Abstract
Background
In recent years, the capacity of tumor cells to maintain high levels of glycolysis, even in the presence of oxygen, has emerged as one of the main metabolic traits and garnered considerable attention. The purpose of this meta-analysis is to investigate the prognostic value of glycolysis markers in liver cancer.
Methods
PubMed, Embase, and Cochrane Library databases were searched for articles on glycolytic marker expression levels associated with the prognosis of liver cancer until April 2023. Stata SE14.0 was used to calculate the aggregate hazard ratios and 95% confidence intervals.
Results
Thirty-five studies were included. The worse overall survival (OS) (P < 0.001), disease-free survival (DFS) (P = 0.001), recurrence-free survival (RFS) (P = 0.004), and time to recurrence (TTR) (P < 0.001) were significantly associated with elevated expression of glycolysis markers. Higher expression of PKM2 (P < 0.001), STMN1 (P = 0.002), MCT4 (P < 0.001), GLUT1 (P = 0.025), HK-2 (P < 0.001), and CA9 (P < 0.001) were significantly related to shorter OS. Increased levels of PKM2 (P < 0.001), CA9 (P = 0.005), and MCT4 (P < 0.001) were associated with worse DFS. Elevated PKM2 expression (P = 0.002) was also associated with poorer RFS in hepatocellular carcinoma patients. GLUT2 expression was not correlated with the prognosis of liver cancer (P = 0.134).
Conclusions
Elevated expression of glycolysis markers was associated with worse OS, DFS, RFS, and TTR in patients with liver cancer. Therefore, these glycolysis markers could serve as potential prognostic markers and therapeutic targets in liver cancer.
Trial registration
PROSPERO registration: CRD42023469645.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12957-023-03275-4.
Keywords: Hepatocellular Carcinoma, Glycolysis, Prognosis, Biomarkers, Meta-analysis
Introduction
Primary liver cancer, being one of the most prevalent malignancies worldwide, presents a substantial threat to human health [1]. According to statistical data, in the year 2012, there were approximately 780,000 newly diagnosed cases of liver cancer and 740,000 deaths attributed to this disease worldwide [2]. Hepatocellular carcinoma (HCC) is the fourth leading cause of cancer-related mortality worldwide, accounting for 80%-90% of primary liver malignancies [3, 4]. Despite the significant progress made in cancer treatment modalities, such as surgical techniques, targeted therapies, chemotherapy, and radiotherapy, the challenges of metastasis and recurrence continue to pose significant clinical challenges [5, 6]. Therefore, the identification of clinical markers that are associated with prognosis is paramount for establishing accurate diagnoses and designing individualized treatments for patients with liver cancer.
Accumulating evidence indicates that changes in cellular metabolism contribute to an increased propensity for tumor development. In cancer, a prominent hallmark involves reprogramming energy metabolism in tumor cells, which enables them to obtain the necessary energy for accelerated cellular proliferation, division, invasion, and migration [7]. One of the metabolic features of HCC cells is that glucose metabolism always terminates in pyruvate and bypasses oxidation via the Krebs cycle, which can convert pyruvate to lactate with sufficient oxygen [8]. This phenomenon, commonly referred to as "aerobic glycolysis" or the "Warburg effect," allows cells to increase glucose uptake and lactate production regardless of the presence of oxygen [9].
Numerous studies in recent years have demonstrated the effectiveness of reprogramming tumor metabolism as a new therapeutic approach to combat cancer [10]. Aerobic glycolysis is crucial for the initiation and progression of most malignancies. Therefore, inhibiting tumor cell glycolysis and interfering with the energy supply have become essential research areas in cancer treatment [11]. In vitro, in vivo, and clinical studies have reported the presence of a number of enzymes which are involved in the glycolytic pathways, including glucose transporter 1 (GLUT1), glucose transporter 2 (GLUT2), glucose transporter 4 (GLUT4), hexokinase 2 (HK- 2), monocarboxylate transporter 4 (MCT4), pyruvate kinase M2 (PKM2), stathmin 1 (STMN1), carbonic anhydrase IX (CA9), choline kinase alpha (CKA), MLX-interacting protein-like (MLXIPL), membrane-associated protein 17 (MAP17), Phosphofructokinase-2/fructose-2,6-bisphosphatase 3 (PFKFB3), phosphoglucose mutase 1 (PGM1), cyclin-dependent kinase 1 (CDK1), alanine-serine-cysteine transporter 2 (ASCT2), lactate dehydrogenase B (LDHB), homer protein homolog 1 (Homer1), tripartite motif inclusion 35 (TRIM35), phosphoglycerate kinase-1 (PGK-1), ATP-binding cassette subfamily B member 6 (ABCB6), and cyclin-dependent kinase 1 (CDC2). Among these key enzymes of glycolysis, the most widely used glycolytic markers include GLUT1, GLUT2, GLUT4, HK- 2, MCT4, PKM2, CA9, MLXIPL, PFKFB3, PGM1, CDK1, ASCT2, LDHB, PGK-1, CDC2. The glycolytic regulators STMN1, MAP17, Homer1, TRIM35, and ABCB6 are considered as potential biomarkers for the prognosis of hepatocellular carcinoma.
