Abstract
Background
Self-care strategies can improve mental health and wellbeing, however, the evidence on preferred strategies among Arabic-speaking refugees and migrants is unclear. This mixed methods systematic review aimed to identify and synthesise the global research on mental health self-care strategies used by these populations.
Methods
English and Arabic language studies reporting on positive mental health self-care strategies to address symptoms of posttraumatic stress disorder, generalised anxiety and depression in the target populations were identified by systematically searching eight electronic databases and grey literature. Studies were deemed eligible if they were published from 2000 onwards and included Arabic-speaking migrants, refugees or asylum seekers aged 12 years and above. A narrative synthesis of study characteristics and relevant key findings was undertaken. The review protocol was registered on PROSPERO (registration number CRD42021265456).
Results
Fifty-nine records reporting 57 studies were identified, the majority appearing after 2019. There were 37 intervention studies that incorporated a self-care component and 20 observational studies that reported on self-generated self-care practices. Across both study types, four broad groups of mental health self-care were identified—social, psychological, religious/spiritual, and other (e.g., expressive arts and exercise). Psychological strategies were the most reported self-care practice overall and featured in all intervention studies. Religious/spiritual and social strategies were more common in the observational studies. Intervention studies in diverse settings reported statistical improvements on a range of outcome measures. Observational studies reported a range of individual and community benefits. Linguistic, cultural and religious considerations, inherent in the observational studies, were variably addressed in the individual and group interventions.
Conclusion
Overall, study participants experienced self-care as helpful although some encountered challenges in practicing their preferred strategies. Further research on mental health self-care strategies among Arabic-speaking refugees and migrants is needed in Western resettlement countries to guide mental health service delivery and primary healthcare initiatives for new arrivals and in transit countries.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-023-17395-9.
Keywords: Mental health, Self-care, Coping, Arabic-speaking, Refugee, Migrant, Global health, Systematic review
Introduction
The world is witnessing an unprecedented rise in the number of international migrants, refugees, and asylum seekers [1]. Forced migration is a growing concern and has been recognised as a major global health issue [2, 3]. By mid-2023, approximately 110 million individuals were forcibly displaced from their homes due to war, conflict or persecution, with 36.4 million recognised as refugees [4]. Many originate from countries where Arabic is widely spoken, such as Syria, accounting for the highest worldwide refugee population at 6.5 million [4].
Refugees and asylum seekers arrive in host countries carrying the psychological burden of their journeys [5]. Systematic reviews and meta-analyses indicate higher prevalence of mental disorders among refugees and asylum seekers than in the general population [6–9]. For example, a recent systematic review and meta-analysis of global refugee populations reported prevalence rates of 31.5% and 31% for depression and posttraumatic stress disorder (PTSD) respectively, compared with 12% and 3.9% for the general population [10]. Among adult Syrian refugees resettled in 10 countries, 43% had PTSD symptoms, 40% had depression and 26% had generalised anxiety disorder [11]. Overall, they were over 10 times more likely to develop PTSD and other mental disorders than the general population [11]. Adolescent refugees also experience challenges which can lead to increased prevalence of PTSD, depression and anxiety [12–14].
Psychological distress often exacerbates upon arrival in the host country due to legal and economic barriers, language barriers, discrimination and acculturation stress [15–17]. These stressors contribute to elevated risk of PTSD and depression among refugees and asylum seekers [18–20]. Migrants who move to another country for better economic, social or educational prospects face similar resettlement stressors, increasing their risk of mental disorders [21, 22]. Many experience discrimination and social exclusion, difficulties in finding work according to their education level and acculturation and adaptation stressors [23–25].
Given such findings, it is of concern that resettled refugees and migrants are significantly less likely to seek professional help or utilise mental health services than the general population [23, 26]. Within Western countries, commonly reported barriers to appropriate and timely treatment-seeking include language limitations, low mental health literacy, healthcare costs, uncertain migration status, unstable housing, limited transportation, poor understanding of healthcare services, discrimination from healthcare professionals and distrust of authority [27–34].
With limited access to culturally appropriate professional mental health services, those with, or at risk of, mental disorders may rely on self-care, self-help or self-management strategies as coping mechanisms. Such strategies can be practiced by individuals to manage or overcome their psychosocial distress with or without professional input [35–37]. ‘Self-care’ has become the preferred term in the global health literature. It is defined by the World Health Organization (WHO) as ‘the ability of individuals, families and communities to promote health, prevent disease, maintain health and cope with illness and disability with or without the support of a health worker’ [38, p.2]. At the base of the WHO service pyramid model, self-care is the foundation for all other forms of care and is critical to achieving optimal mental health [39]. The WHO model highlights the active role individuals with mental disorders can play in caring for themselves with the support of family and community [40]. Studies show that people with mild depression symptoms find informal self-care (without professional guidance) helpful and that such approaches can be cost-effective in reducing symptoms of depression and other mental disorders [41–43].
Currently, a comprehensive understanding of preferred mental health self-care strategies among Arabic-speaking refugees and migrants is lacking. This systematic review, which encompasses self-care strategies used both within people’s everyday lives and as part of therapeutic interventions, will have implications for mental health programs and service delivery, and for future research. At the individual level, self-care strategies can empower people to look after their mental health. At the service level, self-care interventions (therapeutic tools that support self-care practices) can offer cost-effective mental health and wellbeing outcomes, optimising healthcare services and resources [38]. This systematic review aimed to identify and examine the evidence for self-care strategies in these globally significant populations. The primary question was ‘What are the self-care strategies used to mitigate mental health issues within Arabic-speaking refugee and migrant populations globally?’ Related sub-questions were (i) What is the evidence for the effectiveness (presented as measures of outcome) of the identified strategies? (ii) What is the evidence for the cultural appropriateness of the identified strategies? and (iii) What positive and negative experiences are associated with the identified strategies?
Materials and methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidance was followed throughout this review [44]. The review protocol was registered on PROSPERO (registration number CRD42021265456) [45]. It is important to note that, although the term ‘self-help’ was used in the protocol title, the term ‘self-care’ as defined by the WHO is used here [38, 45].
Search strategy and selection criteria
Searches for peer-reviewed studies published from January 2000 to April 2023 were undertaken in eight digital databases: Ovid MEDLINE, Scopus, EMBASE, CINAHL, Web of Science, PTSDpubs (formerly known as PILOTS), PsycINFO, and Dar Al Mandumah (a set of Arabic databases). Non-indexed journals were searched using the Ulrichsweb database. Search terms were searched in titles, abstracts, and keywords. Supplementary searches included registered clinical trials, reference lists of included full-text articles and Google Scholar. We searched the web for non-government organisational reports and unpublished theses using Trove (Australian thesis database) and EThOS (British Library thesis database). The search queries were formulated to achieve all relevant results on self-care strategies and mental disorders (including all their term variants and most common synonyms) among Arabic-speaking refugees and migrants in both transit and resettlement countries. Specific search strategies are detailed in the protocol [45].
Inclusion criteria
Studies (quantitative, qualitative and mixed methods) were included if published in indexed or non-indexed journals in English or Arabic and focused on Arabic-speaking refugees, asylum seekers or migrants aged 12 years and older in any country, including countries of asylum/transit and resettlement. Studies were required to report mental health self-care strategies that address PTSD, depression, generalised anxiety disorder and panic disorder (common disorders in the target population). Psychotherapeutic interventions delivered by health professionals but having self-care components that could be applied by an individual independently (without professional involvement) were also included. We considered registered clinical trials and unpublished (grey) literature such as organisational and technical reports and dissertations.
Exclusion criteria
Reviews, editorials, commentaries, letters to the editor, newsletters, newspapers, magazine articles, and books or book chapters were excluded. Studies on Arabic-speaking refugees, asylum seekers and migrants aged below 12 years and non-Arabic speakers were excluded. Studies that exclusively reported the perspectives of those providing formal support (e.g., mental health professionals, migrant support workers and refugee resettlement workers), prevalence studies, and research focusing on interventions for physical health conditions or social issues were excluded.
Study selection
Systematic search results were first exported into Endnote to remove duplicates and then into Covidence (https://www.covidence.org/), an online screening and data extraction tool for systematic reviews. For English language articles, the first author and primary reviewer (DM) screened all titles and abstracts for eligibility. Full-text articles were double screened by two authors (DM and SSY) and discrepancies resolved by a third (IB). DM, SSY and IB double screened the grey literature titles and abstracts, and full texts. For Arabic language articles and dissertations, PHT performed the title-abstract and full-text screening. PHT also made English translations of the titles and abstracts, which were double screened by DM, SSY and IB.
Quality assessment
Quality assessment was undertaken using the Joanna Briggs Institute (JBI) Critical Appraisal Tools (https://jbi.global/critical-appraisal-tools) relevant to the study design. The JBI tools are study-specific for quantitative (e.g., randomised controlled trials or RCTs, quasi-experimental studies and cross-sectional studies) and qualitative research [46]. For English language articles, two authors (DM and SSY) independently conducted the quality appraisal of the studies with a third (IB) involved in resolving disagreements. For articles in Arabic, PHT performed the quality appraisal. Grey literature was appraised using the JBI tools (independently undertaken by DM, SSY and IB for English language studies and PHT for Arabic language studies). For the RCT tool with a possible total score of thirteen, scores of 7 or below were deemed low quality, 8–10 as medium, and 11 and above as high. For the cross-sectional tool, with a possible total of 8, scores of four or below were deemed low quality, 5–6 as medium, and 7 and above as high. For the quasi-experimental (possible total 9) and qualitative (possible total 10) tools, scores of five or below were deemed low quality, 6–7 as medium, 8 and above were deemed as high. No studies were excluded due to their quality.
Data extraction and synthesis
Relevant data were extracted by DM (English records) or PHT (Arabic). They included study characteristics, nature of self-care strategies, duration and mode of delivery, outcome measures, cultural appropriateness, and participant experience where reported. Our systematic review was designed to answer several interrelated questions. A narrative synthesis was undertaken due to the heterogeneity of study designs, which precluded meta-analysis. Narrative synthesis refers to ‘an approach to the systematic review and synthesis of findings from multiple studies that relies primarily on the use of words and text to summarise and explain the findings of the synthesis’ [47, p.5]. We focused on positive self-care strategies expected to have a beneficial effect on mental health and wellbeing, while excluding negative activities such as the consumption of tobacco, alcohol or drugs [48–55].
Results
Study characteristics
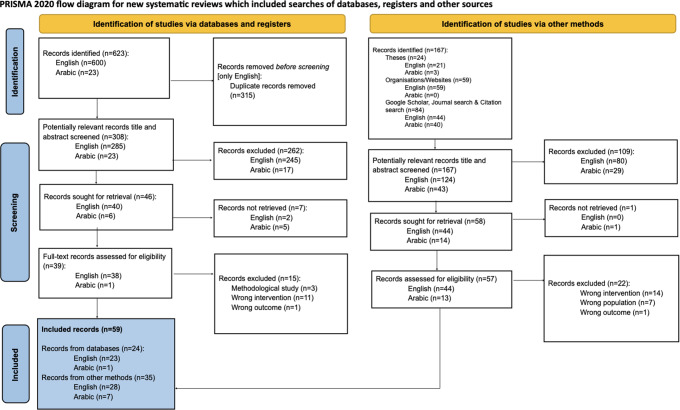
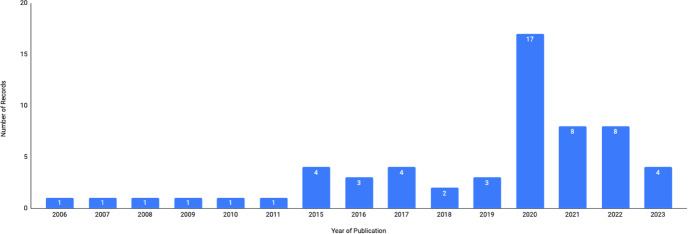
The review flowchart according to PRISMA [56] is presented in Fig. 1. Database searches yielded 623 records, with an additional 167 records identified through organisational reports, theses and manual citation searches. After removing duplicates and screening records for eligibility, we identified 96 records for full text screening. Fifty-nine records were eligible for inclusion. As Fig. 2 shows, most appeared after 2019 (n = 37). Five English language articles were authored by members of the research team (SSY, IB). One journal article and a dissertation discussed the same study [48, 49] and two articles [57, 58] reporting an intervention and the follow-up were considered as one study. The 57 discrete studies were categorised as observational (n = 20) or intervention (n = 37). Of the 20 observational studies, 14 used qualitative methods (semi-structured interviews, focus group discussions and ethnography), five used mixed methods and one was quantitative. Of the 37 intervention studies, 25 were quantitative (randomised controlled trials and quasi-experimental studies), eight were mixed methods and four were qualitative.
Fig. 1.
PRISMA flow diagram of the number of records identified, screened, assessed for eligibility and included in this review
Fig. 2.
Number of included records by year of publication
Table 1 summarises the characteristics of the included studies. A detailed description of each study is provided in S1 File. Studies were classified as high, middle-or low-income countries using the World Bank classification [59]. Fourteen observational studies were conducted in high-income countries (HICs) including Germany (n = 5) and United States (n = 4) [48, 49, 54, 55, 60–70]. Eighteen intervention studies were conducted in upper middle-income countries (UMICs) [57, 58, 71–87], majority in Jordan (n = 14). Sudan was the only low-income country (LIC). For this review, we considered HICs as resettlement countries. As shown in Table 1, all but one of the observational studies were deemed high quality. Of the 37 intervention studies, 25 were deemed as high quality and 12 as medium quality.
Table 1.
