Abstract
Objectives
Vertigo describes symptoms of abnormal movement of the environment or the patient's own body. As such, it affects patients' quality of life, prevents them from following their daily activities, and increases healthcare utilization. The Global Burden of Disease Project aims to quantify morbidity and mortality worldwide. In 2013, a separate disability weight for vertigo was introduced. The aim of this study is to estimate the symptom burden of disease caused by vertigo.
Methods
This study analyzes data from the Gutenberg Health Study (GHS). The GHS is a population‐based cohort study representative of the city of Mainz and its district. Participants were asked whether they suffered from vertigo and, if so, how bothered they felt by it, rating their distress on a six‐level scale from 1 = little stressful to 6 = extremely stressful.
Results
Eight thousand five hundred and nineteen participants could be included in the study. The overall prevalence of vertigo was 21.6% (95%‐confidence interval [CI] [20.7%; 22.5%]). Vertigo prevalence peaked in the age group of 55–64 years. Vertigo annoyance averaged 2.42 (1.28). When an annoyance of 3–6 was considered bothersome, the prevalence of bothersome vertigo was 8.1 % (95%‐CI [7.5%; 8.7%]). Age‐standardized to the European Standard Population 2013, vertigo caused a burden of 2102 years lived with disability per 100,000 population.
Conclusion
In this study, it was found that one in five people suffer at least occasionally from vertigo. This result suggests a significant burden of disease. This burden is reported at the symptom level. Future studies are needed to attribute the burden to specific causes.
Level of Evidence
2.
Keywords: cohort study, global burden of disease, otology/neurotology, vertigo
Assuming a high prevalence of vertigo, it remains unclear how much its morbidity contributes to the global burden of disease. This study calculated the number of years lived with disability as a general measure of morbidity. We could show that vertigo thus contributes significantly to the overall disease burden.
1. INTRODUCTION
The term vertigo summarizes sensations of abnormal movement. This movement may be perceived as either a rotation or swaying of one's own body or the environment. 1 As such, it is a subtype of dizziness, which encompasses a wide range of feelings of weakness, faintness, or unsteadiness. 2 Because of linguistic and cultural differences in the definition of the two terms, reported prevalence figures vary widely. 3 While dizziness occurs with a lifetime prevalence of 17% to 30%, the prevalence of vertigo ranges from 3% to 10%. 3 With an increasing prevalence in the elderly and an aging of the general population, we must expect a further rise in the prevalence of vertigo. 4 , 5
Vertigo can have multiple causes. When diagnosing a patient who complains of vertigo, the clinician must distinguish between central and peripheral causes, as central causes may require emergency care. Vertigo, as opposed to dizziness, is thought to be more commonly associated with peripheral lesions, although this understanding is not true for all patients. 6 , 7
Regardless of the cause, vertigo is an important symptom that increases health care utilization. 8 , 9 , 10 It decreases patients' quality of life and hinders them in activities of daily living. 6 , 11 , 12 , 13 In addition, vertigo is an important risk factor for falls and thus may further increase morbidity and mortality. 14 , 15 , 16
Historically, mortality rates have been reported as the primary outcome in tracking the global burden of disease with a focus on communicable diseases. 17 With the increase in non‐communicable morbidity, reporting years lived with disability (YLD) is evolving to set the research agenda. Therefore, to better understand the burden of disease caused by non‐communicable and non‐fatal health outcomes, the Global Burden of Disease project (GBD) included vertigo as a new health state in the 2013 update. 18 In 2017, vertigo was reported as part of “other sense organ disease” which groups acute and chronic sensory organ diseases. 17 Here, vertigo was included only in chronic sensory organ diseases and is the only cause classified as moderate (out of three groups—mild, moderate, and asymptomatic). With the classification as moderate, vertigo represents a 0.21 proportion of the chronic sensory organ disease. 17 Vertigo was assigned a disability weight (DW) of 0.113.
This study is the first to report the burden of disease for vertigo. Due to its population‐based design, the results of the study can be generalized to the population in Germany and Europe, contributing to the aim of understanding the overall burden of disease in these regions.
