Abstract
Artificial intelligence (AI) has impacted many areas of healthcare. AI in healthcare uses machine learning, deep learning, and natural language processing to analyze copious amounts of healthcare data and yield valuable outcomes. In the sleep medicine field, a large amount of physiological data is gathered compared to other branches of medicine. This field is primed for innovations with the help of AI. A good quality of sleep is crucial for optimal health. About one billion people are estimated to have obstructive sleep apnea worldwide, but it is difficult to diagnose and treat all the people with limited resources. Sleep apnea is one of the major contributors to poor health. Most of the sleep apnea patients remain undiagnosed. Those diagnosed with sleep apnea have difficulty getting it optimally treated due to several factors, and AI can help in this situation. AI can also help in the diagnosis and management of other sleep disorders such as insomnia, hypersomnia, parasomnia, narcolepsy, shift work sleep disorders, periodic leg movement disorders, etc. In this manuscript, we aim to address three critical issues about the use of AI in sleep medicine: (1) How can AI help in diagnosing and treating sleep disorders? (2) How can AI fill the gap in the care of sleep disorders? and (3) What are the ethical and legal considerations of using AI in sleep medicine?
Keywords: Artificial intelligence; Machine learning; Deep learning; Ethical; Legal, and sleep disorders
Core Tip: Most of the sleep apnea patients remain undiagnosed worldwide. Artificial intelligence can help alert people to be evaluated and seek treatment on time to improve overall health. Treatment of sleep apnea may improve or delay certain chronic illnesses.
INTRODUCTION
Approximately one billion people worldwide suffer from obstructive sleep apnea (OSA), a condition characterized by intermittent hypoxia due to upper airway blockage during sleep[1]. The condition is diagnosed with a sleep study test where a positive result shows an apnea and hypopnea index (AHI) of five or more events per hour. Out of those one billion people, about 435 million suffer from moderate to severe degrees of sleep apnea with AHI of 15 or more per hour in the age range of 30-69 years[1]. The prevalence could be even higher in the older population. About 82% of sleep apnea patients remain undiagnosed[2], where untreated intermittent hypoxia leads to significant end-organ damage and debility. Scientists working in different fields are coming to the conclusion that sleep apnea is associated with multiple health conditions. However, the treatment of sleep apnea with positive airway pressure (PAP) still has a lot of compliance issues. A study looked at 20 years of trends of CPAP adherence and found that the non-adherence rate was around 34%[3]. Other treatment options exist for sleep apnea, but individualized assessment and management are required. Artificial intelligence (AI) and machine learning (ML) bring the opportunity to understand and monitor sleep disorders with easy-to-use smart technologies and may lead to better treatment outcomes.
How artificial intelligence can help in diagnosing and treating sleep disorders?
The scoring of sleep studies is a very labor-intensive process that requires significant manual effort to analyze data sets. This can be done easily and efficiently by AI. At present, many automated scoring systems are used with fair accuracy. AI in sleep medicine is currently used for sleep staging, respiratory events scoring, insomnia characterization, prediction of circadian rhythm from gene expression, and phenotyping of OSA[4]. Multiple home sleep testing devices are available that integrate AI for automated scoring using ML. AI can help in scoring in-lab sleep studies using ML, making sleep lab staff and clinicians more efficient. The Food and Drug Administration (FDA) has cleared several auto-scoring software systems. So many wearable devices are directly available to consumers, such as the Fitbit Sense, Samsung Galaxy Watch, Garmin watch, and Apple Watch, which can alert users to seek medical help sooner rather than later. Abnormal sleep data obtained from a wearable device may give clues to its users to get further testing and seek treatment for sleep-disordered breathing.
Treatment of sleep apnea is complex in view of pathophysiology, risk factors, and comorbid health conditions that make the treatment challenging. The treatment non-adherence with PAP therapy is high (29%-83%) in sleep apnea patients[5]. AI can help understand the factors contributing to OSA, pathophysiology, treatment response, and choice of treatment options for individual patients. Thus, it can improve the overall success rate for sleep apnea treatment by choosing the most effective treatment for individual patients[6]. AI can help to predict adherence to PAP therapy in OSA patients and alert clinicians to take early interventions[7]. AI can also help insomnia patients by characterizing insomnia and providing longitudinal sleep-related data monitoring.