The GLUT family mediates glucose uptake, which transports glucose and related hexoses into the cells [12]. PKM2 is one of the major rate-limiting enzymes in glycolysis and has significant significance in the latter stages of the glycolytic pathway [13]. HK-2 catalyzes the first step of glycolysis. MLXIPL can be activated by carbohydrate metabolites, and transactivates glucose metabolism by regulating glycolysis during the circulation of sugars [14]. PFKFB3 is a metabolic enzyme that sustains glycolysis [15, 16].
Previous studies have shown that a risk signature consisting of six glycolysis-related genes can accurately predict the prognosis of HCC patients [17]. Despite the increasing number of studies on glycolysis markers, there is a need for a comprehensive review to summarize their prognostic value in liver cancer. Consequently, this meta-analysis aims to determine the relationship between glycolysis markers and the prognosis of patients with liver cancer.
Methods
This systematic review and meta-analysis was registered on the Prospective Registry for Systematic Reviews (PROSPERO, CRD42023469645) and conducted according to Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) [18, 19].
Literature Retrieval Strategy
We searched PubMed, Embase, and Cochrane Library online databases for studies published from the establishment of each database to April 2023 that evaluated glycolysis markers concerning survival outcomes in liver cancer. The search was restricted to articles published in the English language. The search keywords comprised: “hepatocellular carcinoma”, “HCC”, “glucose transporter 1”, “GLUT1”, “monocarboxylate transporter”, “MCT4”, “hexokinase 2”, “HK2”, “pyruvate kinase M2”, “PKM2”, “Enolase 1”, “ENO1”, “L-lactate dehydrogenase B chain”, “LDHB”, “lactate dehydrogenase 5”, “LDH5”, “carbonic anhydrase 9”, “CA9”, “dihydropyrimidinase-like 4”, “DPYSL4”, “Homer protein homolog 1”, “HOMER1”, “ATP-binding cassette subfamily B member 6”, “ABCB6”, “centromeric protein A”, “CENPA”, “cyclin-dependent kinase 1”, “CDK1”, “stathmin 1”, “STMN1”, “glucose transporters”, “prognosis”, “prognostic”, and “outcome”. After removing duplicates from all identified articles, those that did not meet the inclusion criteria based on title and abstract were excluded. Then, the full text was read and evaluated carefully to identify the included literature based on the inclusion and exclusion criteria. Any differences that arose were resolved through consensus.
Selection of Studies
The following inclusion criteria were established: (1) The diagnosis of liver cancer was based on established guidelines, such as histopathology or other relevant diagnostic criteria. (2) The study investigated the relationship between the expression levels of glycolysis markers and survival outcomes in patients with liver cancer. (3) The study was a cohort study in which patients were divided into high and low expression groups based on the expression levels of glycolytic markers. (4) The study documented the survival outcomes of HCC patients, including OS, DFS, RFS, and TTR. (5) The study presented HR and 95% CI or provided sufficient data for calculating the HR and 95% CI.
Exclusion criteria were as follows: (1) Case reports, systematic reviews, meta-analyses, letters, or conference presentations. (2) Patients included in the study with other malignancies. (3) Publications written in languages other than English. (4) Studies utilized duplicate data or analyses. (5) Studies that did not present available data. (6) The studies with a sample size of less than 20.
Data Extraction Process
Two researchers independently extracted pertinent data from eligible studies. The extracted data for each study included the first author, publication year, population source, sample size, gender distribution, age range, glycolysis markers, detection method, duration of follow-up, and survival outcomes. OS, DFS, RFS, and TTR were the recorded survival outcomes. In instances where the original data or corresponding HR was not provided, the Engauge Digitizer v4.1 was used to extract the necessary information from the Kaplan-Meier survival curve, allowing the calculation of HR and its corresponding 95% CI [20].
Quality Assessment of Studies
The quality of all the included studies was evaluated using the Newcastle-Ottawa Scale (NOS) [21]. The NOS scale assessed the quality of each study across three domains: selection (0–4 points), comparability (0–2 points), and exposure (0–3 points). Studies with an NOS score greater than 7 were classified as high quality, while those with a score between 5 and 7 were classified as medium quality. Studies scoring below 5 were deemed to be of poor quality [22].