2. MATERIALS AND METHODS
The Gutenberg Health Study (GHS) is a large population‐based cohort study located at the University Hospital Mainz, Germany. The study's population sample was randomly drawn from the residents' registration office and 1:1 stratified for sex, age decade, and residency (rural vs. urban). By this population‐based design, the GHS is representative for the population of Mainz and its district Mainz‐Bingen. Exclusion criteria were physical or mental disabilities that might prevent the participant from arriving at the study center in order to take part. A further exclusion criterion was insufficient knowledge of the German language since all questionnaires are applied in German. A detailed description of the study's design can be found elsewhere. 19 , 20
The GHS was initiated in 2007 and between 2007 and 2012 the first cohort (core cohort, n=15,010) was studied. After five years, an initial follow‐up survey was conducted via computer‐assisted telephone interviews. During the first 10‐year follow‐up (10‐FU, 2017 to 2020), all participants were invited to revisit the study site. This 10‐FU introduced an auditory questionnaire included an audiological testing station. In the latter, participants completed pure‐tone audiometry (air and bone conduction) and a German matrix test (Oldenburg Sentence Test). In addition, a picture of the tympanic membrane was taken. In the 10‐FU, additionally to the core cohort, further participants in the age groups of 25 to 44 years (young cohort, n = 4000) and 75 to 85 years (senior cohort, n = 1000) were invited to take part. Participants were asked “Do you regularly experience rotating or swaying vertigo (longer than 30 seconds)?” (yes/no). If yes, they were asked “How much do you feel bothered by it?” They were requested to rate their vertigo on a six‐level scale ranging from “little stressful” (=1) to “extremely stressful” (=6).
The prevalence of vertigo as well as its related stress are reported stratified by sex and age decade. In order to report disease burden, disability‐adjusted life years (DALYs) were calculated as follows:
YLL is assumed to be zero since vertigo depicts a symptom that only causes morbidity. However, underlying causes of vertigo might cause mortality, but the differential diagnoses of vertigo will not further be differentiated in this analysis. With YLL=0, DALY=YLD. For calculating YLD, we used the DW of 0.113 from the GBD update 2013, which includes all grades of severity. 18 We also used a pure prevalence‐based approach utilizing point‐prevalences. The duration of the overall health state of vertigo was set to one year, although the symptom is characterized by recurrent short spells of vertigo (at least 30 s) with a symptom‐free interval in between.
The results were generalized to a reference population of the European Standard Population (ESP) 2013 and the German Standard Population (GSP) 2021 by adjusting the cohort's age structure to the reference populations' age structure disaggregated by sex. Reporting these results make them more comparable to other GBD studies. All statistical analyses were done in R version 4.2.1 (2022‐06‐23, R Core Team (2022), Vienna, Austria).
The study was approved by the local institutional review board (Ethics Commission of the State Chamber of Physicians of Rhineland‐Palatine, reference no. 837.020.07) and was conducted in full compliance with the Declaration of Helsinki. Written informed consent was obtained from all subjects before participation in the study.
3. RESULTS
Nine thousand seven hundred and fifty two participants attended the GHS follow‐up and completed otolaryngologic testing. 1233 participants had to be retrospectively excluded for missing data on vertigo. Hence, 8519 participants could be included in the study. Of these, 4358 were males (51.2%) and 4161 females (48.8%). The average age in years was 60.7 (13.7; see Table 1).
TABLE 1.
Demographics and prevalence of vertigo.
| All (n) | Male (n) | Female (n) | p‐value | |
|---|---|---|---|---|
| n | 8519 | 4358 | 4161 | <.0001 |
| Average Age in years (SD) | 60.7 (13.7) | 61.4 (13.8) | 59.9 (13.5) | <.0001 |
| Vertigo prevalence % (n) | 21.6% (1840) | 19.7% (860) | 23.6% (980) | <.0001 |
| Vertigo annoyance 1–6 (SD) | 2.42 (1.28) | 2.36 (1.26) | 2.47 (1.31) | .056 |
Abbreviation: SD, standard deviation.
