Abstract
Eagle syndrome represents an anatomic variant present in 4% of the population. It is characterized by an elongated styloid process or ossified stylohyoid ligament with resultant irritation of cervical neurovascular structures. Common manifestations include craniofacial or cervical pain related to compression of the glossopharyngeal nerve. In rare cases, patients can present with a stroke or transient ischemic attack due to associated carotid artery injury. Fewer than 25 prior case reports describe vascular symptoms in the setting of associated carotid artery dissection and, in one case, a pseudoaneurysm. Our case report details the diagnosis and management of symptomatic carotid artery stenosis secondary to vascular Eagle syndrome.
Keywords: Carotid artery, Cerebrovascular disease, Stylocarotid
First described in 1937 by Dr. Watt Eagle, Eagle syndrome is characterized by a unilateral or bilateral elongated styloid process that causes compression of the nearby neurovascular structures.1 Since its identification, two distinct forms have been described: classic Eagle syndrome with characteristic pain arising from glossopharyngeal irritation and stylocarotid artery syndrome with compression and damage to the carotid artery.2,3 The styloid process ranges from 2.5 to 3 cm in length, on average, although most symptomatic patients have a styloid process measuring ≥4 cm.4 In the setting of stylocarotid artery syndrome, patients can experience transient compression of the internal carotid artery (ICA) with neck rotation or acute dissection related to cervical trauma.5 In symptomatic patients, duplex ultrasound combined with provocative maneuvers can suggest the diagnosis, and computed tomography angiography (CTA) can demonstrate bony abnormalities and arterial injury.6
The patient provided written informed consent for the report of his case details and imaging studies to describe the diagnosis and management of an uncommon cause of symptomatic carotid artery stenosis in the setting of chronic intermittent compression and trauma from an elongated styloid process.
Case report
The patient is a 48-year-old man with a history of hypertension, who reported acute onset monocular right-sided vision loss, which self-resolved within 5 to 10 minutes. The patient had a second episode of the same transient vision loss 5 days later, prompting him to visit his primary care physician, at which time, an outpatient carotid artery duplex ultrasound was obtained (Fig 1). The duplex ultrasound scan demonstrated findings concerning for near occlusion of the right ICA, and he was sent to the emergency room for emergent vascular surgery evaluation.
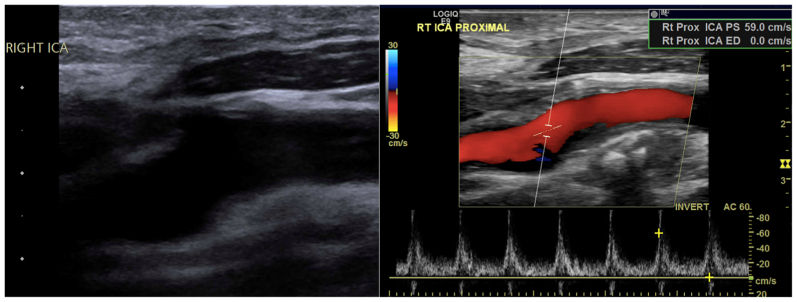
Fig 1.
Preoperative duplex ultrasound demonstrating a severely narrowed flow channel within the right (RT) internal carotid artery (ICA), with concern for possible occlusion in the proximal (P) ICA segment and a small flow channel observed distally in the mid-ICA segment (M).
CTA of the head and neck demonstrated minimal stenosis of the left ICA, a normal right common carotid artery, carotid bulb, and external carotid artery without evidence of atherosclerotic disease and a short segment with near occlusion of the proximal right ICA. Additionally, bilateral styloid processes were present, measuring ∼6 cm in length and adjacent to the vasculature (Figs 2 and 3). A review of the imaging studies and discussion with the otolaryngology team confirmed a diagnosis of Eagle syndrome. To prevent recurrent amaurosis fugax symptoms and possible future transient ischemic attack and/or stroke, the patient was taken for urgent right carotid endarterectomy and planned unilateral styloidectomy by the otolaryngology team.
Fig 2.
Coronal and sagittal cuts of computed tomography demonstrating the length of the styloid process (A; arrow) and carotid artery stenosis (B; arrow). EDV, End-diastolic velocity; PSV, peak systolic velocity.