How AI can fill gap in the care of sleep disorders?
A snoring-based contactless AI system using two dimensions convolutional neural network and visibility graph method can recognize OSA-hypopnea syndrome (OSAHS) with an accuracy of 92.5%. With a predicted sensitivity of 93.9% and specificity of 91.2% of OSAHS, this system seems superior compared to polysomnography (PSG)[8]. This type of AI technology can alert users to get tested and treated for sleep apnea and capture many previously undiagnosed patients. Recently, the FDA cleared Sunrise home sleep testing device that uses machine-based learning to analyze mandibular jaw movement to predict sleep apnea with comparable accuracy to in-home manually scored PSG[9]. This device also offers multi-night longitudinal home testing to minimize the effect of night-to-night variability in the current sleep testing environment.
Polymer sensor embedded, internet of Things (IoT) enabled t-shirts have many sensors to gather multiple cardio-pulmonary physiological data, and it can help diagnose and monitor sleep-disordered breathing, which can be further utilized in the future using ML and AI[10]. This can help clinicians monitor their patients remotely in a variety of settings. The fusion of IoT devices capable of interoperability can produce the IoT, which can help in the smart diagnosis and management of sleep apnea[11].
AI technology can also increase the scope of analysis beyond simple one on one interaction with patients. Using large-scale data obtained from sleep testing numerous patients, AI can help formulate algorithms that can advance the field of sleep medicine. Consumer sleep technologies, such as wearables and phone applications, generate millions of nights of sleep data, which can be analyzed in more meaningful ways with the help of standardized AI technologies. AI can fill this gap by evaluating the data in real-time to predict patterns that will help identify potential patients.
Similar to an alert generated for anticoagulation in atrial fibrillation while using the electronic health record (EHR) system, AI can also create an algorithm to alert clinicians if a certain patient is at high risk of sleep apnea. This algorithm could be generated using patients’ health characteristics, STOP-BANG score, Epworth Sleepiness Scale score, laboratory profile, and imaging results. There is a certain pattern in the lipid profile, which is indicative of sleep apnea, as noted in a recent study[12]. Magnetic resonance imaging brain using diffusion tensor imaging with ML can diagnose sleep apnea with 73%-77% accuracy[13]. The Cleveland Clinic Foundation has developed a sleep app for general consumers to fill out a few questionnaires. It can alert users about their risks of sleep apnea, insomnia, shift work, and insufficient sleep[14]. Since most patients with sleep disorders are undiagnosed, this type of innovation will help them and clinicians manage sleep disorders to improve overall health outcomes.
Diagnosing narcolepsy is very challenging as it requires multiple sleep latency tests (MSLT), which have a lot of limitations with variability and depend upon several factors for their accuracy. The AI algorithm can help diagnose narcolepsy type 1 in a single night by using ML with reasonable accuracy[15]. A recent study found that if sleep parameters are added to routine sleep testing with the help of an interpretable machine-learning model, the Adaboost model, it can predict cardiovascular morbidity and all-cause mortality[16]. This integration and prediction model can help clinicians further intervene in potential future health problems.
Sleep disturbances boost the aging process. Researchers can predict age with fair accuracy from sleep studies analyzed using deep learning[17]. FDA recently cleared ‘Dreem 3S’, a wearable headband that uses AI and ML to provide equivalent data about sleep stages compared to PSG[18]. This type of device has a lot of potential in terms of diagnosis, treatment, research, and monitoring of various diseases caused by sleep disturbances. The Dreem 3S device can provide prolonged monitoring of sleep that is needed to diagnose idiopathic hypersomnia. It can also help monitor accurate sleep data and replace sleep logs and actigraphy prior to PSG and MSLT in the assessment of hypersomnia.
Generative pre-trained transformers such as ChatGPT are large language models that have recently been used in patient education. In healthcare, radiology has been at the forefront of AI adoption. However, ChatGPT has immense potential for patient education in the field of sleep medicine as well[19].
