Abstract
Valvular heart disease (VHD) may lead to morbidities and mortality due to heart failure or sudden death. Concomitant coronary artery disease (CAD) is a crucial condition that needs to be explored in patients with VHD prior to cardiac valve surgery as it may increase morbidity and mortality. Patient age >40 years and mitral regurgitation are key risk factors for CAD in patients with VHD. The present study aimed to identify clinical risk factors for coronary stenosis in patients with high-risk VHD. The retrospective cohort study recruited patients aged >40 years who received cardiac valve surgery and coronary angiogram prior to cardiac valve surgery. Clinical factors predictive of coronary stenosis were computed by logistic regression analysis. There were 533 patients; 114 patients (21.38%) had coronary stenosis. Four factors were positively associated with coronary stenosis including age, male sex, mitral regurgitation and hypertension, while two factors were negatively associated with coronary stenosis, namely estimated glomerular filtration rate and rheumatic heart disease. Hypertension had the highest adjusted odds ratio at 2.596, while rheumatic heart disease had the lowest adjusted odds ratio at 0.428. Patient age >55 years showed a sensitivity and specificity of coronary stenosis of 80.70 and 37.47%, respectively. Clinical factors predictive of coronary stenosis in patients with high-risk VHD were age >55 years, male sex, mitral regurgitation and hypertension, while a high estimated glomerular filtration rate and presence of rheumatic heart disease were protective factors.
Keywords: age, sex, hypertension, renal function, rheumatic heart disease
Introduction
Valvular heart disease (VHD) is a cardiac condition that may lead to morbidity and mortality due to heart failure or sudden death (1-3). The prevalence of VHD is 3.1% in 1,818 Latinos/Hispanics individuals in the United States between October 2011 and June 24, 2014(4). A report from South Korea found that incidence of non-rheumatic valvular heart disease increased from 70.6 to 110.3/100,000 individuals from 2006 to 2011(5). Patients with VHD may require cardiac valvular surgery if symptoms are severe or left ventricle is dysfunction (6).
For those requiring surgical valvular treatment, the 2017 European Society of Cardiology (ESC) guidelines recommend coronary angiography prior to valvular surgery in the high-risk patients (7), including patients with evidence of coronary artery disease or severe mitral regurgitation and those aged >40 years. There are several cardiovascular risk factors that may contribute to coronary artery disease, such as atrial fibrillation, diabetes, obstructive sleep apnea or dyslipidemia (8-13).
Although coronary angiography is an invasive procedure with potential adverse side effects, it may be worthwhile as a means of identifying clinical factors associated with coronary artery stenosis. Additionally, a history of angina pain or non-invasive exercise testing for coronary artery disease may not be sensitive enough to detect stenosis. A study found that 40% of female patients with diabetes and coronary artery disease do not have angina chest pain and exercise testing for coronary artery disease has a sensitivity of 26% (14,15). Therefore, the present study aimed to evaluate which clinical factors are predictive of coronary artery stenosis in patients with high-risk VHD. By using clinical factors other than a history of angina pain or results from non-invasive tests for coronary stenosis, physicians may be able to recommend patients who require valvular heart surgery for coronary angiography prior to valvular surgery to test for coronary stenosis.
Materials and methods
Subjects
The present retrospective cohort study was conducted at University Hospital, Khon Kaen University, Thailand. There were 533 patients with a mean age of 59.86 (SD 9.64) and a proportion of male of 55.35% (295 patients). The inclusion criteria were patients aged ≥40 years who received cardiac valve surgery and coronary angiogram prior to cardiac valve surgery. Exclusion criteria included patients who had prosthetic valves, received emergency cardiac valve surgery or underwent a reoperation for cardiac valve surgery. Data were collected between January 2018 and January 2019. All eligible patients in the study received the standard clinical treatment for VHD.
Baseline characteristics, co-morbid disease, causes of VHD and current medications of eligible patients were recorded. Valvular abnormalities were recorded for those with severe regurgitation or stenosis by echocardiogram as proposed by a previous study (6) and causes of VHD were categorized as follows: Rheumatic heart disease, infective endocarditis, prolapse, ischemic and degenerative. Coronary stenosis was defined by a stenosis ≥50% in any coronary artery prior to cardiac valve surgery.
