Abstract
Background
Peritoneal dialysis (PD) is an essential lifesaving treatment for end-stage renal disease. However, PD therapy is limited by peritoneal inflammation, which leads to peritoneal membrane failure because of progressive peritoneal deterioration. Peritonitis is the most common complication in patients undergoing PD. Thus, elucidating the mechanism of chronic peritoneal inflammation after PD-associated peritonitis is an urgent issue for patients undergoing PD. This first case report suggests that an increased interleukin-1β (IL-1β) expression in the peritoneal dialysate after healing of peritonitis can contribute to peritoneal deterioration.
Case presentation
A 64-year-old woman was diagnosed with diabetes mellitus 10 years ago and had been started on PD for end-stage renal disease. One day, the patient developed PD-associated acute peritonitis and was admitted to our hospital for treatment. Thus, treatment with antimicrobial agents was initiated for PD-associated peritonitis. Dialysate turbidity gradually disappeared after treatment with antimicrobial agents, and the number of cells in the PD fluid decreased. After 2 weeks of antimicrobial therapy, peritonitis was clinically cured, and the patient was discharged. Thereafter, the patient did not develop peritonitis; however, residual renal function tended to decline, and peritoneal function also decreased in a relatively short period. We evaluated pro-inflammatory cytokine levels before and after PD-associated peritonitis; interestingly, the levels of IL-1β remained high in the PD fluid, even after remission of bacterial peritonitis. In addition, it correlated with decreased peritoneal function.
Conclusions
This case suggests that inflammasome-derived pro-inflammatory cytokines may contribute to chronic inflammation-induced peritoneal deterioration after PD-related peritonitis is cured.
Keywords: Chronic inflammation, IL-1β, Inflammasome, Peritoneal dialysis, Peritonitis
Background
Peritoneal dialysis (PD) is a viable option for renal replacement therapy in patients with end-stage renal disease [1]. Moreover, it is a home-based treatment suitable for improving a patient's quality of life [2]. However, prolonged exposure to dialysis solutions often deteriorates the peritoneum [3]. Peritoneal deterioration is a comprehensive concept that comprises decreased peritoneal function and morphological changes in the peritoneum [4, 5]. Additionally, prolonged exposure to PD fluid triggers chronic inflammation and may contribute to peritoneal deterioration [6]. Therefore, it is important to elucidate the main locus of chronic inflammatory pathogenesis to prevent peritoneal deterioration.
Inflammasomes are intracellular multimeric complex molecules that recognize pathogen-associated or danger-associated molecular patterns [7]. The NLRP3 inflammasome can trigger chronic low-grade inflammation [8] and the pathogenesis of multiple complex diseases, including chronic kidney disease [9], atherosclerosis [10], type 2 diabetes [11], and Alzheimer’s disease [12]. Activation the NLRP3 inflammasome and its downstream pathway particularly reduces pro-caspase-1 activation and caspase-1-mediated interleukine-1β (IL-1β) maturation, accelerating organ fibrosis [13]. Moreover, NLRP3 activation and IL-1β release are critical for solute transport defects and tissue remodeling in PD-associated peritonitis [14]. However, the involvement of inflammasome activation in chronic inflammation after the onset of peritonitis and its role in peritoneal deterioration have not been elucidated. To our knowledge, this study is the first to report persistently high levels of IL-1β in a patient who underwent PD and despite being clinically cured for peritonitis, her peritoneal function decreased in a relatively short period.
