Abstract
BACKGROUND
Cutaneous metastasis with gastric cancer (GC) origin is extremely rare and associated with poor prognosis. Nodular type is the most common type, while other forms are extremely rare.
CASE SUMMARY
This study describes severe skin redness, swelling, pain, and fever in a 65-year-old man diagnosed with GC, whose left chest wall, left upper limb, and left back were mainly affected. Firstly, the patient was diagnosed with “lymphangitis” and treated to promote lymphatic return. However, the symptoms were constantly deteriorating, and skin thickening and scattered small nodules gradually appeared. Finally, the skin biopsy confirmed cutaneous metastases, and the patient died 7 d later.
CONCLUSION
Our case highlights that cutaneous metastasis should be considered when skin lesions appear in patients with GC.
Keywords: Cutaneous metastasis, Gastric cancer, Inflammatory, Sclerodermoid, Nodular, Case report
Core Tip: We describe a 65-year-old man with advanced gastric cancer and multiple metastases. He came to our hospital due to severe skin redness, swelling, pain, and fever in his left chest wall, left upper limb, and left back. He was diagnosed with “lymphangitis” and treated to promote lymphatic return. However, pain and swelling were constantly deteriorating, and skin thickening and scattered small nodules gradually appeared. Finally, the skin biopsy confirmed cutaneous metastases, and he died 7 d later. We review the related literatures and emphasize the importance of skin biopsy in case of any skin lesions.
INTRODUCTION
Gastric cancer (GC) is a highly heterogeneous disease, and the typical sites of metastasis are the liver, lung, bone, and the peritoneum[1]. Cutaneous metastasis of GC is extremely rare, occurring in 0.2% to 1% of cases[2-4]. Cutaneous metastasis usually occurs in the late stage but sometimes appears as the first manifestation[5-9]. Single or multiple nodules are the most common clinical presentations[1,2,5-7,10-12]. In this paper, we report a patient with GC who developed cutaneous metastases with extensive redness and swelling, followed by skin thickening and nodules. The patient died 7 d later after the diagnosis.
CASE PRESENTATION
Chief complaints
A 65-year-old man developed redness and swelling in the left chest wall, left upper limb, and left back in April, 2023.
History of present illness
His symptoms were obvious, accompanied by fever and pain.
History of past illness
The patient was admitted to our hospital in February, 2023, due to left shoulder pain. He had been diagnosed with stage IV poorly differentiated adenocarcinoma of the stomach in May 2022 and received eight cycles of XELOX chemotherapy (oxaliplatin plus capecitabine) in other hospitals. Computed tomography (CT) was performed and showed multiple lymph nodes, bones and liver metastases. He underwent an ultrasound-guided left cervical lymph node puncture biopsy. Pathological examination revealed poorly differentiated adenocarcinoma. Immunohistochemistry showed that cancer cells were positive for CK, CK7, and Villin and negative for Syn, CgA, and CD56. A small number of cells revealed CK20. HER2 was negative (Figure 1A), consistent with the primary GC. Sintilimab and albumin-bound paclitaxel were used as the second-line therapy. Unfortunately, he experienced progression after treatment with immune checkpoint inhibitors. Irinotecan was given as the third-line therapy.
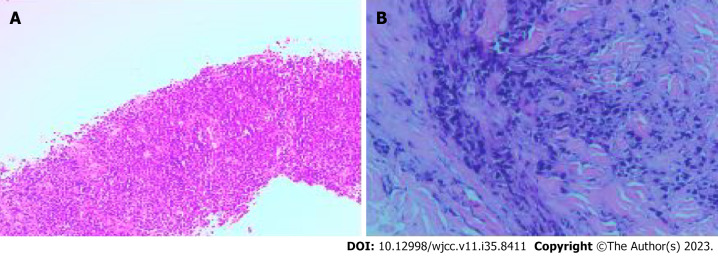
Figure 1.
Pathological findings. Pathological examination revealed poorly differentiated adenocarcinoma. A: Biopsy of cervical lymph node; B: Skin biopsy of the chest wall.
Personal and family history
He had a history of coronary heart disease, but no family history of malignant tumors.
Physical examination
Cutaneous examination revealed the left upper limb, chest wall, and left back edema, with increased skin tension and enlarged pores.
Laboratory examinations
Blood biochemistry tests showed anemia with a hemoglobin level of 95 g/dL and hypoalbuminemia with an albumin level of 28.2 g/L, suggesting poor nutritional status.