Clinicians spend a lot of time charting medical notes, which curbs direct time spent with the patients. As the AI starts capturing and helping more and more patients diagnosed with sleep disorders, time efficiency will be crucial for sleep medicine providers. The AI can help as a scribe for physicians to finish medical charts on time, as many physicians may need to improve at typing[20].
What are the ethical and legal considerations of using AI in sleep medicine?
As the use of AI is increasing, ethical and legal issues also arise. Multiple teams of scientists and researchers are working to develop several different technologies and algorithms, raising the need for governing international bodies for standardization. We need a lot of quality data for ML, but data gathering is difficult due to patients’ privacy concerns, regulations, and organizational policies. The other challenge is using different data-gathering systems used by various organizations, creating roadblocks in interoperability and standardization. There is a potential for data breach while incorporating different organizations. To promote AI in the field of medicine, there should be some immunity for researchers from legal actions.
Furthermore, the baseline datasets should be diverse enough to avoid bias while developing AI algorithms. Most datasets do not include LGBTQ information, so there may be bias and limitations while using AI, especially for those patients[21]. The American Academy of Sleep Medicine has an AI committee that advocates for good practice guidelines in sleep medicine. The FDA also assesses these technologies from a safety point of view. The lack of extensive training data sets for AI and ML is a persistent challenge for more comprehensive clinical utilization of AI, and the regulatory landscape is rapidly evolving. Night-to-night and age-related variation in patients' sleep data limits the generalizability of this data[3,22]. The innovations in sleep medicine are happening quickly, and it is tough for governing bodies to keep pace with a fast-changing landscape. Collaboration between clinicians, researchers, health institutions with big data pools, and AI engineers will be crucial to advance the field of AI in sleep medicine (Figure 1).
Figure 1.
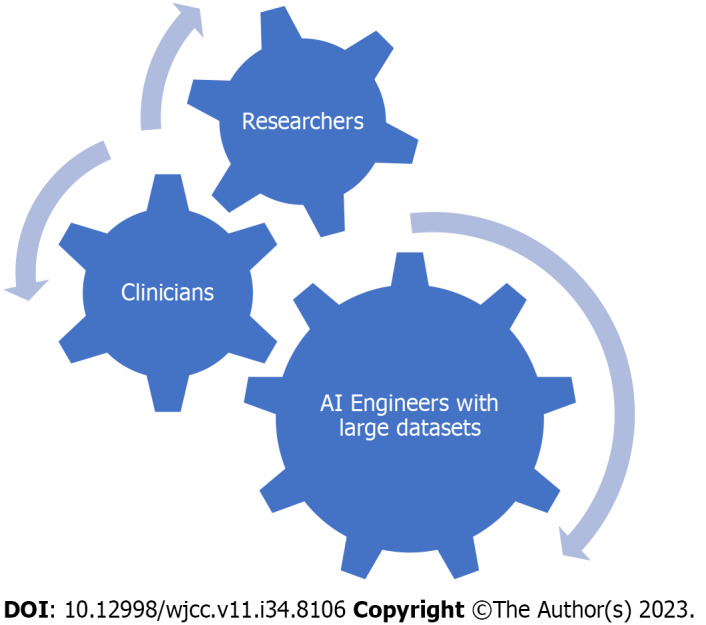
Collaboration of researchers, clinicians, institutions with large datasets, and artificial intelligence engineers is needed for better use of artificial intelligence in medicine. AI: Artificial intelligence.
CONCLUSION
The development of AI technologies can aid in finding those patients who were previously undiagnosed with sleep apnea. It can also help choose the most effective treatment or combination of treatments for specific patients, leading to a higher success rate. Treatment failure signals can be identified earlier, which will alert clinicians to intervene on time. AI can also incorporate large data sets to provide clinical predictions, improving accuracy and long-term fidelity. If AI is integrated with EHR systems, it can alert the treating providers, using readily available objective data, that a specific patient is at risk of sleep-disordered breathing. Integrating AI into clinical workflows can improve efficiency and help sleep providers serve more patients effectively. In the future, AI will play a huge role in sleep disorders’ screening, monitoring, prevention, prediction, diagnosis, and treatment.
Footnotes
Conflict-of-interest statement: All the authors report no relevant conflicts of interest for this article.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author’s Membership in Professional Societies: American Academy of Sleep Medicine.
