Abstract
COPD is a highly prevalent, chronic and irreversible obstructive airway disease without curative treatment. Standard therapeutic strategies, both non-pharmacological and pharmacological, have only limited effects on lung function parameters of patients with severe disease. Despite optimal pharmacological treatment, many patients with severe COPD still have a high burden of dyspnoea and a poor quality of life. If these patients have severe lung emphysema, with hyperinflation as the driver of symptoms and exercise intolerance, lung volume reduction may be an effective treatment with a significant impact on lung function, exercise capacity and quality of life. Currently, different lung volume reduction approaches, both surgical and bronchoscopic, have shown encouraging results and have been implemented in COPD treatment recommendations. Nevertheless, choosing the optimal lung volume reduction strategy for an individual patient remains challenging. Moreover, there is still room for improving durability of effect and safety in all available procedures. Ongoing and innovative research is essential to push this field forwards. This review provides an overview of results and limitations of the current lung volume reduction options for patients with severe lung emphysema and hyperinflation.
Tweetable abstract
Results of lung volume reduction in emphysema patients with hyperinflation range from encouraging to convincing. Overall, the effect on pulmonary function is beyond that of other treatments. Nevertheless, further improvement and innovation are needed. https://bit.ly/3Zt0hPh
Introduction
In COPD, an environmental insult such as tobacco smoke induces a complex chronic inflammatory reaction in a susceptible host. This inflammation can affect (small) airways (chronic bronchitis) and lung parenchyma (emphysema), leading to chronic irreversible airflow limitation. COPD now affects more than 300 million people worldwide with a huge burden on both the patient's quality of life (QoL) and healthcare systems [1, 2].
Because COPD is a very heterogeneous disease, recognising the patient’s phenotype is crucial in allowing the right treatment to be offered to the right patient. In clinical practice, most patients present with characteristics of both lung emphysema and (small) airway disease, in combination with interfering comorbidities. These patients deserve a thorough assessment by the pulmonologist to recognise the treatable traits by which they are most limited. Despite proven beneficial effects of well-known pharmacological and non-pharmacological treatments in COPD, patients remain symptomatic with a high burden of dyspnoea, which impacts exercise capacity and QoL. COPD cannot be cured and the effect of pharmacological treatment on pulmonary function is rather limited. Although current survival after lung transplantation (LTX) in COPD is encouraging [3], the prevalence of severe COPD far exceeds the scarce availability of suitable donor lungs. Furthermore, many patients are not eligible for major surgery or lifelong immunosuppressants owing to advanced age or comorbidities. Therefore, in the emphysematous COPD patient population, the quest for bronchoscopic and surgical techniques that could improve lung function is very relevant. The first surgical interventions were being performed on patients with lung emphysema by the 1950s [4]. In the last decades, an evolution in surgical techniques and the development of innovative bronchoscopic interventions has brought us new, and often successful, treatment options for patients with COPD.
The aim of this review is to discuss all relevant aspects of both surgical and bronchoscopic strategies for emphysema patients with hyperinflation. We performed a search for studies on lung volume reduction surgery (LVRS) and bronchoscopic lung volume reduction (BLVR) in PubMed. Articles with “lung volume reduction”, “lung volume reduction surgery” or “bronchoscopic lung volume reduction” in the title or abstract were screened, if published in English. Clinical trials, observational studies and retrospective analyses were included. Relevant references cited in those articles were reviewed.
Lung volume reduction
In emphysema patients, airway obstruction and loss of elastic recoil cause expiratory airflow limitation, leading to an increase in end-expiratory volumes (so called air trapping), resulting in a reduced inspiratory capacity. This phenomenon is called hyperinflation and is aggravated during exercise, when expiration time shortens. Hyperinflation increases dyspnoea and affects the mechanics of the respiratory muscles. Severe hyperinflation is also associated with worse survival in COPD [5].
Lung volume reduction (LVR) may be an efficacious treatment for patients with hyperinflation due to emphysema. The rationale of this treatment is to reduce residual volume (RV), thereby increasing inspiratory capacity, elastic recoil, airway tethering and expiratory airflow [6]. Moreover, reduction of lung volume improves the mechanics of respiratory muscles, particularly the diaphragm [7, 8]. LVRS was introduced in 1957, with the aim of mitigating hyperinflation by resecting the most destroyed area of the lung [4]. From the early 2000s, different BLVR techniques have been studied to obtain comparable effects. Subsequent improvements in technique and patient selection have led to LVR becoming a valuable treatment with significant improvements in lung function, exercise capacity and QoL [9–12]. A meta-analysis of different LVR strategies showed a mean increase in forced expiratory volume in 1 s (FEV1) of 16%, a mean reduction in RV of −580 mL, an improvement of 6-min walk distance (6MWD) of 43 m and a reduction in St George's Respiratory Questionnaire (SGRQ) (a measure of QoL) of 9 points [13]. These effects, on top of maximal COPD treatment, are revolutionary compared to the pharmacological treatment of COPD. Moreover, LVR treatment shows a significant survival benefit in patients with heterogeneous emphysema who have low exercise capacity (LVRS compared to standard of care) [12]. In comparisons of responders with non-responders of endobronchial valve (EBV) treatment, responders showed better survival in several publications [14, 15]. Furthermore, the median survival of patients treated with EBV or coils is significantly longer when compared to untreated patients [16]. Nevertheless, these are results from observational and retrospective analyses; no randomised controlled trial (RCT) on BLVR has investigated survival as an outcome measure.
Lung volume reduction surgery
History and results
Before Brantigan et al. [4] introduced the new therapeutic option of LVRS in 1957, various surgical procedures had been proposed to treat emphysema. Costochondrectomy was proposed when emphysema was thought to be a consequence of a primary skeletal deformity [17]. Thoracoplasty, phrenic paralysis and pulmonary denervation were undertaken to reduce the volume of the enlarged lung [18–20]. The outcomes were poor, with very infrequent success. Brantigan et al. [4] suggested that lowering the volume of an emphysematous lung by removing functionally worthless areas would enhance respiratory mechanics and the lung's outward traction to keep the small airways open. Staged bilateral thoracotomy was performed, but because of a perioperative mortality of 16% and the lack of data demonstrating subjective improvement in survivors, his work was abandoned. In the early 1990s, Cooper et al. [21] introduced the dawn of a new era when they proposed a modification of the technique described by Brantigan et al. [4], using median sternotomy (bilateral LVRS) in 20 patients with heterogeneous non-bullous emphysema. They reported no perioperative mortality and an FEV1 improvement of 82% at 6 months, associated with marked relief of dyspnoea and improvement in QoL [21]. Re-evaluation of this modified technique by Cooper et al. [21] in 150 consecutive patients demonstrated an increase in FEV1 of 51%, perioperative mortality in six patients (4%) and continuing improvement in QoL [22]. A smaller Canadian case series on bilateral LVRS via median sternotomy was also promising [23]. Unilateral video-assisted thoracic surgery (VATS) with stapled resection to treat heterogenous emphysema was described in 1996 in Pittsburgh, PA, USA, by Keenan et al. [24]. In Zürich, Switzerland, Weder started a bilateral LVRS VATS programme in 1993 and his group reported the initial results from 1994 to 1995 with no perioperative mortality, a 41% improvement of FEV1, an increase in walking distance (12 min: 495 m to 688 m, p<0.001) and a substantial relief of dyspnoea at 3 months [25].
These results inspired many centres to implement their own LVRS programme and called for a randomised trial, the National Emphysema Treatment Trial (NETT), performed in North America evaluating the efficacy of LVRS on QoL and survival benefit in comparison to medical treatment [26]. The results were published in 2003, reporting significantly higher 90-day mortality for the surgical group compared to medical treatment (7.9% versus 1.3%, p<0.001). A sub-analysis of the surgical cohort defined a high-risk population. This patient group, with FEV1 <20% and either a diffusing capacity of the lung for carbon monoxide (DLCO) <20% or homogenous morphology on computed tomography (CT), experienced high mortality (16%) [27]. Further analysis of the NETT data for LVRS patients with heterogeneous emphysema (predominantly upper lobe) and low baseline exercise capacity demonstrated significant improvements in survival (up to 5 years), exercise capacity (up to 3 years) and QoL (up to 5 years) [12]. Out of the 1218 patients included in the NETT, VATS was used in only 30% of cases. This large multicentre and RCT proved on a high evidence-based level that LVRS is very effective in selected patients, but unfortunately led to misconceptions and misinterpretations about the safety and efficacy of the procedure. The major shortcoming was the lack of multidisciplinary evaluation to select the right patients.
Apart from in hospitals with extensive expertise, confidence in this intervention was generally lost and LVRS is still nowadays underperformed. However, results from high-volume centres that continue to perform SLVR demonstrate a low mortality rate (ranging from 0% at 6 months to 4% in-hospital) and significant and maximal functional improvement (spirometry, dyspnoea scores and QoL) from 3 months up to 5 years after LVRS [28–30].
Over the last years, several single-centre trials in expert centres have investigated expanding indications in patients with a suitable morphology or hyperinflation. In a retrospective analysis of prospectively collected, single-centre data from Zürich, 138 out of 250 patients had a more homogenous morphology of emphysema. In this subgroup, similar to heterogenous patients, significant improvement of FEV1 (+35%) and 6MWD (+79 m) at 3 months were shown, with no differences in perioperative and 1-year mortality [29, 31]. Additionally, in experienced centres, LVRS can cautiously be considered in a subgroup of highly selected patients with severely impaired diffusion capacity (DLCO <20%) and the presence of major hyperinflation and heterogeneous emphysema. In a retrospective analysis of 33 patients, good results were achieved at 3 months with a significant increase in FEV1 (23% to 29%) and DLCO (15% to 20%) and no mortality at 3 months [32]. Subgroups of patients presenting with mild to moderate pulmonary hypertension (systolic pulmonary arterial pressure (sPAP) >35 mmHg, median sPAP 41 mmHg) could also potentially benefit from LVRS, and it should no longer be considered an absolute contraindication [33]. Given that endothelial function and blood pressure have been found to improve 3 months after LVRS, the procedure may have a positive impact on cardiovascular outcomes as well [34].
Patient selection
Patient selection is crucial to prevent mortality and morbidity and to achieve long-term benefits from LVR. A case-by-case evaluation by a multidisciplinary team is mandatory [35]. Eligibility criteria are similar for bronchoscopic and surgical LVR and, like the contraindications, are generally based on expert recommendations rather than hard scientific evidence. Candidates should have severe emphysema with severe hyperinflation, have quit smoking and be under optimal pharmacological and non-pharmacological treatment. Comorbidities and contraindications should be checked for (figure 1, table 1). Neither age nor body mass index (BMI) are absolute contraindications, but patients should be fit enough for surgery and these variables should be taken into consideration because they are risk factors for developing postoperative complications. Specifically for LVRS, cardiac assessment should be performed to exclude coronary disease, pulmonary hypertension and right ventricular dysfunction (to be confirmed by right heart catheterisation if cardiac ultrasound is considered unreliable). Patients are expected to be sufficiently motivated to undergo surgical treatment and be willing to join a pulmonary and physical rehabilitation programme and understand the risks associated with LVRS. Therefore, patients should be informed of the pathophysiology of emphysema to understand the purpose of the reduction surgery as well as the expected changes postoperatively.
FIGURE 1.