Characteristics of included studies by study type
| Author (Year) | Study Location | Study Type & Methods | Target Population | Sample Characteristics | JBI Quality Appraisal |
|---|---|---|---|---|---|
| Observational Studies (n = 20) | |||||
| Al-Ajarma (2010) | United States (HIC) | Qualitative: Narrative inquiry and semi-structured interviews | Palestinian graduate students |
n = 7 Age: 28-44 years Gender: 43% females Religion: not specified Education: 57% university Country of origin: 100% Palestine |
Qual = 9/10 High |
| Alhaddad et al. (2021) |
Germany (HIC) |
Qualitative: Semi-structured interviews | Newly arrived Syrian and Iraqi refugee youths |
n = 20 Age: 14–18 years (M = 16, SD = 1.7) Gender: 35% females Religion: 75% Islam, 10% Izidi, 15% none Education: 65% regular classes, 35% welcome classes Country of origin: 70% Syria, 30% Iraq |
Qual = 9/10 High |
| Boswall & Akash (2015) |
Jordan (UMIC) |
Qualitative: In-depth ethnography |
Syrian women and adolescent girls |
n = 50 Age: 14–66 years Gender: 100% females Religion: 100% religious Muslims Education: incomplete education levels Country of origin: 100% Syria |
Qual = 9/10 High |
| Chaaya et al. (2007) | Lebanon (UMIC) |
Mixed Methods: questionnaire and interviews |
Older adults in three poor suburbs of Beirut, one of which was a Palestinian refugee camp |
n = 246 (Palestinian refugees) Age: ≥60 years Gender: 54% females Religion: 100% Muslims Education: 40% literate Country of origin: 95% Palestine, 5% Lebanon |
Cross-sectional = 8/8 High Qual = 9/10 High |
| Darychuk & Jackson (2015) | West Bank/Palestine (LMIC) | Qualitative: Semi-structured interviews | Palestinian women in West Bank camps |
n = 31 Age: 22–48 years (M = 35) Gender: 100% females Religion: not specified Education: not specified Country of origin: 100% Palestine |
Qual = 10/10 High |
| Ferguson (2015) | United States (HIC) | Qualitative: Semi-structured interviews | Iraqi refugee men |
n = 10 Age: 18–60 years Gender: 0% females Religion: 50% Chaldeans, 50% Muslims Education: 10% primary, 90% post primary Country of origin: 100% Iraq |
Qual = 10/10 High |
| International Medical Corps (2017) |
Jordan (UMIC) |
Mixed Methods: Questionnaire, key informant interviews (KII) and focus group discussions (FGDs) | Syrian refugees in 11 cities and 2 camps and Jordanian nationals in same cities |
n = 6,375 Age: ≥18 years (M = 34, SD = 11) Gender: 59% females (Urban); 39% females (Camp) Religion: not specified Education: 90% formal (Urban); 79% formal education (Camp) Country of origin: Syria |
Cross-sectional = 8/8 High Qual = 9/10 High |
| International Medical Corps Lebanon (2011) | Lebanon (UMIC) | Qualitative: Semi-structured interviews | Forcibly displaced Syrians at Lebanon-Syria border |
n = 100 Age: 32 years (mean age only) Gender: 64% females Religion: 100% Sunni Muslims Education: 18% illiterate, 79% elementary & high school Country of origin: 100% Syria |
Qual = 7/10 Medium |
|
Irfaeya (2006) Irfaeya et al. (2008) |
Germany (HIC) |
Mixed Methods: Survey, KII and FGD | Arab migrant women in Cologne |
n = 116 Age: ≥18 years (M = 32) Gender: 100% females Religion: 100% Muslims Education: 8% illiterate, 68% school, 54% post school Country of origin: 31% Morocco, 23% other, 12% Lebanon, 9% Germany, 9% Tunisia, 9% Iraq, 8% Syria |
Cross-sectional = 6/8 Medium Qual = 9/10 High |
| Jamil (2020) |
Canada (HIC) |
Mixed Methods: Questionnaire and semi-structured interviews | First or 1.5 generation adult Arab immigrants |
Quantitative: n = 172 Age: ≥18 years (M = 30, SD = 13, range = 18–65) Gender: 58% females Religion: 67% Muslims, 33% Christians Education: 21% high school, 16% college, 49% university, 15% other Country of origin: 92% Middle Eastern, 9% North and East African Qualitative: n = 11 Age: ≥18 years (M = 29, SD = 10, range = 19–57) Gender: 55% females Religion: 82% Muslims, 9% Christians Education: 9% high school, 18% college, 18% university, 18% other Country of origin: 99% Middle Eastern |
Cross-sectional = 8/8 High Qual = 10/10 High |
| Kadri (2009) | New Zealand (HIC) | Qualitative: Semi-structured interviews | Arabic-speaking Muslim refugees from Arab/Muslim countries |
n = 31 Age: 16–52 years Gender: 52% females Religion: 100% religious Muslims Education: 3% no school, 71% school, 26% university Country of origin: 74.1% Iraq, 9.7% Kuwait, 6.5% Sudan, 6.5% Somalia, 3.2% Tunisia |
Qual = 10/10 High |
| Keshavarzi (2018) |
Canada (HIC) |
Qualitative: Semi-structured individual interviews | Recently arrived Muslim Arab Syrian refugees residing in Ontario |
n = 10 Age: 30–55 years Gender: 50% females Religion: 100% Sunni Muslims Education: 70% elementary to high school; 30% college and university Country of origin: 100% Syria |
Qual = 10/10 High |
| MakkiAlamdari (2020) | United States (HIC) | Quantitative: Cross-sectional study using questionnaire | War-affected Arab refugees in the US |
n = 130 Age: ≥18 years (M = 41, SD = 14, range = 18–72) Gender: 40% females Religion: not specified Education: 5% no school but literate, 47% school, 19% some college, 29% university Country of origin: 77% Middle Eastern countries, 23% African countries, 2% other |
Cross-sectional = 8/8 High |
| Nashwan et al. (2019) | United States (HIC) | Qualitative: Semi-structured interviews | Iraqi female refugees |
n = 22 Age: 50–63 years (M = 54.7, SD = 4.1) Gender: 100% females Religion: 77.3% Muslims, 22.7% Christians Education: 9.1% none, 72.7% primary/secondary education, 18.2% post-secondary/undergraduate degree Country of origin: 100% Iraq |
Qual = 9/10 High |
| Qureshi (2016) |
United Kingdom (HIC) |
Qualitative: Narrative inquiry and semi-structured interviews | Syrian male refugees |
n = 3 Age: 21-35 years Gender: 0% females Religion: not specified Education: 67% university Country of origin: Syria |
Qual = 10/10 High |
| Rayes et al. (2021) |
Germany (HIC) |
Qualitative: Semi-structured interviews | Arabic or Farsi speaking adults with refugee or asylum seeker status in Germany |
n = 17 Age: 22-47 years (M = 35) Gender: 35% females Religion: 100% Muslims, 12% non-religious (or non-practicing) Muslims Education: not specified Country of origin: 71% Syria, 29% Iraq |
Qual = 10/10 High |
| Renner et al. (2020) |
Germany (HIC) |
Qualitative: Semi-structured focus groups | Syrian refugees residing in Germany since 2015 |
n = 20 Age: ≥18 years (M = 28, SD = 9, range = 20–60) Gender: 20% females Religion: not specified Education: 30% university degree, 70% other Country of origin: 100% Syria |
Qual = 8/10 High |
| Sim et al. (2023) |
Canada (HIC) |
Mixed Methods: Quantitative: (survey) & Qualitative (open ended questions) | Arabic-speaking refugee parents experiencing depression and anxiety living in Canada |
n = 40 Age: ≥18 years (M = 43.3, SD = 7.81) Gender: 60% females Religion: not specified Education: 10% no formal education, 77.5% primary and secondary school, 12.5% post-secondary and above Country of origin: 82.5% Syria, 10% Iraq, 7.5% Sudan |
Cross-sectional = 6/8 Medium Qual = 9/10 High |
| Tauson (2017) | Thailand (UMIC) | Qualitative: Participant observation & in-depth interviews | Palestinian-Syrian refugees in Bangkok |
n = 9 Age: 20-50 years Gender: 22% females Religion: 100% Muslims Education: 11% tertiary education Country of origin: Palestine and Syria |
Qual = 10/10 High |
| Zbidat et al. (2020) |
Germany (HIC) |
Qualitative: Semi-structured interviews | Syrian refugees residing in Germany since 2014 or less |
n = 16 Age: ≥18 years (M = 36, SD = 11, range = 21–55) Gender: 50% females Religion: 81% Muslims, 13% Christians, 6% other Education: 43% school, 6% university degree, 18% other Country of origin: 100% Syria |
Qual = 10/10 High |
| Intervention Studies (n = 37) | |||||
| Acarturk et al. (2022) |
Turkey (UMIC) |
Quantitative: randomised controlled trial (RCT) | Arabic-speaking Syrian refugees |
Intervention n = 322 Age: ≥18 years (M = 31.2, SD = 9) Gender: 64% females Religion: 42% Muslims Education: 5.28% illiterate, 62.73% primary, 16.46% high school, 14.60% university Country of origin: 98.4% Syria, 1.2% Iraq |
RCT = 12/13 High |
| Ahmad et al. (2020) |
Egypt (LMIC) and Germany (HIC) |
Quantitative: Quasi-experimental (questionnaire) | Syrian refugee children from Egypt and Germany |
n = 16 Age: ≥14 years (M = 15, SD = 2, range = 14–18) Gender: 25% females (both Egypt and Germany) Religion: not specified Education: not specified Country of origin: 100% Syria |
Quasi-Experimental = 6/9 Medium |
| Aladdin & Hawamdeh (2021) |
Jordan (UMIC) |
Quantitative: RCT | Syrian refugee male students enrolled in the sixth and seventh grades |
n = 40 Age: ≥12 years (M = 13, SD = 1, range = 12–14) Gender: 0% females Religion: not specified Education: school Country of origin: 100% Syria |
RCT = 8/13 Medium |
| Al-Dmour & Al-Safasfeh (2020) |
Jordan (UMIC) |
Quantitative: RCT | Syrian refugee female students |
n = 30 Age: 12-15 years Gender: 100% females Religion: not specified Education: school Country of origin: 100% Syria |
RCT = 8/13 Medium |
| Al-Refai et al. (2022) |
Jordan (UMIC) |
Quantitative: RCT | Syrian refugees |
n = 36 Age: 18–60 years Gender: 50% females Religion: 100% Muslims Education: school Country of origin: 100% Syria |
RCT = 10/13 Medium |
| Al-Shahadat (2021) |
Jordan (UMIC) |
Quantitative: RCT | Syrian refugee female students enrolled in the 7th, 8th and 9th grade |
n = 30 Age: 13-16 years Gender: 100% females Religion: not specified Education: school Country of origin: 100% Syria |
RCT = 8/13 Medium |
| Alsheikh Ali (2020) |
Jordan (UMIC) |
Quantitative: Quasi-experimental (pre-posttest questionnaires) | Syrian refugee females in Jordan |
n = 40 Age: 30-50 years Gender: 100% females Religion: not specified Education: not specified Country of origin: 100% Syria |
Quasi-Experimental = 7/9 Medium |
| Blignault et al. (2019) |
Australia (HIC) |
Quantitative: Quasi-experimental (pre-post and follow-up questionnaire) | Arabic-speaking adults in Sydney |
n = 70 Age: 18–65 years Gender: 73% females Religion: 94% Muslims Education: 49% no post-school qualifications Country of origin: 79% Lebanon, 21% other |
Quasi-Experimental = 8/9 High |
| Blignault et al. (2021a) |
Australia (HIC) |
Mixed Methods: Quantitative Quasi-experimental (questionnaire) & Qualitative (participant feedback) | Arabic-speaking Muslim women in Sydney |
n = 20 [PPA] Age: 18-65 years Gender: 100% females Religion: 100% Muslims Education: 45% post-school qualifications Country of origin: 55% Iraq, 20% Lebanon, 15% Syria, 10% Libya |
Quasi-Experimental = 8/9 High Qual = 10/10 High |
| Blignault et al. (2021b) |
Australia (HIC) |
Mixed Methods: Quantitative (RCT) & Qualitative (participants’ log sheet comments) | Arabic-speaking community members in Sydney |
n = 131 Arabic speakers [PPA] Age: 14% 16-25 years, 24% 26-35 years, 17% 36-45 years, 45% other (M = 13) Gender: 83% females Religion: 63% Muslims, 37% Christians, 1% none Education: 45% Year 12 or less, 39% university, 14% trade certificate Country of origin: 29% Lebanon, 21% Australia, 49% other |
RCT = 9/13 Medium Qual = 10/10 High |
| Blignault et al. (2022) | Australia (HIC) | Mixed Methods: Quantitative (self-report questionnaires) and Qualitative (semi-structured interviews) | Arabic-speaking women in Australia |
n = 18 Age: 26–55 years Gender: 100% females Religion: 80.76% Muslims, 11.5% Christians Education: 69% post-school qualification Country of origin: 92% born overseas (Iraq, Lebanon, Syria) |
Quasi-experimental = 7/9 Medium Qual = 9/10 High |
|
Bryant et al. (2022a) Bryant et al. (2022b) |
Jordan (UMIC) | Quantitative: RCT | Arabic-speaking Syrian refugees living in Azraq Refugee Camp (Jordan) |
Intervention n = 204 Age: ≥18 years (M = 39.38, SD = 6.71) Gender: 71% females Religion: not specified Education: 27.5% none, 63.7% certificate, 6.8% secondary education, 2% university Country of origin: Syria |
RCT = 11/13 High |
| Cuijpers et al. (2022) | Lebanon (UMIC) | Quantitative: RCT | Arabic-speaking Syrian displaced people/refugees in Lebanon |
Intervention n = 283 Age: ≥18 years (M = 31.4, SD = 8.5) Gender: 61.7% females Religion: not specified Education: 67.9% school, 26.1% university, 6% other Country of origin: 100% Syria |
RCT = 12/13 High |
| de Graaff et al. (2020) | Netherlands (HIC) | Mixed Methods: Quantitative (RCT) and Qualitative (semi-structured interviews) | Adult Arabic-speaking Syrian refugees in Rotterdam, Netherlands |
Intervention n = 30 Age: ≥18 years (M = 37.6, SD = 11.8) Gender: 60% females Religion: not specified Education: 51.7% no or basic education, 24.1% secondary education and above Country of origin: Syria |
RCT = 11/13 High Qual = 8/10 High |
| de Graaff et al. (2023) | Netherlands (HIC) | Quantitative: RCT | Arabic-speaking Syrian refugees, experiencing symptoms of PTSD, depression and anxiety living in the Netherlands |
Intervention n = 103 Age: ≥18 years (M = 36.4, SD = 11.97, range = 18–69) Gender: 29.1% females Religion: not specified Education: 9.7% no or basic education, 20.4% technical/vocational/associate degrees, 69.9% secondary to tertiary education Country of origin: Syria |
RCT = 11/13 High |
| DePierro (2020) |
Jordan (UMIC) |
Quantitative: RCT | Syrian refugees, living in the Za’atri Refugee Camp in Jordan able to speak, read and write in Arabic |
n = 128 Age: ≥18 years Gender: 49% females Religion: not specified Education: 100% literate Country of origin: Syria |
RCT = 9/13 Medium |
| Doumit et al. (2020) | Lebanon (UMIC) | Quantitative: Quasi-experimental (questionnaires/surveys) | Adolescent Syrian refugees |
n = 31 [PPA] Age: 13-17 years (M = 14, SD = 1) Gender: 52% females Religion: not specified Education: school Country of origin: 100% Syria |
Quasi-Experimental = 8/9 High |
| Feen-Calligan et al. (2023) | United States (HIC) | Qualitative: Photovoice techniques | Arab American adolescents with refugee or immigrant background recently resettled in Michigan, US. |
n = 8 Age: 15–17 years Gender: 100% females Religion: 100% Muslims Education: school Countries of origin: Syria, Palestine, Yemen, Lebanon, United Arab Emirates, and Iraq |
Qual = 9/10 High |
| Gordon et al. (2016) | Gaza/Palestine (LMIC) | Quantitative: Quasi-experimental (questionnaire) | Palestinian adults in Gaza |
n = 92 Age: 18–49 years (M = 30) Gender: 58% females Religion: not specified Education: 51% school, 49% postsecondary Country of origin: Palestine |
Quasi-Experimental = 8/9 High |
| Hasha et al. (2022) |
Norway (HIC) |
Quantitative: RCT | Arabic-speaking adult Syrian refugees experiencing traumatic events |
Intervention n = 38 Age: ≥16 years (M = 33, SD = 10.4) Gender: 32% females Religion: not specified Education: years of education (M = 10, SD = 4.8) Country of origin: 100% Syria |
RCT = 10/13 Medium |
| Husby et al. (2020) |
Denmark (HIC) |