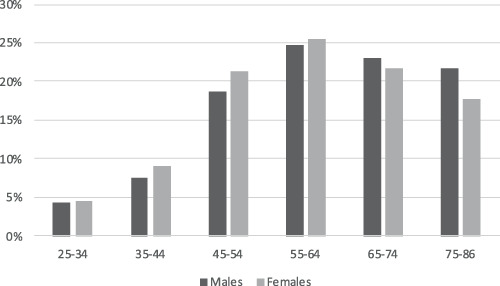
The prevalence of vertigo was 21.6% (n = 1840/8519; 95%‐confidence interval [95%‐CI] [20.7%; 22.5%]). Overall, women were significantly more likely to be affected than men (23.6% vs. 19.7%, p‐value <.0001). Vertigo prevalence peaked in the of 55–64 age group (Figure 1). From the age group of 65–74 years onwards, vertigo prevalence declined more in females as in males leading to a higher prevalence in males than in females for participants 65 years or older.
FIGURE 1.

Prevalence of vertigo for age groups (in years) and sex (males/females).
Among all participants, vertigo annoyance was 2.42 (1.28) (Figure 2). Females were more bothered by their vertigo than males, although this was not statistically significant (p‐value = .056). When considering a vertigo annoyance of 3–6 as bothersome vertigo, the prevalence of bothersome vertigo was 8.1% (7.0% for males and 9.3% for females, p‐value = .074).
FIGURE 2.

Vertigo annoyance (1 = little stressful to 6 = extremely stressful) for all and for both sexes (males, females).
When age‐standardizing these results according to the ESP 2013, overall vertigo prevalence was 18.6% (95%‐CI [17.8%;19.5%]). The prevalence, age‐standardized to the GSP, was 20.1% (95%‐CI [19.3%;21.0%]; see Table 2).
TABLE 2.
Vertigo prevalence age‐standardized to the ESP 2013 and GSP 2021.
| All [95%‐CI] | Male [95%‐CI] | Female [95%‐CI] | |
|---|---|---|---|
| European standard population 2013 | 18.6% [17.8%;19.5%] | 15.3% [14.3%;16.5%] | 21.9% [20.7%;23.2%] |
| German standard population 2021 | 20.1% [19.3%;21.0%] | 16.9% [15.8%;18.1%] | 23.2% [22.0%;24.5%] |
Abbreviation: CI, confidence interval.
In our study cohort, a total of 207.92 YLD were accumulated for vertigo by the participants (97.18 YLD for males and 110.74 YLD for females). Vertigo causes a total of 2101.8 YLD per 100,000 population weighted to the ESP 2013 (males: 1728.9 YLD per 100,000 population, females: 2474.7 YLD per 100,000 population). Age‐standardized to the GSP 2021, the overall burden of vertigo was 2271.3 YLD per 100,000 population (men: 1909.7 YLD per 100,000 population, women: 2621.6 per 100,000 population).
4. DISCUSSION
In this study, we found that one in five people occasionally suffers from vertigo. This leads to a symptom burden of 2101.8 YLD per 100,000 population in Europe. Females seem to be an especially vulnerable population since they show a significantly higher prevalence of vertigo and are more strained by their vertigo.