Statistical analysis
Data are presented as the mean ± SD. Patients were categorized into two groups based on the presence of coronary stenosis. Clinical factors predictive of coronary stenosis were computed using univariate logistic regression analysis. Factors with P<0.20 were used for stepwise multivariate logistic regression analysis. Factors with P<0.25 were accepted into the final model. Hosmer-Lemeshow χ2 was performed to evaluate goodness of fit for the final model. The significant numerical predictive factors were calculated for sensitivity and specificity using the area under a receiver operating characteristic (ROC) curve. The statistical analyses were performed using STATA software version 10.1 (College Station). P<0.05 was considered to indicate a statistically significant difference.
Results
There were 533 patients who met the study criteria; 114 patients (21.38%) had coronary stenosis (Table I). The mean number of coronary arteries exhibiting stenosis was 2.2±1.05. Patients in the coronary stenosis group had significantly older mean age (64.31 vs. 58.64 years; P<0.001) and significantly lower estimated glomerular filtration rate (68.47 vs. 76.81 ml/min/1.73 m2; P<0.001) than the non-coronary stenosis group. Regarding co-morbid diseases, the coronary stenosis group had a higher percentage of diabetes and hypertension (21.93% vs. 9.31%; P=0.001 and 47.37% vs. 18.85%; P<0.001) but a lower proportion of atrial fibrillation (21.93% vs. 44.15%; P<0.001) than the non-coronary stenosis group.
Table I.
Clinical features of patients with valvular heart disease who underwent diagnostic coronary angiography prior to cardiac valve surgery categorized by the presence of CS.
| Factor | No CS (n=419) | CS (n=114) | P-value |
|---|---|---|---|
| Mean age, years | 58.64 (9.26) | 64.31 (9.70) | <0.001 |
| Male sex (%) | 217 (51.79) | 78 (68.42) | 0.002 |
| Mean body mass index | 22.57 (4.08) | 23.20 (3.78) | 0.142 |
| Mean eGFR, ml/min/1.73 m2 | 76.81 (20.61) | 68.47 (23.34) | <0.001 |
| Co-morbidity (%) | |||
| Atrial fibrillation | 185 (44.15) | 25 (21.93) | <0.001 |
| Diabetes mellitus | 39 (9.31) | 25 (21.93) | 0.001 |
| Hypertension | 79 (18.85) | 54 (47.37) | <0.001 |
| Dyslipidemia | 61 (14.56) | 27 (23.68) | 0.023 |
| Stroke/TIA | 27 (6.44) | 4 (3.51) | 0.365 |
| Heart failure | 136 (32.46) | 44 (38.60) | 0.221 |
| Smoker (%) | 115 (28.47) | 38 (34.23) | 0.243 |
| Valve abnormality (%) | |||
| Aortic regurgitation | 114 (27.21) | 22 (19.30) | 0.091 |
| Aortic stenosis | 155 (36.99) | 43 (37.72) | 0.913 |
| Mitral regurgitation | 158 (37.71) | 60 (52.63) | 0.005 |
| Mitral stenosis | 191 (45.58) | 16 (14.04) | <0.001 |
| Tricuspid regurgitation | 149 (35.56) | 28 (24.56) | 0.033 |
| Mean number of abnormal valves | 1.83 (0.90) | 1.48 (0.72) | <0.001 |
| Causes of VHD (%) | |||
| Ischemic | 0 (0.00) | 19 (16.67) | <0.001 |
| Prolapse | 33 (7.88) | 6 (5.26) | 0.421 |
| Degenerative | 98 (23.39) | 40 (35.09) | 0.016 |
| Rheumatic heart disease | 230 (54.89) | 26 (22.81) | <0.001 |
| Infective endocarditis | 17 (4.07) | 2 (1.75) | 0.391 |
| Medication (%) | |||
| ACEI/ARB | 77 (18.42) | 34 (29.82) | 0.009 |
| Aspirin | 114 (27.27) | 65 (57.02) | <0.001 |
| β blocker | 142 (33.97) | 42 (36.84) | 0.580 |
| Digoxin | 115 (27.51) | 14 (12.28) | 0.001 |
| Diuretic | 268 (64.11) | 51 (44.74) | <0.001 |
| Warfarin | 176 (42.11) | 19 (16.67) | <0.001 |
CS, coronary stenosis; eGFR, estimated glomerular filtration rate; TIA, transient ischemic attack; ACEI, angiotensin-converting-enzyme inhibitor; ARB, angiotensin receptor blocker.