Mixed Methods: Quantitative Quasi-experimental (questionnaire survey) & Qualitative (focus group interviews) | Arabic-speaking adult refugees from Syria and Palestine, living in Denmark and had obtained asylum no more than 5 years before the intervention |
Quantitative n = 92 (Quant) Age: ≥18 years Gender: 64% females Religion: not specified Education: not specified Country of origin: 41% Syria, 2% Palestine Qualitative In FGDs, n = 32 |
Quasi-Experimental = 6/9 Medium Qual = 8/10 High |
| Ibrahim (2017) |
Sudan (LIC) |
Quantitative: Quasi-experimental (questionnaire) | Syrian refugees residing in Khartoum state, Sudan |
n = 20 Age: 20-60 years Gender: 55% females Religion: not specified Education: 90% primary, 10% high school Country of origin: 100% Syria |
Quasi-Experimental = 7/9 Medium |
| Kayrouz et al. (2015) |
Australia (HIC) |
Quantitative: Quasi-experimental (pre, post and follow-up test using questionnaire) | People of Arabic ancestry living in Australia (Australia or overseas born) |
n = 11 Age: 18-70 years (M = 34, SD = 9, range = 25–50) Gender: 73% females Religion: not specified Education: 73% Bachelor’s degree, 18% other Country of origin: Australia and overseas |
Quasi-Experimental = 8/9 High |
| Kayrouz et al. (2016) |
International (N/A) |
Quantitative: Quasi-experimental (pre, post and follow-up test using questionnaire) | People of Arabic ancestry living in Australia and elsewhere |
n = 36 Age: 18-70 years (M = 36, SD = 12, range = 19–67) Gender: 58% females Religion: not specified Education: 64% Bachelor’s degree, 36% other Country of origin: 53% Australia, 33% Middle Eastern countries (Lebanon, Egypt, Saudi Arabia), 5.5% UK, 5.5% USA, 3% Algeria |
Quasi-Experimental = 8/9 High |
| Lindegaard et al. (2020) |
Sweden (HIC) |
Quantitative: Pilot RCT | Refugees and immigrants able to read and write Arabic fluently in Sweden |
n = 59 Age: ≥18 years (M = 38, SD = 11, range = 20–69) Gender: 42% females Religion: not specified Education: 46% school, 46% completed or ongoing university education, 15% other Country of origin: not specified (78% refugee, 7% immigrant) |
RCT = 8/13 Medium |
| Lindegaard et al. (2021) |
Sweden (HIC) |
Qualitative: Semi-structured interviews |
Resettled refugees and immigrants, able to read and write Arabic residing in Sweden |
n = 10 Age: ≥18 years (M = 33, SD = 9, range = 20–49) Gender: 60% females Religion: not specified Education: 40% school, 50% completed or ongoing university education, 10% other Country of origin: not specified (80% refugees, 10% immigrant) |
Qual = 9/10 High |
| Mercy Corps (2020) |
Jordan, Lebanon, and Iraq (UMIC) |
Mixed Methods: Quantitative Quasi-experimental (survey) & Qualitative (KIIs and FGDs) | Adolescents and youths were a mix of Iraqi, Jordanian, Lebanese, Palestinian and Syrian, Arabs and Kurds, refugees, internally displaced people, and those from host communities |
Quantitative n = 1,607 Age: 12-19 years Gender: 41% females Religion: not specified Education: not specified Country of origin: 47% Lebanon, 39% Jordan 41% refugees, 45% from host communities Qualitative In KIIs n = 36; no precise gender breakdown for males and females In FGDs n = 32; 20 males, 12 females |
Quasi-Experimental = 7/9 Medium Qual = 9/10 High |
| Nilsson et al. (2019) |
Sweden (HIC) |
Qualitative: FGDs |
Arabic-speaking refugees, women and men |
n = 33 Age: >18 years (M = 45, range = 22–67) Gender: 30% females Religion: not specified Education: not specified Country of origin: Iraq, Syria, Lebanon, Jordan, or Palestine |
Qual = 10/10 High |
| Panter-Brick et al. (2018) |
Jordan (UMIC) |
Quantitative: RCT & Quasi-Experimental | Refugees (Syrian) and host-community (Jordanian) youth |
n = 463 Age: 12-18 years (M = 14, SD = 2) Gender: 47% females Religion: not specified Education: highest educational level (M = 7.04, SD = 2.15) Country of origin: 54% Syria |
RCT = 9/13 Medium Quasi-Experimental = 7/9 Medium |
| Powell et al. (2023) |
Jordan (UMIC) |
Qualitative: FGDs |
Resettled Syrian refugees and Jordanians, experiencing symptoms of depression and impaired functioning |
n = 21 Age: ≥18 years (M = 48) Gender: 66.7% females Religion: not specified Education: 14.3% no school, 61.9% secondary or high school, 19% some college Country of origin: 52% Jordan, 48% Syria |
Qual = 10/10 High |
| Raknes (2020) | Lebanon (UMIC) | Mixed Methods: Quantitative (questionnaire) & Qualitative (open-ended questions, session reports and interviews) | Syrian displaced and refugee adolescents living in Lebanese informal settlements |
n = 20 Age: 13-17 years (M = 14) Gender: 60% females Religion: not specified Education: 70% illiterate or nearly illiterate Country of origin: 100% Syria |
Quasi-Experimental = 6/9 Medium Qual = 9/10 High |
| Rayes (2017) |
Jordan (UMIC) |
Quantitative: Quasi-experimental (pre-post study using survey) | Syrian refugee adolescents in 3 urban districts and 2 camp settings |
n = 7,644 Age: 12-18 years Gender: 50% females Religion: not specified Education: not specified Country of origin: 100% Syria |
Quasi-Experimental = 8/9 High |
| Röhr et al. (2021) |
Germany (HIC) |
Quantitative: Pilot RCT |
Syrian refugees |
Intervention n = 65 Age: ≥18 years (M = 33, SD = 11, range 18–65) Gender: 34% females Religion: not specified Education: 42% high education level, 32% medium, 26% low Country of origin: 100% Syria |
RCT = 13/13 High |
|
Skarneh & Ghaith (2020) |
Jordan (UMIC) |
Quantitative: RCT | Syrian refugee women |
n = 30 Age: 18-50 years Gender: 100% females Religion: not specified Education: not specified Country of origin: 100% Syria |
RCT = 11/13 High |
| Slewa-Younan et al. (2020) |
Australia (HIC) |
Quantitative: Quasi-experimental (pre, post and follow-up using questionnaire) | Arabic-speaking women and men |
n = 33 Age: ≥18 years (M = 48, SD = 9) Gender: 58% females Religion: not specified Education: years of education (M = 8.8, SD = 3.7) Country of origin: Syria and Iraq |
Quasi-Experimental = 8/9 High |
| Spaaij et al. (2022) |
Jordan (UMIC) |
Mixed Methods: Quantitative (RCT) and Qualitative (semi-structured interviews) | Arabic-speaking Syrian refugees and asylum seekers |
Quantitative Intervention n = 31 Age: ≥18 years (M = 39.5, SD = 10.67) Gender: 45.2% females Religion: not specified Education: 80.6% basic & secondary, 19.4% university Country of origin: Syria Qualitative n = 18 Age: ≥18 years (M = 39.4, SD = 9.33) Gender: 50% females |
RCT = 10/13 Medium Qual = 9/10 High |
| Tashtoush & Khawaldeh (2020) |
Jordan (UMIC) |
Quantitative: RCT | Syrian refugee students |
n = 30 Age: 13-15 years (estimated) Gender: not specified Religion: not specified Education: school Country of origin: 100% Syria |
RCT = 9/13 Medium |
Participant characteristics
Observational studies
Of the observational studies (sample size from 3 to 6,375), sixteen focused solely on Arabic-speaking refugees [50, 51, 54, 55, 60–65, 67–70, 88, 89], two on refugees and the host community [53, 90], one on refugees and migrants [66], and one solely on migrants [48, 49]. Countries of origin were mainly Palestine, Syria and Iraq. The mostly female participants ranged in age from 14 to over 80 years, with most being youths and young adults. Nineteen studies reported on participants’ literacy or education; most were literate [48–51, 53–55, 60–70, 89, 90]. Thirteen studies reported participants’ religion; most were practicing Muslims [48–51, 55, 60, 62, 64–66, 68, 69, 89, 90].
Intervention studies
The sample size for the intervention studies ranged from 8 to 7,644. Twenty-six studies focused on refugees or those with a refugee-like background [57, 58, 71, 73–76, 78–86, 91–101], three on refugees and the host community [72, 77, 87], three on refugees and migrants [102–104], and five solely on migrants [105–109]. Lebanon, Syria, Jordan and Palestine were the main countries of origin. As in the observational studies, most participants were female. They ranged in age from 12 to 70 years, with most aged 12–18 years. Twenty-nine studies reported on participants’ education; most were university educated [57, 58, 72, 73, 75, 76, 78, 80–82, 84–87, 91, 92, 96–109]. Eight studies reported participants’ religion; most were Muslims [83, 84, 98, 99, 104, 107–109].
Mental health self-care strategies
After reviewing all included studies, we found mental health self-care activities fell into four broad groups—social strategies, psychological strategies, religious/spiritual strategies, and other strategies; findings were consistent with research on self-care and coping in other populations including African migrants and East African refugees [110–113]. Social strategies involved connecting with social networks. Psychological strategies were of two types—cognitive and behavioural. Cognitive strategies involved relying on inner resources to positively reframe negative situations. Behavioural strategies included taking action to address daily life stressors. Religious/spiritual strategies included relying on faith to find meaning in life and performing religious activities. The final group of strategies comprised various activities related to keeping oneself busy, including engaging in physical activity, pursuing hobbies or studying.
Table 2 summarises the broad self-care strategies reported in the included studies, and the study outcome measures where applicable. After this, we detail the different strategies included in each of the four groups, with the findings organised by study type.
Table 2.
Self-care strategies and study outcome measures by study type
| Author (Year) | Self-care strategy | Outcome measures | |||
|---|---|---|---|---|---|
| Social | Psychological | Religious/Spiritual | Other | ||
| Observational Studies (n = 20) | |||||
| Al-Ajarma (2010) | ✓ | ✓ | ✓ | ✓ | NA |
| Alhaddad et al. (2021) | ✓ | ✓ | ✓ | ✓ | NA |
| Boswall & Akash (2015) | ✓ | ✓ | ✓ | NA | |
| Chaaya et al. (2007) | ✓ | GDS-15 | |||
| Darychuk & Jackson (2015) | ✓ | ✓ | ✓ | NA | |
| Ferguson (2015) | ✓ | ✓ | ✓ | ✓ | NA |
| International Medical Corps (2017) | ✓ | ✓ | ✓ | ✓ | NA |
| International Medical Corps Lebanon (2011) | ✓ | ✓ | ✓ | ✓ | NA |
|
Irfaeya (2006) Irfaeya et al. (2008) |
✓ | ✓ | ✓ | ✓ | NA |
| Jamil (2020) | ✓ | ✓ | ✓ | ✓ | NA |
| Kadri (2009) | ✓ | ✓ | ✓ | NA | |
| Keshavarzi (2018) | ✓ | ✓ | ✓ | NA | |
| Makki Alamdari (2020) | ✓ | ✓ | ✓ | ✓ | NA |
| Nashwan et al. (2019) | ✓ | ✓ | ✓ | ✓ | NA |
| Qureshi (2016) | ✓ | ✓ | ✓ | ✓ | NA |
| Rayes et al. (2021) | ✓ | ✓ | NA | ||
| Renner et al. (2020) | ✓ | ✓ | ✓ | ✓ | NA |
| Sim et al. (2023) | ✓ | ✓ | ✓ | ✓ | NA |
| Tauson (2017) | ✓ | ✓ | ✓ | ✓ | NA |
| Zbidat et al. (2020) | ✓ | ✓ | ✓ | ✓ | NA |
| Intervention Studies (n = 37) | |||||
| Acarturk et al. (2022) | ✓ | ✓ | MINI, GHQ-12, PCL-5, PHQ-9, PSYCHLOPS, WHO- DAS 2.0, WHO-5, EQ-5D-3 L | ||
| Ahmad et al. (2020) | ✓ | ✓ | ✓ | ✓ | PCL-5 |
| Aladdin & Hawamdeh (2021) | ✓ | ✓ | SDQ | ||
| Al-Dmour & Al-Safasfeh (2020) * | ✓ |
PTSD scale Satisfaction with Life scale |
|||
| Al-Refai et al. (2022) * | ✓ | ✓ | Psychological Empowerment Scale | ||
| Al-Shahadat (2021) * | ✓ |
Psychological stress scale Self-esteem scale |
|||
| Alsheikh Ali (2020) | ✓ | PCL, PWB | |||
| Blignault et al. (2019) | ✓ | ✓ | K-10+, DASS-21 | ||
| Blignault et al. (2021a) | ✓ | ✓ | ✓ | DASS-21 | |
| Blignault et al. (2021b) | ✓ | ✓ | ✓ | K-10+, DASS-21 | |
| Blignault et al. (2022) | ✓ | ✓ | ✓ | K-10+ | |
|
Bryant et al. (2022a) Bryant et al. (2022b) |
✓ | HSCL-25, PCL-5 | |||
| Cuijpers et al. (2022) | ✓ | PHQ-9, WHODAS-12 2.0, WHO5WBI, GAD-7, PCL-5, PSYCHLOPS | |||
| de Graaff et al. (2020) | ✓ | ✓ | HSCL-25, WHODAS 2.0, PCL-5, PSYCHLOPS | ||
| de Graaff et al. (2023) | ✓ | HSCL-25, WHODAS 2.0, PCL-5, PSYCHLOPS | |||
| DePierro (2020) | ✓ | ✓ | ✓ | ITQ, K-10 | |
| Doumit et al. (2020) | ✓ | ✓ | PHQ-9, GAD-7, PedsQL | ||
| Feen-Calligan et al. (2023) | ✓ | ✓ | ✓ | ✓ | Self-report from selected participants |
| Gordon et al. (2016) | ✓ | ✓ | ✓ | HTQ, HSCL-25, WHOQOL-BREF | |
| Hasha et al. (2022) | ✓ | IES-R, GHQ-12 | |||
| Husby et al. (2020) | ✓ | ✓ | WHO-5 | ||
| Ibrahim (2017) | ✓ | ✓ | DTS | ||
| Kayrouz et al. (2015) | ✓ | PHQ-9, GAD-7, K-10 | |||
| Kayrouz et al. (2016) | ✓ | ✓ | PHQ-9, GAD-7, K-10 | ||
| Lindegaard et al. (2020) | ✓ | PHQ-9, IES-R, GAD-7 | |||
| Lindegaard et al. (2021) | ✓ | Self-report from selected participants | |||
| Mercy Corps (2020) * | ✓ | ✓ | ✓ | AYMH | |
| Nilsson et al. (2019) | ✓ | ✓ | ✓ | Self-report from selected participants | |
| Panter-Brick et al. (2018) * | ✓ | ✓ | ✓ | AYMH, CRIES-8 | |
| Powell et al. (2023) | ✓ | ✓ | ✓ | ✓ | NA |
| Raknes (2020) * | ✓ | WHO5WBI | |||
| Rayes (2017) * | ✓ | ✓ | YEP index | ||
| Röhr et al. (2021) | ✓ | PDS-5, PHQ-9, GAD-7 | |||
| Skarneh & Ghaith (2020) | ✓ | ✓ | ✓ | HTQ | |
| Slewa-Younan et al. (2020) | ✓ | ✓ | K-10 | ||
| Spaaij et al. (2022) | ✓ | HSCL-25, PCL-5 | |||
| Tashtoush & Khawaldeh (2020) * | ✓ | ✓ | Psychological and social adjustment scale | ||
Translated Arabic versions of the psychometric scales were used
*These scales were developed in Arabic
AYMH, Arab Youth Mental Health; CRIES-8, Child Revised Impact of Events Scale; DASS-21, Depression Anxiety and Stress Scale; DTS, Davidson Trauma Scale; EQ-5D-3 L, European Quality of Life 5-Dimensions 3-Level; GAD-7, Generalized Anxiety Disorder; GHQ-12, General Health Questionnaire; GDS, Geriatric Depression Scale; HSCL-25, Hopkins Symptom Checklist-25; HTQ, Harvard Trauma Questionnaire; IES-R, Impact of Event Scale-Revised; ITQ, International Trauma Questionnaire; K-10, Kessler Psychological Distress Scale; MINI, Mini International Neuropsychiatric Interview; PCL-5, PTSD Checklist; PDS-5, Posttraumatic Diagnostic Scale; PedsQL, Paediatric Quality of Life Inventory; PHQ-9, Patient Health Questionnaire; PSYCHLOPS, Psychological Outcome Profiles; PWB, Ryff’s Psychological Well-Being; SDQ, Strengths and Difficulties Questionnaire; WHO-DAS 2.0, WHO Disability Assessment Schedule 2.0; WHO-5/WHO5WBI, World Health Organization-Five Well-Being Index; WHOQOL-BREF, World Health Organization Quality of Life Instrument; YEP, Youth Empowerment Program Index
Observational studies
Social strategies
Nineteen observational studies reported the use of social strategies. This involved having a network of immediate and extended family, friends, and neighbours and connecting with them in person and via phone or social media [48–50, 55, 60, 62, 64, 65, 67, 88]. Talking with family, community members, authority figures, social service providers, and those with similar experiences for emotional support, advice, assistance and resources was common [53, 61, 63, 65, 66, 68, 70]. Raising children together, as a community with traditional values; participating in informal women’s groups where they could bring their children and discuss problems; and organising or attending cultural events to connect with new people of the same culture, faith or ethnicity were also reported [51, 53–55, 69, 88, 89].