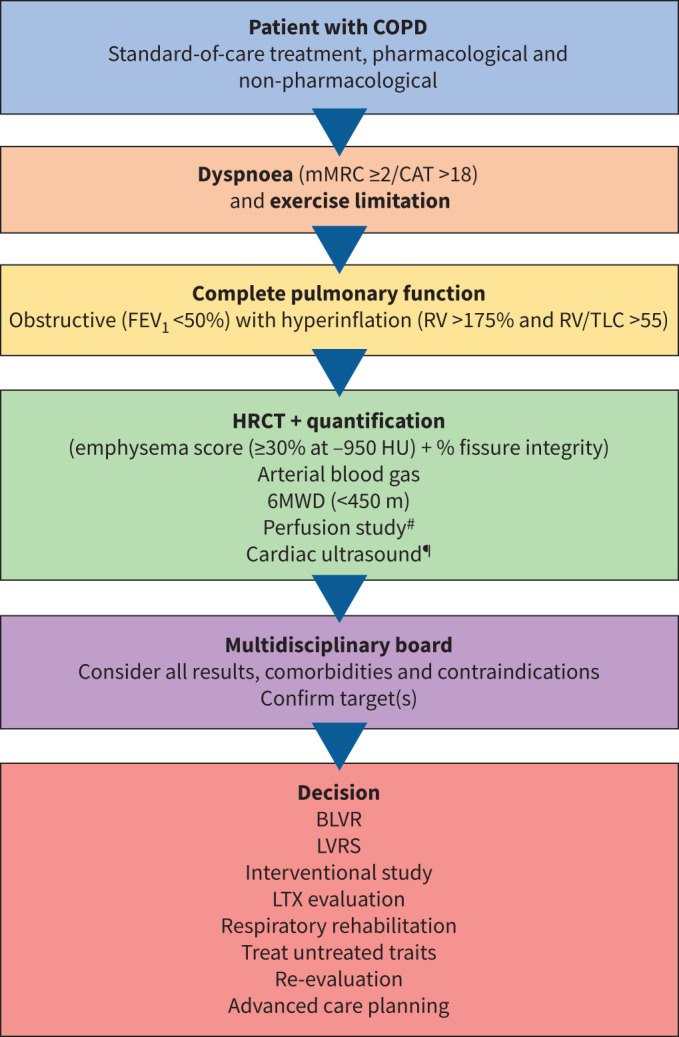
Clinical decision flow in selecting patients for lung volume reduction. mMRC: modified Medical Research Council dyspnoea scale; CAT: COPD Assessment Test; FEV1: forced expiratory volume in 1 s; RV: residual volume; TLC: total lung capacity; HRCT: high-resolution computed tomography; HU: Hounsfield units; 6MWD: 6-min walk distance; BLVR: bronchoscopic lung volume reduction; LVRS: lung volume reduction surgery; LTX: lung transplantation. #: perfusion study is recommended in homogeneous emphysema or difficult target selection; ¶: consider cardiac ultrasound if history of cardiac disease, clinical suspicion of heart failure or pulmonary hypertension and in candidates for LVRS.
TABLE 1.
Contraindications for lung volume reduction
| Recommended contraindications for lung volume reduction procedures |
| DLCO or FEV1 <20% predicted# |
| 6MWD <100 m |
| PaCO2 >60 mmHg or PaO2 <45 mmHg at room air or >3 L·min−1 O2 supplementation |
| Frequent exacerbations and/or bronchiectasis or infection (Aspergillus fumigatus, NTM etc.) |
| Other pulmonary disease: ILD, ABPA, SAD or bronchiolitis without emphysema |
| Pulmonary hypertension with invasively measured sPAP >45 mmHg# |
| Immunosuppression or maintenance oral corticosteroids prednisolone >10 mg·day−1 |
| Heart failure with left ventricle ejection fraction <40% |
| Therapeutic anticoagulation which cannot be interrupted |
| Active malignancy or need for follow-up of nodule |
| Life expectancy <3 months |
| Inability to increase physical activity |
| BMI <18 or >35 kg·m−2# |
| Specific for bronchoscopic lung volume reduction with endobronchial valves |
| History of pleurodesis, lobectomy or LVRS |
| Paraseptal emphysema, pleural adhesions |
DLCO: diffusion capacity of the lung for carbon monoxide; FEV1: forced expiratory volume in 1 s; 6MWD: 6-min walk distance; PaCO2: arterial carbon dioxide tension; PaO2: arterial oxygen tension; NTM: nontuberculous mycobacteria; ILD: interstitial lung disease; ABPA: allergic bronchopulmonary aspergillosis; SAD: small airway dysfunction; sPAP: systolic pulmonary arterial pressure; BMI: body mass index; LVRS: lung volume reduction surgery. #: no absolute contraindication, case-by-case discussion depending on individual patient characteristics and type of intervention. Reports on interventions in patients with poor lung function or hypercapnia have been published [32, 36–40] and for endobronchial valves experts recommend a cut-off of 50 mmHg for sPAP.
Surgical technique
Surgery offers a unique volume-oriented strategy because the resection has the intrinsic advantage of resecting several target zones while leaving the better-preserved lung parenchyma unaltered and the shape of the lung intact (figure 2). Identifying the target zones is a primary objective in conducting LVRS because the hyperinflation morphology of every patient is unique.
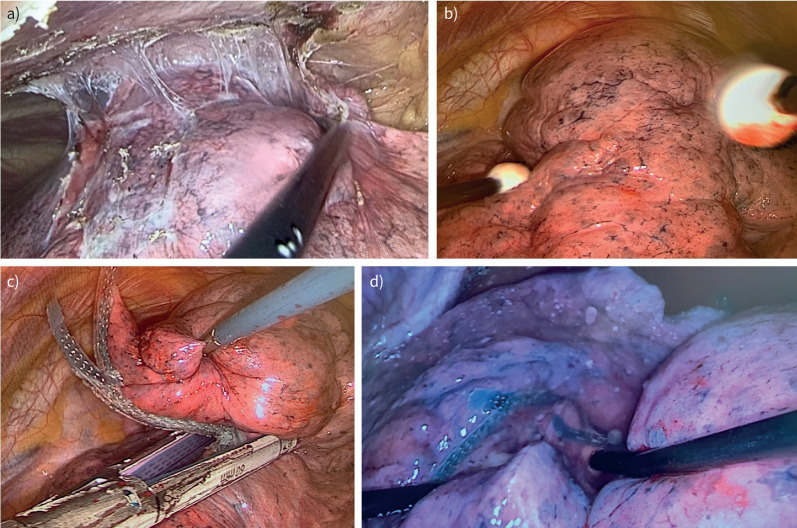
FIGURE 2.
Intraoperative images visualising the crucial steps of lung volume reduction surgery through video-assisted thoracic surgery. a) Release of all adhesions by preserving the visceral pleura. b) Minimal touch shaping of the volume intended to be resected, based on the preoperative computed tomography assessment, preserving the shape of the lung. c) Buttressed stapling of the voluminous target area. d) Underwater test to rule out air leak post-intervention.
Several techniques have been described for LVRS and the choice of technique currently still depends on the experience of the institution and the surgeon. Nowadays it is preferably performed by minimally invasive VATS and consists of unilateral or bilateral LVRS by stapling (figure 2). In patients with bilateral target zones, bilateral LVRS is preferred over unilateral LVRS because the functional benefits achieved are of a greater dimension than those achieved with the unilateral procedure [41]. Moreover, a staged bilateral procedure can lower postoperative morbidity and can improve functional results for up to 6 years [42–44]. A series of wedge excisions in regions with the most pronounced emphysematous alterations is performed. If the tissue is severely destroyed, buttressed staplers are recommended (polyglycolic acid) (figure 2) [45, 46]. Usually, between 20% and 35% of each lung (2–3 L in total) is removed, depending on the volume excess in total lung capacity.
While resectional LVRS is still the gold standard for most thoracic surgeons, non-resectional LVR is also described. The technique is performed by plicating the most emphysematous lung regions and using non-cutting stapling [47, 48]. The main hypothesis is to minimise air leaks by avoiding discontinuation of the pleura and buttressing the staple line, leaving the non-resected tissue as coverage over the manipulated area. Surgery can be carried out through general or epidural anaesthesia. In a single-centre, randomised trial, non-resectional (awake) LVRS was compared with resectional (non-awake) LVRS (32 versus 31 patients, respectively) and resulted in a significantly shorter hospital stay in the awake, non-resectional patients (6 versus 7.5 days) with similar lung function improvements at 6 months [49]. However, the bias of comparing two different techniques in different settings (awake/non-awake) must be recognised. Additionally, when not resecting lung tissue, the risk of infection and resultant malignancies must be considered. Other prospectively collected multicentre data are needed to confirm the potential benefits of non-resectional and awake surgery. Experience with awake thoracic surgery is increasing worldwide, with the primary objective of improving outcomes by avoiding side-effects associated with general anaesthesia and one-lung ventilation (pneumonia, bronchospasm, lung injury related to ventilation) [48]. However, non-awake LVRS can only be performed after thorough patient selection. Patients with radiological evidence of extensive pleural adhesions, contraindications for epidural anaesthesia and who are uncomfortable with the idea of being awake during surgery are prohibited. Technically demanding cases are preferably performed under general anaesthesia because maintaining diaphragmatic motion and cough reflexes can hinder surgical manipulation.
Some points of note when performing LVRS are the position of the thoracic ports in relation to the target zones; uniportal and multiportal approaches are valid. Lung manipulation should be performed in a “no-touch” fashion with maximal care to avoid air fistulas (figure 2). If in doubt of an air leak, the lung can be submerged under water while restarting ventilation (figure 2). A polyglycolic acid sheet (Neoveil sheet; Gunze Kyoto, Japan) or coverage with Progel Pleural Air Leak Sealant (Becton Dickinson and Company, Franklin Lakes, NJ, USA) along the staple lines can be used to decrease the risk of parenchymal tears in the remaining lung after re-expansion [46, 50, 51]. When restarting mechanical ventilation, aggressive recruitment should be avoided [45].
The implementation of three-dimensional visualisation during surgery or robotic surgery could be a future goal, given that LVRS targets the most destroyed areas identified on preoperative imaging [52].
An enhanced recovery programme (ERP) for LVRS is advised, with the main objective of returning the patient to a normal functional status as quickly as possible. This could be adapted from other thoracic ERPs, e.g. for VATS lobectomy. Good preoperative information on the patient, safe and short surgery (avoiding air leaks), adequate pain management, fast recovery with early extubation and avoidance of admission to the intensive care unit, and early ambulation and physiotherapy are all key elements of such an ERP.
Complications
The NETT trial reported rates of pulmonary morbidity (tracheostomy, pneumonia, re-intubation, ventilator use) of 30% and cardiovascular morbidity (arrhythmia requiring treatment, myocardial infarction, pulmonary embolus) of 20% in the non-high-risk population (511 patients) [53].
The main complication of LVRS remains air leak, which can be explained by tearing of the remaining emphysematous non-resected lung. This was observed in the NETT in 90% of patients within 30 days of LVRS, of which 3.3% required surgical re-intervention [54]. Identified risk factors for air leak are upper-lobe disease (p=0.04), important pleural adhesions (p=0.007) and use of inhaled steroids (p=0.004) [54].
In a separate cohort of bilateral LVRS through median sternotomy (n=250), prolonged air leak (≥7 days) was present in 45.2% of cases, of which 3.2% required re-intervention [30]. Furthermore, pulmonary infections and cardiac arrhythmias can occur. Surgical mortality was initially reported in the NETT to be around 5% at 90 days (non-high-risk population) but has decreased to ≤0.5% in experienced centres including our own (UZ Leuven; January 2019–May 2023: 0.6% 30-day mortality) [30, 55, 56].
Mortality and morbidity have been compared between different LVRS approaches in a series of 104 LVRS procedures (2000–2012; 81 unilateral, 23 bilateral) [57]. No deaths were reported in the unilateral cohort versus 17.3% in the bilateral cohort. Major cardiovascular and pulmonary morbidity occurred in 13% versus 6.3% (versus 20% in NETT) and 39.1% versus 11.4% (versus 29.8% in NETT) in unilateral versus bilateral approaches, respectively. Similar functional results were attained. Although this single-centre study suggests that unilateral LVRS can have benefits over bilateral procedures, the functional benefits of bilateral LVRS in patients with bilateral disease should not be underestimated. A retrospective comparison is also sensitive to bias because there could be several reasons to convert a planned bilateral approach to a unilateral procedure. A staged bilateral approach can therefore be considered, with the timing of the contralateral procedure dependent on evidence of deterioration in improvement after the first procedure, to reduce postoperative complications of a one-staged bilateral approach [43].