Coronary stenosis group had more patients with mitral regurgitation (52.63 vs. 37.71%; P=0.005) but fewer patients with tricuspid regurgitation (24.56 vs. 35.56%; P=0.033) and mitral stenosis (14.04 vs. 45.58%; P<0.001) than the non-coronary stenosis group. The coronary stenosis group had a greater occurrence of degenerative causes of VHD (35.09%; P=0.016), while the non-coronary stenosis group had more patients with rheumatic heart disease (54.89%; P<0.001). The coronary stenosis group had a higher proportion of patients receiving angiotensin-converting-enzyme inhibitor/angiotensin receptor blocker (ACEI/ARB) and aspirin therapy than the non-coronary stenosis group (29.82% vs. 18.42%; P=0.009). Patients with rheumatic heart disease had a significantly lower mean age than those without (56.07 vs. 63.35 years; P<0.001), while patients with ischemic VHD had slightly older age than those with non-ischemic VHD (62.63 vs. 59.75 years; P=0.202).
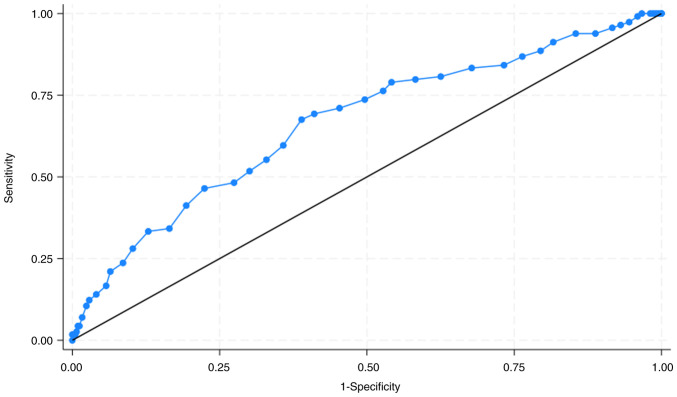
Factors included in the stepwise logistic regression analysis were age, sex, body mass index, estimated glomerular filtration rate, atrial fibrillation, diabetes mellitus, hypertension, dyslipidemia, rheumatic heart disease, mitral regurgitation, mitral stenosis, tricuspid regurgitation and history of smoking, heart failure and stroke/TIA. There were eight factors included in the final model predictive of coronary stenosis (Table II). A total of six factors were significant risk factors for coronary stenosis. Of these, four factors were positively associated with coronary stenosis, namely age, male sex, mitral regurgitation and hypertension, while two factors were negatively associated with coronary stenosis, namely estimated glomerular filtration rate and rheumatic heart disease. Hypertension had the highest adjusted odds ratio at 2.596 (95% confidence interval of 1.574, 4.280; P<0.05), while both high estimated glomerular filtration rate and rheumatic heart disease had adjusted odds ratios of 0.985 (95% confidence interval of 0.981, 0.997; P<0.05). The Hosmer-Lemeshow χ2 value of the final model was 8.64 (P=0.374; data not shown). Patient age >55 years had a sensitivity and specificity of coronary stenosis of 80.70 and 37.47%, respectively. The area under ROC curve was 66.45% (95% confidence interval, 60.69, 72.21; Fig. 1).
Table II.