Psychological strategies
Fifteen studies reported psychological strategies. Cognitive strategies involved positive thinking and positive self-talk, thinking deeply, changing mindset, realism, goal-setting, and being future-focused [48, 49, 54, 55, 60, 62, 63, 66–68, 70, 89]. Behavioural strategies involved active problem-focused strategies such as talking about problems and taking steps to improve situations, writing about stressors, and distraction with other activities [48, 49, 53, 54, 62, 66, 68, 70, 89]. Mind-body techniques such as slow breathing and meditation were noted [50, 61, 68]. Studies in high-income resettlement countries (Germany, New Zealand, United States and United Kingdom) and transit (Thailand) countries highlighted building self-determination, self-motivation, self-efficacy, self-control, perseverance, persistence and willpower to overcome obstacles [55, 60, 62–65, 68, 89].
Religious/spiritual strategies
All twenty studies reported strategies related to spirituality or religion (Islam and Christianity). These included praying and offering supplications, fasting, attending religious talks and services at churches or mosques (Friday prayers), meeting with others of the same faith, seeking help from local religious leaders, reading and listening to religious scriptures, and using Arabic expressions such as ‘Thank God’ and ‘God willing’ to convey hope for a better future [48–51, 55, 60, 61, 63, 64, 68, 69, 88–90]. Spirituality, having faith in a higher power, accepting and surrendering to God’s will, believing in divine judgement based on the consequences of one’s actions, and expressing gratitude to God were also mentioned [50, 51, 53–55, 61–67, 70, 88, 89].
Other strategies
Seventeen studies identified other strategies—leisure activities, daily life activities, expressive arts, physical activity and self-development. Leisure activities included watching television and comedy programs, going to the cinema, watching humorous videos and playing games on mobile phones, vacations, and reading [48–51, 54, 55, 61–64]. Seeking pleasure from daily life involved partaking of sustenance (food and sleep), doing housework, gardening, and spending time with children [48–50, 54, 55, 62, 64, 68]. Expressive arts practice included poetry, music, dance, singing, drawing, journaling, acting, filmmaking and photography [48–50, 55, 61–63, 67, 68]. Physical activities included sports, exercise walks, and going to the gym [48–50, 55, 62, 63, 66–68]. Studies, particularly in resettlement countries, reported self-development through learning the host country language, education, employment, and volunteering [48, 49, 51, 53, 55, 61–65, 67, 70, 88, 89].
Intervention studies
As detailed in Table 3, 25 of the 37 interventions were delivered in groups [57, 58, 71–74, 76–84, 87, 91, 93–96, 98, 100, 104, 108, 109], 11 were delivered individually [85, 86, 92, 97, 99, 101–103, 105–107], and one was delivered in both formats [75]. Most interventions were delivered in person [57, 58, 71–74, 76, 77, 79–84, 86, 87, 91–98, 100, 108], with four also having a digital component [75, 78, 101, 104]. Seven interventions were delivered online [85, 99, 102, 103, 105, 106, 109] and one via compact disc [107]. Interventions were predominantly delivered in community settings [57, 58, 71–78, 80–85, 93–99, 101–109]. Twenty-two of the interventions were delivered by mental health professionals [71, 73, 74, 76, 78–82, 84, 91, 92, 94, 96, 98, 100, 102, 103, 105, 107–109], while ten were delivered by trained peer volunteers [57, 58, 72, 75, 77, 83, 85, 86, 95, 97, 101].
Table 3.
Intervention details
| Author (Year) | Intervention | Setting | Provider training/skill | ||
|---|---|---|---|---|---|
| Duration | Format | Delivery | |||
| Acarturk et al. (2022) | 5 weeks; 5 sessions each 2 h | Group | In-person | Refugee camps/city settlements | Trained peer non-specialist facilitators |
| Ahmad et al. (2020) | 4 weeks; 15 sessions each 1.5 h | Group | In-person | City settlement | Mental health and education researchers |
| Aladdin & Hawamdeh (2021) | 14 weeks; 14 sessions each 45–50 min | Group | In-person | Elementary school hall | Skilled in CBT counselling |
| Al-Dmour & Al-Safasfeh (2020) | 7 weeks; 14 sessions, twice/week and each for 60 min | Group | In-person | School | Educational psychologist, special education researchers, counsellors |
| Al-Refai et al. (2022) | 12 weeks; 12 sessions, over 3 months, with one session a week, each for 60 min | Group | In-person | City settlement | Researchers with Islamic studies, Psychology and ICT background |
| Al-Shahadat (2021) | 7 weeks; 14 sessions; two sessions/week, each 45–60 min | Group | In-person | School theatre hall | Family counselling skills |
| Alsheikh Ali (2020) | 7 weeks; 2 sessions/week over 1.5 months | Group | In-person | City settlement | Licensed psychotherapist/clinical psychologist |
| Blignault et al. (2019) | 5 weeks; Instructions to listen to 2–3 tracks at least 3 times a week over 4 weeks, and one track 3 times a week in the 5th week. 60 min/week | Individual | Compact disc | Home | Psychologist |
| Blignault et al. (2021a) | 5 weeks; one session per week over five weeks | Group | In-person | NGO; Home | Psychologist supported by a bilingual multicultural health worker |
| Blignault et al. (2021b) | 5 weeks; once a week over 5 weeks, most groups held in the morning and a couple in the evening | Group | In-person | Migrant resource centres and community facilities attached to mosques and churches; Home. | Psychologists and trained community workers |
| Blignault et al. (2022) | 4 weeks; session once a week for four weeks | Group | Online | Home | Bilingual (Arabic/English) mental health clinician (psychologist) and bilingual community worker |
|
Bryant et al. (2022a) Bryant et al. (2022b) |
5 weeks; 5 sessions, 2 h | Group separated by gender | In-person | Refugee camp | Trained facilitators, proficient in Arabic |
| Cuijpers et al. (2022) | 5–8 weeks; 5 sessions, 20 min (average) | Individual | Online | Home | Trained non-specialists (e-helpers) with psychology or health background. User contact via phone or message |
| de Graaff et al. (2020) | 5weeks; 5 weekly sessions, each 90 min | Individual | In-person | Local NGO | Trained Arabic-speaking Syrian non-specialist peer-refugee helpers |
| de Graaff et al. (2023) | 5 weeks; 5 sessions, 90 min | Individual | In-person and online | University or home | Trained Arabic-speaking Syrian non-specialist peer-refugee helpers |
| DePierro (2020) |
Workshop condition: 8 weeks; 16 sessions 120 min twice weekly Reading at Home condition: weekly program content review, twice weekly SMS text reminders |
Workshop condition: Group Reading at Home condition: Individual |
In-person and SMS | Refugee camp | Trained community facilitators, with personal experiences as refugees and life in refugee camps |
| Doumit et al. (2020) | 7 weeks; one weekly session each 60 min | Group | In-person | Community centre | Licensed instructor and therapist |
| Feen-Calligan et al. (2023) | 10 weeks; 10 sessions for 5 months | Group | In-person and online | Museum; Home | Photography instructor, art therapy student interns, and their faculty supervisor, with support from the museum staff. Artistic and technical guidance via WhatsApp or Zoom |
| Gordon et al. (2016) | 10 weeks; 10 sessions/week of 2 h | Group | In-person | Health clinic | Mental health professionals and educators supervised by Centre for Mind-Body Medicine (CMBM) faculty |
| Hasha et al. (2022) | 6 weeks; 2.5 h weekly group sessions | Group separated by gender | In-person | The Centre for Crisis Psychology, University of Bergen | Research team members with prior experience working with refugees |
| Husby et al. (2020) | [Weeks undetermined]; 9 sessions of 2 h each | Group | In-person | Local (Danish) municipalities | Trainer of refugee background, social worker as co-trainer and an interpreter |
| Ibrahim (2017) | 3 weeks; 6 sessions (2 sessions/week), each 45–60 min over 2 months | Individual | In-person | Not specified | Psychologist |
| Kayrouz et al. (2015) | 8 weeks; 5 sessions | Individual | Online | Home |
Bilingual counsellor and therapist Clinical support via email and phone |
| Kayrouz et al. (2016) | 8 weeks; 5 sessions | Individual | Online | Home | Automated weekly emails. No direct contact or clinical support |
| Lindegaard et al. (2020) | 8 weeks | Individual | Online | Home | Therapist support via email |
| Lindegaard et al. (2021) | 8 weeks | Individual | Online | Home | Therapist support via email |
| Mercy Corps (2020) | 13 weeks (approx.) for 3 months | Groups separated by gender | In-person | Community centres | Local volunteers, coaches and life-skill trainers with refugee background |
| Nilsson et al. (2019) | [Weeks undetermined]; 1–2 h sessions | Groups separated by gender | In-person | NGO | Physiotherapists |
| Panter-Brick et al. (2018) | 8 weeks; 16 sessions usually 2 sessions/week | Groups separated by gender and age | In-person | Youth centres | Lay volunteers/trained local coaches |
| Powell et al. (2023) | [Weeks undetermined]; 4 sessions over a year, each 45 min (approx.) | Group | In-person | Primary care clinic | Health educators and nurses from local health clinics |
| Raknes (2020) | 10 weeks; 10 sessions weekly | Group | In-person (smartphone/tablet-based game app) | Refugee camp tents | Psychologist (displaced Syrian background) |
| Rayes (2017) | 10 weeks | Group | In-person | Urban refugee camps | Mental Health and Psychosocial Support (MHPSS) team |
| Röhr et al. (2021) | 4 weeks | Individual | Online (smartphone-based app) | Home | NA |
| Skarneh & Ghaith (2020) | 8 weeks; 15 sessions over 2 months, each 90–120 min, twice per week | Group | In-person | Healthcare institute | Counsellors from the local community |
| Slewa-Younan et al. (2020) | 4 weeks; 3 h sessions weekly | Group | In-person | TAFE College, Adult Migrant English Program | Mental health clinicians and/or bilingual health educators |
| Spaaij et al. (2022) | 5 weeks; Five 90-minute sessions once a week | Individual | In-person | Outpatient clinic | Trained Syrian non-specialist ‘helpers’ fluent in Arabic and German or English. |
| Tashtoush and Khawaldeh (2020) | 7 weeks; 14 sessions, twice per week for 90 min each | Group | In-person | School | Counsellor or educational psychologist familiar with the local community and culture |
Intervention studies
Social strategies
Eighteen of the 25 group interventions clearly promoted social strategies—engaging with peers having similar problems, empathising with others and motivating them, providing a safe space for dialogue and opportunities to build connections, and continuing to meet for support post-intervention [72, 75–77, 79, 80, 83, 84, 87, 91, 93–95, 97, 98, 104, 108, 109]. Trained facilitators played key roles in building social cohesion, rapport and trust, leading to participants openly disclosing their problems in both group and individual formats [72, 77, 83, 93, 97, 98, 104].
Psychological strategies
All 37 interventions incorporated psychological strategies. In the 25 group interventions, these were typically based on cognitive behavioural therapy (CBT), cognitive behavioural play therapy (CBPT), narrative therapy, teaching recovery techniques (TRT), and emotional or behavioural self-regulation [71–74, 76–78, 80–83, 93–95, 100]. Cognitive restructuring and problem-solving techniques were often reported [57, 58, 71, 73, 74, 76, 78, 80–82, 84, 87, 93–95, 104]. Mind-body techniques included deep-breathing, yoga, mindfulness and meditation [73, 76, 79, 86, 87, 91, 93, 95–98, 101, 108, 109]. The 11 individual interventions included in-person, online and smartphone app-based CBT-informed techniques [85, 86, 92, 97, 99, 101–103, 105–107]. One hybrid intervention included psychoeducation, mindfulness, and self-care exercises delivered in groups and individually [75].
Religious/spiritual strategies
Six group interventions incorporated a religious or spiritual component, namely, designing CBT and mindfulness program content according to participants’ spiritual and religious beliefs, writing positive religious statements as daily practice, or praying [87, 94, 98, 104, 108, 109]. Three individual interventions, involving in-person and online CBT and compact disc-based mindfulness therapy respectively, were similarly tailored to participants’ faith and culture [92, 106, 107].
Other strategies
Twelve interventions incorporated other strategies, with four involving physical activity—exercise, nature walks, football, and a physiotherapeutic intervention (tension and trauma releasing exercises and aerobics) [72, 77, 87, 93]. Eight interventions involved expressive arts—drawing, craftwork, graphic design, photography, music, storytelling, theatre and drama [72, 75, 77, 79, 82, 91, 94, 104]. Skill-based psychosocial programs focused on vocational skills and mental health promotion and literacy [71, 72, 77, 91, 96].
Effectiveness
Thirty intervention studies incorporating CBT, mind-body techniques or psychosocial programs showed statistically significant improvements in psychological wellbeing, quality of life, life satisfaction, and social cohesion, with a reduction in symptoms of psychological distress, depression, generalised anxiety and PTSD on a range of psychometric scales as listed in Table 2 [57, 58, 71–86, 91, 92, 94–98, 101, 105–109]. Fourteen studies reported improved outcomes maintained at follow-up [57, 58, 79, 81–83, 85, 86, 91, 94, 96, 97, 101, 105, 107]. Four studies reported a reduction in depression symptoms but not for anxiety or PTSD [90, 100, 102, 103]. Two studies noted self-reported reductions in somatic symptoms of depression, anxiety and PTSD [93, 104]. Only one intervention, the smartphone based Sanadak app, reported no statistically or clinically significant outcomes for refugees as compared to the control group. The authors suggest that the app may be more effective with support from trained facilitators [99].
Cultural appropriateness
Twenty-seven intervention studies provided information relating to cultural appropriateness. Interventions were delivered in Arabic, with culturally and linguistically appropriate program content, led by non-specialist instructors with similar culture or refugee background, same language, and gender as the participants, in safe gender-segregated groups [57, 58, 72, 75–78, 82, 83, 85–87, 93, 95, 97–101, 103, 104, 107, 108]. The self-care components were grounded in participants’ sociocultural and religious practices and were beneficial and easy-to-use independently. Provision of refreshments during group interventions and eating together reflected cultural norms [76, 108]. Eight studies reported high program attendance and compliance and completion rates [75, 76, 98, 104, 106–109], which may be taken as an indication of broad cultural acceptability. Popularity of the strategies spread by word-of-mouth to family nearby and overseas, friends, and community members including those with mental disorders [75, 78, 87, 91, 98, 105, 106, 108, 109].
Participant experiences
Social strategies
Twelve observational studies reported that activities involving family and friends were the most common source of emotional and practical support among Arabic-speaking refugees and migrants, with participants feeling safe, resilient, motivated, happy, and experiencing a sense of community, ease and belonging [48, 49, 53–55, 60–64, 66, 67, 70]. The following quotes are illustrative.
… We talk about our kids and we cook. We share all the food we make together throughout the community. We most often talk about life in general. Like the things that stress us. We talk about how we want to make ourselves happy. We talk also about depression and mental health.
Palestinian female refugee (age unspecified), West Bank, Palestine [88, p.452].
The only feeling of safety I felt was when I was with my family.
28-year-old Palestinian female refugee, United States [61, p.88].
Participants in thirteen intervention studies reported becoming more communicative and expressive about their feelings, which improved their relationships with family and friends [72, 75–77, 79, 80, 87, 93, 95, 97, 98, 104, 108].
[Hearing] the calamity of others makes your calamity easier for you.
Syrian female refugee (age unspecified), Jordan [79, p.288].
I considered her [peer facilitator] a friend. Not a durable friendship but friendship in the session’s time. I was feeling comfortable talking to her.
Syrian refugee (age and gender unspecified), Netherlands [97, p.19].
Key challenges included feelings of isolation and distress due to inadequate emotional and practical support from settlement workers, triggering of past trauma by peers, and limited opportunities for outdoor socialisation, particularly for female migrants and refugees [48, 49, 70, 88, 95].
Psychological strategies
Nine observational studies reported participants becoming more ambitious, determined, adaptable, resourceful and self-reliant [55, 60, 62, 63, 65, 66, 68, 70, 89].