In its 2017 update, the GBD calculated a global YLD prevalence in thousands of 103,750.5 for other sense organ disease (including both acute and chronic states). Chronic other sense organ disease accounted for 84.6% of these YLD (namely 87,788.5). These results were similar for Western Europe (YLD prevalence in thousands of 8948.6 for other sense organ disease and 7971.8 for chronic other sense organ disease). 17 Vertigo is defined as moderate chronic other sense organ disease and holds a share of 0.21 of all chronic other sense organ disease YLD. The most recent GBD update did not distinguish between acute and chronic other sense organ disease. 21 They reported a global age‐standardized rate of 41.2 DALY per 100,000 population for all other sense organ disease. This rate was slightly higher when focusing on Germany and Western Europe (48.5 and 50.9, respectively). Hence, the burden of other sense organ disease was higher in these regions. Assuming a constant proportion of vertigo in these rates, the burden of vertigo is considerably lower than that reported in this study. This could be due to a smaller prevalence rate and adjustment for comorbidity. Direct comparison of rates is not possible because the YLD rate caused by vertigo alone has not been published to date and, to the best of our knowledge, this is the first study to report on it. In addition to this, in 2016, YLD rates were 10% higher in females than in males, indicating sex‐specific health disparities that we also see in the symptom of vertigo. 22
A recent report by Porst et al. reported the results of the BURDEN2020 project aiming to estimate the burden of disease in Germany. 23 The total burden of 19 major diseases was 14,584 DALY per 100,000 population (generalized to the ESP). Coronary heart disease (2321 DALY) was found to account for the largest share of the total burden, followed by low back pain (1735 DALY) and lung cancer (1197 DALY). Our results of 2101.8 YLD are in line with these results. However, as discussed further below in the limitation section, our report is a symptom‐based approach not attributable to a certain cause of vertigo (i.e., Meniere's disease). Although vertigo does not contribute to mortality, the overall prevalence of vertigo is high, resulting in a significant symptom burden.
The previous literature reports a prevalence of 15.8% to 36.2% for dizziness and/or vertigo. 13 , 24 , 25 , 26 , 27 When focusing on vertigo alone, the reported prevalence ranges from 3% to 10 %. 3 , 28 , 29 Our study shows a higher prevalence of 21.6%. This might be due to the average age of 60.7 years among our study participants and the fact that the age group of 55–64 years shows the highest prevalence of vertigo. In addition to this, as described above, the term vertigo is sensitive to cultural and linguistical differences. 30 Studies reporting on vertigo prevalence are therefore strongly depending on the exact wording in their interviews or questionnaires. 31 Study participants reporting upon their symptoms may not be aware of small distinctions. 32 Therefore, it is necessary to provide the exact wording of the questioning in the methods section to facilitate comparison with other studies. Prevalence estimates may be higher if no minimum symptom severity of vertigo is required in the questioning. 33 Therefore, we additionally reported results where only an annoyance of 3–6 is considered to be bothersome vertigo. The prevalence for bothersome vertigo was 8.1% and thereby significantly smaller. In addition, vertigo as a symptom cannot be clearly attributed to a defined clinical cause (e.g., vestibular deficit). Nevertheless, the aim of this study was to estimate the burden of disease caused by the health state of vertigo. Therefore, assignment to a specific cause is not required.
A particularly interesting finding of this study is that females were affected significantly more often than males. This is true up to the peak of prevalence in the age groups 55–64 years. From age 65 years, males showed a higher prevalence than females. Discussing sex differences of a symptom without attributing it to a specific cause is difficult. Previous epidemiological studies reported a predominance of vertigo in females, especially in the elderly population. 16 , 29 This is because vestibular causes such as vestibular migraine, Menière's disease, or benign paroxysmal positional vertigo are more common in females. 34 , 35 , 36 Whether hormonal differences increase the risk of vestibular disorders is controversial in the literature. 29 , 37 , 38 , 39 A higher prevalence of vertigo in the elderly could also be due to a higher prevalence of comorbidities and/or higher medication use due to comorbidities. 40 Further studies are needed to investigate this sex difference in vertigo prevalence.