Clinical factors predictive of coronary stenosis in patients with valvular heart disease patients who received diagnostic coronary angiography prior to cardiac valve surgery.
| Factor | Unadjusted odds ratio (95% confidence interval) | Adjusted odds ratio (95% confidence interval) |
|---|---|---|
| Age | 1.066 (1.041, 1.091) | 1.038 (1.009, 1.068)a |
| Male sex | 2.016 (1.300, 3.128) | 2.210 (1.340, 3.646)a |
| Body mass index | 1.038 (0.987, 1.092) | 1.041 (0.981, 1.105) |
| eGFR | 0.980 (0.970, 0.991) | 0.985 (0.981, 0.997)a |
| Atrial fibrillation | 0.355 (0.219, 0.576) | 0.584 (0.321, 1.059) |
| Mitral regurgitation | 1.835 (1.209, 2.786) | 1.878 (1.160, 3.041)a |
| Hypertension | 3.873 (2.490, 6.024) | 2.596 (1.574, 4.280)a |
| Rheumatic heart disease | 0.242 (0.150, 0.391) | 0.985 (0.981, 0.997)a |
aP<0.05. eGFR, estimated glomerular filtration rate; Bold indicating significant factor.
Figure 1.
ROC curve of age in patients with coronary stenosis and valvular heart who received diagnostic coronary angiography prior to cardiac valve surgery. The area under the ROC curve was 66.45%. ROC, receiver operating characteristic.
Discussion
The present study showed a prevalence of coronary stenosis in patients with VHD of 21.38%, which was lower than a previous report from Lebanon (27.75%) (16). These differences may be due to a different study population (17). Unlike the report from Lebanon, the present study did not find significant differences in aortic stenosis. The aforementioned report showed that severe aortic stenosis is the most common form of VHD associated significant coronary stenosis (16). The present study found mitral regurgitation was the most common type of VHD associated with CAD and was independently associated with significant coronary stenosis, as previously reported (7).
Other than mitral regurgitation, the present study showed predictors for coronary stenosis in VHD were age, sex, estimated glomerular filtration rate, hypertension and rheumatic heart disease. Certain cardiovascular risk factors included in the analysis were not retained in the final model, such as atrial fibrillation, diabetes and dyslipidemia. As previously reported, age, male sex and hypertension were associated with coronary artery disease (18-21), while low glomerular filtration rate may increase risk of coronary artery disease (22). A previous study found that age and male sex have an adjusted odds ratio of 1.0560 and 2.6003, which were comparable to those found in the present study (23). The 2017 ESC guidelines recommend pre-operative coronary angiogram in patients with VHD aged >40 years (7); here, patient age >55 years had a sensitivity of 80%.
Rheumatic heart disease was negatively associated with coronary stenosis. Even though a previous study found that mitral regurgitation is the most common type of rheumatic heart disease (24), only 101 patients in the present study had mitral regurgitation from rheumatic heart disease (39.45%). The aforementioned negative association may be explained by patient age since mitral regurgitation was negatively associated with age (coefficient of -0.188) (24). Patients with rheumatic heart disease may be younger and therefore at a lower risk for coronary artery disease. Here, patients with rheumatic heart disease had a significantly lower mean age than those without. A study from Brazil found that only 4% of patients with rheumatic heart disease have coronary artery disease compared with 33.61% of patients without rheumatic heart disease (25). A study from China found that patients with rheumatic heart disease undergoing valvular surgery for coronary artery disease are older than those without coronary artery disease (63 vs. 54 years; P<0.01) (26). Although the mean age of the present study was comparable with the aforementioned studies, the present study found that rheumatic heart disease was protective factor for coronary stenosis in patients who underwent valvular surgery.
Risk factors for coronary stenosis in patients with VHD include male sex, age >55 years, hypertension and low estimated glomerular filtration rate. Those with rheumatic heart disease may be at a lower risk of coronary artery disease. Finally, these risk factors were identified independently of chest pain or other non-invasive exercise testing for coronary artery disease. Physicians may consider these risk factors when deciding on pre-operative coronary angiography prior to cardiac valve surgery in patients with VHD who are aged >40 years, regardless of history of angina pain or non-invasive exercise testing for coronary artery disease.
There are limitations in the present study. First, the present study population was a single, referral, university hospital resulting in small sample size. An interpretation of the results should be performed cautiously as the logistic model may lack sufficient power. The trace back power of the dataset was 99.7%. Second, certain factors for coronary artery disease were not included such as obstructive sleep apnea (27-34). Clinicians may use the model as a guide to evaluate the risk of coronary stenosis. Finally, the prevalence of rheumatic heart disease was high (48.03%). The results of this study may be applicable for populations with a similar prevalence of rheumatic heart disease. The primary outcome of this study was presence of coronary stenosis of >50%, not the percentage of coronary stenosis. The presence of significant coronary stenosis may be more clinical relevant than the percentage of coronary stenosis as the guideline recommends coronary bypass graft surgery prior to heart valve surgery if coronary stenosis is over 50% (7).