I always try to convince myself that I am stronger than the situation and can survive it.
Syrian refugee (age and gender unspecified), Germany [55, p.9].
It [hard times before coming to Thailand] is behind us; why do I want to think about these things? Sure I was scared, but now I am not, what is the point?
Palestinian-Syrian female refugee in her 40s, Thailand [89, p.183].
Eleven of the intervention studies noted that participants practicing mind-body techniques and relaxation exercises reported feeling calmer, energised and mindful [75, 76, 79, 86, 87, 93, 95, 97, 98, 103, 107, 108]. They reported functioning better at school and work, and within the family [76, 86, 93]. Through learning about mental health awareness and ways to cope with psychological distress, participants became more compassionate, confident and empowered [72, 76–78, 80, 93–95, 98, 103, 108]. Six studies reported improved sleep; reduced feelings of anxiety and depression; lower intake of medications; higher referrals to psychologists and overall improved quality of life and wellbeing [77, 93, 98, 103, 108, 109].
Sometimes I remembered my children they are away…so I breath in and out and feel relaxed.
Syrian male refugee (age unspecified), Jordan [87, p.167].
The way I integrate myself is for an example by active listening, which we have discussed. It is to listen to your children. […] Things like this make me better mentally and psychically. This makes me able to take time to be a part of society.
Female refugee (age unspecified), Denmark [95, p.1035].
Ten studies reported psychological interventions (group or individual) with a digital component [78, 85, 99, 101–106, 109]. Using psychological self-care strategies via internet and smartphone apps, participants felt supported by facilitators and found them convenient due to privacy and time and cost efficiency [78, 85, 99, 103, 105, 109]. However, participants also faced some challenges while practicing self-care strategies adopted from the interventions due to stigma against mental illness, work commitments; technological problems (e.g., lack of electronic devices, online platform access, internet and electricity); low literacy; difficulty understanding, retaining and applying the program concepts; dissatisfaction with program content and short duration; inability to practice self-care exercises due to insufficient focus or physical pain and emotional distress; trauma triggers; distractions at home; and negative interaction with facilitators [78, 86, 95, 97, 98, 103, 108].
Religious/spiritual strategies
Eighteen of the observational studies stated that practicing religious and spiritual strategies during flight and afterwards served as sources of comfort, security, hope, and peace [48, 49, 51, 53–55, 60, 62–66, 68–70, 88–90].
It [praying or listening to Quran recitations] makes you feel better and comforts all your pains.
Syrian female refugee (age unspecified), Jordan [51, p.211].
Five of the intervention studies highlighted the benefits of daily prayers and religious practices [87, 98, 104, 107, 108].
Most important point for me is that mindfulness relates to my religion. For example, prayers require the person to be mindful. My mind used to wander during prayers. Mindfulness has strengthened my faith and reduced stress.
Muslim female refugee (age unspecified), Australia [98, p.9].
Male refugees in Germany expressed concerns about the lack of nearby mosques, especially those of the same Islamic sect and language, praying less frequently than in their country of origin, missing Friday prayers due to work, and distrust of and lack of engagement with imams (religious clerics) [69].
I am finding some difficulties in maintaining prayer here. In Syria, I used to never miss a prayer, but not because I am less convinced [by my faith]. It is a shortage on my end. Near my house, there is no mosque near my house. The closest one is an hour away. My faith practice is inside my house, mainly.
Syrian Muslim male refugee (age unspecified), Germany [69, p.6].
Other strategies
Participants in sixteen observational studies reported feeling inspired and confident by keeping busy with various self-development activities and hobbies without facing any overt challenges [48–51, 54, 55, 61–68, 70, 88, 89].
For me, music was a relief. I would feel relaxed even when I blew into the flute without actually playing it or when holding the flute in my hand. It had become an inseparable companion.
35-year-old female with refugee background, United States [61, p.109].
Eight interventions incorporating other self-care strategies, particularly expressive arts and physical activity, reported participants feeling relaxed and forgetting previous trauma and daily stressors [72, 75, 77, 79, 87, 93, 96, 104]. For example,
The sports make us forget. I think about winning, and I laugh with my friends. … There is nothing that can make us forget what has happened to us, or make our problems go away, but at least we have this.
37-year-old male refugee, Sweden [93, p.7].
… I use photography as a way of relaxation at stressful times.
Adolescent female with immigrant-refugee background, United States [104, p.8].
Discussion
This systematic review sought to identify and examine the global evidence on mental health self-care strategies for Arabic-speaking refugees and migrants, addressing depression, anxiety and PTSD, which are prevalent among these populations [6–10, 114, 115]. Over the past decade, this area has attracted increased attention from researchers prompted by political unrest and violent conflict in the Middle East and the resultant rise in Arabic-speaking refugees and asylum seekers. Since 2014, Syria has been a major source country for refugees, with approximately 13.5 million forcibly displaced people worldwide [116]. A comprehensive search of the published and grey literature in English and Arabic since 2000, identified 37 interventions and 20 observational studies that met the inclusion criteria. The majority of studies were dated from 2020 onwards, conducted in upper-middle and high-income countries, and focused on refugees. Across both study types, four broad groups of mental health self-care strategies were identified: social, psychological, religious/spiritual and other (including expressive arts and physical activity). Psychological strategies featured in all the interventions. Social and religious/spiritual strategies were more commonly reported in observational studies, although psychological strategies were also utilised. Interventions that integrated self-care components based on cultural and religious practices of the target community resulted in positive user experiences and improved mental health and wellbeing.
Contextual factors are critical in designing and implementing local solutions for global health concerns, such as mental health interventions for refugees and asylum seekers [117]. This review suggests that there are many similarities in self-care strategies used by Arabic-speaking refugees in transit and resettlement countries, including finding comfort in religious and spiritual beliefs, seeking support from social connections, and engaging in relief-providing activities. An Australian qualitative study with 23 Sudanese refugees (mostly Christians with 10 Arabic speakers) found that while they experienced various difficulties across pre-migration, transit and post-migration phases, the self-care strategies they employed were similar; relying mainly on religion, social networks and cognitive approaches [110].
Social strategies
Social strategies identified in this review, such as maintaining a strong network of family, friends and community, elicited feelings of safety, belonging and resilience. Research highlights the mental health benefits of social connections and receiving emotional or practical support from them, with limited peer connections linked to overall poor mental health and increased depression symptoms [118–121]. Digital technology was commonly reported in both observational and intervention studies. Four studies in our review [50, 51, 65, 66] noted that refugees and migrants used social media and phone calls to family and friends in the home country, supporting the role of technology for social connection [122]. Group interventions with self-care components, facilitated by trained peers, often involved social support. This aligns with a recent systematic review on mental health intervention delivery amongst refugees and asylum seekers in low-and middle-income countries (LMICs), highlighting the role of trained facilitators, usually well-respected community members, in guiding participants and fostering strong relationships to improve program feasibility [117].
Within Middle Eastern Arab cultures, Muslims and Christians pursue happiness and satisfaction through mutual assistance and fulfilment of social duties [123–127]. Seeking support from family, friends and community is deeply rooted in the collectivist culture and identity [33, 128–130]. Following traditional customs and bonding over meals shared with family and community help in building trust, agency and resilience among Arabic-speaking refugees [130–132]. We identified one study of Palestinian women in West Bank refugee camps where raising children within the community and upholding traditional values contributed to enhanced resilience and mental wellbeing [88]. The cultural significance of sharing food and communal eating was noted in two studies [76, 108].
Two studies reported significant challenges related to gender, such as inadequate female-friendly recreation facilities and unsafe meeting spaces, particularly, but not only, in refugee camps [48, 49, 88]. Unsafe living conditions were associated with depression and PTSD symptoms, especially among women [133–136]. Generally, women experience higher rates of mental disorders than men [137, 138]. Arabic-speaking women often face limitations on public interactions and need to be accompanied by a male family member when outside [139–141]. Traditional beliefs also restrict women’s participation in physical recreation [142, 143].
Psychological strategies
Cognitive self-care generally involved utilising internal resources such as inner strength, positive self-talk and optimism. Interventions with self-care components often introduced CBT skills such as problem-solving, cognitive restructuring and mind-body techniques. Participants who practiced these psychological strategies reported an improved quality of life and mental wellbeing. Mind-body techniques are popular, easy-to-use, affordable and clinically effective in reducing anxiety, depression, and PTSD symptoms, and can be considered in psychological interventions for migrants, refugees and asylum seekers [144–146].
Challenges in practicing psychological strategies, including limited device access and low literacy levels were identified in seven studies. While these challenges are common among migrants and refugees [147–149], culturally tailored technology-mediated platforms, including self-care apps, show promise in transit settings (UMICs and LMICs) with limited mental health services [150, 151]. However, it is recommended to supplement app-based platforms with on-demand guidance from health professionals sharing the same race, gender, religion or language as the Arabic-speaking migrants and refugees [149, 152–155].
Group interventions incorporating self-care and peer support can empower clients and positively impact their relationships and quality of life [120, 156]. Most interventions in this review, in both transit and resettlement countries, were delivered in a group setting that offered peer support and general psychoeducation. A qualitative study involving 30 refugees from Burundi, Burma, Congo, Rwanda and Bhutan, resettled in the United States and receiving treatment for symptoms of depression, PTSD or anxiety highlighted the importance of culturally competent peer-centred programs. The authors recommended intervention programs providing group-based social support and addressing practical needs such as employment, language and literacy training and healthcare access [157].
Religious/spiritual strategies
Religious and spiritual strategies included praying, fasting, reading religious texts, and attending religious gatherings. Whether self-generated or delivered through intervention, these practices instilled a sense of peace, relief, endurance and perseverance. These findings align with other research illustrating the benefits of culturally tailored psycho-spiritual interventions and religious practices for the mental health and wellbeing of refugees and migrants [158–163].
The Arab culture emphasises religious and spiritual traditions [130, 164]. Studies in the United States and elsewhere indicate that Christians who attend church services experience great support from fellow churchgoers and a sense of comfort from prayers [124, 165]. Similarly, within the Islamic faith, absolute submission to God’s will, regular prayer, observing Ramadan, Quran reading and expressing gratitude to Allah significantly increase happiness and inner peace [123, 125, 166, 167]. The daily prayers promote relaxation and alleviate symptoms of anxiety and stress [123, 168, 169].
A German study identified numerous challenges to practicing religious self-care [69]. Worshippers generally prefer attending mosques that cater to their specific Islamic sect [170, 171]. Muslim males are encouraged to perform the five obligatory prayers at the mosque, particularly, the Friday noon prayer [172]. Religious clerics have significant social standing within the Arab-Muslim community and may offer counselling to those dealing with mental disorders [152, 173]. However, clerics often lack formal training in counselling and may stigmatise mental disorders, viewing them as God’s punishment [173–175].
Other strategies
Although psychological, social and religious/spiritual strategies were dominant in this review, a range of other self-care strategies were also identified. Participants practicing physical activity and exercise, expressive arts, and self-development activities reported increased confidence and motivation. Growing research demonstrates the physiological and psychological benefits of physical activity among refugees and migrants in diverse settings [176–178]. Arts-based interventions have effectively reduced symptoms of anxiety, stress and depression [179]. Alongside talk therapies, evidence-based psychological interventions incorporating arts-based cultural activities could be suitable for individuals seeking mental health support in the Arab culture, where stigma around mental illness is prevalent [141, 152]. Further research is needed on incorporating Islamic art and culture into mental health interventions [180].
Unstable economic circumstances increase the risk of PTSD and depression among refugees and migrants [23]. Interventions combining social and economic skill-building with mental health support are considered an emerging practice to enhance economic empowerment and mental wellbeing for refugee and migrant youth [117, 181]. Addressing structural barriers to social and economic participation as well as social determinants of health will benefit new arrivals of all age groups [182]. Besides culturally and linguistically appropriate mental health interventions, addressing uncertain visa status, racism and discrimination, financial difficulties and lack of resources is essential [183, 184]. Implementing visa reforms, enforcing fair migration and workplace laws, and adopting anti-discriminatory policies can enhance the overall wellbeing of refugees and migrants [17, 185].
Implications for practice and service delivery
Specialist mental health services, which typically focus on treating individual patients, should consider group interventions incorporating self-care and peer support. For Arabic-speaking refugees and migrants, delivering these interventions in gender-specific groups that align with sociocultural norms can be beneficial for program engagement and outcomes. Supplementing standard psychological interventions with culturally relevant religious/spiritual strategies, social self-care and expressive arts-based strategies, as identified in this review, is also likely to be helpful.
Within the primary and community health context, collaborating with and training of religious leaders and community health workers on culturally and linguistically adapted mental health self-care strategies is beneficial for Arabic-speaking refugees and migrants. Investment in facilities to engage in religious practices, recreational activities, and female-friendly meeting spaces in refugee camps and resettlement countries is crucial. Integrating digital technology-mediated mental health self-care into primary healthcare services can potentially minimise psychiatric outpatient care, particularly in UMICs and LMICs [39, 149, 186]. Improving internet access, offering affordable mobile data packages, providing digital health literacy training, and incorporating clear instructions in local Arabic dialects for refugees and migrants with low education levels would enhance user experiences and the adoption of digital self-care strategies [149].
Recommendations for research
Additional research is needed to explore mental health self-care strategies among Arabic-speaking migrants and refugees in Western resettlement countries, focusing on at-risk groups such as unaccompanied refugee minors, females, and older adults. Examining mental health self-care strategies among Arabic-speaking refugees and asylum seekers in low-income transit countries is also recommended. Studies in this review focused on Arabic-speaking migrants, refugees and asylum seekers aged 12 years and older. Given the significance of developmental factors in coping with stress [187], future reviews should consider adolescents and children separately from adults. Including a qualitative component in intervention studies would provide valuable insights into participant experiences and community perspectives. Promising areas for future research include the development of group interventions to facilitate social networks and the design, delivery, and further evaluation of guided psychological self-care apps. Further examination of the effectiveness, cultural appropriateness, and user experiences associated with physical activity, arts-based activities, and religious/spiritual practices as mental health self-care strategies is also warranted. Finally, further research is needed to better understand the relationship between various self-care strategies and measures of mental health and wellbeing, their effectiveness in alleviating symptoms of common mental disorders, and their impact on daily functioning within the target population in different contexts.
Strengths and limitations
This review employed a rigorous systematic methodology and a comprehensive search strategy to examine the published and grey literature on mental health self-care strategies for Arabic-speaking refugees and migrants, including intervention and observational studies in English and Arabic. We adopted a broad definition of self-care, with implications for both public health and clinical practice [38]. The inclusion of observational studies provided a better understanding of self-generated strategies. All included intervention and observational studies were appraised as high or medium quality. Multiple reviewers independently screened and assessed the studies, including the five records authored by members of the research team, to remove selection bias. The inclusion of grey literature helped mitigate publication bias effects. Findings were reported according to the PRISMA guidelines [44, 56]. There are several limitations to note. Firstly, despite a comprehensive search strategy, it is possible that some potentially eligible studies may have been overlooked due to the vast scope of the concept definitions. Furthermore, papers published in languages other than English or Arabic may have yielded additional results. Moreover, in this review the target population was treated as a homogenous group, however cultural, religious and ethnic diversities within Arabic-speaking countries, along with differences in healthcare infrastructure across their countries of origin, may impact the generalisability of our findings to all Arabic-speaking individuals. The diversity of intervention studies, including variation in design, samples, intervention components, and outcome measures, made it challenging to determine the most effective and culturally appropriate self-care strategies. Despite the absence of diagnostic labels for participants, observational studies substantially add to the evidence of self-generated self-care practices. Given the known high prevalence of depression, anxiety and PTSD among Arabic-speaking refugees and migrants, these disorders are likely to be common in the study samples. Finally, most studies described multiple self-care strategies, making it difficult to reach definitive conclusions about the effectiveness of specific or groups of self-care practices.