Case presentation
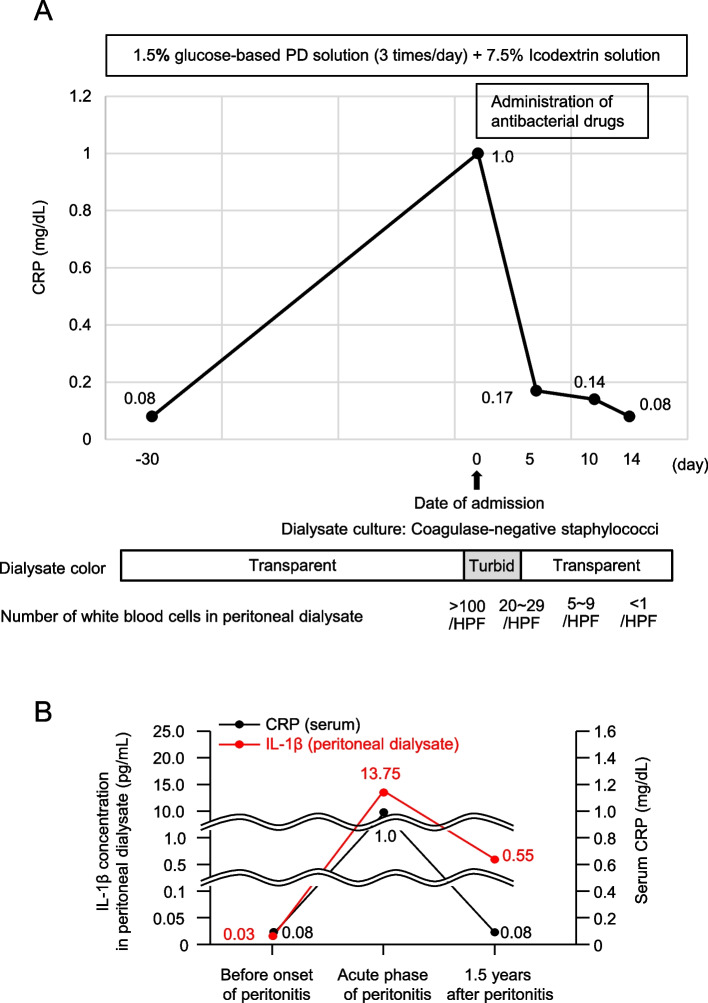
A 64-year-old woman was diagnosed with diabetes mellitus 10 years ago and had been started on PD for end-stage renal disease. Continuous ambulatory PD (low-calcium PD solution with 1.5% dextrose three times per day and 7.5% icodextrin solution once per day; Baxter, Deerfield, IL, USA) was administered, and the patient performed well in an outpatient setting. However, one day, the patient suddenly noticed turbid PD fluid accompanied by a low-grade fever. The patient developed PD-associated acute peritonitis and was admitted to our hospital for treatment. Laboratory results showed elevated C-reactive protein levels and an increased number of white blood cells in the peritoneal dialysate. Coagulase-negative staphylococci were detected in dialysate cultures. Thus, treatment with antimicrobial agents was initiated for PD-associated peritonitis. Dialysate turbidity gradually disappeared after treatment with antimicrobial agents, and the number of cells in the PD fluid decreased. After 2 weeks of antimicrobial therapy, peritonitis was clinically cured, and the patient was discharged (Fig. 1A). Thereafter, the patient did not develop peritonitis; however, residual renal function tended to decline, and peritoneal function also decreased in a relatively short period. We evaluated pro-inflammatory cytokine levels before and after PD-associated peritonitis; interestingly, the levels of IL-1β remained high in the PD fluid, even after remission of bacterial peritonitis (Fig. 1B). However, it became difficult to continue PD any further (Fig. 2A). The protein expression of IL-1β (R&D Systems) in the PD effluent was examined using commercial Quantikine ELISA kits, according to the manufacturer’s protocol. The PD effluent was concentrated using centrifugal filters (Amicon Ultra Centrifugal Filters; Millipore) and the concentration of cytokines in the PD effluent was expressed as pg/mg total protein.
Fig. 1.
Clinical course and IL-1β concentrations of dialysate. A Clinical course during PD-associated peritonitis. After 2 weeks of antimicrobial therapy, peritonitis was clinically cured, and the patient was discharged. B Clinical course before and after the onset of bacterial peritonitis. CRP, C-reactive protein; HPF, high-power field; IL-1β, interleukin-1β
Fig. 2.