Imaging examinations
Ultrasonography revealed subcutaneous edema, but no thrombosis was observed.
MULTIDISCIPLINARY EXPERT CONSULTATION
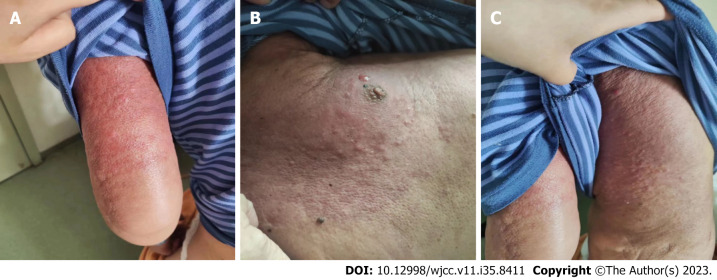
After a multidisciplinary consultation with oncologists, vascular surgeons, and dermatologists, he was diagnosed with “lymphangitis” and treated to promote lymphatic return. However, pain and swelling were constantly deteriorating, and skin thickening and scattered nodules gradually appeared (Figure 2). A skin biopsy was obtained from the left chest wall 7 wk later, and pathological assessment revealed poorly differentiated adenocarcinoma. Immunohistochemical staining showed CK7 (+), Villin (+), CK20 (weak+), CDX2(-), GATA-3(-), GCDFP-15(-), Mammaglobin (-) (Figure 1B), consistent with metastatic GC.
Figure 2.
Cutaneous metastases from gastric cancer. The extensive skin redness and swelling, accompanied by skin thickening and scattered small nodules. This image is published with the patient’s guardian consent. A: Left upper limb; B: Left chest wall; C: Left back.
FINAL DIAGNOSIS
The patient was diagnosed with cutaneous metastases of GC.
TREATMENT
He received hospice care due to the low ECOG performance.
OUTCOME AND FOLLOW-UP
Unfortunately, the patient died 7 d later after the diagnosis of cutaneous metastasis.
DISCUSSION
Cutaneous metastasis occurs in 0.7%-9% of patients with internal cancers[3,13,14], usually originating from breast cancer, lung cancer and colorectal cancer[13,15]. Approximately 70% of cutaneous metastases in women are caused by breast cancer[16]. There are few reports on the cutaneous metastasis of GC. We found 13 cases in the PubMed database between 2014 and 2023 (Table 1). The most common site of cutaneous metastasis in GC is around the umbilicus and mainly occurs in males[2,3,5,13,17], and signet-ring cell carcinoma has a greater tendency[2-5,17].
Table 1.
Thirteen cases of cutaneous metastases of gastric cancer
|
Ref.
|
Year
|
Age
|
Sex
|
Site
|
First symptoms
|
Type
|
SRC
|
Resection
|
Prognosis
|
| Yao et al[2] | 2023 | 61 | M | Groin, scalp, thigh | No | Nodular, inflammatory, sclerodermoid | Yes | No | Unknown |
| Pliakou et al[3] | 2022 | 42 | M | Abdomen, hemithorax, back | No | Inflammatory | Yes | No | Died 4 mo later |
| Bajoghli et al[5] | 2022 | 44 | M | Face, trunk, upper limbs | Yes | Nodular | Yes | No | Unknown |
| Şahin et al[10] | 2021 | 81 | F | Abdomen | No | Nodular | Unknown | No | Died 5 d later |
| Demircioğlu et al[4] | 2021 | 53 | F | Abdomen, thigh | No | Inflammatory | Yes | No | Died 7 mo later |
| He et al[1] | 2019 | 69 | M | Armpit | No | Nodular | Unknown | No | Unknown |
| Koyama et al[11] | 2019 | 89 | M | Armpit | No | Nodular | No | Yes | Over 6 yr |
| Kirchberger[6] | 2018 | 91 | M | Chin | Yes | Nodular | Unknown | No | Died 1 mo later |
| Namikawa et al[7] | 2017 | 59 | M | Chest wall | Yes | Nodular | No | Yes | Died 6 mo later |
| Gündüz et al[12] | 2017 | 57 | F | Face, neck, shoulders | No | Nodular | Yes | No | Unknown |
| Ahmad et al[8] | 2015 | 49 | F | Scalp, face, upper limbs, shoulder, back, chest | Yes | Nodular | No | No | Unknown |
| Kaur et al[9] | 2015 | 55 | M | Abdomen | Yes | Sclerodermoid | Yes | No | Unknown |
| Arslan et al[17] | 2014 | 52 | M | Face, scalp | Yes | Nodular | Yes | No | Unknown |
M: Male; F: Female; SRC: Signet-ring cell.