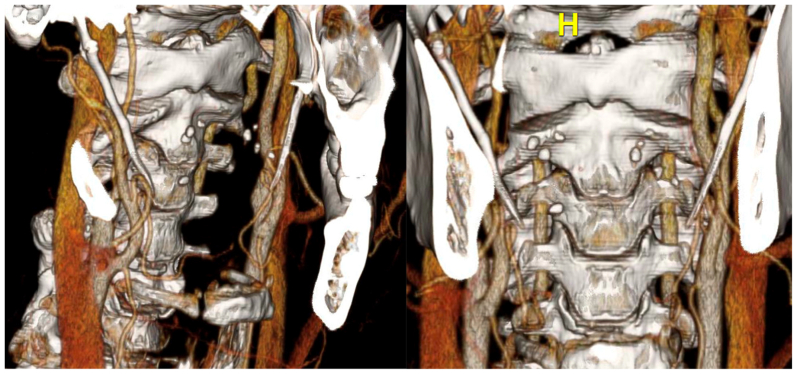
Fig 3.
Computed tomography angiography (CTA) reconstruction demonstrating bony abnormality and degree of carotid artery stenosis.
After a preoperative discussion with otolaryngology, the location of the offending styloid process and carotid stenosis were both located at the level of C3-C4, which would be amenable to standard orotracheal intubation and the use of a standard longitudinal carotid artery incision. Nasotracheal intubation and am alternate incision would have been considered if the lesion were more distal in the ICA. The patient was placed in a beach chair position, a shoulder roll was placed, and the head was rotated to the left to extend the neck. Intraoperative neuromonitoring of somatosensory evoked potentials and electroencephalography were used. Carotid artery exposure was completed through a traditional longitudinal neck incision overlying the anterior border of the sternocleidomastoid muscle. Carotid endarterectomy revealed no atherosclerotic disease but chronic inflammation and scarring were present, causing a near occlusion of a 1-cm segment of the ICA, with a normal caliber vessel proximal and distal to the lesion. A dissection plane was successfully developed between the media and adventitia, and endarterectomy with bovine pericardial patch angioplasty was completed without incident. There were no changes in the electroencephalogram during clamping, and no intimal flaps were seen on our completion intraoperative duplex ultrasound scan. Using the same incision, the otolaryngology surgeon was able to extend the transcervical exposure proximally with the assistance of bipolar electrocautery through division of the stylomandibular ligament, allowing for resection of 3 cm of the offending styloid process (Fig 4). Pathologic examination demonstrated rubbery tissue with fatty streaks (Fig 5).
Fig 4.
Photograph of resected right styloid process.
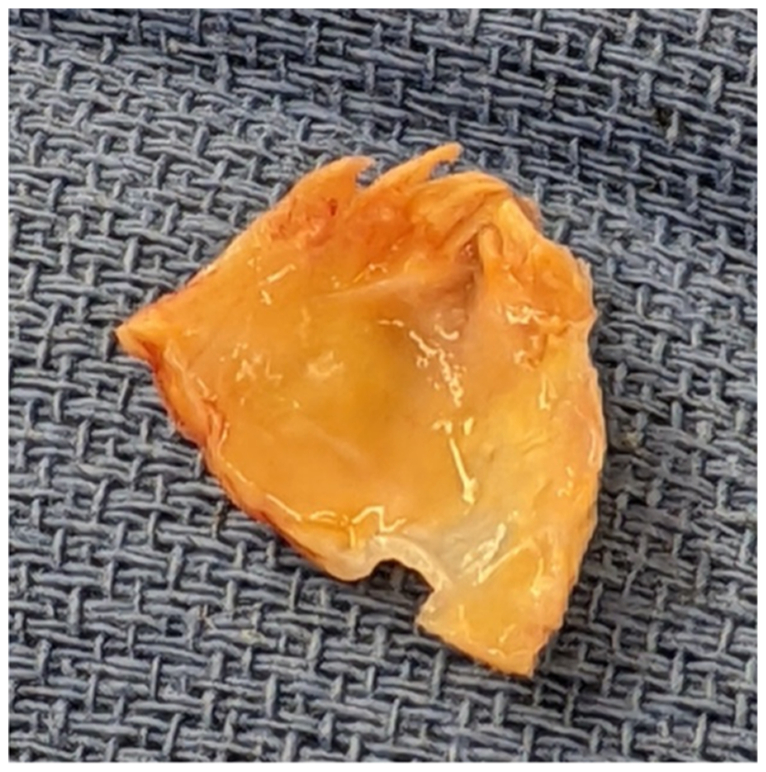
Fig 5.
Gross pathology from endarterectomy of right internal carotid artery (ICA).
Following surgery, the patient had an uneventful hospital course. The patient was discharged to home on postoperative day 1 with instructions to take daily aspirin and high-intensity statin therapy. The patient has since remained neurologically intact, with no stenosis in the right ICA and stable minimal stenosis of the contralateral carotid artery at his most recent follow-up, ∼20 months after the initial intervention (Fig 6). After extensive discussion regarding his options for prophylactic contralateral styloidectomy vs annual observation, the patient preferred to proceed with annual duplex ultrasound surveillance to monitor for worsening left carotid artery stenosis.