Peer-review started: October 14, 2023
First decision: November 2, 2023
Article in press: November 24, 2023
Specialty type: Medicine, research and experimental
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Sun D, China S-Editor: Wang JJ L-Editor: A P-Editor: Zhao S
Contributor Information
Ram Kishun Verma, Department of Sleep Medicine, Parkview Health System, Fort Wayne, IN 46845, United States.
Gagandeep Dhillon, Department of Medicine, UM Baltimore Washington Medical Center, Glen Burnie, MD 21061, United States.
Harpreet Grewal, Department of Radiology, Ascension Sacred Heart Hospital, Pensacola, FL 32504, United States.
Vinita Prasad, Department of Psychiatry, Parkview Health System, Fort Wayne, IN 46845, United States.
Ripudaman Singh Munjal, Department of Medicine, Kaiser Permanente Medical Center, Modesto, CA 95356, United States.
Pranjal Sharma, Department of Medicine, Banner Health, Phoenix, AZ 85006, United States.
Venkata Buddhavarapu, Department of Medicine, Norteast Ohio Medical University, Rootstown, OH 44272, United States.
Ramprakash Devadoss, Department of Cardiology, Carle Methodist Medical Center, Peroria, IL 61637, United States.
Rahul Kashyap, Department of Research, Wellspan Health, York, PA 17403, United States.
Salim Surani, Department of Medicine & Pharmacology, Texas A&M University, College Station, TX 77843, United States. srsurani@hotmail.com.
References
- 1.Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MSM, Morrell MJ, Nunez CM, Patel SR, Penzel T, Pépin JL, Peppard PE, Sinha S, Tufik S, Valentine K, Malhotra A. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019;7:687–698. doi: 10.1016/S2213-2600(19)30198-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Finkel KJ, Searleman AC, Tymkew H, Tanaka CY, Saager L, Safer-Zadeh E, Bottros M, Selvidge JA, Jacobsohn E, Pulley D, Duntley S, Becker C, Avidan MS. Prevalence of undiagnosed obstructive sleep apnea among adult surgical patients in an academic medical center. Sleep Med. 2009;10:753–758. doi: 10.1016/j.sleep.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 3.Rotenberg BW, Murariu D, Pang KP. Trends in CPAP adherence over twenty years of data collection: a flattened curve. J Otolaryngol Head Neck Surg. 2016;45:43. doi: 10.1186/s40463-016-0156-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bandyopadhyay A, Goldstein C. Clinical applications of artificial intelligence in sleep medicine: a sleep clinician's perspective. Sleep Breath. 2023;27:39–55. doi: 10.1007/s11325-022-02592-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sawyer AM, Gooneratne NS, Marcus CL, Ofer D, Richards KC, Weaver TE. A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev. 2011;15:343–356. doi: 10.1016/j.smrv.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brennan HL, Kirby SD. The role of artificial intelligence in the treatment of obstructive sleep apnea. J Otolaryngol Head Neck Surg. 2023;52:7. doi: 10.1186/s40463-023-00621-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scioscia G, Tondo P, Foschino Barbaro MP, Sabato R, Gallo C, Maci F, Lacedonia D. Machine learning-based prediction of adherence to continuous positive airway pressure (CPAP) in obstructive sleep apnea (OSA) Inform Health Soc Care. 2022;47:274–282. doi: 10.1080/17538157.2021.1990300. [DOI] [PubMed] [Google Scholar]
- 8.Li R, Li W, Yue K, Li Y. Convolutional neural network for screening of obstructive sleep apnea using snoring sounds. Biomed Signal Process Control. 2023;86:104966. [Google Scholar]