Clinical factors predictive of coronary stenosis in patients with high-risk VHD were age >55 years, male sex, mitral regurgitation and hypertension, while high estimated glomerular filtration rate and rheumatic heart disease were protective factors. Patients who are identified as higher risk based on these risk factors should be considered for coronary angiogram prior to cardiac valve surgery.
Acknowledgements
Not applicable.
Funding Statement
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present study are available from the corresponding author upon reasonable request.
Authors' contributions
SW and KS conceived and designed the study. DK and VC interpreted data. KS performed statistical analysis. All authors have read and approved the final manuscript. SW and DK confirm the authenticity of all the raw data.
Ethics approval and consent to participate
The present study was approved by the Institutional Review Board at the Ethical Committee of Khon Kaen University, Thailand (approval no. HE591473.) The requirement for informed consent was waived due to the retrospective nature of the study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Rizzi MA, Sarasola AG, Arbé AA, Mateo SH, Gil V, Llorens P, Jacob J, Martín-Sánchez FJ, Puente PH, Escoda R, et al. Factors associated with in-hospital mortality and adverse outcomes during the vulnerable post-discharge phase after the first episode of acute heart failure: Results of the NOVICA-2 study. Clin Res Cardiol. 2021;110:993–1005. doi: 10.1007/s00392-020-01710-0. [DOI] [PubMed] [Google Scholar]
- 2.Noubiap JJ, Nyaga UF, Ndoadoumgue AL, Nkeck JR, Ngouo A, Bigna JJ. Meta-Analysis of the incidence, prevalence, and correlates of atrial fibrillation in rheumatic heart disease. Glob Heart. 2020;15(38) doi: 10.5334/gh.807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Henriques de Gouveia RHAM, Corte Real Gonçalves FMA. Sudden cardiac death and valvular pathology. Forensic Sci Res. 2019;4:280–286. doi: 10.1080/20961790.2019.1595351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rubin J, Aggarwal SR, Swett KR, Kirtane AJ, Kodali SK, Nazif TM, Pu M, Dadhania R, Kaplan RC, Rodriguez CJ. Burden of valvular heart diseases in hispanic/latino individuals in the United States: The echocardiographic study of latinos. Mayo Clin Proc. 2019;94:1488–1498. doi: 10.1016/j.mayocp.2018.12.035. [DOI] [PubMed] [Google Scholar]
- 5.Jang SY, Ju EY, Seo SR, Choi JY, Park SJ, Kim DK, Park SW. Changes in the etiology of valvular heart disease in the rapidly aging Korean population. Int J Cardiol. 2014;174:355–359. doi: 10.1016/j.ijcard.2014.04.112. [DOI] [PubMed] [Google Scholar]
- 6.Brinkley DM, Gelfand EV. Valvular heart disease: Classic teaching and emerging paradigms. Am J Med. 2013;126:1035–1042. doi: 10.1016/j.amjmed.2013.05.022. [DOI] [PubMed] [Google Scholar]
- 7.Falk V, Baumgartner H, Bax JJ, De Bonis M, Hamm C, Holm PJ, Iung B, Lancellotti P, Lansac E, Muñoz DR, et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur J Cardiothorac Surg. 2017;52:616–664. doi: 10.1093/ejcts/ezx324. [DOI] [PubMed] [Google Scholar]
- 8.Khamsai S, Chootrakool A, Limpawattana P, Chindaprasirt J, Sukeepaisarnjaroen W, Chotmongkol V, Silaruks S, Senthong V, Sittichanbuncha Y, Sawunyavisuth B, Sawanyawisuth K. Hypertensive crisis in patients with obstructive sleep apnea-induced hypertension. BMC Cardiovasc Disord. 2021;21(310) doi: 10.1186/s12872-021-02119-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Soontornrungsun B, Khamsai S, Sawunyavisuth B, Limpawattana P, Chindaprasirt J, Senthong V, Chotmongkol V, Sawanyawisuth K. Obstructive sleep apnea in patients with diabetes less than 40 years of age. Diabetes Metab Syndr. 2020;14:1859–1863. doi: 10.1016/j.dsx.2020.09.008. [DOI] [PubMed] [Google Scholar]