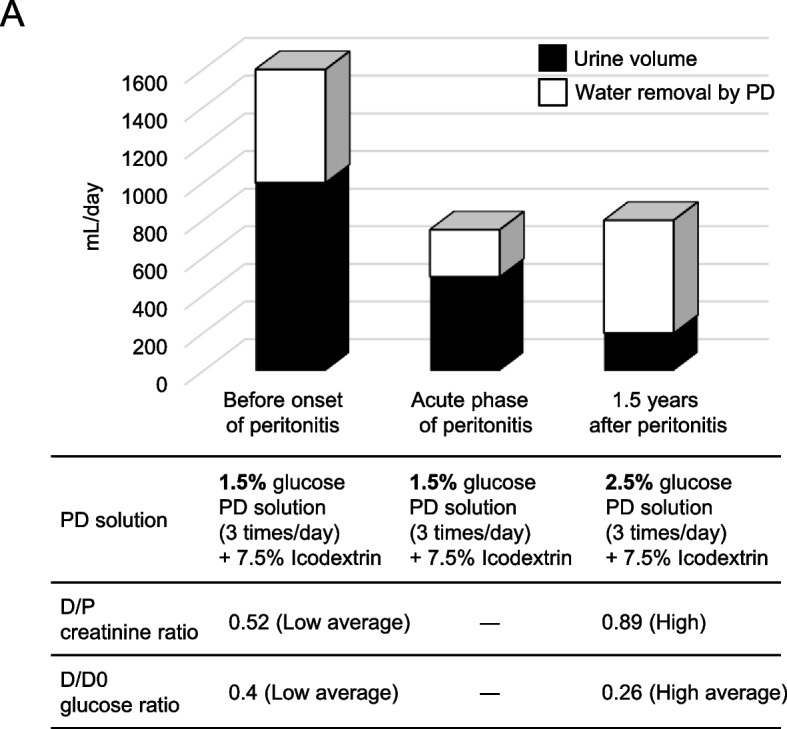
Analysis of peritoneal equilibration test in a patient with PD. A Analysis of peritoneal equilibration test before and after the onset of bacterial peritonitis. D, dialysate; P, plasma; PD, peritoneal dialysis
Discussion and conclusions
To the best of our knowledge, this case report is the first to report an increase in the IL-1β levels of peritoneal dialysate despite healing from PD-related bacterial peritonitis. We also assessed IL-1β expression in the peritoneal dialysate of patients without a history of peritonitis and found no increase in IL-1β levels in the peritoneal dialysate (data not shown), suggesting that IL-1β can affect peritoneal deterioration.
Peritoneal deterioration is inevitable in patients undergoing long-term PD. It is essential to treat patients with PD, while minimizing their peritoneal burden as much as possible. Peritonitis is the most common complication in the aforementioned type of patients [15]. Therefore, preventing it is of utmost importance; if peritonitis develops, surrogate markers are needed to assess subsequent peritoneal deterioration. Recently, NLRP3 inflammasome activation and IL-1β release have been reported to play critical roles in solute transport defects and tissue remodeling in PD-associated acute peritonitis [14]. However, it remains unclear whether inflammasome-dependent inflammatory cytokine levels are persistently elevated after PD-related acute peritonitis. We showed that, even if patients who underwent PD are clinically cured of PD-related acute peritonitis, chronic inflammation may affect the long-term effectiveness of PD.
As for cells releasing IL-1β, PD-related peritonitis has been reported to occur predominantly in resident peritoneal monocytes and macrophages [14], with the former playing a pivotal role in the progression of peritoneal deterioration [16–18]. Macrophages are likely to remain in peritoneal tissue after the onset of PD-related acute peritonitis. Notably, significant changes in the prevalence of macrophage/monocyte populations vary widely in patients undergoing PD depending on the history of peritonitis [19]. Accordingly, macrophage accumulation in peritoneal tissue may reflect chronic peritoneal inflammation after PD-related acute peritonitis. We were unable to identify the source of cells because we were unable to obtain peritoneal tissue from the patient, making this an issue for future consideration.