Bronchoscopic lung volume reduction
Airway bypass
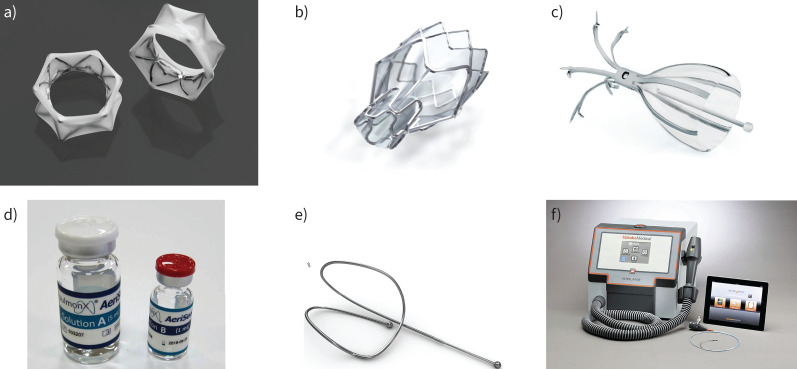
Some of the first bronchoscopic experiments to reduce lung volume in patients with severe emphysema were attempts to deflate the hyperinflated regions by transbronchial stents [58–60]. The EASE trial was a randomised, double-blind, sham-controlled study which included patients with severe, homogeneous emphysema and severe hyperinflation [61]. Drug-eluting (paclitaxel) stents (figure 3) were used to maintain passageway. One to six stents were placed with a maximum of two stents per lobe based on radiological emphysema assessment and anatomy [62]. At day 1, a significant difference in forced vital capacity, RV and FEV1 was measured in treated versus sham patients; unfortunately, the effect was not maintained at 1 month. The trial failed to show improvement of lung function and modified Medical Research Council dyspnoea score at a 6-month follow-up (table 2). This was mainly attributed to a failure to maintain stent patency. Safety was acceptable, and we learned from this trial that complex bronchoscopic interventions under general anaesthesia are safe, even in these vulnerable patients. Along with transbronchial artificial airways, transthoracic approaches have also been explored [76, 77]. Unfortunately, rapid occlusion of these artificial airways has impeded further clinical research. New bronchial stents, called implantable artificial bronchus, are under clinical investigation (NCT05087641).
FIGURE 3.
Overview of the bronchoscopic lung volume reduction devices used in randomised controlled trials. a) A transbronchial airway stent (Exhale Drug-Eluting Stent; Broncus Technologies, Mountain View, CA, USA; reproduced with permission from [62]), b) Zephyr Endobronchial Valve (reproduced with the permission of Pulmonx Corporation, Redwood City, CA, USA), c) Spiration Valve System (reproduced with the permission of Olympus, Redmond, WA, USA), d) AeriSeal Sealant (reproduced with the permission of Pulmonx Corporation, Redwood City, CA, USA), e) lung volume reduction coil (RePneu; PneumRx Inc., Mountain View, CA, USA; reproduced with permission from [63]), f) InterVapor System for thermal vapour ablation (reproduced with the permission of BTVA, Uptake Medical Technology Inc., Seattle, WA, USA).
TABLE 2.
Overview of randomised controlled trials on bronchoscopic lung volume reduction
| Trial | Design | Treated (n) | Emphysema and CV | Follow-up (months) | FEV1 | RV | 6MWD | SGRQ | Advantage | Risk | ||||
| % | R (%) | mL | R (%) | m | R (%) | Points | R (%) | |||||||
| Drug-eluting transbronchial stent | ||||||||||||||
| EASE, 2011 [61] | Multicentre double-blind, sham-controlled, 2:1 | 208 | Homogeneous | 6 | −1.5# | / | −61# | / | −7# | / | −2# | / | Possible in CV+ Large short-term effect | Low stent patency Severe respiratory adverse events |
| EBV: Pulmonx | ||||||||||||||
| VENT, 2010 [64] | Multicentre, 2:1 | 220 | Heterogeneous No fissure or CV assessment | 6 | +7¶ | 24 | / | / | +19¶ | 25 | −3.4¶ | / | FDA approved Reversible | Pneumothorax Granulation tissue |
| BeLieVer-HiFi, 2015 [65] | Single-centre double-blind, sham-controlled, 1:1 | 25 | Heterogeneous Visual fissure intact | 3 | +9#,¶ | 39 | −260# | 48 | +25#,¶ | 52 | −4.4# | 48 | ||
| STELVIO, 2015 [66] | Single-centre, 1:1 | 34 | Hetero- and homogeneous Chartis CV− | 6 | +18¶ | 72 | −831¶ | 71 | +74¶ | 87 | −14.7¶ | 79 | ||
| IMPACT, 2016 [67] | Multicentre, 1:1 | 43 | Homogeneous Chartis CV− | 3 | +17¶ | 42 | −480¶ | 44 | +40¶ | 48 | −9.64¶ | 68 | ||
| TRANSFORM, 2017 [10] | Multicentre, 2:1 | 65 | Heterogeneous Chartis CV− | 6 | +29¶ | 66 | −670¶ | 68 | +79¶ | 65 | −6.5¶ | 66 | ||
| LIBERATE, 2018 [11] | Multicentre, 2:1 | 128 | Heterogeneous Chartis CV− | 12 | +18¶ | 56 | −522¶ | 62 | +39¶ | 42 | −7,05¶ | 56 | ||
| EBV: Spiration Valve System | ||||||||||||||
| REACH, 2018 [68] | Multicentre, 2:1 | 66 | Heterogeneous Visual fissure intact | 6 | +91 mL#,¶ | 41 | −420# | 66 | +21#,¶ | / | −8.4#,¶ | / | FDA approved Reversible |
Severe respiratory adverse events: exacerbations, pneumothorax Granulation tissue |
| EMPROVE, 2019 [69] | Multicentre, 2:1 | 113 | Heterogeneous Visual fissure intact | 6 | +101 mL¶ | 37 | −361¶ | 51 | +7 | 32 | −13¶ | 54 | ||
| AeriSeal sealant | ||||||||||||||
| ASPIRE, 2015 [70] | Multicentre, 3:2 | 34 | Heterogeneous upper lobe-predominant | 6 | +19#,¶ | 52 | / | / | +31#,¶ | 52 | −12#,¶ | 76 | Possible in CV+ Low pneumothorax risk No foreign body |
Severe respiratory adverse events: acute inflammatory response, exacerbations, pneumonia |
| Endobronchial coils | ||||||||||||||
| RESET, 2013 [71] | Multicentre, 1:1 | 23 | Heterogeneous and homogeneous | 3 | +11¶ | 57 | −310¶ | 57 | +64¶ | 74 | −8.4¶ | 65 | Possible in CV+ and/or homogeneous emphysema Low pneumothorax risk |
Staged treatment Not in clinical airway disease Severe respiratory adverse events: coil-associated opacity, exacerbations, pneumonia Granulation tissue |
| REVOLENS, 2016 [72] | Multicentre, 1:1 | 50 | Heterogeneous and homogeneous | 6 | +11¶ | / | −370¶ | / | +21 | 36 | −13.4¶ | / | ||
| RENEW, 2016 [73] | Multicentre, 1:1 | 158 | Heterogeneous and homogeneous | 12 | +7¶ | / | −310¶ | / | +15¶ | 40 | −8.9¶ | 61 | ||
| ELEVATE, 2021 [74] | Multicentre, 2:1 | 57 | Heterogeneous and homogeneous | 6 | +10¶ | 42 | −460¶ | 50 | / | / | −10.6¶ | 57 | ||
| Thermal vapour ablation | ||||||||||||||
| STEP-UP, 2016 [75] | Multicentre, 2:1 | 46 | Heterogeneous upper lobe-predominant | 6 | +15¶ | 50 | −303¶ | / | +31 | 42 | −9.7¶ | 70 | Possible in CV+ Low pneumothorax risk No foreign body |
Staged treatment Severe respiratory adverse events: exacerbations, pneumonia, pneumonitis |
Outcome results (FEV1, RV, 6MWD and SGRQ) are presented as between-group difference in change from baseline (treated versus standard of care). The reported response rate (R) is shown as % in the per protocol population, unless only the response rate of the intention-to-treat population was reported (in RESET, REVOLENS and RENEW). For the minimal clinically important differences used, we refer to the specific study reports. FEV1: forced expiratory volume in 1 s; RV: residual volume; 6MWD: 6-min walk distance; SGRQ: St George's Respiratory Questionnaire; CV: collateral ventilation; CV−: absence of CV; CV+: presence of CV; EBV: endobronchial valve; FDA: US Food and Drug Administration. #: results presented as change from baseline in the treated group; ¶: significant between-group difference or significant difference between treated and standard of care group, p<0.05.
Endobronchial valves
LVR with EBVs is the most extensively investigated bronchoscopic method to improve hyperinflation. One-way EBVs are designed to deflate the targeted lung lobe, inducing atelectasis and thereby reducing lung volume and hyperinflation [78]. The history of EBVs goes back to the early 2000s, when animal and experimental studies investigated the effects of blocking inward airflow to emphysematous lung segments [79, 80]. Soon afterwards, the concept of one-way EBVs was introduced and several studies [81–83] and RCTs using one-way EBVs followed. Since 2019, LVR with EBVs is mentioned as an evidence level A treatment option for patients with severe lung emphysema and hyperinflation in the international Global Initiative for Chronic Obstructive Lung Disease (GOLD) recommendations [84].
Two different devices are commercially available, the Zephyr EBV (Pulmonx, Redwood City, CA, USA) and the Spiration Valve System (Olympus, Redmond, WA, USA) (figure 3). These are made of a nitinol frame with a silicone (Zephyr) or polyurethane (Spiration) membrane. Both the Zephyr and Spiration have four different sizes available, and have unique sizing and delivery systems. The compressed valves are delivered via the instrument channel of a flexible bronchoscope through a catheter in all the (sub)segmental bronchi of the target lobe. The frame expands against the airway wall, and the valve allows outward flow of air and mucus while preventing inward airflow. The Zephyr and Spiration valves are removable by forceps using a flexible bronchoscope and, in case of dislocation, they may be coughed up safely.
The first RCT with the Zephyr EBV in heterogeneous emphysema with hyperinflation was published in 2010, but the effects on FEV1, 6MWD and SGRQ did not reach minimal clinically important differences (MCIDs) (table 2) [64]. It was from post hoc data analyses that the importance of intact fissures, as a surrogate of absent interlobar collateral ventilation, became clear [85]. Interlobar collateral ventilation through incomplete fissures prevents the desired atelectasis of the target lobe. Subsequent studies did select patients based on fissure completeness [9, 65] and visual scoring of fissure completeness and emphysema improved results significantly [65]. Outcomes continued to improve after implementing quantitative CT analysis for emphysema and fissures and invasive measurement of collateral ventilation by Chartis (Pulmonx) [9, 65, 86]. The Chartis assessment system comprises a balloon catheter, inserted via the working channel of the flexible bronchoscope, and a console. Inflating the balloon occludes the bronchus to the targeted lobe and a sensor at the distal end of the balloon measures air flowing out through the central lumen of the catheter. Meanwhile the console displays the flow and pressure in real time. In the absence of collateral ventilation, outward airflow from the target lobe will gradually decline. The STELVIO trial [9] was the first RCT to use quantitative software and Chartis measurement to select patients for EBV treatment. The trial showed highly significant improvement in FEV1, RV, 6MWD and SGRQ in treated compared to control patients, all reaching their respective MCIDs (table 2). The following large multicentre trials confirmed these results (table 2) [10, 11]. One RCT with Zephyr valves has been performed in homogeneous emphysema; treatment effects were less pronounced but significantly better compared to standard of care (table 2) [87].
In the first trials with the Spiration Valve System, a bilateral, but incomplete, lobar occlusion was performed, and failed to show meaningful results in patients with heterogeneous upper lobe-predominant emphysema [88, 89]. Two more recent RCTs with Spiration Valve System aimed for unilateral but complete lobar occlusion in patients with heterogeneous emphysema and intact fissures based on CT assessment. Results showed significant improvement compared to standard of care in some but not all outcomes (table 2) [68, 69].
The long-term safety profile of this intervention is good, but pneumothorax occurs in 4–34% of treated patients [90]. This variability is at least partly explained by the increasing awareness of the importance of fissure completeness for successful treatment, given that the pneumothorax rates went up from 4.2% in the first RCT to 34.4% in the more recent LIBERATE trial [11]. By inducing atelectasis of the target lobe, the ipsilateral lobe will expand to fill the created space in the thoracic cavity. This expansion of destructed lung tissue or presence of pleural adhesions may cause a pneumothorax. The majority of pneumothoraces (>85%) occur within the first 72 h after treatment [91, 92]. A distinction has to be made between a clinically important, symptomatic pneumothorax with air leak versus a clinically well-tolerated pneumothorax ex vacuo, which results from increased negative intrapleural pressure and will resolve spontaneously [93]. Risk factors and a clear management scheme have been proposed by an expert statement but research on this topic is sparse [93]. The outcome and BLVR results after pneumothorax are good, but prolonged air leak with need for additional interventions is common [94]. With 0.75% of 799 patients treated in RCTs dying from pneumothorax, the fatality rate of pneumothorax is low [93]. Other complications are less common, less severe, temporary or reversible by extraction of valves [91]. However, despite careful patient selection, the high rate of revision bronchoscopy (19–41%) and the lack of effect in some patients is still an unresolved concern in EBV treatment [95]. Regarding foreign bodies in the airway, granulation tissue may cause loss of effect and is currently an issue we are not able to prevent [96]. However, the ability to undo the treatment in case of complications or lack of effect is a major advantage of EBVs.