This study contains a couple of limitations, which we will address below. In our methodology, we chose a pure prevalence‐based approach. At the beginning of the GBD study, an incidence‐based approach was used. In the 2010 study update, the methodology was revised and a prevalence‐based approach was introduced. 41 Subsequently, many national burden of disease studies that used the revised GBD study methodology adhered to this change in estimation. 42 , 43 , 44 The pure prevalence‐based approach estimates the burden of disease within the year of collection of the point‐prevalences. For shorter disease duration (i.e., for an acute health state, meaning less than one year), a fraction of that year is used. In general, it is recommended that pure prevalence‐based approaches be used to estimate the burden of disease in a given year and for non‐fatal diseases. 45 In this context, the choice of time horizon may influence study results and therefore need to be defined in the methodology. We calculated the burden of vertigo assuming that it accumulates over a one‐year period. Vertigo is a symptom that is often episodic and does not require patients to experience it throughout the year. In the GBD study, vertigo is defined as a chronic sensory organ disease (see introduction). The lay description of vertigo on which the DW is based, is as follows: “has short spells of dizziness and loss of balance; between spells the person is worried the spells will occur again.” 18 Therefore, even between acute episodes of vertigo, the patient suffers from anxiety or worries about the next episode. This is part of the symptom of vertigo and infringes on the patient's quality of life even between episodes. The lay description as given by the GBD may not apply to every individual in a clinical context, but from a population‐based perspective that includes a large number of participants, this definition will hopefully approximate. It needs to be kept in mind that vertigo as a symptom cannot be differentiated at the causative level. In addition to that, we did not adjust for comorbidities as the GBD does. 22 , 23 This decision is based on the fact that we do not want to report on the overall burden of disease, as Porst et al. did, but only to add the burden of vertigo to the literature. As a burden of disease report, this study does not provide further information on the causes of vertigo, but is a report on the burden of disease at the symptom‐level.
5. CONCLUSION
Vertigo contributes significantly to the overall burden of disease. To our knowledge, this is the first study establishing the burden of disease for vertigo based on the GBD methodology. Even though vertigo does not cause direct mortality, its morbidity still depicts a significant burden due to its high prevalence and should therefore be regarded as a major contributor to the overall burden of disease. Further studies are needed to make results comparable and should include further examinations to differentiate vertigo by its cause even on an epidemiological level.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interest to declare.
ACKNOWLEDGMENTS
The Gutenberg Health Study (GHS) is funded through the government of Rhineland‐Palatinate (“Stiftung Rheinland‐Pfalz für Innovation”, contract AZ 961‐386261/733), the research programs “Wissen schafft Zukunft” and “Center for Translational Vascular Biology (CTVB)” of the Johannes Gutenberg‐University of Mainz, and its contracts with Boehringer Ingelheim, and PHILIPS Medical Systems, including an unrestricted grant for the Gutenberg Health Study. Philipp S Wild is funded by the Federal Ministry of Education and Research (BMBF 01EO1503). Philipp S Wild and Thomas Münzel are PI of the German Center for Vascular Research (DZHK Rhein Main).
Hackenberg B, O'Brien K, Döge J, et al. Vertigo and its burden of disease—Results from a population‐based cohort study. Laryngoscope Investigative Otolaryngology. 2023;8(6):1624‐1630. doi: 10.1002/lio2.1169
REFERENCES
- 1. Strupp M, Brandt T. Diagnosis and treatment of vertigo and dizziness. Dtsch Arztebl Int. 2008;105:173‐180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Baloh RW. Vertigo. Lancet. 1998;352:1841‐1846. [DOI] [PubMed] [Google Scholar]
