . 2019; 21 ( 2 ): e10362 . 10.2196/10362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Abdolkhani R, Gray K, Borda A, DeSouza R . Patient-generated health data management and quality challenges in remote patient monitoring . JAMIA Open . 2019; 2 ( 4 ): 471 – 478 . 10.1093/jamiaopen/ooz036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ding EY, Svennberg E, Wurster C, et al . Survey of current perspectives on consumer-available digital health devices for detecting atrial fibrillation . Cardiovasc Digit Health J . 2020; 1 ( 1 ): 21 – 29 . 10.1016/j.cvdhj.2020.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hollenbach JP, Cushing A, Melvin E, McGowan B, Cloutier MM, Manice M . Understanding clinicians’ attitudes toward a mobile health strategy to childhood asthma management: A qualitative study . J Asthma . 2017; 54 ( 7 ): 754 – 760 . 10.1080/02770903.2016.1263649 [DOI] [PubMed] [Google Scholar]
- 14. Korpershoek YJG, Vervoort S, Trappenburg JCA, Schuurmans MJ . Perceptions of patients with chronic obstructive pulmonary disease and their health care providers towards using mHealth for self-management of exacerbations: A qualitative study . BMC Health Serv Res . 2018; 18 ( 1 ): 757 . 10.1186/s12913-018-3545-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Maguire R, Connaghan J, Arber A, et al . Advanced symptom management system for patients with malignant pleural mesothelioma (ASyMSmeso): Mixed methods study . J Med Internet Res . 2020; 22 ( 11 ): e19180 . 10.2196/19180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mansell SK, Kilbride C, Wood MJ, Gowing F, Mandal S . Experiences and views of patients, carers and healthcare professionals on using modems in domiciliary non-invasive ventilation (NIV): A qualitative study . BMJ Open Respir Res . 2020; 7 ( 1 ). 10.1136/bmjresp-2019-000510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lanssens D, Vandenberk T, Lodewijckx J, et al . Midwives’, obstetricians’, and recently delivered mothers’ perceptions of remote monitoring for prenatal care: Retrospective survey . J Med Internet Res . 2019; 21 ( 4 ). 10.2196/10887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Runkle J, Sugg M, Boase D, Galvin SL, C Coulson C . Use of wearable sensors for pregnancy health and environmental monitoring: Descriptive findings from the perspective of patients and providers . Digit Health . 2019; 5 : 2055207619828220 . 10.1177/2055207619828220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Craven MP, Andrews JA, Lang AR, et al . Informing the development of a digital health platform through universal points of care: Qualitative survey study . JMIR Form Res . 2020; 4 ( 11 ). 10.2196/22756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jeffs L, Jamieson T, Saragosa M, et al . Improving safety and efficiency in care: Multi-stakeholders’ perceptions associated with a peritoneal dialysis virtual care solution . Patient Prefer Adherence . 2018; 12 : 2623 – 2629 . 10.2147/PPA.S181604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sharif F, Rahman A, Tonner E, et al . Can technology optimise the pre-operative pathway for elective hip and knee replacement surgery: A qualitative study . Perioper Med (Lond) . 2020; 9 ( 1 ): 33 . 10.1186/s13741-020-00166-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lanssens D, Vonck S, Storms V, Thijs IM, Grieten L, Gyselaers W . The impact of a remote monitoring program on the prenatal follow-up of women with gestational hypertensive disorders . Eur J Obstet Gynecol Reprod Biol . 2018; 223 : 72 – 78 . 10.1016/j.ejogrb.2018.02.015 [DOI] [PubMed] [Google Scholar]
- 23. Jeffs L, Jain AK, Man RH, et al . Exploring the utility and scalability of a telehomecare intervention for patients with chronic kidney disease undergoing peritoneal dialysis-a study protocol . BMC Nephrol . 2017; 18 ( 1 ): 155 . 10.1186/s12882-017-0557-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Turakhia MP, Desai M, Hedlin H, et al . Rationale and design of a large-scale, app-based study to identify cardiac arrhythmias using a smartwatch: The Apple Heart Study . Am Heart J . 2019; 207 : 66 – 75 . 10.1016/j.ahj.2018.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Riegel B, Jaarsma T, Strömberg A . A middle-range theory of self-care of chronic illness . ANS Adv Nurs Sci . 2012; 35 ( 3 ): 194 – 204 . 10.1097/ANS.0b013e318261b1ba [DOI] [PubMed] [Google Scholar]