In clinical practice, the durability of treatment effect seems variable and few reports have been published on long-term efficacy. Post hoc analyses of some RCTs showed comparable response rates at 6 and 12 months [66, 67]. The LIBERATE trial is the only RCT investigating treatment effect of EBV at 12 months as a primary outcome. Lung function, exercise capacity and QoL were significantly improved at 12 months, compared to standard of care (table 2) [11, 97]. This trial is ongoing to collect 5-year follow-up data. Other prospective, randomised controlled long-term follow-up studies are lacking. A German retrospective analysis of 256 treated patients reported on 1-, 2- and 3-year real-world follow-up data and showed a sustained effect on FEV1, RV and 6MWD at 1 year, whereafter the clinical benefit declined, especially for FEV1 [98]. At 3 years, the response rate was 71% for RV and 46% for 6MWD. These rates were higher in patients with successful lobar atelectasis, except for FEV1 (10%), probably reflecting general disease progression. A recent real-world analysis on 280 treated patients from The Netherlands confirmed a gradual decline, but showed better durability of effect on FEV1 and RV at 3-year follow-up, and added a persistent significant effect on QoL [99]. At 3 years, the response rate was 33% for FEV1, 50% for RV, 49% for 6MWD and 46% for SGRQ. One should be aware of selection bias and the presence of sustained target lobe volume reduction while interpreting long-term outcome data.
The experience and results of all these RCTs has led to better and comprehensive selection of patients and target lobes in clinical practice, which is invaluable in achieving good treatment results [100–102]. Based on the inclusion criteria of RCTs and expert opinion, cut-offs of hyperinflation parameters and destruction scores have been suggested to select patients. In summary, candidates should have severe emphysema with severe hyperinflation (recommended RV >175% in heterogeneous and RV >200% in homogeneous emphysema) and comorbidities and contraindications should be checked for (figure 1, table 1). The preferred target lobe has the highest level of emphysema heterogeneity, with at least 30% emphysematous destruction at ≤−950 Hounsfield units (HU) recommended, no collateral ventilation based on fissure completeness and/or Chartis measurement, the lowest perfusion, balanced lung volumes and no local contraindications such as pleural adhesions or paraseptal emphysema in the adjacent lobe. A detailed description of patient assessment for BLVR has previously been published [100, 101].
Sealant
Biological LVR has been studied for over a decade with promising results [103–106]. Nevertheless, the administration of a synthetic, two-component foam (polyvinylalcohol and glutaraldehyde, AeriSeal System (currently Pulmonx)) to provoke atelectasis by absorption, inflammation and scar formation has only been investigated in one RCT [70]. Patients with upper lobe-predominant emphysema, airflow limitation and hyperinflation were treated bilaterally in two subsegments per upper lobe. Unfortunately, this trial ended prematurely owing to funding problems. Although significant improvements in FEV1, 6MWD and SGRQ at 6 months were reported, no data on LVR have been published (table 2). Moreover, a significantly larger group of treated patients experienced respiratory-related serious adverse events with a hospitalisation rate >40%, despite a steroid and antibiotic course to prevent post-treatment acute inflammatory response [70]. An attempt to reduce inflammatory side-effects by a staged approach, with lower doses of sealant, was not successful and could not show clinically significant volume reduction [107]. The development of bio-adhesives capable of reducing static and dynamic hyperinflation, without inducing a pronounced inflammatory reaction, is challenging but worth exploring because it may induce durable LVR effects without the concern of interlobar collateral ventilation [108]. Furthermore, reversing collateral ventilation by using low doses of AeriSeal, thereby making patients eligible for EBV treatment, is attractive and under investigation (NCT04256408, NCT04559464) [109].
Lung volume reduction coils
Although placement of EBVs is currently the most effective BLVR option, placement of coils may be an alternative treatment in symptomatic patients with homogeneous emphysema and/or collateral ventilation. Endobronchial coils do not induce lobar atelectasis because they do not completely block inspiratory airflow. Therefore, the presence of collateral ventilation between the target and ipsilateral lobe is irrelevant for this device. The working mechanism is explained as follows: compression of the lung parenchyma reduces the lobar RV and increases airflow to untreated regions; thereby, hyperinflation may be reduced and diaphragm function may improve. By pulling together the most destroyed segments, the elastic recoil of the lung improves, ameliorating expiratory flow and air trapping [110, 111]. This is also reflected by the beneficial effect of coil-associated opacities [73, 112].
Endobronchial coils (PneumRx/BTG, Mountain View, CA, USA) are shape-memory nitinol devices which are placed in the subsegmental bronchi under fluoroscopic guidance by a skilled interventional bronchoscopist (figure 1). The intention is to treat the most destroyed lobes bilaterally, in two stages with an interval of 4–8 weeks [113]. Depending on airway length, the interventionist can choose from three different sizes of coils (100 mm, 125 mm and 150 mm) and a median of 10 coils per procedure is used [114]. Production of the PneumRx endobronchial coil system was terminated in 2020, when the then manufacturer was acquired by Boston Scientific. Nevertheless, we discuss results and experience with this device, because some aspects are promising. It is mentioned with level B evidence in the current GOLD recommendations [115] and new LVR-coil devices have been produced and are under investigation in clinical trials (NCT04520152, NCT03685526).
So far, several studies [63, 111, 116–118], four RCTs [71–74] and three meta-analyses [13, 114, 119] have been published on LVR with coils. No sham-controlled trial has been performed. The first RCT showed significantly better outcomes in coil-treated patients versus standard of care after 3 months [71]. Subsequent, larger trials confirmed the significant improvement in treated patients, but mean values did not reach the MCID for lung function and exercise capacity [72, 73]. One may assume that these rather poor results were a consequence of a large variability in response and the lack of quantitative CT analysis [112]. The latest trial, in which the target lobe was identified by quantitative CT analysis, was terminated prematurely by the study sponsor, but showed significantly better outcomes in coil-treated patients, for whom the decrease in RV and SGRQ score reached the MCID at 6 months (table 2) [74]. The most recent meta-analysis used individual participant data from both single-arm and randomised trials (n=680) [114]. Based on this analysis, LVR-coil treatment resulted in a significant increase in FEV1 at 3- and 6-month follow-up (+90 mL and +70 mL), a significant reduction in RV and SGRQ score at 3-, 6- and 12-month follow-up (−450 mL, −330 mL and −380 mL, and −12.3 points, −10.1 points and −9.8 points, respectively) and a significant increase in 6MWD at 3 months (+38 m).
Longer-term data have been published and show a preserved clinically meaningful effect on SGRQ score, 6MWD and RV in the treated patients at 12 months [120] and 24 months [121]. 3-year follow-up data from 22 treated patients demonstrated that the change from baseline gradually declined to nonsignificant differences [122]. However, at 5 years, a survival advantage became apparent in patients with 10% RV reduction at 3 months [123].
Severe adverse events were reported in up to 52% of coil-treated patients [72–74]. Pneumonia was the most frequent severe adverse event, with a 15% excess incidence in the patients treated with coils [72, 73, 122]. However, pneumonia may be over-diagnosed owing to a coil-associated opacity that occurs in up to 50% of treated patients, and is in fact an inflammatory reaction behaving as pneumonia. Experts recommend the use of corticosteroids and antibiotics in the presence of opacities and/or suspicion of pneumonia after coil treatment [113]. Unfortunately, cases of fatal pneumonia, major hemoptysis (1%) and rare cases of peri-procedural deaths have been reported [73, 124]. Lifelong need for systemic anticoagulants is considered a contraindication for coil LVR. The treating physician should be aware of these and other rare but severe procedure-related adverse events [125]. Pneumothorax does occur in relation to this procedure, but seems uncommon in experienced sites (1–4%) [73, 74].
Severe hyperinflation (RV ≥225%), more pronounced emphysema in the target lobes (≥20% below −950 HU), a lower physical activity level and bilateral treatment of the upper lobes have been put forward as predictors of response to coil treatment. Patients with both heterogeneous and homogeneous disease have been successfully treated in trials, although treatment of the most destroyed lobes seems essential. The presence of clinically relevant airway disease or frequent infectious exacerbations are unfavourable for this treatment [111–113].
Thermal vapour ablation
The use of thermal energy has been investigated to induce LVR in patients with severe heterogeneous lung emphysema. The required energy is calculated based on the quantitative CT-estimated weight of the segment to be treated. An inflammatory reaction is triggered by the application of heated water vapour via a catheter (InterVapor System, Uptake Medical Technology, Inc., Seattle, WA, USA) to the most destroyed segment of the emphysematous upper lobes. An inflatable balloon at the distal end of the catheter isolates the target segment during the delivery of vapour. The provoked inflammation gives rise to fibrotic remodelling and subsequent LVR. Early studies, treating large lobar volumes of lung, suffered from respiratory severe adverse events [126–128]. By reducing the volumes to segmental level and staged treatment (3-month interval), the safety profile improved [129]. One multicentre randomised trial has been published on segmental bronchoscopic thermal vapour ablation (BTVA), showing a significant relative increase in FEV1, decrease in SGRQ for COPD patients score and reduction of RV in treated patients compared to controls at 6 months [75]. These effects were maintained at 12 months [130]. No significant improvement in exercise capacity was measured (table 2). Moreover, the inflammatory response can be very pronounced in some patients with pneumonitis, pneumonia (18% versus 8%) and exacerbations (24% versus 4%), whereas the rate of pneumothorax was only 2%. An analysis of data from two single-arm studies showed better long-term results in patients who experienced respiratory adverse events in the first 30 days [126].
Selection criteria and contraindications are comparable to other LVR strategies (figure 1, table 1), except that only patients with heterogeneous upper lobe-predominant emphysema should be treated by BTVA. Results of a study on homogeneous emphysema (NCT03670121) have not been published so far. A detailed recommendation on selection and procedure has been previously published [129]. BTVA is mentioned in the GOLD recommendations with level B evidence [115]. Although BTVA has several advantages, such as targeted treatment within a lobe, not leaving any devices behind and independency of fissure completeness, the rate of severe respiratory events is an important issue. Together with low availability and expertise, widespread clinical use is hampered and more RCTs on this technique and its safety are needed for further implementation.
Discussion
COPD is a very heterogeneous disease, with clinically and radiologically divergent presentations, complicated by exacerbations and the presence of several comorbidities. As in all chronic diseases, there is no one-size-fits-all treatment and the importance of phenotyping patients and recognising treatable traits cannot be overemphasised when selecting these patients for surgical or bronchoscopic interventions. The implementation of a dedicated multidisciplinary team with at least a pulmonologist, interventional pulmonologist, thoracic surgeon and radiologist should be mandatory to discuss all facets of the patient and thoroughly consider risks and benefits on the individual level. The importance of multidisciplinary case selection and work-up has been acknowledged in several reports on LVR [131–133]. Involvement of a LTX expert, respiratory rehabilitation coordinator or physiotherapist and nurse specialist is a bonus. This multidisciplinary expert team may also propose other therapeutic options (figure 1). Moreover, a nurse coordinator may play a crucial role in the patients’ pathway from referral to follow-up [134].