What are the possible factors that lead to persistent peritoneal inflammation and lead to rapid deterioration of peritoneal function? We consider the CD44-hyaluronan interaction an important factor in the persistence of inflammasome-derived microinflammation, despite the clinical resolution of peritonitis. We recently reported that inflammasome activation in CD44-positive macrophages contributes to peritoneal degradation [20]. Based on our most recent research data, we used in vivo imaging techniques to demonstrate that CD44-positive macrophages infiltrate the subperitoneal mesothelial cells from the blood as a mechanism for the development of peritoneal fibrosis. The ligand for CD44 is hyaluronic acid (HA), which has emerged as an important adhesion molecule for cellular trafficking in multiple organs and contributes to the pathogenesis of various inflammatory diseases [21]. HA in peritoneal dialysate may be useful as a marker for assessing functional and morphological changes in patients undergoing long-term PD [22]. Moreover, CD44 and subsequent HA catabolism trigger the activation of inflammasomes [23]. Although we were not able to analyze this in our case report, it is likely that some mechanism caused small amounts of HA and CD44-positive macrophages to remain after the peritonitis had healed, resulting in persistent inflammation. HA accumulation and several CD44-positive macrophages may regulate the transition from acute to chronic inflammation.
Several studies have indicated that diabetes mellitus (DM) is a risk factor for PD-associated peritonitis [24–26]. Patients with diabetes are compromised hosts and experience several complications. In addition, PD is often mistaken as a potential contributor to visual disorders and peripheral neuropathy [27, 28]. Moreover, Joshi et al. found that glucose load impairs the peritoneal defense system [29]. Thus, DM may affect the incidence of PD-associated peritonitis through several mechanisms.
Regarding the association between DM and decline of residual renal function, inflammasome activation has also been reported in patients with DM [30]. In a previous study, renal biopsies of patients with diabetic nephropathy with proteinuria revealed the expression of inflammasome-associated proteins, such as caspase-1, IL-1β, and IL-18, in the distal and proximal tubules, which is correlated with the degree of proteinuria [31]. Proteinuria can independently predict the rate of decline in residual renal dysfunction in patients with PD [32–34]. Thus, inflammasome activation in diabetic nephropathy may have contributed to the decline in residual renal function in our patient. Conversely, it is difficult to explain why residual renal function declined after peritonitis in our case. It is evident that a multifunctional process, including fluctuations in body fluid status, the antibiotics used for the peritonitis [35], and the peritonitis itself, may individually or collectively contribute to this process. Moreover, the persistence of inflammasome activation after peritonitis may contribute to the decline of residual renal function in patients with DM through some mechanism. However, there are no reports that diabetes itself contributes to peritoneal deterioration associated with inflammasome activation. Furthermore, whether inflammasome-derived proinflammatory cytokines in the peritoneal dialysate of patients with PD contribute to peritoneal degradation remains unclear. Our study could not confirm a causal relationship between IL-1β and peritoneal deterioration. However, in patients without a history of peritonitis, IL-1β levels in the peritoneal dialysate were not elevated, and their peritoneal function was not compromised (data not shown). We consider IL-1β immediately before and after the onset of peritonitis to be clinically essential findings. Increasing the number of cases in future studies to determine whether inflammasome-derived IL-1β serves as a surrogate marker for peritoneal deterioration after peritonitis will have great clinical significance.
In conclusion, the findings of this case report suggest that IL-1β expression in peritoneal dialysate is an important factor in peritoneal deterioration after healing of PD-associated peritonitis. After the onset of bacterial-induced acute peritonitis in patients undergoing PD, inflammasome-dependent inflammation was prolonged, even though peritonitis was clinically cured. Thus, inflammasome-derived pro-inflammatory cytokines may contribute to chronic inflammation-induced peritoneal deterioration after PD-related peritonitis is cured.