Fig 6.
Surveillance duplex ultrasound showing repaired right (RT) internal carotid artery (ICA) segment. Rt Prox ICA PS, right proximal internal carotid artery peak systolic velocity; Rt Prox ICA ED, right proximal internal carotid artery end-diastolic velocity.
Discussion
This case highlights some of the rare, but important, nuances associated with management of carotid artery occlusive disease. The initial carotid duplex ultrasound scan was considered to show a short segment occlusion of the proximal ICA; however, it was patent distally with antegrade flow. These are contradictory findings, because a typical carotid artery occlusion will thrombose from the proximal ICA to the ophthalmic artery. In cases of carotid artery occlusion, the standard is not to offer any surgical intervention due to the risk of an intraoperative embolus or intracerebral hemorrhage. CTA was necessary in the workup because it demonstrated the “string sign” and very large styloid processes bilaterally that seemed to overlap with the right near focal occlusion. The lack of disease in the remainder of his extracranial vessels suggested a more focal traumatic cause than a global atherosclerotic picture. Given these findings and his symptoms, we elected to operate, and the final pathologic examination of the occlusive carotid artery plaque confirmed the presence of chronic inflammation, indicating trauma and compression as the driving cause of the stenosis.
The exact cause of our patient's right ICA stenosis is unknown. He has minimal atherosclerotic risk factors, aside from mild hypertension. He did not have any new or prior trauma to his neck nor chiropractic manipulation to suggest a dissection. The patient is a dog trainer, and he repetitively turns his head over his right shoulder as opposed to the left. This could cause repetitive low-grade trauma to the artery over time and correlated with the affected side. Both the vascular and otolaryngology teams counseled the patient about possible prophylactic left styloidectomy to avoid trauma to the left ICA; however, the patient ultimately chose to have annual duplex ultrasound surveillance and wait until an issue occurred. The patient is very reliable and understands the risks of waiting.
Endovascular intervention was not considered for several reasons.7,8 The patient's young age and surgically accessible lesion made him an ideal candidate for standard carotid endarterectomy. Additionally, there was risk of stent compression and/or fracture due to the tough sclerotic plaque and persistent bony trauma from the styloid process. Given the severe stenosis driven by aberrant anatomy, open repair was chosen to simultaneously address the vessel stenosis and underlying anatomic cause.
Conclusions
Eagle syndrome represents a rare cause of symptomatic carotid artery disease and can be managed safely through traditional endarterectomy when combined with styloidectomy to prevent recurrent vascular injury. We would recommend preoperative involvement with a head and neck specialist to help determine the ideal sequence of the operation.
Disclosures
None.
Footnotes
The editors and reviewers of this article have no relevant financial relationships to disclose per the JVS policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Eagle W.W. Elongated styloid processes: report of two cases. Arch Otolaryngol Head Neck Surg. 1937;25:584–587. [Google Scholar]
- 2.Warrier A., Nanthini K.C., Subadra K., Harini D.M. Eagle’s syndrome: a case report of a unilateral elongated styloid process. Cureus. 2019;11 doi: 10.7759/cureus.4430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.David J., Lieb M., Rahimi S.A. Stylocarotid artery syndrome. J Vasc Surg. 2014;60:1661–1663. doi: 10.1016/j.jvs.2014.05.048. [DOI] [PubMed] [Google Scholar]
- 4.Esiobu P.C., Yoo M.J., Kirkham E.M., Zierler R.E., Starnes B.W., Sweet M.P. The role of vascular laboratory in the management of Eagle syndrome. J Vasc Surg Cases Innov Tech. 2018;4:41–44. doi: 10.1016/j.jvscit.2017.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mann A., Wood C., Carter R., Stark K., Kujath S., Friedell M. Eagle syndrome presenting after blunt trauma: a case series. J Vasc Surg. 2016;63:297–298. doi: 10.1016/j.avsg.2016.07.077. [DOI] [PubMed] [Google Scholar]
- 6.Li Z., Hua Y., Yang J., Li J. Ultrasound evaluation of transient ischemic attack caused by styloid process elongation: a case report. Front Neurol. 2019;10:26. doi: 10.3389/fneur.2019.00026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brott T.G., Hobson R.W., Howard G., et al. Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med. 2010;363:11–23. doi: 10.1056/NEJMoa0912321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baldino G., Di Girolamo C., De Blasis G., Gori A. Eagle syndrome and internal carotid artery dissection: description of five cases treated in two Italian institutions and review of the literature. Ann Vasc Surg. 2020;67:565.e17–565.e24. doi: 10.1016/j.avsg.2020.02.033. [DOI] [PubMed] [Google Scholar]