LVR interventions require experienced surgeons and pulmonologists, capable of coping with and treating procedure-related side-effects and complications, alongside organising a decent follow-up. That is why these interventions are preferably carried out in expert referral centres. The downside to referral centres is the underuse of the current LVR strategies, both bronchoscopic and surgical, which is prompted by limited knowledge and awareness, along with a natural fear of exposing frail patients to treatments that could lead to complications. Although there is high variability in response in most studies, the evidence for LVR is clear at present, and it is a treatment with a proven beneficial effect on pulmonary function, exercise capacity and QoL in well-selected patients. In addition to survival benefits, an impressive effect on cardiac function has recently been demonstrated for patients treated with EBVs [135]. However, many patients referred for LVR treatment will be disappointed because they do not fulfil the recommend criteria for treatment, because devices or expertise are not available or because reimbursement is lacking. Zephyr and Spiration EBV are the only US Food and Drug Administration-approved bronchoscopic interventions at the time of writing. There is continued need for improvement and new developments in this field, especially for other COPD phenotypes. Some promising interventional bronchoscopic procedures are currently under development for COPD patients who mainly experience productive cough and/or exacerbations, as reviewed in this journal before [136]. As recently stated in a Lancet Commission on the elimination of COPD [137], we should look beyond smoking-induced COPD and take other causes and contributing factors into account. Whether LVR works in nonsmoking-induced lung emphysema is not clear. In case of ɑ1-antitrypsin deficiency, results of LVRS in older studies were poor [138, 139], but results of more recent surgical approaches are not available. However, BLVR with EBV seems an efficient and safe treatment in ɑ1-antitrypsin-deficient patients [140]. Patients with infection-related COPD will presumably present with airway disease rather than emphysema. LVRS in congenital emphysema and/or bronchopulmonary dysplasia has only been described in a few case reports [141–143]. In general, we assume that LVR will work in all patients with severe emphysema and severe hyperinflation, regardless of the causing factors, as long as no contraindications for the specific treatment are present.
Relation between LVR and lung transplantation
Techniques that affect (lung) functional status of patients with COPD have the potential to delay the need for LTX. Although LTX is only available to a select group of patients, postponing this treatment may be pertinent to prolong overall survival. Reports on LTX after LVRS have been contradictory. A study on 117 transplanted patients, 52 of whom had previous LVRS, showed no effect of LVRS on short- and long-term outcomes after LTX [144]. Another single-centre report on BLVR before LTX reported no significant difference in 12-month outcome, but found there were significantly more patients with bronchiectasis and airway colonisation in the BLVR group compared to transplanted patients without previous BLVR [145]. A recent multicentre matched retrospective study on both LVRS (n=26 versus n=328 controls) and BLVR (n=60 versus n=270 controls) before LTX confirmed no effect on short- and long-term survival. However, bacterial colonisation was also significantly more prevalent after any LVR procedure prior to LTX. Patients with previous LVRS more often needed extracorporeal membrane oxygenation post lung transplantation, whereas wound infections were more often present in patients who underwent BLVR before LTX [146]. In contrast, a propensity-matched multicentre analysis of 106 COPD patients who underwent LVRS before LTX showed a significantly higher risk of graft failure and lower median survival in this group [147]. The most obvious explanation is the technical challenge of re-operation in the thoracic cavity, where adhesions after LVRS can complicate lung explantation or phrenic nerve injury. This may increase the duration of the LTX procedure and the risk of bleeding, adding the requirement of a blood transfusion, both of which are risk factors for primary graft dysfunction. In summary, outcomes from LTX after prior LVR may not differ, but more perioperative complications and bacterial colonisation mean that increased awareness is required when caring for these patients. On the other hand, LVR offers the potential of bridging towards LTX, gaining additional QoL and improving survival, which cannot be offered after failure of LTX.
Comparison between surgical and bronchoscopic lung volume reduction
A burning and unresolved question in this field is if bronchoscopic and surgical LVR are comparable. Bronchoscopic interventions are less invasive and, in case of valves, reversible, although a complete lobe is sacrificed. LVRS, by contrast, has the potential to reduce more targeted volumes bilaterally and a more customised approach that may result in more favourable outcomes. Moreover, a thoracoscopic approach and implementation of early recovery protocols can reduce the length of hospital stay after LVRS. If BLVR fails, the patient could still be a candidate for a surgical approach. BLVR, however, is contraindicated in a lung where LVRS has been performed. In clinical practice the durability of effect seems comparable, but this has never been compared in a well-designed trial. Considering the advantages and disadvantages of both strategies, it is not clear which is the best option for a patient that is eligible for both BLVR and LVRS. Because EBVs are the most investigated and successful BLVR so far, there is an urgent need for a head-to-head comparison with LVRS in terms of efficacy, safety and durability of effect. One single-centre study on LVR reported results of patients treated with BLVR (n=20) or bilateral LVRS if collateral ventilation was present or BLVR failed (n=16) [148]. Both groups showed significant improvement in FEV1, RV, 6MWD and SGRQ at 3-month follow-up and a similar response rate of 70% for the primary outcome measure (FEV1 increase of 100 mL). The first randomised study comparing BLVR and unilateral LVRS in patients eligible for both procedures was a superiority trial comparing outcomes at 12 months using the iBODE score, a composite disease severity measure (using BMI, airflow obstruction, dyspnoea and exercise capacity) [149, 150]. The study included 88 patients (n=41 unilateral LVRS and n=47 BLVR) and demonstrated that unilateral LVRS was not superior based on iBODE. Nevertheless, it was a unilateral LVRS approach and analyses suffered from missing data. A randomised multicentre study comparing BLVR and bilateral LVRS is currently recruiting (NCT04537182) and will hopefully answer at least some of the remaining questions.
Questions for future research
How can we reduce or prevent granulation tissue related to endobronchial devices?
Can we reduce inflammatory reactions in biological lung volume reduction?
How does pulmonary rehabilitation and physical activity relate to outcomes and durability of lung volume reduction effect?
What is the driver of the gradual decline after lung volume reduction treatment?
What is the preferred surgical strategy: unilateral, bilateral or staged?
When to bridge or when to transplant?
Advantage of robotic lung volume reduction surgery?
Footnotes
Provenance: Commissioned article, peer reviewed.
Number 8 in the Series “Non-pharmacological interventions in COPD: state of the art and future directions” Edited by Geert M. Verleden and Wim Janssens
This article has an editorial commentary: https://doi.org/10.1183/16000617.0028-2023
Previous articles in this series: No. 1: Montes de Oca M, Laucho-Contreras ME. Smoking cessation and vaccination. Eur Respir Rev 2023; 32: 220187. No. 2: Volpato E, Farver-Vestergaard I, Brighton LJ, et al. Nonpharmacological management of psychological distress in people with COPD. Eur Respir Rev 2023; 32: 220170. No. 3: Owens RL, Derom E, Ambrosino N. Supplemental oxygen and noninvasive ventilation. Eur Respir Rev 2023; 32: 220159. No. 4: Verleden GM, Gottlieb J. Lung transplantation for COPD/pulmonary emphysema. Eur Respir Rev 2023; 32: 220116. No. 5: Troosters T, Janssens W, Demeyer H, et al. Pulmonary rehabilitation and physical interventions. Eur Respir Rev 2023; 32: 220222. No. 5: Troosters T, Janssens W, Demeyer H, et al. Pulmonary rehabilitation and physical interventions. Eur Respir Rev 2023; 32: 220222. No. 6: Beijers RJHCG, Steiner MC, Schols AMWJ. The role of diet and nutrition in the management of COPD. Eur Respir Rev 2023; 32: 220003. No. 7: Simon S, Joean O, Welte T, et al. The role of vaccination in COPD: influenza, SARS-CoV-2, pneumococcus, pertussis, RSV and varicella zoster virus. Eur Respir Rev 2023; 32: 230034.
Conflict of interest: S. Everaerts, C.M. Vandervelde and P. Shah have no conflicts of interest related to the content of the manuscript. D-J. Slebos reports grants or contracts, study material, registration fees and travel costs, and participation on a Data and Safety Monitoring Board for Pulmonx, Corp., BTG/PneumRx Inc, FreeFlowMedical, Nuvaira, PulmAir, GALA, CSA Medical and Apreo, most of them paid to his institution. L.J. Ceulemans received an unrestricted university chair from Medtronic and a philanthropic grant from Gunze.
References
- 1.Soriano JB, Kendrick PJ, Paulson KR, et al. Prevalence and attributable health burden of chronic respiratory diseases, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Respir Med 2020; 8: 585–596. doi: 10.1016/S2213-2600(20)30105-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO Department of Data and Analytics . Global Health Estimates 2019: Disease Burden by Cause, Age, Sex, by Country and by Region, 2000–2019. Geneva, World Health Organization, 2020. [Google Scholar]
- 3.Perch M, Hayes D, Cherikh WS, et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Thirty-ninth adult lung transplantation report—2022; focus on lung transplant recipients with chronic obstructive pulmonary disease. J Heart Lung Transplant 2022; 41: S1053249822020745. doi: 10.1016/j.healun.2022.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brantigan OC, Mueller E, Kress MB. A surgical approach to pulmonary emphysema. Am Rev Respir Dis 1959; 80: 194–206. [DOI] [PubMed] [Google Scholar]
- 5.Celli BR, Cote CG, Marin JM, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med 2004; 350: 1005–1012. doi: 10.1056/NEJMoa021322 [DOI] [PubMed] [Google Scholar]
- 6.Sciurba FC, Rogers RM, Keenan RJ, et al. Improvement in pulmonary function and elastic recoil after lung-reduction surgery for diffuse emphysema. N Engl J Med 1996; 334: 1095–1099. doi: 10.1056/NEJM199604253341704 [DOI] [PubMed] [Google Scholar]
- 7.Estenne M. Effect of lung transplant and volume reduction surgery on respiratory muscle function. J Appl Physiol (1985) 2009; 107: 977–986. [DOI] [PubMed] [Google Scholar]
- 8.Martinez FJ, de Oca MM, Whyte RI, et al. Lung-volume reduction improves dyspnea, dynamic hyperinflation, and respiratory muscle function. Am J Respir Crit Care Med 1997; 155: 1984–1990. doi: 10.1164/ajrccm.155.6.9196106 [DOI] [PubMed] [Google Scholar]
- 9.Klooster K, ten Hacken NHT, Hartman JE, et al. Endobronchial valves for emphysema without interlobar collateral ventilation. N Engl J Med 2015; 373: 2325–2335. doi: 10.1056/NEJMoa1507807 [DOI] [PubMed] [Google Scholar]