The mechanisms of cutaneous metastasis are complex and incompletely understood. Some potential mechanisms include hematogenous, lymphatic, direct invasion and surgical implantation[5,15]. Chemokines and their receptors have been demonstrated to be involved in cutaneous metastasis, but previous findings are still controversial[14]. Hematogenous spread is the most likely manner of metastasis in our case due to the widespread nature of metastases.
Cutaneous metastases of GC mainly manifest as nodules or masses[1,5,10,11]. Less frequently, they appear like sclerodermoid or inflammatory lesions[2,3,4,9]. In most cases, the latter two manifestations gradually develop from nodules[2,4]. In this case, we first observed the inflammatory lesions, followed by sclerodermoid lesions and nodules. To our knowledge, this form of progression has not been reported before. The most common site for cutaneous metastasis in GC is the abdomen, known as “Sister Mary Joseph Nodules”, while lesions of the chest wall, back and upper limbs were involved in this case. After being treated for lymphangitis and lymphedema, his symptoms did not alleviate. The diagnosis was not confirmed until a skin biopsy was taken 7 wk later.
Generally, cutaneous metastasis from GC implies that the tumor is inoperable and systemic therapy is needed. So far, only a few cases of resection have been reported[7,11]. Extended survival can be achieved by complete resection of cutaneous metastases when other lesions are well controlled[11]. Sometimes, surgical resection is performed as palliative treatment to relieve symptoms, such as pain[7].
Cutaneous metastasis in GC is generally a sign of poor prognosis[6,10], and the average survival time ranges from 1 to 28 wk in patients with cutaneous metastasis of GC[3,4,7,10]. Compared to nodular forms, inflammatory lesions might mean a worse survival[4]. Our patient died 7 d later after the diagnosis.
CONCLUSION
In conclusion, more attention should be paid to patients with GC who present with any skin lesions. If necessary, a skin biopsy specimen should be obtained to make an accurate and prompt diagnosis.
Footnotes
Informed consent statement: The patient’s family has verbally agreed to the reporting of the case.
Conflict-of-interest statement: All the authors report no relevant conflicts of interest for this article.
CARE Checklist (2016) statement: The authors have read CARE Checklist (2016), and the manuscript was prepared and revised according to CARE Checklist (2016).
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: September 24, 2023
First decision: October 7, 2023
Article in press: December 4, 2023
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Croce MV, Argentina; Iwamuro M, Japan S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
Contributor Information
Lei Tian, Department of Oncology, Hebei General Hospital, Shijiazhuang 050051, Hebei Province, China.
Zhi-Bin Ye, Department of Gastrointestinal Surgery, Hebei General Hospital, Shijiazhuang 050051, Hebei Province, China.
Yun-Lei Du, Department of Emergency, Hebei General Hospital, Shijiazhuang 050051, Hebei Province, China.
Qiao-Fang Li, Department of Oncology, Hebei General Hospital, Shijiazhuang 050051, Hebei Province, China.
Li-Ya He, Department of Oncology, Hebei General Hospital, Shijiazhuang 050051, Hebei Province, China.
Hong-Zhen Zhang, Department of Oncology, Hebei General Hospital, Shijiazhuang 050051, Hebei Province, China. 931848183@qq.com.