Acknowledgements
The authors would like to thank the patient and her family for their contribution to this study. We also thank Yoshiko Shirakiya for her assistance with the analysis of IL-1β expression in the peritoneal dialysate.
Authors’ contributions
HK prepared the manuscript. AH, YY, and SK managed PD. TS and NK reviewed and edited the manuscript. All authors have read and approved the final manuscript.
Funding
None.
Availability of data and materials
No datasets were generated or analyzed during the current study.
Declarations
Ethics approval and consent to participate
This study was designed in accordance with the Helsinki Declaration, and was approved by Kawasaki Medical School Institutional Review Board.
Consent for publication
Written informed consent was obtained from the patient for the publication of this case report.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Jain AK, Blake P, Cordy P, Garg AX. Global trends in rates of peritoneal dialysis. J Am Soc Nephrol. 2012;23(3):533–544. doi: 10.1681/ASN.2011060607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chaudhary K, Sangha H, Khanna R. Peritoneal dialysis first: rationale. Clin J Am Soc Nephrol. 2011;6(2):447–456. doi: 10.2215/CJN.07920910. [DOI] [PubMed] [Google Scholar]
- 3.Churchill DN, Thorpe KE, Nolph KD, Keshaviah PR, Oreopoulos DG, Page D. Increased peritoneal membrane transport is associated with decreased patient and technique survival for continuous peritoneal dialysis patients. The Canada-USA (CANUSA) Peritoneal Dialysis Study Group. J Am Soc Nephrol. 1998;9(7):1285–1292. doi: 10.1681/ASN.V971285. [DOI] [PubMed] [Google Scholar]
- 4.Pletinck A, Vanholder R, Veys N, Van Biesen W. Protecting the peritoneal membrane: factors beyond peritoneal dialysis solutions. Nat Rev Nephrol. 2012;8(9):542–550. doi: 10.1038/nrneph.2012.144. [DOI] [PubMed] [Google Scholar]
- 5.Kadoya H, Satoh M, Nishi Y, Kondo M, Wada Y, Sogawa Y, et al. Klotho is a novel therapeutic target in peritoneal fibrosis via Wnt signaling inhibition. Nephrol Dial Transplant. 2020;35(5):773–781. doi: 10.1093/ndt/gfz298. [DOI] [PubMed] [Google Scholar]
- 6.Aroeira LS, Aguilera A, Sanchez-Tomero JA, Bajo MA, del Peso G, Jimenez-Heffernan JA, et al. Epithelial to mesenchymal transition and peritoneal membrane failure in peritoneal dialysis patients: pathologic significance and potential therapeutic interventions. J Am Soc Nephrol. 2007;18(7):2004–2013. doi: 10.1681/ASN.2006111292. [DOI] [PubMed] [Google Scholar]
- 7.Herwald H, Egesten A. On PAMPs and DAMPs. J Innate Immun. 2016;8(5):427–428. doi: 10.1159/000448437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lu A, Magupalli VG, Ruan J, Yin Q, Atianand MK, Vos MR, et al. Unified polymerization mechanism for the assembly of ASC-dependent inflammasomes. Cell. 2014;156(6):1193–1206. doi: 10.1016/j.cell.2014.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vilaysane A, Chun J, Seamone ME, Wang W, Chin R, Hirota S, et al. The NLRP3 inflammasome promotes renal inflammation and contributes to CKD. J Am Soc Nephrol. 2010;21(10):1732–1744. doi: 10.1681/ASN.2010020143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grebe A, Hoss F, Latz E. NLRP3 Inflammasome and the IL-1 Pathway in Atherosclerosis. Circ Res. 2018;122(12):1722–1740. doi: 10.1161/CIRCRESAHA.118.311362. [DOI] [PubMed] [Google Scholar]