- 26. Dalfrà MG, Nicolucci A, Lapolla A, TISG . The effect of telemedicine on outcome and quality of life in pregnant women with diabetes . J Telemed Telecare . 2009; 15 ( 5 ): 238 – 242 . 10.1258/jtt.2009.081213 [DOI] [PubMed] [Google Scholar]
- 27. Homko CJ, Santamore WP, Whiteman V, et al . Use of an internet-based telemedicine system to manage underserved women with gestational diabetes mellitus . Diabetes Technol Ther . 2007; 9 ( 3 ): 297 – 306 . 10.1089/dia.2006.0034 [DOI] [PubMed] [Google Scholar]
- 28. Lundell S, Modig M, Holmner Å, Wadell K . Perceptions of home telemonitoring use among patients with chronic obstructive pulmonary disease: Qualitative study . JMIR Mhealth Uhealth . 2020; 8 ( 6 ): e16343 . 10.2196/16343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Marko KI, Krapf JM, Meltzer AC, et al . Testing the feasibility of remote patient monitoring in prenatal care using a mobile app and connected devices: A prospective observational trial . JMIR Res Protoc . 2016; 5 ( 4 ): e200 . 10.2196/resprot.6167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Pérez-Ferre N, Galindo M, Fernández MD, et al . A telemedicine system based on internet and short message service as a new approach in the follow-up of patients with gestational diabetes . Diabetes Res Clin Pract . 2010; 87 ( 2 ): e15 – e17 . 10.1016/j.diabres.2009.12.002 [DOI] [PubMed] [Google Scholar]
- 31. Gay V, Leijdekkers P . Bringing health and fitness data together for connected health care: Mobile apps as enablers of interoperability . J Med Internet Res . 2015; 17 ( 11 ): e260 . 10.2196/jmir.5094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mergel I . The long way from government open data to mobile health apps: Overcoming institutional barriers in the US federal government . JMIR Mhealth Uhealth . 2014; 2 ( 4 ): e58 . 10.2196/mhealth.3694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Nissen L, Lindhardt T . A qualitative study of COPD-patients’ experience of a telemedicine intervention . Int J Med Inform . 2017; 107 : 11 – 17 . 10.1016/j.ijmedinf.2017.08.004 [DOI] [PubMed] [Google Scholar]
- 34. Huniche L, Dinesen B, Nielsen C, Grann O, Toft E . Patients’ use of self-monitored readings for managing everyday life with COPD: A qualitative study . Telemed J E Health . 2013; 19 ( 5 ): 396 – 402 . 10.1089/tmj.2012.0135 [DOI] [PubMed] [Google Scholar]
- 35. Bumgarner JM, Lambert CT, Hussein AA, et al . Smartwatch algorithm for automated detection of atrial fibrillation . J Am Coll Cardiol . 2018; 71 ( 21 ): 2381 – 2388 . 10.1016/j.jacc.2018.03.003 [DOI] [PubMed] [Google Scholar]
- 36. Walker RC, Tong A, Howard K, Palmer SC . Patient expectations and experiences of remote monitoring for chronic diseases: Systematic review and thematic synthesis of qualitative studies . Int J Med Inform . 2019; 124 : 78 – 85 . 10.1016/j.ijmedinf.2019.01.013 [DOI] [PubMed] [Google Scholar]
- 37. Willems DCM, Joore MA, Hendriks JJE, Nieman FHM, Severens JL, Wouters EFM . The effectiveness of nurse-led telemonitoring of asthma: Results of a randomized controlled trial . J Eval Clin Pract . 2008; 14 ( 4 ): 600 – 609 . 10.1111/j.1365-2753.2007.00936.x [DOI] [PubMed] [Google Scholar]
- 38. Chatwin M, Hawkins G, Panicchia L, et al . Randomised crossover trial of telemonitoring in chronic respiratory patients (TeleCRAFT trial) . Thorax . 2016; 71 ( 4 ): 305 – 311 . 10.1136/thoraxjnl-2015-207045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Engler R, Routh TL, Lucisano JY . Adoption barriers for continuous glucose monitoring and their potential reduction with a fully implanted system: Results from patient preference surveys . Clin Diabetes . 2018; 36 ( 1 ): 50 – 58 . 10.2337/cd17-0053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Darvall JN, Parker A, Story DA . Feasibility and acceptability of remotely monitored pedometer-guided physical activity . Anaesth Intensive Care . 2016; 44 ( 4 ): 501 – 506 . 10.1177/0310057X1604400415 [DOI] [PubMed] [Google Scholar]
- 41. Thilly N, Chanliau J, Frimat L, et al . Cost-effectiveness of home telemonitoring in chronic kidney disease patients at different stages by a pragmatic randomized controlled trial (eNephro): Rationale and study design . BMC Nephrol . 2017; 18 ( 1 ): 126 . 10.1186/s12882-017-0529-2 [DOI] [PMC free article] [PubMed] [Google Scholar]