- 10.Kemp SV, Slebos DJ, Kirk A, et al. A multicenter randomized controlled trial of Zephyr endobronchial valve treatment in heterogeneous emphysema (TRANSFORM). Am J Respir Crit Care Med 2017; 196: 1535–1543. doi: 10.1164/rccm.201707-1327OC [DOI] [PubMed] [Google Scholar]
- 11.Criner GJ, Sue R, Wright S, et al. A multicenter randomized controlled trial of Zephyr endobronchial valve treatment in heterogeneous emphysema (LIBERATE). Am J Respir Crit Care Med 2018; 198: 1151–1164. doi: 10.1164/rccm.201803-0590OC [DOI] [PubMed] [Google Scholar]
- 12.Naunheim KS, Wood DE, Mohsenifar Z, et al. Long-term follow-up of patients receiving lung-volume-reduction surgery versus medical therapy for severe emphysema by the National Emphysema Treatment Trial Research Group. Ann Thorac Surg 2006; 82: 431–443. doi: 10.1016/j.athoracsur.2006.05.069 [DOI] [PubMed] [Google Scholar]
- 13.van Geffen WH, Slebos DJ, Herth FJ, et al. Surgical and endoscopic interventions that reduce lung volume for emphysema: a systemic review and meta-analysis. Lancet Respir Med 2019; 7: 313–324. doi: 10.1016/S2213-2600(18)30431-4 [DOI] [PubMed] [Google Scholar]
- 14.Garner J, Kemp SV, Toma TP, et al. Survival after endobronchial valve placement for emphysema: a 10-year follow-up study. Am J Respir Crit Care Med 2016; 194: 519–521. doi: 10.1164/rccm.201604-0852LE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gompelmann D, Benjamin N, Bischoff E, et al. Survival after endoscopic valve therapy in patients with severe emphysema. Respiration 2019; 97: 145–152. doi: 10.1159/000492274 [DOI] [PubMed] [Google Scholar]
- 16.Hartman JE, Welling JBA, Klooster K, et al. Survival in COPD patients treated with bronchoscopic lung volume reduction. Respir Med 2022; 196: 106825. doi: 10.1016/j.rmed.2022.106825 [DOI] [PubMed] [Google Scholar]
- 17.Freund WA. Zur operativen Behandlung gewisser Lungenkrankheiten, insbesondere des auf starrer Thoraxidlatation beruhenden alveolären Emphysems (mit einem Operationsfalle) [On the surgical treatment of certain lung diseases, in particular thoracic dilatation of rigid thorax for alveolar emphysema]. Z Für Exp Pathol Ther 1906; 3: 479–498. doi: 10.1007/BF02622074 [DOI] [Google Scholar]
- 18.Gaensler EA, Strieder JW. Progressive changes in pulmonary function after pneumonectomy: the influence of thoracoplasty, pneumothorax, oleothorax, and plastic sponge plombage on the side of pneumonectomy. J Thorac Surg 1951; 22: 1–34. doi: 10.1016/S0096-5588(20)31139-9 [DOI] [PubMed] [Google Scholar]
- 19.Allison PR. Giant bullous cysts of the lung. Thorax 1947; 2: 169–175. doi: 10.1136/thx.2.4.169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abbott OA, Hopkins WA, Van Fleit WE, et al. A new approach to pulmonary emphysema. Thorax 1953; 8: 116–132. doi: 10.1136/thx.8.2.116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cooper JD, Trulock EP, Triantafillou AN, et al. Bilateral pneumectomy (volume reduction) for chronic obstructive pulmonary disease. J Thorac Cardiovasc Surg 1995; 109: 106–119. doi: 10.1016/S0022-5223(95)70426-4 [DOI] [PubMed] [Google Scholar]
- 22.Cooper JD, Patterson GA, Sundaresan RS, et al. Results of 150 consecutive bilateral lung volume reduction procedures in patients with severe emphysema. J Thorac Cardiovasc Surg 1996; 112: 1319–1330. doi: 10.1016/S0022-5223(96)70147-2 [DOI] [PubMed] [Google Scholar]
- 23.Miller JD, Malthaner RA, Goldsmith CH, et al. Lung volume reduction for emphysema and the Canadian Lung Volume Reduction Surgery (CLVR) Project. Can Respir J 1999; 6: 26–32. doi: 10.1155/1999/817812 [DOI] [PubMed] [Google Scholar]
- 24.Keenan RJ, Landreneau RJ, Sciurba FC, et al. Unilateral thoracoscopic surgical approach for diffuse emphysema. J Thorac Cardiovasc Surg 1996; 111: 308–316. doi: 10.1016/S0022-5223(96)70439-7 [DOI] [PubMed] [Google Scholar]
- 25.Bingisser R, Zollinger A, Hauser M, et al. Bilateral volume reduction surgery for diffuse pulmonary emphysema by video-assisted thoracoscopy. J Thorac Cardiovasc Surg 1996; 112: 875–882. doi: 10.1016/S0022-5223(96)70086-7 [DOI] [PubMed] [Google Scholar]
- 26.Fishman A, Martinez F, Naunheim K, et al. A randomized trial comparing lung-volume–reduction surgery with medical therapy for severe emphysema. N Engl J Med 2003; 348: 2059–2073. doi: 10.1056/NEJMoa030287 [DOI] [PubMed] [Google Scholar]
- 27.National Emphysema Treatment Trial Research Group , Fishman A, Fessler H, et al. Patients at high risk of death after lung-volume–reduction surgery. N Engl J Med 2001; 345: 1075–1083. doi: 10.1056/NEJMoa11798 [DOI] [PubMed] [Google Scholar]
- 28.Ginsburg ME, Thomashow BM, Bulman WA, et al. The safety, efficacy, and durability of lung-volume reduction surgery: a 10-year experience. J Thorac Cardiovasc Surg 2016; 151: 717–724. doi: 10.1016/j.jtcvs.2015.10.095 [DOI] [PubMed] [Google Scholar]
- 29.Weder W, Tutic M, Lardinois D, et al. Persistent benefit from lung volume reduction surgery in patients with homogeneous emphysema. Ann Thorac Surg 2009; 87: 229–237. doi: 10.1016/j.athoracsur.2008.10.012 [DOI] [PubMed] [Google Scholar]
- 30.Ciccone AM, Meyers BF, Guthrie TJ, et al. Long-term outcome of bilateral lung volume reduction in 250 consecutive patients with emphysema. J Thorac Cardiovasc Surg 2003; 125: 513–525. doi: 10.1067/mtc.2003.147 [DOI] [PubMed] [Google Scholar]
- 31.Weder W, Ceulemans LJ, Opitz I, et al. Lung volume reduction surgery in patients with homogeneous emphysema. Thorac Surg Clin 2021; 31: 203–209. doi: 10.1016/j.thorsurg.2021.02.007 [DOI] [PubMed] [Google Scholar]
- 32.Caviezel C, Schaffter N, Schneiter D, et al. Outcome after lung volume reduction surgery in patients with severely impaired diffusion capacity. Ann Thorac Surg 2018; 105: 379–385. doi: 10.1016/j.athoracsur.2017.09.006 [DOI] [PubMed] [Google Scholar]
- 33.Caviezel C, Aruldas C, Franzen D, et al. Lung volume reduction surgery in selected patients with emphysema and pulmonary hypertension. Eur J Cardiothorac Surg 2018; 54: 565–571. doi: 10.1093/ejcts/ezy092 [DOI] [PubMed] [Google Scholar]
- 34.Clarenbach CF, Sievi NA, Brock M, et al. Lung volume reduction surgery and improvement of endothelial function and blood pressure in patients with chronic obstructive pulmonary disease. A randomized controlled trial. Am J Respir Crit Care Med 2015; 192: 307–314. doi: 10.1164/rccm.201503-0453OC [DOI] [PubMed] [Google Scholar]
- 35.Oey I, Waller D. The role of the multidisciplinary emphysema team meeting in the provision of lung volume reduction. J Thorac Dis 2018; 10: S2824–S2829. doi: 10.21037/jtd.2018.02.68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Darwiche K, Karpf-Wissel R, Eisenmann S, et al. Bronchoscopic lung volume reduction with endobronchial valves in low-FEV1 patients. Respiration 2016; 92: 414–419. [DOI] [PubMed] [Google Scholar]
- 37.Trudzinski FC, Höink AJ, Leppert D, et al. Endoscopic lung volume reduction using endobronchial valves in patients with severe emphysema and very low FEV1. Respiration 2016; 92: 258–265. doi: 10.1159/000448761 [DOI] [PubMed] [Google Scholar]
- 38.van Dijk M, Hartman JE, Klooster K, et al. Endobronchial valve treatment in emphysema patients with a very low DLCO. Respiration 2020; 99: 163–170. doi: 10.1159/000505428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lenga P, Ruwwe-Glösenkamp C, Grah C, et al. Endoscopic lung volume reduction with endobronchial valves in very low DLCO patients: results from the German Registry – Lungenemphysemregister e.V. ERJ Open Res 2021; 7: 00449-2020. doi: 10.1183/23120541.00449-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Roetting M, Kriegsmann K, Polke M, et al. Endoscopic valve therapy in COPD patients with hypercapnia. Respiration 2022; 101: 918–924. doi: 10.1159/000525729 [DOI] [PubMed] [Google Scholar]
- 41.Meyers BF, Sultan PK, Guthrie TJ, et al. Outcomes after unilateral lung volume reduction. Ann Thorac Surg 2008; 86: 204–212. doi: 10.1016/j.athoracsur.2008.03.029 [DOI] [PubMed] [Google Scholar]
- 42.Pompeo E, Mineo TC, Pulmonary Emphysema Research group . Long-term outcome of staged versus one-stage bilateral thoracoscopic reduction pneumoplasty. Eur J Cardiothorac Surg 2002; 21: 627–633. doi: 10.1016/S1010-7940(02)00038-6 [DOI] [PubMed] [Google Scholar]
- 43.Oey IF, Morgan MDL, Spyt TJ, et al. Staged bilateral lung volume reduction surgery - the benefits of a patient-led strategy. Eur J Cardiothorac Surg 2010; 37: 846–852. doi: 10.1016/j.ejcts.2009.10.025 [DOI] [PubMed] [Google Scholar]
- 44.Oey I, Steiner M, Morgan M, et al. Patient-directed volume reduction for emphysema: sequential surgical and endobronchial techniques. Ann Thorac Surg 2021; 112: 295–301. doi: 10.1016/j.athoracsur.2020.08.015 [DOI] [PubMed] [Google Scholar]
- 45.Boasquevisque CHR, Yildirim E, Waddel TK, et al. Surgical techniques: lung transplant and lung volume reduction. Proc Am Thorac Soc 2009; 6: 66–78. doi: 10.1513/pats.200808-083GO [DOI] [PubMed] [Google Scholar]
- 46.Kawai N, Kawaguchi T, Suzuki S, et al. Low-voltage coagulation, polyglycolic acid sheets, and fibrin glue to control air leaks in lung surgery. Gen Thorac Cardiovasc Surg 2017; 65: 705–709. doi: 10.1007/s11748-017-0829-2 [DOI] [PubMed] [Google Scholar]
- 47.Pompeo E, Rogliani P, Cristino B, et al. Staged unilateral lung volume reduction surgery: from mini-invasive to minimalist treatment strategies. J Thorac Dis 2018; 10: S2754–S2762. doi: 10.21037/jtd.2018.05.171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mineo TC, Pompeo E, Mineo D, et al. Awake nonresectional lung volume reduction surgery. Ann Surg 2006; 243: 131–136. doi: 10.1097/01.sla.0000182917.39534.2c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pompeo E, Rogliani P, Tacconi F, et al. Randomized comparison of awake nonresectional versus nonawake resectional lung volume reduction surgery. J Thorac Cardiovasc Surg 2012; 143: 47–54. doi: 10.1016/j.jtcvs.2011.09.050 [DOI] [PubMed] [Google Scholar]
- 50.Klijian A. A novel approach to control air leaks in complex lung surgery: a retrospective review. J Cardiothorac Surg 2012; 7: 49. doi: 10.1186/1749-8090-7-49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Allen MS, Wood DE, Hawkinson RW, et al. Prospective randomized study evaluating a biodegradable polymeric sealant for sealing intraoperative air leaks that occur during pulmonary resection. Ann Thorac Surg 2004; 77: 1792–1801. doi: 10.1016/j.athoracsur.2003.10.049 [DOI] [PubMed] [Google Scholar]
- 52.Caviezel C, Schneiter D, Lauk O, et al. Firefly robotic lung volume reduction surgery: case report. J Vis Surg 2021; 7: 19. doi: 10.21037/jovs-20-73 [DOI] [Google Scholar]
- 53.Naunheim KS, Wood DE, Krasna MJ, et al. Predictors of operative mortality and cardiopulmonary morbidity in the National Emphysema Treatment Trial. J Thorac Cardiovasc Surg 2006; 131: 43–53. doi: 10.1016/j.jtcvs.2005.09.006 [DOI] [PubMed] [Google Scholar]
- 54.DeCamp MM, Blackstone EH, Naunheim KS, et al. Patient and surgical factors influencing air leak after lung volume reduction surgery: lessons learned from the National Emphysema Treatment Trial. Ann Thorac Surg 2006; 82: 197–206. doi: 10.1016/j.athoracsur.2006.02.050 [DOI] [PubMed] [Google Scholar]
- 55.Horwood CR, Mansour D, Abdel-Rasoul M, et al. Long-term results after lung volume reduction surgery: a single institution's experience. Ann Thorac Surg 2019; 107: 1068–1073. doi: 10.1016/j.athoracsur.2018.10.014 [DOI] [PubMed] [Google Scholar]