- 3. Murdin L, Schilder AG. Epidemiology of balance symptoms and disorders in the community: a systematic review. Otol Neurotol. 2015;36:387‐392. [DOI] [PubMed] [Google Scholar]
- 4. Fernández L, Breinbauer HA, Delano PH. Vertigo and dizziness in the elderly. Front Neurol. 2015;6:144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Maarsingh OR, Dros J, Schellevis FG, van Weert HC, Bindels PJ, Horst HE. Dizziness reported by elderly patients in family practice: prevalence, incidence, and clinical characteristics. BMC Fam Pract. 2010;11:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Neuhauser HK, Radtke A, von Brevern M, Lezius F, Feldmann M, Lempert T. Burden of dizziness and vertigo in the community. Arch Intern Med. 2008;168:2118‐2124. [DOI] [PubMed] [Google Scholar]
- 7. Newman‐Toker DE, Dy FJ, Stanton VA, Zee DS, Calkins H, Robinson KA. How often is dizziness from primary cardiovascular disease true vertigo? A systematic review. J Gen Intern Med. 2008;23:2087‐2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rieger A, Mansmann U, Maier W, et al. Management of patients with the cardinal symptom dizziness or vertigo. Gesundheitswesen. 2014;76:e32‐e38. [DOI] [PubMed] [Google Scholar]
- 9. Kovacs E, Wang X, Grill E. Economic burden of vertigo: a systematic review. Heal Econ Rev. 2019;9:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Benecke H, Agus S, Kuessner D, Goodall G, Strupp M. The burden and impact of Vertigo: findings from the REVERT patient registry. Front Neurol. 2013;4:136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ciorba A, Bianchini C, Scanelli G, Pala M, Zurlo A, Aimoni C. The impact of dizziness on quality‐of‐life in the elderly. Eur Arch Otorhinolaryngol. 2017;274:1245‐1250. [DOI] [PubMed] [Google Scholar]
- 12. Bronstein AM, Golding JF, Gresty MA, et al. The social impact of dizziness in London and Siena. J Neurol. 2010;257:183‐190. [DOI] [PubMed] [Google Scholar]
- 13. Gopinath B, McMahon CM, Rochtchina E, Mitchell P. Dizziness and vertigo in an older population: the Blue Mountains prospective cross‐sectional study. Clin Otolaryngol. 2009;34:552‐556. [DOI] [PubMed] [Google Scholar]
- 14. Agrawal Y, Carey JP, Della Santina CC, Schubert MC, Minor LB. Disorders of balance and vestibular function in US adults: data from the National Health and Nutrition Examination Survey, 2001–2004. Arch Intern Med. 2009;169:938‐944. [DOI] [PubMed] [Google Scholar]
- 15. Siracuse JJ, Odell DD, Gondek SP, et al. Health care and socioeconomic impact of falls in the elderly. Am J Surg. 2012;203:335‐338. discussion 338. [DOI] [PubMed] [Google Scholar]
- 16. Lin HW, Bhattacharyya N. Impact of dizziness and obesity on the prevalence of falls and fall‐related injuries. Laryngoscope. 2014;124:2797‐2801. [DOI] [PubMed] [Google Scholar]
- 17. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators . Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789‐1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Salomon JA, Haagsma JA, Davis A, et al. Disability weights for the Global Burden of Disease 2013 study. Lancet Glob Health. 2015;3:e712‐e723. [DOI] [PubMed] [Google Scholar]
- 19. Wild PS, Zeller T, Beutel M, et al. The Gutenberg health study. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2012;55:824‐829. [DOI] [PubMed] [Google Scholar]
- 20. Hackenberg B, Döge J, Lackner KJ, et al. Hearing loss and its burden of disease in a large German cohort‐hearing loss in Germany. Laryngoscope 2021;132:1843‐1849. [DOI] [PubMed] [Google Scholar]
- 21. GBD 2019 Diseases and Injuries Collaborators . Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204‐1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1211‐1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Porst M, Lippe EV, Leddin J, et al. The burden of disease in Germany at the National and Regional Level‐Results in Terms of Disability–Adjusted Life Years (DALY) from the BURDEN 2020 study. Dtsch Arztebl Int. 2022;119(46):785‐792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kroenke K, Price RK. Symptoms in the community. Prevalence, classification, and psychiatric comorbidity. Arch Intern Med. 1993;153:2474‐2480. [PubMed] [Google Scholar]