- 10.Khamsai S, Mahawarakorn P, Limpawattana P, Chindaprasirt J, Sukeepaisarnjaroen W, Silaruks S, Senthong V, Sawunyavisuth B, Sawanyawisuth K. Prevalence and factors correlated with hypertension secondary from obstructive sleep apnea. Multidiscip Respir Med. 2021;16(777) doi: 10.4081/mrm.2021.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khamsai S, Kachenchart S, Sawunyavisuth B, Limpawattana P, Chindaprasirt J, Senthong V, Chotmongkol V, Pongkulkiat P, Sawanyawisuth K. Prevalence and risk factors of obstructive sleep apnea in hypertensive emergency. J Emerg Trauma Shock. 2021;14:104–107. doi: 10.4103/JETS.JETS_47_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Manasirisuk P, Chainirun N, Tiamkao S, Lertsinudom S, Phunikhom K, Sawunyavisuth B, Sawanyawisuth K. Efficacy of generic atorvastatin in a real-world setting. Clin Pharmacol Adv Appl. 2021;13:45–51. doi: 10.2147/CPAA.S285750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sanlung T, Sawanyawisuth K, Silaruks S, Khamsai S, Limpawattana P, Chindaprasirt J, Senthong V, Kongbunkiat K, Timinkul A, Phitsanuwong C, et al. Clinical characteristics and complications of obstructive sleep apnea in srinagarind hospital. J Med Assoc Thai. 2020;103(36) [Google Scholar]
- 14.Krul MM, Bogaard K, Knol RJ, van Rossum AC, Knaapen P, Cornel JH, van der Zant FM. Coronary artery disease in patients with atypical chest pain with and without diabetes mellitus assessed with coronary CT angiography. BMJ Open Diabetes Res Care. 2014;2(e000004) doi: 10.1136/bmjdrc-2013-000004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goldkorn R, Naimushin A, Shlomo N, Dan A, Oieru D, Moalem I, Rozen E, Gur I, Levitan J, Rosenmann D, et al. Comparison of the usefulness of heart rate variability versus exercise stress testing for the detection of myocardial ischemia in patients without known coronary artery disease. Am J Cardiol. 2015;115:1518–1522. doi: 10.1016/j.amjcard.2015.02.054. [DOI] [PubMed] [Google Scholar]
- 16.Matta A, Moussallem N. Coronary artery disease is associated with valvular heart disease, but could it Be a predictive factor? Indian Heart J. 2019;71:284–287. doi: 10.1016/j.ihj.2019.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rostomian AH, Soverow J, Sanchez DR. Exploring Armenian Ethnicity as an independent risk factor for cardiovascular disease: Findings from a prospective cohort of patients in a County Hospital. JRSM Cardiovasc Dis. 2020;9(2048004020956853) doi: 10.1177/2048004020956853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yu YT, Hou ZH, Lu B, An YQ, Gao Y, Yin WH, Ren XS. Prevalence of coronary artery disease in symptomatic patients with zero coronary artery calcium score in different age population. Int J Cardiovasc Imaging. 2021;37:723–729. doi: 10.1007/s10554-020-02028-8. [DOI] [PubMed] [Google Scholar]
- 19.Faber M, Will A, Hendrich E, Martinoff S, Hadamitzky M. Sex- and age-specific differences in the long-term prognostic value of morphological plaque features detected by coronary computed tomography angiography. J Cardiovasc Comput Tomogr. 2021;15:274–280. doi: 10.1016/j.jcct.2020.09.003. [DOI] [PubMed] [Google Scholar]