- 56.Lacour M, Caviezel C, Weder W, et al. Postoperative complications and management after lung volume reduction surgery. J Thorac Dis 2018; 10: S2775–S2779. doi: 10.21037/jtd.2018.08.75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Clark SJ, Zoumot Z, Bamsey O, et al. Surgical approaches for lung volume reduction in emphysema. Clin Med 2014; 14: 122–127. doi: 10.7861/clinmedicine.14-2-122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lausberg HF, Chino K, Patterson GA, et al. Bronchial fenestration improves expiratory flow in emphysematous human lungs. Ann Thorac Surg 2003; 75: 393–398. doi: 10.1016/S0003-4975(02)04553-8 [DOI] [PubMed] [Google Scholar]
- 59.Choong CK, Phan L, Massetti P, et al. Prolongation of patency of airway bypass stents with use of drug-eluting stents. J Thorac Cardiovasc Surg 2006; 131: 60–64. doi: 10.1016/j.jtcvs.2005.07.057 [DOI] [PubMed] [Google Scholar]
- 60.Cardoso PFG, Snell GI, Hopkins P, et al. Clinical application of airway bypass with paclitaxel-eluting stents: early results. J Thorac Cardiovasc Surg 2007; 134: 974–981. doi: 10.1016/j.jtcvs.2007.05.040 [DOI] [PubMed] [Google Scholar]
- 61.Shah P, Slebos DJ, Cardoso P, et al. Bronchoscopic lung-volume reduction with Exhale airway stents for emphysema (EASE trial): randomised, sham-controlled, multicentre trial. Lancet 2011; 378: 997–1005. doi: 10.1016/S0140-6736(11)61050-7 [DOI] [PubMed] [Google Scholar]
- 62.Shah PL, Slebos DJ, Cardoso PF, et al. Design of the exhale airway stents for emphysema (EASE) trial: an endoscopic procedure for reducing hyperinflation. BMC Pulm Med 2011; 11: 1. doi: 10.1186/1471-2466-11-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Deslée G, Klooster K, Hetzel M. Lung volume reduction coil treatment for patients with severe emphysema: a European multicentre trial. Thorax 2014; 69: 980–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sciurba FC, Ernst A, Herth FJF, et al. A randomized study of endobronchial valves for advanced emphysema. N Engl J Med 2010; 363: 1233–1244. doi: 10.1056/NEJMoa0900928 [DOI] [PubMed] [Google Scholar]
- 65.Davey C, Zoumot Z, Jordan S, et al. Bronchoscopic lung volume reduction with endobronchial valves for patients with heterogeneous emphysema and intact interlobar fissures (the BeLieVeR-HIFi study): a randomised controlled trial. Lancet 2015; 386: 1066–1073. doi: 10.1016/S0140-6736(15)60001-0 [DOI] [PubMed] [Google Scholar]
- 66.Klooster K, Hartman JE, Ten Hacken NHT, et al. One-year follow-up after endobronchial valve treatment in patients with emphysema without collateral ventilation treated in the STELVIO trial. Respiration 2017; 93: 112–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Eberhardt R, Slebos DJ, Herth FJF, et al. Endobronchial valve (Zephyr) treatment in homogeneous emphysema: one-year results from the IMPACT randomized clinical trial. Respiration 2021; 100: 1174–1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Li S, Wang G, Wang C, et al. The REACH trial: a randomized controlled trial assessing the safety and effectiveness of the Spiration valve system in the treatment of severe emphysema. Respiration 2019; 97: 416–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Criner GJ, Delage A, Voelker K, et al. Improving lung function in severe heterogenous emphysema with the Spiration Valve System (EMPROVE). A multicenter, open-label randomized controlled clinical trial. Am J Respir Crit Care Med 2019; 200: 1354–1362. doi: 10.1164/rccm.201902-0383OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Come CE, Kramer MR, Dransfield MT, et al. A randomised trial of lung sealant versus medical therapy for advanced emphysema. Eur Respir J 2015; 46: 651–662. doi: 10.1183/09031936.00205614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Shah PL, Zoumot Z, Singh S, et al. Endobronchial coils for the treatment of severe emphysema with hyperinflation (RESET): a randomised controlled trial. Lancet Respir Med 2013; 1: 233–240. doi: 10.1016/S2213-2600(13)70047-X [DOI] [PubMed] [Google Scholar]
- 72.Deslée G, Mal H, Dutau H, et al. Lung volume reduction coil treatment vs usual care in patients with severe emphysema: the REVOLENS randomized clinical trial. JAMA 2016; 315: 175. doi: 10.1001/jama.2015.17821 [DOI] [PubMed] [Google Scholar]
- 73.Sciurba FC, Criner GJ, Strange C, et al. Effect of endobronchial coils vs usual care on exercise tolerance in patients with severe emphysema: the RENEW randomized clinical trial. JAMA 2016; 315: 2178–2189. doi: 10.1001/jama.2016.6261 [DOI] [PubMed] [Google Scholar]
- 74.Klooster K, Valipour A, Marquette CH, et al. Endobronchial coil system versus standard-of-care medical management in the treatment of subjects with severe emphysema. Respiration 2021; 100: 804–810. doi: 10.1159/000515744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Herth FJF, Valipour A, Shah PL, et al. Segmental volume reduction using thermal vapour ablation in patients with severe emphysema: 6-month results of the multicentre, parallel-group, open-label, randomised controlled STEP-UP trial. Lancet Respir Med 2016; 4: 185–193. doi: 10.1016/S2213-2600(16)00045-X [DOI] [PubMed] [Google Scholar]
- 76.Moore AJ, Cetti E, Haj-Yahia S, et al. Unilateral extrapulmonary airway bypass in advanced emphysema. Ann Thorac Surg 2010; 89: 899–906. doi: 10.1016/j.athoracsur.2009.10.067 [DOI] [PubMed] [Google Scholar]
- 77.Snell GI, Holsworth L, Khorramnia S, et al. Feasibility and safety of a transthoracic pneumostoma airway bypass in severe emphysema patients. Respiration 2017; 93: 236–246. [DOI] [PubMed] [Google Scholar]
- 78.Hopkinson NS, Toma TP, Hansell DM, et al. Effect of bronchoscopic lung volume reduction on dynamic hyperinflation and exercise in emphysema. Am J Respir Crit Care Med 2005; 171: 453–460. doi: 10.1164/rccm.200407-961OC [DOI] [PubMed] [Google Scholar]
- 79.Ingenito EP, Reilly JJ, Mentzer SJ, et al. Bronchoscopic volume reduction: a safe and effective alternative to surgical therapy for emphysema. Am J Respir Crit Care Med 2001; 164: 295–301. doi: 10.1164/ajrccm.164.2.2011085 [DOI] [PubMed] [Google Scholar]
- 80.Sabanathan S, Richardson J, Pieri-Davies S. Bronchoscopic lung volume reduction. J Cardiovasc Surg (Torino) 2003; 44: 101–108. [PubMed] [Google Scholar]
- 81.Snell GI, Holsworth L, Borrill ZL, et al. The potential for bronchoscopic lung volume reduction using bronchial prostheses: a pilot study. Chest 2003; 124: 1073–1080. doi: 10.1378/chest.124.3.1073 [DOI] [PubMed] [Google Scholar]
- 82.Toma TP, Hopkinson NS, Hillier J, et al. Bronchoscopic volume reduction with valve implants in patients with severe emphysema. Lancet 2003; 361: 931–933. doi: 10.1016/S0140-6736(03)12762-6 [DOI] [PubMed] [Google Scholar]
- 83.Yim APC, Hwong TMT, Lee TW, et al. Early results of endoscopic lung volume reduction for emphysema. J Thorac Cardiovasc Surg 2004; 127: 1564–1573. doi: 10.1016/j.jtcvs.2003.10.005 [DOI] [PubMed] [Google Scholar]
- 84.Singh D, Agusti A, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease: the GOLD science committee report 2019. Eur Respir J 2019; 53: 1900164. doi: 10.1183/13993003.00164-2019 [DOI] [PubMed] [Google Scholar]
- 85.Herth FJF, Noppen M, Valipour A, et al. Efficacy predictors of lung volume reduction with Zephyr valves in a European cohort. Eur Respir J 2012; 39: 1334–1342. doi: 10.1183/09031936.00161611 [DOI] [PubMed] [Google Scholar]
- 86.Herth FJF, Eberhardt R, Gompelmann D, et al. Radiological and clinical outcomes of using Chartis to plan endobronchial valve treatment. Eur Respir J 2013; 41: 302–308. doi: 10.1183/09031936.00015312 [DOI] [PubMed] [Google Scholar]
- 87.Valipour A, Slebos DJ, Herth F, et al. Endobronchial valve therapy in patients with homogeneous emphysema. Results from the IMPACT study. Am J Respir Crit Care Med 2016; 194: 1073–1082. doi: 10.1164/rccm.201607-1383OC [DOI] [PubMed] [Google Scholar]
- 88.Ninane V, Geltner C, Bezzi M, et al. Multicentre European study for the treatment of advanced emphysema with bronchial valves. Eur Respir J 2012; 39: 1319–1325. doi: 10.1183/09031936.00019711 [DOI] [PubMed] [Google Scholar]
- 89.Wood DE, Nader DA, Springmeyer SC, et al. The IBV Valve trial: a multicenter, randomized, double-blind trial of endobronchial therapy for severe emphysema. J Bronchol Interv Pulmonol 2014; 21: 288–297. doi: 10.1097/LBR.0000000000000110 [DOI] [PubMed] [Google Scholar]
- 90.Koster TD, Klooster K, Ten Hacken NHT, et al. Endobronchial valve therapy for severe emphysema: an overview of valve-related complications and its management. Expert Rev Respir Med 2020; 14: 1235–1247. doi: 10.1080/17476348.2020.1813571 [DOI] [PubMed] [Google Scholar]
- 91.Fiorelli A, D'Andrilli A, Bezzi M, et al. Complications related to endoscopic lung volume reduction for emphysema with endobronchial valves: results of a multicenter study. J Thorac Dis 2018; 10: Suppl. 27, S3315–S3325. doi: 10.21037/jtd.2018.06.69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gompelmann D, Lim HJ, Eberhardt R, et al. Predictors of pneumothorax following endoscopic valve therapy in patients with severe emphysema. Int J Chron Obstruct Pulmon Dis 2016; 11: 1767–1773. doi: 10.2147/COPD.S106439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.van Dijk M, Sue R, Criner GJ, et al. Expert statement: pneumothorax associated with one-way valve therapy for emphysema: 2020 update. Respiration 2021; 100: 969–978. doi: 10.1159/000516326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Gompelmann D, Benjamin N, Kontogianni K, et al. Clinical and radiological outcome following pneumothorax after endoscopic lung volume reduction with valves. Int J Chron Obstruct Pulmon Dis 2016; 11: 3093–3099. doi: 10.2147/COPD.S117890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Roodenburg SA, Klooster K, Hartman JE, et al. Revision bronchoscopy after endobronchial valve treatment for emphysema: indications, findings and outcomes. Int J Chron Obstruct Pulmon Dis 2021; 16: 1127–1136. doi: 10.2147/COPD.S302662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Roodenburg SA, Pouwels SD, Slebos DJ. Airway granulation response to lung-implantable medical devices: a concise overview. Eur Respir Rev 2021; 30: 210066. doi: 10.1183/16000617.0066-2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Dransfield MT, Garner JL, Bhatt SP, et al. Effect of Zephyr endobronchial valves on dyspnea, activity levels, and quality of life at one year. Results from a randomized clinical trial. Ann Am Thorac Soc 2020; 17: 829–838. doi: 10.1513/AnnalsATS.201909-666OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Gompelmann D, Heinhold T, Rötting M, et al. Long-term follow up after endoscopic valve therapy in patients with severe emphysema. Ther Adv Respir Dis 2019; 13: 175346661986610. doi: 10.1177/1753466619866101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hartman JE, Klooster K, Koster TD, et al. Long-term follow up after bronchoscopic lung volume reduction valve treatment for emphysema. ERJ Open Res 2022; 8: 00235-2022. doi: 10.1183/23120541.00235-2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Herth FJF, Slebos DJ, Criner GJ, et al. Endoscopic lung volume reduction: an expert panel recommendation - update 2019. Respiration 2019; 97: 548–557. [DOI] [PubMed] [Google Scholar]
- 101.Klooster K, Slebos DJ. Endobronchial valves for the treatment of advanced emphysema. Chest 2021; 159: 1833–1842. doi: 10.1016/j.chest.2020.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Slebos DJ, Shah PL, Herth FJF, et al. Endobronchial valves for endoscopic lung volume reduction: best practice recommendations from expert panel on endoscopic lung volume reduction. Respiration 2017; 93: 138–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Herth FJF, Gompelmann D, Stanzel F, et al. Treatment of advanced emphysema with emphysematous lung sealant (AeriSeal). Respiration 2011; 82: 36–45. doi: 10.1159/000322649 [DOI] [PubMed] [Google Scholar]