- 25. Hannaford PC, Simpson JA, Bisset AF, Davis A, McKerrow W, Mills R. The prevalence of ear, nose and throat problems in the community: results from a national cross‐sectional postal survey in Scotland. Fam Pract. 2005;22:227‐233. [DOI] [PubMed] [Google Scholar]
- 26. Wiltink J, Tschan R, Michal M, et al. Dizziness: anxiety, health care utilization and health behavior—results from a representative German community survey. J Psychosom Res. 2009;66:417‐424. [DOI] [PubMed] [Google Scholar]
- 27. Mendel B, Bergenius J, Langius‐Eklöf A. Dizziness: a common, troublesome symptom but often treatable. J Vestib Res. 2010;20:391‐398. [DOI] [PubMed] [Google Scholar]
- 28. Kruschinski C, Kersting M, Breull A, Kochen MM, Koschack J. Hummers‐Pradier E. [Frequency of dizziness‐related diagnoses and prescriptions in a general practice database]. Z Evid Fortbild Qual Gesundhwes. 2008;102:313‐319. [DOI] [PubMed] [Google Scholar]
- 29. Neuhauser HK, von Brevern M, Radtke A, et al. Epidemiology of vestibular vertigo: a neurotologic survey of the general population. Neurology. 2005;65:898‐904. [DOI] [PubMed] [Google Scholar]
- 30. Neuhauser HK. The epidemiology of dizziness and vertigo. Handb Clin Neurol. 2016;137:67‐82. [DOI] [PubMed] [Google Scholar]
- 31. Maarsingh OR, Dros J, Schellevis FG, et al. Causes of persistent dizziness in elderly patients in primary care. Ann Fam Med. 2010;8:196‐205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Newman‐Toker DE, Cannon LM, Stofferahn ME, Rothman RE, Hsieh YH, Zee DS. Imprecision in patient reports of dizziness symptom quality: a cross‐sectional study conducted in an acute care setting. Mayo Clin Proc. 2007;82:1329‐1340. [DOI] [PubMed] [Google Scholar]
- 33. Bittar RS, Oiticica J, Bottino MA, Ganança FF, Dimitrov R. Population epidemiological study on the prevalence of dizziness in the city of São Paulo. Braz J Otorhinolaryngol. 2013;79:688‐698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Katsarkas A. Benign paroxysmal positional vertigo (BPPV): idiopathic versus post‐traumatic. Acta Otolaryngol. 1999;119:745‐749. [DOI] [PubMed] [Google Scholar]
- 35. Radtke A, Lempert T, Gresty MA, Brookes GB, Bronstein AM, Neuhauser H. Migraine and Ménière's disease: is there a link? Neurology. 2002;59:1700‐1704. [DOI] [PubMed] [Google Scholar]
- 36. Neuhauser H, Leopold M, von Brevern M, Arnold G, Lempert T. The interrelations of migraine, vertigo, and migrainous vertigo. Neurology. 2001;56:436‐441. [DOI] [PubMed] [Google Scholar]
- 37. Andrews JC, Ator GA, Honrubia V. The exacerbation of symptoms in Menière's disease during the premenstrual period. Arch Otolaryngol Head Neck Surg. 1992;118:74‐78. [DOI] [PubMed] [Google Scholar]
- 38. Rybak LP. Metabolic disorders of the vestibular system. Otolaryngol Head Neck Surg. 1995;112:128‐132. [DOI] [PubMed] [Google Scholar]
- 39. Vessey M, Painter R. Oral contraception and ear disease: findings in a large cohort study. Contraception. 2001;63:61‐63. [DOI] [PubMed] [Google Scholar]
- 40. Bisdorff A, Bosser G, Gueguen R, Perrin P. The epidemiology of vertigo, dizziness, and unsteadiness and its links to co‐morbidities. Front Neurol. 2013;4:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2163‐2196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ciobanu LG, Ferrari AJ, Erskine HE, et al. The prevalence and burden of mental and substance use disorders in Australia: findings from the Global Burden of Disease Study 2015. Aust N Z J Psychiatry. 2018;52:483‐490. [DOI] [PubMed] [Google Scholar]
- 43. Te Ao B, Tobias M, Ameratunga S, et al. Burden of traumatic brain injury in New Zealand: incidence, prevalence and disability‐adjusted life years. Neuroepidemiology. 2015;44:255‐261. [DOI] [PubMed] [Google Scholar]
- 44. Lee KS, Park JH. Burden of disease in Korea during 2000–10. J Public Health (Oxf). 2014;36:225‐234. [DOI] [PubMed] [Google Scholar]
- 45. Kim YE, Jung YS, Ock M, Yoon SJ. DALY Estimation Approaches: understanding and Using the Incidence‐based Approach and the Prevalence‐based Approach. J Prev Med Public Health. 2022;55:10‐18. [DOI] [PMC free article] [PubMed] [Google Scholar]