- 20.Manfrini O, Yoon J, van der Schaar M, Kedev S, Vavlukis M, Stankovic G, Scarpone M, Miličić D, Vasiljevic Z, Badimon L, et al. Sex differences in modifiable risk factors and severity of coronary artery disease. J Am Heart Assoc. 2020;9(e017235) doi: 10.1161/JAHA.120.017235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Whelton SP, McEvoy JW, Shaw L, Psaty BM, Lima JAC, Budoff M, Nasir K, Szklo M, Blumenthal RS, Blaha MJ. Association of normal systolic blood pressure level with cardiovascular disease in the absence of risk factors. JAMA Cardiol. 2020;5:1011–1018. doi: 10.1001/jamacardio.2020.1731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shroff GR, Sanchez OA, Miedema MD, Kramer H, Ix JH, Duprez DA, Jacobs DR Jr. Coronary artery calcium progresses rapidly and discriminates incident cardiovascular events in chronic kidney disease regardless of diabetes: The Multi-Ethnic Study of Atherosclerosis (MESA) Atherosclerosis. 2020;310:75–82. doi: 10.1016/j.atherosclerosis.2020.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sharma K, Singhal R, Jadhav N, Shah K, Patil S. Evaluation of SERENE-CAG score for assessing suitability for coronary angiography preoperatively in patients undergoing valve replacement surgery. Indian Heart J. 2018;70 (Suppl 3):S189–S193. doi: 10.1016/j.ihj.2018.10.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Butt HI, Shahbaz A, Nawaz H, Butt K. Comparative clinical characteristics of rheumatic heart disease patients undergoing surgical valve replacement. Cureus. 2019;11(e4889) doi: 10.7759/cureus.4889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li BL, Li L, Hou XL, He B, Zhang GX, Chen KB, Xu ZY. Prevalence of coronary artery disease in patients with rheumatic heart disease in China. Zhonghua Yi Xue Za Zhi. 2007;87:3313–3316. (In Chinese) [PubMed] [Google Scholar]
- 26.Kruczan DD, Silva NA, Pereira Bde B, Romão VA, Correa Filho WB, Morales FE. Coronary artery disease in patients with rheumatic and non-rheumatic valvular heart disease treated at a public hospital in Rio de Janeiro. Arq Bras Cardiol. 2008;90:197–203. doi: 10.1590/s0066-782x2008000300010. [DOI] [PubMed] [Google Scholar]
- 27.Perera A, Mudannayake SD, Azamathulla HM, Rathnayake U. Recent climatic trends in Trinidad and Tobago, West Indies. Asia-Pac J Sci Technol. 2020;25(25) [Google Scholar]
- 28.Jeerasuwannakul B, Sawunyavisuth B, Khamsai S, Sawanyawisuth K. Prevalence and risk factors of proteinuria in patients with type 2 diabetes mellitus. Asia-Pac J Sci Technol. 2021;26(26) [Google Scholar]
- 29.Suebsamran P, Aekplakorn W, Chamnan P, Bumrerraj S, Kuhiranyaratn P, Kessomboon P. Association of body mass index and other factors with metabolically unhealthy status: Results from the national health examination survey IV. Asia-Pac J Sci Technol. 2021;26(26) [Google Scholar]
- 30.Sawunyavisuth B. What are predictors for a continuous positive airway pressure machine purchasing in obstructive sleep apnea patients? Asia-Pac J Sci Technol. 2018;23:APST–23. [Google Scholar]
- 31.Sawunyavisuth B, Ngamjarus C, Sawanyawisuth K. Any effective intervention to improve CPAP adherence in children with obstructive sleep apnea: A systematic review. Glob Pediatr Health. 2021;8(2333794X211019884) doi: 10.1177/2333794X211019884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hlaing SS, Puntumetakul R, Wanpen S, Saiklang P. Updates on core stabilization exercise and strengthening exercise: A review article. Asia-Pac J Sci Technol. 2021;26:APST–26. [Google Scholar]
- 33.Kaewkes C, Sawanyawisuth K, Sawunyavisuth B. Are symptoms of obstructive sleep apnoea related to good continuous positive airway pressure compliance? ERJ Open Res. 2020;6:00169–02019. doi: 10.1183/23120541.00169-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sawunyavisuth B. What personal experiences of CPAP use affect CPAP adherence and duration of CPAP use in OSA patients? J Med Assoc Thai. 2018;101(S245) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the present study are available from the corresponding author upon reasonable request.