Conclusions
Refugees and migrants are more vulnerable to mental disorders than the general population yet are less likely to seek professional help or utilise mental health services. This review contributes to the expanding knowledge on mental health self-care for Arabic-speaking refugees and migrants. It describes how social, religious/spiritual, psychological and other self-care strategies provide meaningful and positive experiences for these populations and reinforces the effectiveness of culturally appropriate interventions in reducing symptoms. Insights from this review can be used to inform mental health interventions in diverse settings among this vulnerable population, adhering to the WHO service pyramid model, which has self-care as the basis for all other forms of care, including informal community care and formal services. Further research is needed in resettlement and transit countries to guide mental health service delivery and primary healthcare initiatives.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1: Table 1-Study characteristics. Table 2-Participant characteristics. Table 3-Intervention. Table 4-Effectiveness. Table 5-Cultural appropriateness. Table 6-Participant experience
Supplementary Material 2: PRISMA 2020 Checklist
Acknowledgements
The authors express their gratitude to the School Librarian, Ms Lily Collison, for her time during multiple consultations and reviewing the initial search strategy.
List of abbreviations
- CBPT
Cognitive Behavioural Play Therapy
- CBT
Cognitive Behavioural Therapy
- HIC
High-Income Country
- JBI
Joanna Briggs Institute
- LIC
Low-Income Country
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PTSD
Posttraumatic Stress Disorder
- TRT
Teaching Recovery Techniques
- UMIC
Upper Middle-Income Country
- WHO
World Health Organization
Author contributions
DM, IB, PHT, NR and SSY contributed to the conception and design of the study. DM, IB, PHT and SSY were involved in the study methodology (study selection, quality assessment and data extraction). DM performed the data interpretation under the guidance of IB and SSY. DM drafted the initial manuscript. All authors contributed to the manuscript revisions. All authors read and approved the final manuscript.
Funding
No funding was sought for this study. Access to Covidence was provided by Translational Health Research Institute and open access publishing was supported by Western Sydney University Library and supervisor funds.
Data Availability
The authors confirm that the data supporting the findings of this study are available within the article [and its supplementary information files].
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.United Nations High Commissioner for Refugees (UNHCR) Global trends: forced displacement in 2022. Geneva: Switzerland; 2023. [Google Scholar]
- 2.United Nations High Commissioner for Refugees (UNHCR). UNHCR Resettlement Handbook 2011. 2011.
- 3.Organization for Economic Co-operation and Development (OECD). International Migration Outlook 2020. 2020. Paris, France: OECD Publishing. 10.1787/ec98f531-en
- 4.United Nations High Commissioner for Refugees (UNHCR). Refugee Data Finder. 2023 [cited 2023 November 6]. Available from: https://www.unhcr.org/refugee-statistics/
- 5.Silove D, Ventevogel P, Rees S. The contemporary refugee crisis: an overview of mental health challenges. World Psychiatry. 2017;16(2):130–9. doi: 10.1002/wps.20438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fazel M, Wheeler J, Danesh J. Prevalence of serious mental disorder in 7000 refugees resettled in western countries: a systematic review. Lancet. 2005;365(9467):1309–14. doi: 10.1016/S0140-6736(05)61027-6. [DOI] [PubMed] [Google Scholar]
- 7.Porter M, Haslam N. Predisplacement and postdisplacement factors associated with mental health of refugees and internally displaced persons: a meta-analysis. JAMA. 2005;294(5):602–12. doi: 10.1001/jama.294.5.602. [DOI] [PubMed] [Google Scholar]
- 8.Steel Z, Chey T, Silove D, Marnane C, Bryant RA, Van Ommeren M. Association of Torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: a systematic review and meta-analysis. JAMA. 2009;302(5):537–49. doi: 10.1001/jama.2009.1132. [DOI] [PubMed] [Google Scholar]
- 9.Bogic M, Njoku A, Priebe S. Long-term mental health of war-refugees: a systematic literature review. BMC Int Health Hum Rights. 2015;15:29. doi: 10.1186/s12914-015-0064-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blackmore R, Boyle JA, Fazel M, Ranasinha S, Gray KM, Fitzgerald G, et al. The prevalence of mental Illness in refugees and asylum seekers: a systematic review and meta-analysis. PLoS Med. 2020;17(9):e1003337. doi: 10.1371/journal.pmed.1003337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peconga EK, Høgh Thøgersen M. Post-traumatic stress disorder, depression, and anxiety in adult Syrian refugees: what do we know? Scand J Public Health. 2020;48(7):677–87. doi: 10.1177/1403494819882137. [DOI] [PubMed] [Google Scholar]
- 12.Jakobsen M, Demott MA, Heir T. Prevalence of psychiatric disorders among unaccompanied asylum-seeking adolescents in Norway. Clin Pract Epidemiology Ment Health. 2014;10:53–8. doi: 10.2174/1745017901410010053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fazel M, Betancourt TS. Preventive mental health interventions for refugee children and adolescents in high-income settings. Lancet Child Adolesc Health. 2018;2(2):121–32. doi: 10.1016/S2352-4642(17)30147-5. [DOI] [PubMed] [Google Scholar]
- 14.Stark L, Robinson MV, Gillespie A, Aldrich J, Hassan W, Wessells M, et al. Supporting mental health and psychosocial wellbeing through social and emotional learning: a participatory study of conflict-affected youth resettled to the U.S. BMC Public Health. 2021;21(1):1620. doi: 10.1186/s12889-021-11674-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization (WHO). Mental health promotion and mental health care in refugees and migrants: technical guidance. Knowledge hub on health and migration. 2018.
- 16.Walther L, Kröger H, Tibubos AN, Ta T, von Scheve C, Schupp J, et al. Psychological distress among refugees in Germany: a cross-sectional analysis of individual and contextual risk factors and potential consequences for integration using a nationally representative survey. BMJ Open. 2020;10(8):e033658. doi: 10.1136/bmjopen-2019-033658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ziersch A, Due C, Walsh M. Discrimination: a health hazard for people from refugee and asylum-seeking backgrounds resettled in Australia. BMC Public Health. 2020;20(1):108. doi: 10.1186/s12889-019-8068-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Steel Z, Silove D, Brooks R, Momartin S, Alzuhairi B, Susljik I. Impact of immigration detention and temporary protection on the mental health of refugees. Br J Psychiatry. 2006;188:58–64. doi: 10.1192/bjp.bp.104.007864. [DOI] [PubMed] [Google Scholar]
- 19.Li SS, Liddell BJ, Nickerson A. The relationship between post-migration stress and psychological disorders in refugees and Asylum Seekers. Curr Psychiatry Rep. 2016;18(9):82. doi: 10.1007/s11920-016-0723-0. [DOI] [PubMed] [Google Scholar]
- 20.Ahmad F, Othman N, Hynie M, Bayoumi AM, Oda A, McKenzie K. Depression-level symptoms among Syrian refugees: findings from a Canadian longitudinal study. J Ment Health. 2021;30(2):246–54. doi: 10.1080/09638237.2020.1765998. [DOI] [PubMed] [Google Scholar]
- 21.Chu T, Keller AS, Rasmussen A. Effects of post-migration factors on PTSD outcomes among immigrant survivors of political Violence. J Immigr Minor Health. 2013;15(5):890–7. doi: 10.1007/s10903-012-9696-1. [DOI] [PubMed] [Google Scholar]
- 22.Minas H, Kakuma R, Too LS, Vayani H, Orapeleng S, Prasad-Ildes R, et al. Mental health research and evaluation in multicultural Australia: developing a culture of inclusion. Int J Ment Health Syst. 2013;7(1):23. doi: 10.1186/1752-4458-7-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kirmayer LJ, Narasiah L, Munoz M, Rashid M, Ryder AG, Guzder J, et al. Common mental health problems in immigrants and refugees: general approach in primary care. CMAJ. 2011;183(12):E959–E67. doi: 10.1503/cmaj.090292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ferdinand AS, Paradies Y, Kelaher M. Mental health impacts of racial discrimination in Australian culturally and linguistically diverse communities: a cross-sectional survey. BMC Public Health. 2015;15:401. doi: 10.1186/s12889-015-1661-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Renzaho AM, Dhingra N, Georgeou N. Youth as contested sites of culture: the intergenerational acculturation gap amongst new migrant communities-parental and young adult perspectives. PLoS ONE. 2017;12(2):e0170700. doi: 10.1371/journal.pone.0170700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Correa-Velez I, Sundararajan V, Brown K, Gifford SM. Hospital utilisation among people born in refugee-source countries: an analysis of hospital admissions, Victoria, 1998–2004. Med J Aust. 2007;186(11):577–80. doi: 10.5694/j.1326-5377.2007.tb01058.x. [DOI] [PubMed] [Google Scholar]
- 27.Sareen J, Jagdeo A, Cox BJ, Clara I, ten Have M, Belik SL, et al. Perceived barriers to mental health service utilization in the United States, Ontario, and the Netherlands. Psychiatr Serv. 2007;58(3):357–64. doi: 10.1176/ps.2007.58.3.357. [DOI] [PubMed] [Google Scholar]
- 28.Kim G, Aguado Loi CX, Chiriboga DA, Jang Y, Parmelee P, Allen RS. Limited English proficiency as a barrier to mental health service use: a study of Latino and Asian immigrants with psychiatric disorders. J Psychiatr Res. 2011;45(1):104–10. doi: 10.1016/j.jpsychires.2010.04.031. [DOI] [PubMed] [Google Scholar]
- 29.Mitschke DB, Mitschke AE, Slater HM, Teboh C. Uncovering Health and Wellness Needs of Recently Resettled Karen Refugees from Burma. J Hum Behav Soc Environ. 2011;21(5):490–501. doi: 10.1080/10911359.2011.566466. [DOI] [Google Scholar]
- 30.Slewa-Younan S, Mond J, Bussion E, Mohammad Y, Uribe Guajardo MG, Smith M, et al. Mental health literacy of resettled Iraqi refugees in Australia: knowledge about posttraumatic stress disorder and beliefs about helpfulness of interventions. BMC Psychiatry. 2014;14:320. doi: 10.1186/s12888-014-0320-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Straiton M, Grant JF, Winefield HR, Taylor A. Mental health in immigrant men and women in Australia: the North West Adelaide health study. BMC Public Health. 2014;14:1–15. doi: 10.1186/1471-2458-14-1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim I, Beyond Trauma Post-resettlement factors and Mental Health outcomes among latino and Asian refugees in the United States. J Immigr Minor Health. 2016;18(4):740–8. doi: 10.1007/s10903-015-0251-8. [DOI] [PubMed] [Google Scholar]
- 33.Byrow Y, Pajak R, McMahon T, Rajouria A, Nickerson A. Barriers to Mental Health help-seeking Amongst Refugee men. Int J Environ Res Public Health. 2019;16(15):2634. doi: 10.3390/ijerph16152634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Byrow Y, Pajak R, Specker P, Nickerson A. Perceptions of mental health and perceived barriers to mental health help-seeking amongst refugees: a systematic review. Clin Psychol Rev. 2020;75:101812. doi: 10.1016/j.cpr.2019.101812. [DOI] [PubMed] [Google Scholar]
- 35.Folkman S, Chesney M, McKusick L, Ironson G, Johnson D, Coates TJ. The social context of coping. NY: Plenum Press; 1991. Translating coping theory into an intervention. [Google Scholar]
- 36.Carpinello S, Knight E, Janis L. A study of the meaning of self-help, self-help processes, and outcomes. Third Annual Conference on State Mental Health Agency Services Research NASMHPD Research Institute, Inc; Arlington, VA. 1992:37–44.
- 37.World Health Organization (WHO). Promoting mental health: concepts, emerging evidence, practice. Summary report. Geneva; 2004.
- 38.World Health Organization (WHO) WHO guideline on self-care interventions for health and well-being, 2022 revision: executive summary. Geneva: World Health Organization; 2022. [Google Scholar]
- 39.World Health Organization (WHO). Improving health systems and services for mental health. WHO mental health policy and service guidance package. 2009.
- 40.World Health Organization (WHO). Self-care in the context of primary health care. 2009.
- 41.Jorm AF, Christensen H, Griffiths KM, Rodgers B. Effectiveness of complementary and self-help treatments for depression. MJA. 2002;176(10):84–96. doi: 10.5694/j.1326-5377.2002.tb04508.x. [DOI] [PubMed] [Google Scholar]
- 42.Jorm AF, Griffiths KM. Population promotion of informal self-help strategies for early intervention against depression and anxiety. Psychol Med. 2006;36(1):3–6. doi: 10.1017/S0033291705005659. [DOI] [PubMed] [Google Scholar]
- 43.Morgan AJ, Jorm AF. Self-help interventions for depressive disorders and depressive symptoms: a systematic review. Ann Gen Psychiatry. 2008;7(1):13. doi: 10.1186/1744-859X-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mehjabeen D, Slewa-Younan S, Blignault I, Reavley N, Taha P. Examining self-help strategies to mitigate mental health issues within Arabic-speaking refugee and migrant populations globally: A systematic review protocol. PROSPERO 2021 CRD42021265456 2021 Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021265456
- 46.Barker TH, Stone JC, Sears K, Klugar M, Leonardi-Bee J, Tufanaru C et al. Revising the JBI quantitative critical appraisal tools to improve their applicability: an overview of methods and the development process. JBI Evid Synth. 2022. [DOI] [PubMed]
- 47.Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the conduct of narrative synthesis in systematic reviews. Lancaster University; 2006.
- 48.Irfaeya M, The application of Community Oriented Primary Care (COPC). Approach on assessing psychological stress among Arab migrant women in the City of Cologne/Germany. [Doctoral thesis]. Germany: University of Bielefeld; 2006.
- 49.Irfaeya M, Maxwell AE, Krämer A. Assessing psychological stress among Arab migrant women in the City of Cologne/Germany using the Community Oriented Primary Care (COPC) approach. J Immigr Minor Health. 2008;10(4):337–44. doi: 10.1007/s10903-007-9091-5. [DOI] [PubMed] [Google Scholar]
- 50.International Medical Corps Lebanon. Psychosocial assessment of displaced Syrians at the Lebanese-Syrian northern border. 2011.
- 51.Boswall K, Akash RA. Personal perspectives of protracted displacement: an ethnographic insight into the isolation and coping mechanisms of Syrian women and girls living as urban refugees in northern Jordan. Interv. 2015;13(3):203–15. [Google Scholar]
- 52.Campbell R. ‘What Can We Do? We Have To Live This Life!’ The lived experiences of elderly Palestinian refugees living in Lebanon, how do those experiences influence health and the refugees’ ability to manage health as they age? [Doctoral thesis]. Australia: Flinders University; 2017.
- 53.International Medical Corps. Understanding the mental health and psychosocial needs, and service utilization of Syrian refugees and Jordanian nationals: a qualitative & quantitative analysis in the Kingdom of Jordan. (Assessment Report). 2017.
- 54.MakkiAlamdari S. Resilience-related outcomes among war-affected Arab refugees in the U.S. [Doctoral Thesis]. United States: Indiana University; 2020.
- 55.Zbidat A, Georgiadou E, Borho A, Erim Y, Morawa E. The perceptions of trauma, complaints, somatization, and coping strategies among Syrian refugees in Germany—A qualitative study of an at-risk population. Int J Environ Res Public Health. 2020;17(3). [DOI] [PMC free article] [PubMed]
- 56.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bryant RA, Bawaneh A, Awwad M, Al-Hayek H, Giardinelli L, Whitney C, et al. Effectiveness of a brief group behavioral intervention for common mental disorders in Syrian refugees in Jordan: a randomized controlled trial. PLoS Med. 2022;19(3):e1003949. doi: 10.1371/journal.pmed.1003949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bryant RA, Bawaneh A, Awwad M, Al-Hayek H, Giardinelli L, Whitney C, et al. Twelve-month follow-up of a randomised clinical trial of a brief group psychological intervention for common mental disorders in Syrian refugees in Jordan. Epidemiol Psychiatr Sci. 2022;31:e81. doi: 10.1017/S2045796022000658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.The World Bank. World Bank country and lending groups. 2022 [cited 2022 March 16]. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups
- 60.Kadri R. Resettling the unsettled: the refugee journey of Arab Muslims to New Zealand. [Doctoral thesis]. New Zealand: Auckland University of Technology; 2009.