- 11.Grant RW, Dixit VD. Mechanisms of disease: inflammasome activation and the development of type 2 diabetes. Front Immunol. 2013;4:50. doi: 10.3389/fimmu.2013.00050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ishii Y, Sawada T, Shimizu A, Tojimbara T, Nakajima I, Fuchinoue S, et al. An experimental sclerosing encapsulating peritonitis model in mice. Nephrol Dial Transplant. 2001;16(6):1262–1266. doi: 10.1093/ndt/16.6.1262. [DOI] [PubMed] [Google Scholar]
- 13.Kadoya H, Satoh M, Sasaki T, Taniguchi S, Takahashi M, Kashihara N. Excess aldosterone is a critical danger signal for inflammasome activation in the development of renal fibrosis in mice. FASEB J. 2015;29(9):3899–3910. doi: 10.1096/fj.15-271734. [DOI] [PubMed] [Google Scholar]
- 14.Hautem N, Morelle J, Sow A, Corbet C, Feron O, Goffin E, et al. The NLRP3 inflammasome has a critical role in peritoneal dialysis-related peritonitis. J Am Soc Nephrol. 2017;28(7):2038–2052. doi: 10.1681/ASN.2016070729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Williams JD, Craig KJ, Topley N, Von Ruhland C, Fallon M, Newman GR, et al. Morphologic changes in the peritoneal membrane of patients with renal disease. J Am Soc Nephrol. 2002;13(2):470–479. doi: 10.1681/ASN.V132470. [DOI] [PubMed] [Google Scholar]
- 16.Bellon T, Martinez V, Lucendo B, del Peso G, Castro MJ, Aroeira LS, et al. Alternative activation of macrophages in human peritoneum: implications for peritoneal fibrosis. Nephrol Dial Transplant. 2011;26(9):2995–3005. doi: 10.1093/ndt/gfq771. [DOI] [PubMed] [Google Scholar]
- 17.Sutherland TE, Shaw TN, Lennon R, Herrick SE, Ruckerl D. Ongoing exposure to peritoneal dialysis fluid alters resident peritoneal macrophage phenotype and activation propensity. Front Immunol. 2021;12:715209. doi: 10.3389/fimmu.2021.715209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li Q, Zheng M, Liu Y, Sun W, Shi J, Ni J, et al. A pathogenetic role for M1 macrophages in peritoneal dialysis-associated fibrosis. Mol Immunol. 2018;94:131–139. doi: 10.1016/j.molimm.2017.12.023. [DOI] [PubMed] [Google Scholar]
- 19.Liao CT, Andrews R, Wallace LE, Khan MW, Kift-Morgan A, Topley N, et al. Peritoneal macrophage heterogeneity is associated with different peritoneal dialysis outcomes. Kidney Int. 2017;91(5):1088–1103. doi: 10.1016/j.kint.2016.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kadoya H, Hirano A, Umeno R, Kajimoto E, Iwakura T, Kondo M, et al. Activation of the inflammasome drives peritoneal deterioration in a mouse model of peritoneal fibrosis. FASEB J. 2023;37(9):e23129. doi: 10.1096/fj.202201777RRR. [DOI] [PubMed] [Google Scholar]
- 21.McDonald B, Kubes P. Interactions between CD44 and Hyaluronan in Leukocyte Trafficking. Front Immunol. 2015;6:68. doi: 10.3389/fimmu.2015.00068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yamagata K, Tomida C, Koyama A. Intraperitoneal hyaluronan production in stable continuous ambulatory peritoneal dialysis patients. Perit Dial Int. 1999;19(2):131–137. doi: 10.1177/089686089901900210. [DOI] [PubMed] [Google Scholar]