References
- 1.He FJ, Zhang P, Wang MJ, Chen Y, Zhuang W. Left armpit subcutaneous metastasis of gastric cancer: A case report. World J Clin Cases. 2019;7:4137–4143. doi: 10.12998/wjcc.v7.i23.4137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yao S, Zhou P, Li Y, Li Q. Case report: A case of delayed cutaneous metastases from signet-ring cell mixed-type gastric cancer. Front Oncol. 2023;13:1105080. doi: 10.3389/fonc.2023.1105080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pliakou E, Lampropoulou DI, Nasi D, Aravantinos G. Skin metastases from gastric cancer, a rare entity masquerading as erysipelas: A case report. Mol Clin Oncol. 2022;16:110. doi: 10.3892/mco.2022.2543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Demircioğlu D, Öztürk Durmaz E, Demirkesen C, Şahin S. Livedoid cutaneous metastasis of signet-ring cell gastric carcinoma. J Cutan Pathol. 2021;48:785–788. doi: 10.1111/cup.13969. [DOI] [PubMed] [Google Scholar]
- 5.Bajoghli AA, Piselli A, Kemprecos H, Khosravi H, Cardis MA, Noel MS. Gastric carcinoma's primary presentation as multiple cutaneous nodules throughout the body. Cancer Treat Res Commun. 2022;31:100532. doi: 10.1016/j.ctarc.2022.100532. [DOI] [PubMed] [Google Scholar]
- 6.Kirchberger MC. Unusual presentation of a cutaneous metastasis in the face arising from gastric cancer: a case report. SAGE Open Med Case Rep. 2018;6:2050313X18795080. doi: 10.1177/2050313X18795080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Namikawa T, Munekage E, Munekage M, Maeda H, Yatabe T, Kitagawa H, Kobayashi M, Hanazaki K. Subcutaneous metastasis arising from gastric cancer: A case report. Mol Clin Oncol. 2017;6:515–516. doi: 10.3892/mco.2017.1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahmad B, Pierson N, Adnan MM, Phan M, Jenkins J, Pant S, Cherry M, Khawandanah M. Distant skin metastases as primary presentation of gastric cancer. J Community Support Oncol. 2015;13:156–158. doi: 10.12788/jcso.0127. [DOI] [PubMed] [Google Scholar]
- 9.Kaur S, Aggarwal P, Dayal S, Sangwan A, Jain VK, Jindal N. Cutaneous Metastasis from Signet-ring Gastric Adenocarcinoma in a Carcinoma En Cuirasse Pattern: An Unusual Clinical-diagnostic Sequence. Indian J Dermatol. 2015;60:637. doi: 10.4103/0019-5154.169162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Şahin M, Ekinci F, Çelik C, Temiz P, Erdoğan AP, Göksel G. A Rare Case Report of Skin Metastasis in Gastric Cancer. J Gastrointest Cancer. 2021;52:1156–1158. doi: 10.1007/s12029-021-00603-3. [DOI] [PubMed] [Google Scholar]
- 11.Koyama R, Maeda Y, Minagawa N, Shinohara T, Hamada T. Late Cutaneous Metastasis Originating from Gastric Cancer with Synchronous Metastasis. Case Rep Gastroenterol. 2019;13:95–101. doi: 10.1159/000497099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gündüz Ö, Emeksiz MC, Atasoy P, Kidir M, Yalçin S, Demirkan S. Signet-ring Cells in the Skin: A Case of Late-onset Cutaneous Metastasis of Gastric Carcinoma and a Brief Review of Histological Approach. Dermatol Reports. 2016;8:6819. doi: 10.4081/dr.2016.6819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schadt CR. The cutaneous manifestations of gastrointestinal malignancy. Semin Oncol. 2016;43:341–346. doi: 10.1053/j.seminoncol.2016.02.028. [DOI] [PubMed] [Google Scholar]
- 14.Hu SC, Chen GS, Wu CS, Chai CY, Chen WT, Lan CC. Rates of cutaneous metastases from different internal malignancies: experience from a Taiwanese medical center. J Am Acad Dermatol. 2009;60:379–387. doi: 10.1016/j.jaad.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 15.Nienhaus A, Rajakulendran R, Bernad E. Cutaneous Metastasis of Endometrial Cancer and Long-Term Survival: A Scoping Review and Our Experience. Diagnostics (Basel) 2023;13 doi: 10.3390/diagnostics13152603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tabak GH, Akdogan N, Ates Ozdemir D. Cutaneous metastasis of breast carcinoma presenting as milia-en-plaque. J Cosmet Dermatol. 2022;21:1297–1299. doi: 10.1111/jocd.14167. [DOI] [PubMed] [Google Scholar]
- 17.Arslan D, Uysal M, Tatlı AM, Gunduz S, Goksu SS, Başsorgun Cİ, Coskun HS, Bozcuk H, Savaş B. Her-2 positive gastric cancer presented with thrombocytopenia and skin involvement: a case report. Case Rep Oncol Med. 2014;2014:194636. doi: 10.1155/2014/194636. [DOI] [PMC free article] [PubMed] [Google Scholar]