- 61.Al-Ajarma Y. The role of the arts toward healing trauma and building resilience in the Palestinian community. [Doctoral thesis]. United States: Lesley University; 2010.
- 62.Ferguson C. Stress and coping among Iraqi refugee men. [Master’s thesis]. United States: California State University; 2015.
- 63.Qureshi R. An exploration of Syrian refugees’ coping strategies during the Syrian conflict: a UK-based study. [Doctoral thesis]. United Kingdom: The University of Manchester; 2016.
- 64.Keshavarzi S. Stress, coping, and religiosity among recent Syrian refugees in Canada. [Master’s thesis]. Canada: University of Windsor; 2018.
- 65.Nashwan A, Cummings SM, Gagnon K. Older female Iraqi refugees in the United States: voices of struggle and strength. Int Soc Work. 2019;62(2):653–68. doi: 10.1177/0020872817742699. [DOI] [Google Scholar]
- 66.Jamil RR. Mental health and Arab Canadian immigrants: risks, protective factors, and resilience. [Doctoral Thesis]. Canada: University of Windsor; 2020.
- 67.Renner A, Hoffmann R, Nagl M, Roehr S, Jung F, Grochtdreis T, et al. Syrian refugees in Germany: perspectives on mental health and coping strategies. J Psychosom Res. 2020;129:109906. doi: 10.1016/j.jpsychores.2019.109906. [DOI] [PubMed] [Google Scholar]
- 68.Alhaddad L, Goodwin R, Kanngiesser P. Challenges and coping: perspectives of Syrian and Iraqi refugee youth in Germany. J Adolesc Res. 2021.
- 69.Rayes D, Karnouk C, Churbaji D, Walther L, Bajbouj M. Faith-based coping among Arabic-speaking refugees seeking mental health services in Berlin, Germany: an exploratory qualitative study. Front Psychiatry. 2021;12. [DOI] [PMC free article] [PubMed]
- 70.Sim A, Puffer E, Ahmad A, Hammad L, Georgiades K. Resettlement, mental health, and coping: a mixed methods survey with recently resettled refugee parents in Canada. BMC Public Health. 2023;23(1):386. doi: 10.1186/s12889-023-15300-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rayes D. Empowering Syrian refugee youth living in urban and camp settings in Jordan: summary of International Medical Corps Youth Empowerment Program evaluation. 2017.
- 72.Panter-Brick C, Dajani R, Eggerman M, Hermosilla S, Sancilio A, Ager A. Insecurity, distress and mental health: experimental and randomized controlled trials of a psychosocial intervention for youth affected by the Syrian crisis. J Child Psychol Psychiatry. 2018;59(5):523–41. doi: 10.1111/jcpp.12832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Al-Dmour KA, Al-Safasfeh M. The impact of a counselling program on reducing the symptoms of posttraumatic stress disorder and developing life satisfaction among Syrian refugee female students. Dirasat: Hum Soc Sci. 2020:213–46.
- 74.Alsheikh Ali A. Efficiency of Intervention Counseling Program on the enhanced Psychological Well-being and reduced post-traumatic stress disorder symptoms among Syrian Women Refugee survivors. Clin Pract Epidemiol Ment Health. 2020;16:134–41. doi: 10.2174/1745017902016010134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.DePierro VK. Story, science, and self-care in a refugee community: initial impact of the field guide for Barefoot Psychology. 2020.
- 76.Doumit R, Kazandjian C, Militello LK. COPE for adolescent Syrian refugees in Lebanon: a brief cognitive-behavioral skill-building intervention to Improve Quality of Life and promote positive Mental Health. Clin Nurs Res. 2020;29(4):226–34. doi: 10.1177/1054773818808114. [DOI] [PubMed] [Google Scholar]
- 77.Mercy Corps. Middle East regional report. Middle East; 2020.
- 78.Raknes S. The Happy Helping Hand used by Syrian displaced adolescents in Lebanon: a pilot study of feasibility, usefulness and impact. White paper. 2020.
- 79.Skarneh HA, Ghaith SM. The effectiveness of a counseling program based on the mind-body model in reducing symptoms of post-traumatic stress disorder among trauma victims of Syrian refugee women to Jordan. J Educ Psychol. 2020;28(6):821–40. [Google Scholar]
- 80.Tashtoush R, Khawaldeh A. The effectiveness of a cognitive-behavioral counseling program in improving the level of psychosocial adjustment among a sample of Syrian refugee students in Jordan. Dirasat: Hum Soc Sci. 2020;29(3):555–78.
- 81.Al-Shahadat MS. The effect of a cognitive-behavioral counseling program on improving self-esteem and reducing psychological stress among Syrian refugee children in Jordan. Dirasat: Educ Sci. 2021;48(2):270–88. [Google Scholar]
- 82.Aladdin J, Hawamdeh S. The effect of a group counseling program based on cognitive-behavioral play therapy in reducing emotional and behavioral problems among a sample of Syrian refugee students. Jordan J Educ Sci. 2021;17(2):205–20. [Google Scholar]
- 83.Acarturk C, Uygun E, Ilkkursun Z, Carswell K, Tedeschi F, Batu M, et al. Effectiveness of a WHO self-help psychological intervention for preventing mental disorders among Syrian refugees in Turkey: a randomized controlled trial. World Psychiatry. 2022;21(1):88–95. doi: 10.1002/wps.20939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Al-Refai NS, Albahr NA, Migdady AF, Al-Mifleh EI, Shatnawi A, AlSobeh A. The effectiveness of a training program based on psychosocial support to improve psychological empowerment level among refugees in Jordan. J Psychol Educ Res. 2022;1(2).
- 85.Cuijpers P, Heim E, Abi Ramia J, Burchert S, Carswell K, Cornelisz I, et al. Effects of a WHO-guided digital health intervention for depression in Syrian refugees in Lebanon: a randomized controlled trial. PLoS Med. 2022;19(6):e1004025. doi: 10.1371/journal.pmed.1004025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Spaaij J, Kiselev N, Berger C, Bryant RA, Cuijpers P, de Graaff AM, et al. Feasibility and acceptability of Problem Management Plus (PM+) among Syrian refugees and asylum seekers in Switzerland: a mixed-method pilot randomized controlled trial. Eur J Psychotraumatol. 2022;13(1):2002027. doi: 10.1080/20008198.2021.2002027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Powell TM, Qushua N. A qualitative study of a mental health awareness intervention for Jordanian and resettled Syrian refugees in host communities. Int J Soc Psychiatry. 2023;69(1):161–72. doi: 10.1177/00207640221074808. [DOI] [PubMed] [Google Scholar]
- 88.Darychuk A, Jackson S. Understanding Community Resilience through the accounts of women living in West Bank Refugee Camps. Affil- J Women Soc Work. 2015;30(4):447–60. doi: 10.1177/0886109915572845. [DOI] [Google Scholar]
- 89.Tauson MM. Seeking asylum in Bangkok, Thailand: surviving, coping, and the wellbeing strategies of Palestinian-Syrian refugees. [Doctoral Thesis]. United Kingdom: University of Sussex; 2017.
- 90.Chaaya M, Sibai AM, Fayad R, El-Roueiheb Z. Religiosity and depression in older people: evidence from underprivileged refugee and non-refugee communities in Lebanon. Aging Ment Health. 2007;11(1):37–44. doi: 10.1080/13607860600735812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Gordon JS, Staples JK, He DY, Atti JA. Mind–body skills groups for posttraumatic stress disorder in Palestinian adults in Gaza. Traumatol. 2016;22(3):155–64. doi: 10.1037/trm0000081. [DOI] [Google Scholar]
- 92.Ibrahim A. Effectiveness of cognitive behavioral therapy in post-traumatic stress disorder for Syrian refugees in Khartoum State. [Master’s Thesis]. Sudan: Al Neelain University; 2017.
- 93.Nilsson H, Saboonchi F, Gustavsson C, Malm A, Gottvall M. Trauma-afflicted refugees’ experiences of participating in physical activity and exercise treatment: a qualitative study based on focus group discussions. Eur J Psychotraumatol. 2019;10(1):1699327. doi: 10.1080/20008198.2019.1699327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ahmad AO, Mansi MA, Abu Al-Fadl MA, Khattab KS. The effectiveness of a selective treatment program to reduce post-traumatic stress disorder among Syrian refugee children in Egypt and Germany. A pilot study (Egypt-Germany) J Educ Sci. 2020;3(3):1–34. [Google Scholar]
- 95.Husby SR, Carlsson J, Mathilde Scotte Jensen A, Glahder Lindberg L, Sonne C. Prevention of trauma-related mental health problems among refugees: a mixed-methods evaluation of the MindSpring group programme in Denmark. J Community Psychol. 2020;48(3):1028–39. doi: 10.1002/jcop.22323. [DOI] [PubMed] [Google Scholar]
- 96.Slewa-Younan S, McKenzie M, Thomson R, Smith M, Mohammad Y, Mond J. Improving the mental wellbeing of Arabic speaking refugees: an evaluation of a mental health promotion program. BMC Psychiatry. 2020;20(1):314. doi: 10.1186/s12888-020-02732-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.de Graaff AM, Cuijpers P, McDaid D, Park A, Woodward A, Bryant RA, et al. Peer-provided Problem Management Plus (PM+) for adult Syrian refugees: a pilot randomised controlled trial on effectiveness and cost-effectiveness. Epidemiol Psychiatr Sci. 2020;29:e162. doi: 10.1017/S2045796020000724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Blignault I, Saab H, Woodland L, O’Callaghan C. Cultivating mindfulness: evaluation of a community-based mindfulness program for Arabic-speaking women in Australia. Curr Psychol. 2021.
- 99.Röhr S, Jung FU, Pabst A, Grochtdreis T, Dams J, Nagl M, et al. A self-help app for Syrian refugees with posttraumatic stress (Sanadak): Randomized Controlled Trial. JMIR Mhealth Uhealth. 2021;9(1):e24807. doi: 10.2196/24807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hasha W, Igland J, Fadnes LT, Kumar BN, Heltne UM, Diaz E. Effect of a self-help group intervention using teaching recovery techniques to improve mental health among Syrian refugees in Norway: a randomized controlled trial. Int J Ment Health Syst. 2022;16(1):47. doi: 10.1186/s13033-022-00557-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.de Graaff AM, Cuijpers P, Twisk JWR, Kieft B, Hunaidy S, Elsawy M et al. Peer-provided psychological intervention for Syrian refugees: results of a randomised controlled trial on the effectiveness of Problem Management Plus. BMJ Mental Health. 2023;26(1). [DOI] [PMC free article] [PubMed]
- 102.Lindegaard T, Seaton F, Halaj A, Berg M, Kashoush F, Barchini R, et al. Internet-based cognitive behavioural therapy for depression and anxiety among Arabic-speaking individuals in Sweden: a pilot randomized controlled trial. Cogn Behav Ther. 2020;50(1):47–66. doi: 10.1080/16506073.2020.1771414. [DOI] [PubMed] [Google Scholar]
- 103.Lindegaard T, Kashoush F, Holm S, Halaj A, Berg M, Andersson G. Experiences of internet-based cognitive behavioural therapy for depression and anxiety among Arabic-speaking individuals in Sweden: a qualitative study. BMC Psychiatry. 2021;21(1):288. doi: 10.1186/s12888-021-03297-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Feen-Calligan H, Grasser LR, Nasser S, Sniderman D, Javanbakht A. Photovoice techniques and art therapy approaches with refugee and immigrant adolescents. Arts Psychother. 2023;83. [DOI] [PMC free article] [PubMed]
- 105.Kayrouz R, Dear BF, Johnston L, Gandy M, Fogliati VJ, Sheehan J, et al. A feasibility open trial of guided internet-delivered cognitive behavioural therapy for anxiety and depression amongst Arab australians. Internet Interv. 2015;2(1):32–8. doi: 10.1016/j.invent.2014.12.001. [DOI] [Google Scholar]
- 106.Kayrouz R, Dear BF, Karin E, Gandy M, Fogliati VJ, Terides MD, et al. A pilot study of self-guided internet-delivered cognitive behavioural therapy for anxiety and depression among Arabs. Internet Interv. 2016;3:18–24. doi: 10.1016/j.invent.2015.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Blignault I, Saab H, Woodland L, Comino E. Evaluation of the acceptability and clinical utility of an Arabic-language mindfulness CD in an Australian community setting. Transcult Psychiatry. 2019;56(3). [DOI] [PubMed]
- 108.Blignault I, Saab H, Woodland L, Mannan H, Kaur A. Effectiveness of a Community-based Group Mindfulness Program tailored for Arabic and Bangla-speaking migrants. Int J Ment Health Syst. 2021;15(1):32. doi: 10.1186/s13033-021-00456-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Blignault I, Saab H, Woodland L, Giourgas K, Baddah H. Promoting mental health and wellbeing in multicultural Australia: a collaborative regional approach. Int J Environ Res Public Health. 2022;19(5). [DOI] [PMC free article] [PubMed]
- 110.Khawaja NG, White KM, Schweitzer R, Greenslade JH. Difficulties and coping strategies of Sudanese refugees: a qualitative approach. Transcult Psychiatry. 2008;45(3):489–512. doi: 10.1177/1363461508094678. [DOI] [PubMed] [Google Scholar]
- 111.Gladden J. The coping skills of East African refugees: a Literature Review. Refug Surv Q. 2012;31(3):177–96. doi: 10.1093/rsq/hds009. [DOI] [Google Scholar]
- 112.Gladden J. Coping strategies of Sudanese Refugee women in Kakuma Refugee Camp, Kenya. Refug Surv Q. 2013;32(4):66–89. doi: 10.1093/rsq/hdt017. [DOI] [Google Scholar]
- 113.Ikafa I, Hack-Polay D, Walker J, Mahmoud AB. African migrants and stress coping strategies in Australia: implications for social work. Int Soc Work. 2021.
- 114.Close C, Kouvonen A, Bosqui T, Patel K, O’Reilly D, Donnelly M. The mental health and wellbeing of first generation migrants: a systematic-narrative review of reviews. Global Health. 2016;12(1):47. doi: 10.1186/s12992-016-0187-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Hasan SI, Yee A, Rinaldi A, Azham AA, Mohd Hairi F, Amer Nordin AS. Prevalence of common mental health issues among migrant workers: a systematic review and meta-analysis. PLoS ONE. 2021;16(12):e0260221. doi: 10.1371/journal.pone.0260221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.United Nations High Commissioner for Refugees (UNHCR) Global trends: forced displacement 2019. Geneva: Switzerland; 2020. [Google Scholar]
- 117.Jannesari S, Lotito C, Oram S, Turrini G. How does context influence the delivery of mental health interventions for asylum seekers and refugees in low- and middle-income countries? A qualitative systematic review. Int J Ment Health Syst. 2021;15(1):80. doi: 10.1186/s13033-021-00501-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Cruwys T, Haslam SA, Dingle GA, Haslam C, Jetten J. Depression and social identity: an integrative review. Pers Soc Psychol Rev. 2014;18(3):215–38. doi: 10.1177/1088868314523839. [DOI] [PubMed] [Google Scholar]
- 119.Siedlecki KL, Salthouse TA, Oishi S, Jeswani S. The relationship between Social Support and Subjective Well-Being Across Age. Soc Indic Res. 2014;117(2):561–76. doi: 10.1007/s11205-013-0361-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Bellamy C, Schmutte T, Davidson L. An update on the growing evidence base for peer support. Ment Health Soc Incl. 2017;21(3).