- 23.Yamasaki K, Muto J, Taylor KR, Cogen AL, Audish D, Bertin J, et al. NLRP3/cryopyrin is necessary for interleukin-1beta (IL-1beta) release in response to hyaluronan, an endogenous trigger of inflammation in response to injury. J Biol Chem. 2009;284(19):12762–12771. doi: 10.1074/jbc.M806084200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tsai CC, Lee JJ, Liu TP, Ko WC, Wu CJ, Pan CF, et al. Effects of age and diabetes mellitus on clinical outcomes in patients with peritoneal dialysis-related peritonitis. Surg Infect (Larchmt) 2013;14(6):540–546. doi: 10.1089/sur.2012.195. [DOI] [PubMed] [Google Scholar]
- 25.Nishina M, Yanagi H, Kakuta T, Endoh M, Fukagawa M, Takagi A. A 10-year retrospective cohort study on the risk factors for peritoneal dialysis-related peritonitis: a single-center study at Tokai University Hospital. Clin Exp Nephrol. 2014;18(4):649–654. doi: 10.1007/s10157-013-0872-y. [DOI] [PubMed] [Google Scholar]
- 26.Ueda R, Nakao M, Maruyama Y, Nakashima A, Yamamoto I, Matsuo N, et al. Effect of diabetes on incidence of peritoneal dialysis-associated peritonitis. PLoS ONE. 2019;14(12):e0225316. doi: 10.1371/journal.pone.0225316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chow KM, Szeto CC, Leung CB, Kwan BC, Law MC, Li PK. A risk analysis of continuous ambulatory peritoneal dialysis-related peritonitis. Perit Dial Int. 2005;25(4):374–379. doi: 10.1177/089686080502500413. [DOI] [PubMed] [Google Scholar]
- 28.Oo TN, Roberts TL, Collins AJ. A comparison of peritonitis rates from the United States Renal Data System database: CAPD versus continuous cycling peritoneal dialysis patients. Am J Kidney Dis. 2005;45(2):372–380. doi: 10.1053/j.ajkd.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 29.Joshi N, Caputo GM, Weitekamp MR, Karchmer AW. Infections in patients with diabetes mellitus. N Engl J Med. 1999;341(25):1906–1912. doi: 10.1056/NEJM199912163412507. [DOI] [PubMed] [Google Scholar]
- 30.Schroder K, Zhou R, Tschopp J. The NLRP3 inflammasome: a sensor for metabolic danger? Science. 2010;327(5963):296–300. doi: 10.1126/science.1184003. [DOI] [PubMed] [Google Scholar]
- 31.Fang L, Xie D, Wu X, Cao H, Su W, Yang J. Involvement of endoplasmic reticulum stress in albuminuria induced inflammasome activation in renal proximal tubular cells. PLoS ONE. 2013;8(8):e72344. doi: 10.1371/journal.pone.0072344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Uchiyama K, Yanai A, Maeda K, Ono K, Honda K, Tsujimoto R, et al. Baseline and time-averaged values predicting residual renal function decline rate in Japanese peritoneal dialysis patients. Ther Apher Dial. 2017;21(6):599–605. doi: 10.1111/1744-9987.12589. [DOI] [PubMed] [Google Scholar]
- 33.Kang SH, Cho KH, Park JW, Yoon KW, Do JY. Proteinuria as a risk factor for decline in residual renal function in non-diabetic peritoneal dialysis patients. Kidney Blood Press Res. 2013;37(2–3):199–210. doi: 10.1159/000350145. [DOI] [PubMed] [Google Scholar]
- 34.Jansen MA, Hart AA, Korevaar JC, Dekker FW, Boeschoten EW, Krediet RT. Predictors of the rate of decline of residual renal function in incident dialysis patients. Kidney Int. 2002;62(3):1046–1053. doi: 10.1046/j.1523-1755.2002.00505.x. [DOI] [PubMed] [Google Scholar]
- 35.Whitty R, Bargman JM, Kiss A, Dresser L, Lui P. Residual kidney function and peritoneal dialysis-associated peritonitis treatment outcomes. Clin J Am Soc Nephrol. 2017;12(12):2016–2022. doi: 10.2215/CJN.00630117. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analyzed during the current study.