- 9.Kelly JL, Ben Messaoud R, Joyeux-Faure M, Terrail R, Tamisier R, Martinot JB, Le-Dong NN, Morrell MJ, Pépin JL. Diagnosis of Sleep Apnoea Using a Mandibular Monitor and Machine Learning Analysis: One-Night Agreement Compared to in-Home Polysomnography. Front Neurosci. 2022;16:726880. doi: 10.3389/fnins.2022.726880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jayarathna T, Gargiulo GD, Breen P. Polymer sensor embedded, IOT enabled t-shirt for long-term monitoring of sleep disordered breathing. Proceedings of the 2019 IEEE 5th World Forum on Internet of Things (WF-IoT); 2019 Apr 15-18; Limerick, Ireland: IEEE, 2019: 139-143. [Google Scholar]
- 11.Abdel-Basset M, Ding W, Abdel-Fatah L. The fusion of Internet of Intelligent Things (IoIT) in remote diagnosis of obstructive Sleep Apnea: A survey and a new model. Inform Fusion. 2020;61:84–100. [Google Scholar]
- 12.Bajpai J, Pradhan A, Bajaj D, Verma AK, Kant S, Pandey AK, Sethi R, Dubey A. Prevalence of dyslipidaemia in OSA patients at a tertiary care center. Am J Cardiovasc Dis. 2023;13:1–9. [PMC free article] [PubMed] [Google Scholar]
- 13.Pang B, Doshi S, Roy B, Lai M, Ehlert L, Aysola RS, Kang DW, Anderson A, Joshi SH, Tward D, Scalzo F, Vacas S, Kumar R. Machine learning approach for obstructive sleep apnea screening using brain diffusion tensor imaging. J Sleep Res. 2023;32:e13729. doi: 10.1111/jsr.13729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cleveland Clinic. Neurological Institute Outcomes. [cited 10 July 2023]. Available from: https://my.clevelandclinic.org/departments/neurological/outcomes/1095-cleveland-clinic-sleep-app .
- 15.Nygate Y, Rusk S, Fernandez C, Winzurk Z, Wickwire E, Mignot E, Watson NF. 0574 Artificial Intelligence to Aid in Diagnosis of Type I Narcolepsy. Sleep. 2023;46:A252. [Google Scholar]
- 16.Blanchard M, Feuilloy M, Gervès-Pinquié C, Trzepizur W, Meslier N, Goupil F, Pigeanne T, Racineux JL, Balusson F, Oger E, Gagnadoux F, Girault JM. Cardiovascular risk and mortality prediction in patients suspected of sleep apnea: a model based on an artificial intelligence system. Physiol Meas. 2021;42 doi: 10.1088/1361-6579/ac2a8f. [DOI] [PubMed] [Google Scholar]
- 17.Brink-Kjaer A, Leary EB, Sun H, Westover MB, Stone KL, Peppard PE, Lane NE, Cawthon PM, Redline S, Jennum P, Sorensen HBD, Mignot E. Age estimation from sleep studies using deep learning predicts life expectancy. NPJ Digit Med. 2022;5:103. doi: 10.1038/s41746-022-00630-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arnal PJ, Thorey V, Debellemaniere E, Ballard ME, Bou Hernandez A, Guillot A, Jourde H, Harris M, Guillard M, Van Beers P, Chennaoui M, Sauvet F. The Dreem Headband compared to polysomnography for electroencephalographic signal acquisition and sleep staging. Sleep. 2020;43 doi: 10.1093/sleep/zsaa097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grewal H, Dhillon G, Monga V, Sharma P, Buddhavarapu VS, Sidhu G, Kashyap R. Radiology Gets Chatty: The ChatGPT Saga Unfolds. Cureus. 2023;15:e40135. doi: 10.7759/cureus.40135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kalava A, Ravindranath S, Bronshteyn I, Munjal RS, Schianodicola J, Yarmush JM. Typing skills of physicians in training. J Grad Med Educ. 2014;6:155–157. doi: 10.4300/JGME-D-13-00164.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dhillon G, Grewal H, Monga V, Munjal R, Buddhavarapu VS, Verma RK, Sharma P, Kashyap R. Gender inclusive care toolkit for hospitals. Lancet Reg Health Am. 2023;26:100583. doi: 10.1016/j.lana.2023.100583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goldstein CA, Berry RB, Kent DT, Kristo DA, Seixas AA, Redline S, Westover MB. Artificial intelligence in sleep medicine: background and implications for clinicians. J Clin Sleep Med. 2020;16:609–618. doi: 10.5664/jcsm.8388. [DOI] [PMC free article] [PubMed] [Google Scholar]


