Extract
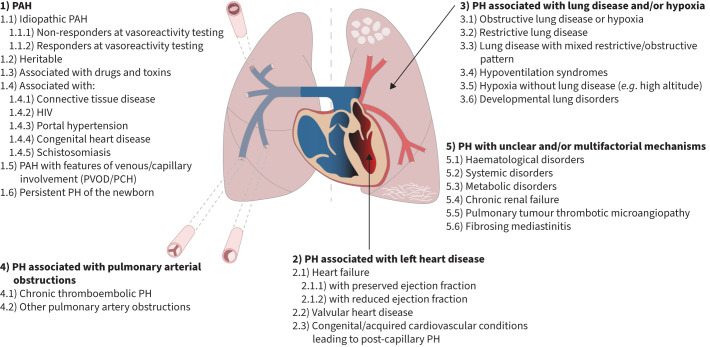
Pulmonary hypertension (PH) is defined as the presence of a mean pulmonary arterial pressure >20 mmHg [1]. This simple haemodynamic definition encompasses a heterogenous collection of conditions. It is now appreciated that although treatable forms of PH are relatively rare, PH itself is not an uncommon entity, affecting ∼1% of the global population [1]. Current international guidelines describe five classification groups: group 1 (pulmonary arterial hypertension (PAH)), group 2 (PH associated with left heart disease), group 3 (PH associated with lung disease), group 4 (PH associated with pulmonary arterial obstructions) and group 5 (PH with unclear and/or multifactorial causes) figure 1 [1]. These groups are characterised by shared clinical, haemodynamic and radiological features which are underpinned by common histopathological changes.
Tweetable abstract
This editorial introduces a new European Respiratory Review series focusing on clinical, radiological and histopathological features in pulmonary hypertension. https://bit.ly/3RtiFVK
Pulmonary hypertension (PH) is defined as the presence of a mean pulmonary arterial pressure >20 mmHg [1]. This simple haemodynamic definition encompasses a heterogenous collection of conditions. It is now appreciated that although treatable forms of PH are relatively rare, PH itself is not an uncommon entity, affecting ∼1% of the global population [1]. Current international guidelines describe five classification groups: group 1 (pulmonary arterial hypertension (PAH)), group 2 (PH associated with left heart disease), group 3 (PH associated with lung disease), group 4 (PH associated with pulmonary arterial obstructions) and group 5 (PH with unclear and/or multifactorial causes) figure 1 [1]. These groups are characterised by shared clinical, haemodynamic and radiological features which are underpinned by common histopathological changes. Pre-capillary PH (defined by a pulmonary arterial wedge pressure ≤15 mmHg and a pulmonary vascular resistance >2 Wood units (WU)) may result from remodelling, obstruction or loss of the pulmonary arterial bed while post-capillary PH (defined by a pulmonary arterial wedge pressure >15 mmHg) results from passive backwards transmission of elevated left heart filling pressures into the pulmonary circulation (isolated post-capillary PH) [2]. Some patients with post-capillary disease may develop subsequent pulmonary vascular remodelling with a subsequent increase in pulmonary vascular resistance to >2 WU (combined pre- and post-capillary PH). Three main classes of PAH therapies have been shown to be of benefit in group 1 disease (targeting the nitric oxide, endothelin-1 and prostacyclin pathways) while chronic thromboembolic PH can be effectively treated with pulmonary endarterectomy surgery together with important roles for balloon pulmonary angioplasty and pulmonary vasodilators [3, 4]. The optimal treatment in the majority of patients in groups 2, 3 and 5 is less well defined. Recent advances in our understanding of the histopathological changes in different forms of PH have the potential to further inform classification and patient management [5].
FIGURE 1.
Clinical classification of pulmonary hypertension (PH). PAH: pulmonary arterial hypertension; PVOD: pulmonary veno-occlusive disease; PCH: pulmonary capillary haemangiomatosis. Reproduced and modified from Kiely et al. [11] with permission, with updated classification reproduced from Humbert et al. [1] with permission.
It is, therefore, vital that clinicians who diagnose and manage patients with PH have a good understanding of the histopathological basis and radiological features associated with these different forms of PH. To this end, a series of reviews focusing on four of these diagnostic groups plus a bonus review specifically covering PAH with features of venous/capillary involvement (pulmonary veno-occlusive disease and pulmonary capillary hemangiomatosis) begins in this issue of the European Respiratory Review [6–10]. In these review articles, key histopathological and radiological patterns are explored using illustrative clinical case studies with particular attention being paid to the development of a systematic approach to radiological interpretation. It is hoped that the series will be an invaluable resource for all clinicians involved in the care of patients with PH.
Footnotes
Provenance: Commissioned article, peer reviewed.
Conflicts of interests: R. Condliffe reports consulting fees from Janssen and MSD, lecture fees and support for attending meetings and/or travel from Janssen, and participation on a data safety monitoring board or advisory board with Boston Scientific. A. Vonk Noordegraaf has received speaker fees for lectures and educational events from Janssen, MSD and United Therapeutics/Ferrer, and has received consulting fees from Janssen, MSD and United Therapeutics/Ferrer. The remaining authors declare no conflicts of interest related to this manuscript.
References
- 1.Humbert M, Kovacs G, Hoeper MM, et al. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Respir J 2023; 61: 2200879. doi: 10.1183/13993003.00879-2022 [DOI] [PubMed] [Google Scholar]
- 2.Vachiéry JL, Tedford RJ, Rosenkranz S, et al. Pulmonary hypertension due to left heart disease. Eur Respir J 2019; 53: 1801897. doi: 10.1183/13993003.01897-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Galiè N, Channick RN, Frantz RP, et al. Risk stratification and medical therapy of pulmonary arterial hypertension. Eur Respir J 2019; 53: 1801889. doi: 10.1183/13993003.01889-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim NH, Delcroix M, Jais X, et al. Chronic thromboembolic pulmonary hypertension. Eur Respir J 2019; 53: 339–351. doi: 10.1183/13993003.01915-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Humbert M, Guignabert C, Bonnet S, et al. Pathology and pathobiology of pulmonary hypertension: state of the art and research perspectives. Eur Respir J 2019; 53: 1801887. doi: 10.1183/13993003.01887-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Condliffe R, Durrington C, Hameed A, et al. Clinical–radiological–pathological correlation in pulmonary arterial hypertension. Eur Respir Rev 2023; 32: 230138. doi: 10.1183/16000617.0138-2023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lechartier B, Boucly A, Solinas S, et al. Pulmonary veno-occlusive disease: illustrative cases and literature review. Eur Respir Rev 2023; in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van de Veerdonk MC, Roosma L, Trip P, et al. Clinical–imaging–pathological correlation in pulmonary hypertension associated with left heart disease. Eur Respir Rev 2023; in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Verbelen T, Godinas L, Dorfmüller P, et al. Clinical–radiological–pathological correlation in chronic thromboembolic pulmonary hypertension. Eur Respir Rev 2023; 32: 230149. doi: 10.1183/16000617.0149-2023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lichtblau M, Mayer L, Gopalan D, et al. Clinical–radiological–pathological correlation in pulmonary hypertension with unclear and/or multifactorial mechanisms. Eur Respir Rev 2023; 32: 230119. doi: 10.1183/16000617.0119-2023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kiely DG, Elliot CA, Sabroe I, et al. Pulmonary hypertension: diagnosis and management. BMJ 2013; 346: f2028. doi: 10.1136/bmj.f2028 [DOI] [PubMed] [Google Scholar]