- 121.Saeri AK, Cruwys T, Barlow FK, Stronge S, Sibley CG. Social connectedness improves public mental health: investigating bidirectional relationships in the New Zealand attitudes and values survey. Aust N Z J Psychiatry. 2017;52(4):365–74. doi: 10.1177/0004867417723990. [DOI] [PubMed] [Google Scholar]
- 122.Marlowe J. Refugee resettlement, social media and the social organization of difference. Glob Netw. 2020;20(2):274–91. doi: 10.1111/glob.12233. [DOI] [Google Scholar]
- 123.El Azayem GA, Hedayat-Diba Z. The psychological aspects of Islam: Basic principles of Islam and their psychological corollary. Int J Psychol Relig. 1994;4(1):41–50. doi: 10.1207/s15327582ijpr0401_6. [DOI] [Google Scholar]
- 124.Krause N, Ellison C, Shaw B, Marcum J, Boardman J. Church-based Social Support and Religious Coping. J Sci Study Relig. 2001;40(4):637–56. doi: 10.1111/0021-8294.00082. [DOI] [Google Scholar]
- 125.Joshanloo M. A comparison of western and Islamic conceptions of happiness. J Happiness Stud. 2013;14(6):1857–74. doi: 10.1007/s10902-012-9406-7. [DOI] [Google Scholar]
- 126.Lambert L, Passmore H-A, Joshanloo M. A positive psychology intervention program in a culturally-diverse university: boosting happiness and reducing fear. J Happiness Stud. 2019;20(4):1141–62. doi: 10.1007/s10902-018-9993-z. [DOI] [Google Scholar]
- 127.Lutz PK, Passmore H-A. Repercussions of individual and societal valuing of happiness. Positive psychology in the Middle East/North Africa: Research, policy, and practice. Springer; 2019. pp. 363–90.
- 128.Markus HR, Kitayama S. Culture and the self: implications for cognition, emotion, and motivation. Psychol Rev. 1991;98(2):224. doi: 10.1037/0033-295X.98.2.224. [DOI] [Google Scholar]
- 129.Brewer MB, Chen YR. Where (who) are collectives in collectivism? Toward conceptual clarification of individualism and collectivism. Psychol Rev. 2007;114(1):133–51. doi: 10.1037/0033-295X.114.1.133. [DOI] [PubMed] [Google Scholar]
- 130.Basurrah AA, Al-Haj Baddar M, Di Blasi Z. Positive psychology interventions as an opportunity in Arab countries to promoting well-being. Front Psychol. 2022;12. [DOI] [PMC free article] [PubMed]
- 131.Hutchinson M, Dorsett P. What does the literature say about resilience in refugee people? Implications for practice. J Soc Incl. 2012;3(2):1–24. [Google Scholar]
- 132.Kanal M, Rottmann SB. Everyday agency: rethinking refugee women’s agency in specific cultural contexts. Front Psychol. 2021;12. [DOI] [PMC free article] [PubMed]
- 133.Miller KE, Rasmussen A. War experiences, daily stressors and mental health five years on: elaborations and future directions. Intervention. 2014;12:33–42. doi: 10.1097/WTF.0000000000000066. [DOI] [Google Scholar]
- 134.Riley A, Varner A, Ventevogel P, Taimur Hasan MM, Welton-Mitchell C. Daily stressors, trauma exposure, and mental health among stateless rohingya refugees in Bangladesh. Transcult Psychiatry. 2017;54(3):304–31. doi: 10.1177/1363461517705571. [DOI] [PubMed] [Google Scholar]
- 135.Eleftherakos C, van den Boogaard W, Barry D, Severy N, Kotsioni I, Roland-Gosselin L. I prefer dying fast than dying slowly, how institutional abuse worsens the mental health of stranded Syrian, Afghan and Congolese migrants on Lesbos island following the implementation of EU-Turkey deal. Confl Health. 2018;12:38. doi: 10.1186/s13031-018-0172-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Episkopou M, Venables E, Whitehouse K, Eleftherakos C, Zamatto F, de Bartolome Gisbert F, et al. In island containment: a qualitative exploration of social support systems among asylum seekers in a mental health care programme on Lesvos Island, Greece. Confl Health. 2019;13:34. doi: 10.1186/s13031-019-0218-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Spitzer C, Gläser S, Grabe HJ, Ewert R, Barnow S, Felix SB, et al. Mental health problems, obstructive lung Disease and lung function: findings from the general population. J Psychosom Res. 2011;71(3):174–9. doi: 10.1016/j.jpsychores.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 138.Wiltink J, Beutel ME, Till Y, Ojeda FM, Wild PS, Münzel T, et al. Prevalence of distress, comorbid conditions and well being in the general population. J Affect Disord. 2011;130(3):429–37. doi: 10.1016/j.jad.2010.10.041. [DOI] [PubMed] [Google Scholar]
- 139.Douki S, Ben Zineb S, Nacef F, Halbreich U. Women’s mental health in the Muslim world: Cultural, religious, and social issues. J Affect Disord. 2007;102(1):177–89. doi: 10.1016/j.jad.2006.09.027. [DOI] [PubMed] [Google Scholar]
- 140.Bener A, Ghuloum S. Gender difference on patients’ satisfaction and expectation towards mental health care. Niger J Clin Pract. 2013;16(3):285–91. doi: 10.4103/1119-3077.113448. [DOI] [PubMed] [Google Scholar]
- 141.AlSabah I. Why cultural context is vital when treating women traumatised by war: Weforum; 2021 Jun 2 [cited 2022 Jun 4]. Available from: https://www.weforum.org/agenda/2021/06/cultural-context-treating-women-traumatised-war/
- 142.Donnelly TT, Al Suwaidi J, Al Bulushi A, Al Enazi N, Yassin K, Rehman AM et al. The influence of cultural and social factors on healthy lifestyle of Arabic women. Avicenna. 2011;2011(1).
- 143.Donnelly TT, Al-Thani ABM, Benjamin K, Al-Khater AH, Fung TS, Ahmedna M, et al. Arab female and male perceptions of factors facilitating and inhibiting their physical activity: findings from a qualitative study in the Middle East. PLoS ONE. 2018;13(7):e0199336. doi: 10.1371/journal.pone.0199336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Koithan M. The inner healer: mind-body strategies for Health. J Nurse Pract. 2009;5(5):374–5. doi: 10.1016/j.nurpra.2009.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Ament-Lemke A. Healing the mind and body: practitioner perspectives on integrating cognitive and somatic approaches in psychotherapy with refugees, asylees, and asylum seekers. [Master’s thesis]. United States: St. Catherine University; 2018.
- 146.Anand A, Ghani A, Sharma K, Kaur G, Khosla R, Devi C, et al. War-related Mental Health issues and need for Yoga intervention studies: a scoping review. Int J Yoga. 2021;14(3):175–87. doi: 10.4103/ijoy.ijoy_60_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Felton E. Migrants’ use of the internet in re-settlement. 2012.
- 148.Wall M, Otis Campbell M, Janbek D. Syrian refugees and information precarity. New Media Soc. 2017;19(2):240–54. doi: 10.1177/1461444815591967. [DOI] [Google Scholar]
- 149.Burchert S, Alkneme MS, Bird M, Carswell K, Cuijpers P, Hansen P et al. User-centered app adaptation of a low-intensity e-mental health intervention for Syrian refugees. Front Psychiatry. 2019;9. [DOI] [PMC free article] [PubMed]
- 150.Carter H, Araya R, Anjur K, Deng D, Naslund JA. The emergence of digital mental health in low-income and middle-income countries: a review of recent advances and implications for the treatment and prevention of mental disorders. J Psychiatr Res. 2021;133:223–46. doi: 10.1016/j.jpsychires.2020.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Fu Z, Burger H, Arjadi R, Bockting CLH. Effectiveness of digital psychological interventions for mental health problems in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Psychiatry. 2020;7(10):851–64. doi: 10.1016/S2215-0366(20)30256-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Youssef J, Deane FP. Factors influencing mental-health help-seeking in Arabic-speaking communities in Sydney, Australia. Ment Health Relig Cult. 2006;9(1):43–66. doi: 10.1080/13674670512331335686. [DOI] [Google Scholar]
- 153.Kirmayer LJ. Rethinking cultural competence. Transcult Psychiatry. 2012;49(2):149–64. doi: 10.1177/1363461512444673. [DOI] [PubMed] [Google Scholar]
- 154.Alsan M, Garrick O, Graziani G. Does Diversity Matter for Health? Experimental evidence from Oakland. Am Econ Rev. 2019;109(12):4071–111. doi: 10.1257/aer.20181446. [DOI] [Google Scholar]
- 155.Lau LS, Rodgers G. Cultural competence in Refugee Service settings: a scoping review. Health Equity. 2021;5(1):124–34. doi: 10.1089/heq.2020.0094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Sullivan J, Thorn N, Amin M, Mason K, Lue N, Nawzir M. Using simple acupressure and breathing techniques to improve mood, sleep and pain management in refugees: a peer-to-peer approach in a Rohingya refugee camp. Intervention. 2019;17(2):252–8. doi: 10.4103/INTV.INTV_13_19. [DOI] [Google Scholar]
- 157.Mitschke DB, Praetorius RT, Kelly DR, Small E, Kim YK. Listening to refugees: how traditional mental health interventions may miss the mark. Int Soc Work. 2016;60(3):588–600. doi: 10.1177/0020872816648256. [DOI] [Google Scholar]
- 158.Holloway M, Moss B. Spirituality and social work. Macmillan International Higher Education; 2010.
- 159.Gray M, Coates J. Changing values and valuing change: toward an ecospiritual perspective in social work. Int J Soc Work. 2013;56(3):356–68. doi: 10.1177/0020872812474009. [DOI] [Google Scholar]
- 160.Hodge D. Spiritual assessment in social work and mental health practice. Columbia University Press; 2015.
- 161.George M, Ellison V. Incorporating spirituality into Social Work practice with migrants. Br J Soc Work. 2015;45(6):1717–33. doi: 10.1093/bjsw/bcu035. [DOI] [Google Scholar]
- 162.Pandya SP. Spirituality for Mental Health and Well-Being of Adult refugees in Europe. J Immigr Minor Health. 2018;20(6):1396–403. doi: 10.1007/s10903-018-0717-6. [DOI] [PubMed] [Google Scholar]
- 163.Maier K, Konaszewski K, Skalski SB, Büssing A, Surzykiewicz J. Spiritual needs, Religious Coping and Mental Wellbeing: a cross-sectional study among migrants and refugees in Germany. Int J Environ Res Public Health. 2022;19(6):3415. doi: 10.3390/ijerph19063415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Hall RE, Livingston JN. Mental health practice with Arab families: the implications of spirituality vis-a-vis Islam. Am J Fam Ther. 2006;34(2):139–50. doi: 10.1080/01926180500357883. [DOI] [Google Scholar]
- 165.Hiller RM, Halligan SL, Tomlinson M, Stewart J, Skeen S, Christie H. Post-trauma coping in the context of significant adversity: a qualitative study of young people living in an urban township in South Africa. BMJ Open. 2017;7(10):e016560. doi: 10.1136/bmjopen-2017-016560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Al-Seheel AY, Noor NM. Effects of an Islamic-based gratitude strategy on Muslim students’ level of happiness. Ment Health Relig Cult. 2016;19(7):686–703. doi: 10.1080/13674676.2016.1229287. [DOI] [Google Scholar]
- 167.Joshanloo M, Weijers D. Islamic perspectives on Wellbeing. In: Lambert L, Pasha-Zaidi N, editors. Positive Psychology in the Middle East/North Africa: Research, Policy, and Practise. Cham: Springer International Publishing; 2019. pp. 237–56. [Google Scholar]
- 168.Abdullah CH, Ismail HN, Ahmad NS, Hissan WS. Genaralized anxiety disorder (GAD) from Islamic and western perspectives. World J of Islamic History Civilization. 2012;2:44–52. [Google Scholar]
- 169.Doufesh H, Faisal T, Lim KS, Ibrahim F. EEG spectral analysis on Muslim prayers. Appl Psychophysiol Biofeedback. 2012;37:11–8. doi: 10.1007/s10484-011-9170-1. [DOI] [PubMed] [Google Scholar]
- 170.Dewiyanti D, Kusuma HE. Spaces for muslims spiritual meanings. Procedia Soc Behav Sci. 2012;50:969–78. doi: 10.1016/j.sbspro.2012.08.098. [DOI] [Google Scholar]
- 171.Council on Foreign Relations. The Sunni-Shia divide. 2016 [cited 2022 Jun 2]. Available from: https://www.cfr.org/article/sunni-shia-divide
- 172.Sayeed SA, Prakash A. The Islamic prayer (Salah/Namaaz) and Yoga togetherness in mental health. Indian J Psychiatry. 2013;55(Suppl 2):224–S30. doi: 10.4103/0019-5545.105537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Abu-Ras W, Gheith A, Cournos F. The imam’s role in mental health promotion: a study at 22 mosques in New York City’s Muslim community. J Muslim Ment Health. 2008;3(2):155–76. doi: 10.1080/15564900802487576. [DOI] [Google Scholar]
- 174.Ciftci A, Jones N, Corrigan PW. Mental health stigma in the Muslim community. J Muslim Ment Health. 2013;7(1).
- 175.Krstanoska-Blazeska K, Thomson R, Slewa-Younan S. Mental Illness Stigma and Associated factors among Arabic-speaking Religious and Community leaders. Int J Environ Res Public Health. 2021;18(15):7991. doi: 10.3390/ijerph18157991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Haith-Cooper M, Waskett C, Montague J, Horne M. Exercise and physical activity in asylum seekers in Northern England; using the theoretical domains framework to identify barriers and facilitators. BMC Public Health. 2018;18(1):762. doi: 10.1186/s12889-018-5692-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Knappe F, Colledge F, Gerber M. Impact of an 8-Week Exercise and Sport Intervention on Post-traumatic Stress Disorder Symptoms, Mental Health, and physical fitness among male refugees living in a Greek Refugee Camp. Int J Environ Res Public Health. 2019;16(20):3904. doi: 10.3390/ijerph16203904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Purgato M, Richards J, Prina E, Kip A, Del Piccolo L, Michencigh G, et al. Efficacy of physical activity interventions on psychological outcomes in refugee, asylum seeker and migrant populations: a systematic review and meta-analysis. Sport Exerc Perform Psychol. 2021;54:101901. doi: 10.1016/j.psychsport.2021.101901. [DOI] [Google Scholar]
- 179.Stuckey HL, Nobel J. The connection between art, healing, and public health: a review of current literature. Am J Public Health. 2010;100(2):254–63. doi: 10.2105/AJPH.2008.156497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Hajra B, Saleem T. The Use of Islamic Patterned Art Therapy: Healing of psychological problems among University students. J Relig Health. 2021;60(6):4361–86. doi: 10.1007/s10943-021-01240-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Heyeres M, Perera N, Udah H, Attakey A, Whiteside M, Tsey K. Interventions targeting the wellbeing of migrant youths: a systematic review of the literature. SAGE Open 2021;11(3).
- 182.Commission on Social Determinants of Health (CSDH) Closing the gap in a generation: health equity through action on the social determinants of health. Final report of the Commission on Social Determinants of Health. Geneva: World Health Organization; 2008. [Google Scholar]
- 183.Derr AS. Mental Health Service Use among immigrants in the United States: a systematic review. Psychiatr Serv. 2016;67(3):265–74. doi: 10.1176/appi.ps.201500004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Kiselev N, Pfaltz M, Haas F, Schick M, Kappen M, Sijbrandij M, et al. Structural and socio-cultural barriers to accessing mental healthcare among Syrian refugees and asylum seekers in Switzerland. Eur J Psychotraumatol. 2020;11(1):1717825. doi: 10.1080/20008198.2020.1717825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Coates B, Wiltshire T, Reysenbach T. Short-changed: how to stop the exploitation of migrant workers in Australia. Grattan Institute; 2023.
- 186.World Health Organization (WHO) WHO Guideline: recommendations on Digital interventions for Health System strengthening. Geneva: World Health Organization; 2019. [PubMed] [Google Scholar]
- 187.Aldridge AA, Roesch SC. Developing coping typologies of minority adolescents: a latent profile analysis. J Adolesc. 2008;31(4):499–517. doi: 10.1016/j.adolescence.2007.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material 1: Table 1-Study characteristics. Table 2-Participant characteristics. Table 3-Intervention. Table 4-Effectiveness. Table 5-Cultural appropriateness. Table 6-Participant experience
Supplementary Material 2: PRISMA 2020 Checklist
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article [and its supplementary information files].