- 104.Kramer MR, Refaely Y, Maimon N, et al. Bilateral endoscopic sealant lung volume reduction therapy for advanced emphysema. Chest 2012; 142: 1111–1117. doi: 10.1378/chest.12-0421 [DOI] [PubMed] [Google Scholar]
- 105.Kramer MR, Refaely Y, Maimon N, et al. Two-year follow-up in patients treated with emphysematous lung sealant for advanced emphysema. Chest 2013; 144: 1677–1680. doi: 10.1378/chest.13-0446 [DOI] [PubMed] [Google Scholar]
- 106.Refaely Y, Dransfield M, Kramer MR, et al. Biologic lung volume reduction therapy for advanced homogeneous emphysema. Eur Respir J 2010; 36: 20–27. doi: 10.1183/09031936.00106009 [DOI] [PubMed] [Google Scholar]
- 107.Koster TD, Eberhardt R, Huebner RH, et al. A multicenter, prospective, single-arm clinical investigation of a modified staged treatment algorithm using the AeriSeal system - The STAGE trial. Respir Med 2022; 203: 106989. doi: 10.1016/j.rmed.2022.106989 [DOI] [PubMed] [Google Scholar]
- 108.Joglekar MM, Slebos DJ, Leijten J, et al. Crosslink bio-adhesives for bronchoscopic lung volume reduction: current status and future direction. Eur Respir Rev 2021; 30: 210142. doi: 10.1183/16000617.0142-2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ing AJ, Jayapadman A, Kim W, et al. Reversal of collateral ventilation using endoscopic polymer foam in COPD patients undergoing endoscopic lung volume reduction with endobronchial valves: a controlled parallel group trial. Respirology 2022; 27: 1064–1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Hartman JE, Shah PL, Sciurba F, et al. Endobronchial coils for emphysema: dual mechanism of action on lobar residual volume reduction. Respirology 2020; 25: 1160–1166. doi: 10.1111/resp.13816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Hartman JE, Klooster K, Augustijn SWS, et al. Identifying responders and exploring mechanisms of action of the endobronchial coil treatment for emphysema. Respiration 2021; 100: 443–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Slebos DJ, Cicenia J, Sciurba FC, et al. Predictors of response to endobronchial coil therapy in patients with advanced emphysema. Chest 2019; 155: 928–937. doi: 10.1016/j.chest.2019.02.012 [DOI] [PubMed] [Google Scholar]
- 113.Slebos DJ, Ten Hacken NH, Hetzel M, et al. Endobronchial coils for endoscopic lung volume reduction: best practice recommendations from an expert panel. Respiration 2018; 96: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Roodenburg SA, Hartman JE, Deslée G, et al. Bronchoscopic lung volume reduction coil treatment for severe emphysema: a systematic review and meta-analysis of individual participant data. Respiration 2022; 101: 697–705. doi: 10.1159/000524148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Global Initiative for Chronic Obstructive Lung Disease (GOLD) . Global Strategy for the Diagnosis, Management and Prevention of COPD. 2016. Available from: https://goldcopd.org/
- 116.Slebos DJ, Klooster K, Ernst A. Bronchoscopic lung volume reduction coil treatment of patients with severe heterogeneous emphysema. Chest 2012; 142: 574–582. [DOI] [PubMed] [Google Scholar]
- 117.Klooster K, Ten Hacken NHT, Franz I, et al. Lung volume reduction coil treatment in chronic obstructive pulmonary disease patients with homogeneous emphysema: a prospective feasibility trial. Respiration 2014; 88: 116–125. [DOI] [PubMed] [Google Scholar]
- 118.Fellrath JM, Scherer T, Franzen DP, et al. Endobronchial coil therapy in severe emphysema: 6-month outcomes from a Swiss National Registry. J Thorac Dis 2018; 10: Suppl. 23, S2711–S2718. doi: 10.21037/jtd.2018.04.53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Slebos DJ, Hartman JE, Klooster K, et al. Bronchoscopic coil treatment for patients with severe emphysema: a meta-analysis. Respiration 2015; 90: 136–145. [DOI] [PubMed] [Google Scholar]
- 120.Zoumot Z, Kemp SV, Singh S, et al. Endobronchial coils for severe emphysema are effective up to 12 months following treatment: medium term and cross-over results from a randomised controlled trial. PLoS One 2015; 10: e0122656. doi: 10.1371/journal.pone.0122656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Deslée G, Leroy S, Perotin JM, et al. Two-year follow-up after endobronchial coil treatment in emphysema: results from the REVOLENS study. Eur Respir J 2017; 50: 1701740. doi: 10.1183/13993003.01740-2017 [DOI] [PubMed] [Google Scholar]
- 122.Hartman JE, Klooster K, Gortzak K, et al. Long-term follow-up after bronchoscopic lung volume reduction treatment with coils in patients with severe emphysema. Respirology 2015; 20: 319–326. doi: 10.1111/resp.12435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Garner JL, Kemp SV, Srikanthan K, et al. 5-Year survival after endobronchial coil implantation: secondary analysis of the first randomised controlled trial, RESET. Respiration 2020; 99: 154–162. [DOI] [PubMed] [Google Scholar]
- 124.Kontogianni K, Gerovasili V, Gompelmann D, et al. Coil therapy for patients with severe emphysema and bilateral incomplete fissures – effectiveness and complications after 1-year follow-up: a single-center experience. Int J Chron Obstruct Pulmon Dis 2017; 12: 383–394. doi: 10.2147/COPD.S117655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Gulsen A. Bronchoscopic lung volume reduction using coil therapy: complications and management. Adv Respir Med 2020; 88: 433–442. doi: 10.5603/ARM.a2020.0152 [DOI] [PubMed] [Google Scholar]
- 126.Gompelmann D, Eberhardt R, Ernst A, et al. The localized inflammatory response to bronchoscopic thermal vapor ablation. Respiration 2013; 86: 324–331. doi: 10.1159/000354175 [DOI] [PubMed] [Google Scholar]
- 127.Snell GI, Hopkins P, Westall G, et al. A feasibility and safety study of bronchoscopic thermal vapor ablation: a novel emphysema therapy. Ann Thorac Surg 2009; 88: 1993–1998. doi: 10.1016/j.athoracsur.2009.06.038 [DOI] [PubMed] [Google Scholar]
- 128.Snell G, Herth FJF, Hopkins P, et al. Bronchoscopic thermal vapour ablation therapy in the management of heterogeneous emphysema. Eur Respir J 2012; 39: 1326–1333. doi: 10.1183/09031936.00092411 [DOI] [PubMed] [Google Scholar]
- 129.Gompelmann D, Shah PL, Valipour A, et al. Bronchoscopic thermal vapor ablation: best practice recommendations from an expert panel on endoscopic lung volume reduction. Respiration 2018; 95: 392–400. doi: 10.1159/000489815 [DOI] [PubMed] [Google Scholar]
- 130.Shah PL, Gompelmann D, Valipour A, et al. Thermal vapour ablation to reduce segmental volume in patients with severe emphysema: STEP-UP 12-month results. Lancet Respir Med 2016; 4: e44–e45. doi: 10.1016/S2213-2600(16)30199-0 [DOI] [PubMed] [Google Scholar]
- 131.Rathinam S, Oey I, Steiner M, et al. The role of the emphysema multidisciplinary team in a successful lung volume reduction surgery programme. Eur J Cardiothorac Surg 2014; 46: 1021–1026. doi: 10.1093/ejcts/ezu129 [DOI] [PubMed] [Google Scholar]
- 132.Chew J, Mahadeva R. The role of a multidisciplinary severe chronic obstructive pulmonary disease hyperinflation service in patient selection for lung volume reduction. J Thorac Dis 2018; 10: S3335–S3343. doi: 10.21037/jtd.2018.07.36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Wightman SC, McKenna RJ. Value of a multidisciplinary team approach to treatment of emphysema. Thorac Surg Clin 2021; 31: 171–175. doi: 10.1016/j.thorsurg.2021.02.004 [DOI] [PubMed] [Google Scholar]
- 134.Hazelett BN, Paton A, Majid A, et al. Nurse coordinator roles and responsibilities for bronchoscopic lung volume reduction with endobronchial valves. Chest 2021; 159: 2090–2098. doi: 10.1016/j.chest.2020.11.041 [DOI] [PubMed] [Google Scholar]
- 135.van der Molen MC, Hartman JE, Vanfleteren LEGW, et al. Reduction of lung hyperinflation improves cardiac preload, contractility, and output in emphysema: a clinical trial in patients who received endobronchial valves. Am J Respir Crit Care Med 2022; 206: 704–711. doi: 10.1164/rccm.202201-0214OC [DOI] [PubMed] [Google Scholar]
- 136.Hartman JE, Garner JL, Shah PL, et al. New bronchoscopic treatment modalities for patients with chronic bronchitis. Eur Respir Rev 2021; 30: 200281. doi: 10.1183/16000617.0281-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Stolz D, Mkorombindo T, Schumann DM, et al. Towards the elimination of chronic obstructive pulmonary disease: a Lancet Commission. Lancet 2022; 400: 921–972. doi: 10.1016/S0140-6736(22)01273-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Dauriat G, Mal H, Jebrak G, et al. Functional results of unilateral lung volume reduction surgery in ɑ1-antitrypsin deficient patients. Int J Chron Obstruct Pulmon Dis 2006; 1: 201–206. doi: 10.2147/copd.2006.1.2.201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Stoller JK, Gildea TR, Ries AL, et al. Lung volume reduction surgery in patients with emphysema and α1-antitrypsin deficiency. Ann Thorac Surg 2007; 83: 241–251. doi: 10.1016/j.athoracsur.2006.07.080 [DOI] [PubMed] [Google Scholar]
- 140.Everaerts S, Hartman JE, Van Dijk M, et al. Bronchoscopic lung volume reduction in patients with emphysema due to ɑ1-antitrypsin deficiency. Respiration 2023; 102: 134–142. doi: 10.1159/000528182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Siaplaouras J, Heckmann M, Reiss I, et al. Lung volume reduction surgery in bronchopulmonary dysplasia. Acta Paediatr 2003; 92: 754–756. [DOI] [PubMed] [Google Scholar]
- 142.de Laffolie J, Hirschburger M, Bauer J, et al. Lung volume reduction surgery in preterm infants with bronchopulmonary dysplasia. A case report. Clin Case Rep 2013; 1: 96–99. doi: 10.1002/ccr3.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Sohn B, Park S, Park IK, et al. Lung volume reduction surgery for respiratory failure in infants with bronchopulmonary dysplasia. Pediatrics 2018; 141: Suppl. 5, S395–S398. doi: 10.1542/peds.2016-3901 [DOI] [PubMed] [Google Scholar]
- 144.Inci I, Iskender I, Ehrsam J, et al. Previous lung volume reduction surgery does not negatively affect survival after lung transplantation. Eur J Cardiothorac Surg 2018; 53: 596–602. doi: 10.1093/ejcts/ezx318 [DOI] [PubMed] [Google Scholar]
- 145.Fuehner T, Clajus C, Fuge J, et al. Lung transplantation after endoscopic lung volume reduction. Respiration 2015; 90: 243–250. doi: 10.1159/000434685 [DOI] [PubMed] [Google Scholar]
- 146.Slama A, Ceulemans LJ, Hedderich C, et al. Lung volume reduction followed by lung transplantation in emphysema—a multicenter matched analysis. Transpl Int 2022; 35: 10048. doi: 10.3389/ti.2022.10048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Krishnan A, Chidi A, Merlo CA, et al. Lung volume reduction surgery before lung transplantation: a propensity-matched analysis. Ann Thorac Surg 2022; 113: 491–497. doi: 10.1016/j.athoracsur.2021.02.009 [DOI] [PubMed] [Google Scholar]
- 148.Dooms C, Blondeel A, Ceulemans LJ, et al. Lung volume reduction in emphysema: a pragmatic prospective cohort study. ERJ Open Res 2021; 7: 00877-2020. doi: 10.1183/23120541.00877-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Buttery S, Kemp SV, Shah PL, et al. CELEB trial: comparative effectiveness of lung volume reduction surgery for emphysema and bronchoscopic lung volume reduction with valve placement: a protocol for a randomised controlled trial. BMJ Open 2018; 8: e021368. doi: 10.1136/bmjopen-2017-021368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Buttery SC, Banya W, Bilancia R, et al. Lung volume reduction surgery versus endobronchial valves: a randomised controlled trial. Eur Respir J 2023; 61: 2202063. doi: 10.1183/13993003.02063-2022 [DOI] [PMC free article] [PubMed] [Google Scholar]