Statistical Analysis
All statistical analyses and graphical representations were performed using STATA 16.0. The association between the expression levels of glycolysis markers and OS, DFS, RFS, and TTR in patients with liver cancer was evaluated by pooled HRs and corresponding 95% CIs. The pooled HRs and corresponding 95% CIs were calculated using the random-effects model [23]. The heterogeneity among studies was assessed using the Cochran Q test and the I2 statistic [24]. An I2 value ≤ 25% indicated low heterogeneity, 25% < I2 < 50% showed moderate heterogeneity, and I2 ≥ 50% indicated high heterogeneity [24]. Subgroup analyses were conducted based on glycolysis markers and study regions. The robustness of this meta-analysis was evaluated by sequentially excluding individual studies and assessing their impact on the pooled results. Publication bias was evaluated using Begg's test and Egger's test. All statistical tests were two-tailed, and a significance level of P < 0.05 was considered statistically significant.
Results
Search Results
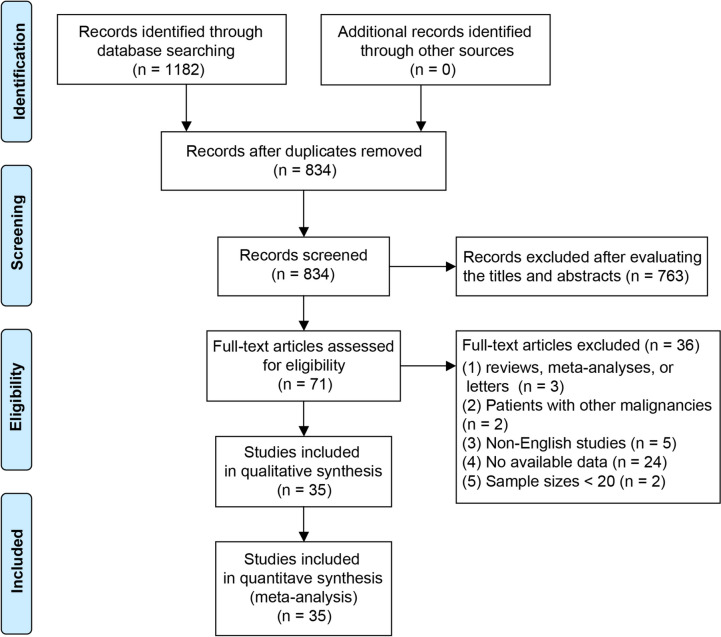
Figure 1 presents the results of the literature search and screening procedure. Initial identification yielded a total of 1182 studies. After removing duplicates, 834 investigations remained. Following a review of the titles and abstracts, 763 studies were determined to be irrelevant to the topic and were therefore excluded. The remaining 71 studies were subsequently subjected to thoroughly examining the full text. In the end, a total of 35 studies satisfied the inclusion criteria for this meta-analysis [25–59].
Fig. 1.
Flow diagram for selection strategy of articles in this meta-analysis
Characteristics and Quality of the Included Studies
We included 35 eligible studies with a total of 5234 patients. All studies were published between 2000 and 2023, covering seven regions. A total of 22 investigations were conducted in China, 6 in Japan, 2 in Germany, 1 in South Korea, 1 in the United States, 3 in Taiwan, and 1 in Hong Kong. The sample sizes ranged from 30 to 638 individuals. In 34 investigations, tumor samples were utilized, while serum samples were utilized in only two. To measure the expression levels of glycolysis markers, 29 studies used the immunohistochemistry method, whereas 4 studies used qRT-PCR, 1 used the immunofluorescence method, and 1 used the ELISA. Glycolysis markers assessed in these studies included: MLXIPL (n = 1), GLUT4 (n = 1), PKM2 (n = 9), MAP17 (n = 1), PFKFB3 (n = 1), STMN1 (n = 3), PGM1 (n = 1), MCT4 (n = 3), GLUT1 (n = 2), CDK1 (n = 1), HK-2 (n = 4), CA9 (n = 4), Homer1 (n = 1), ASCT2 (n = 1), LDHB (n = 1), TRIM35 (n = 1), ABCB6 (n = 1), PGK-1 (n = 1), GLUT2 (n = 2), CDC2 (n = 1). The prognostic value of glycolysis markers was assessed by examining OS in 32 studies, DFS in 14 studies, RFS in 3 studies, and TTR in 3 studies. Supplementary Table 1 presented the characteristics of all eligible studies, including publication region, year, sample size, gender, age, and other relevant details.
The NOS score for the 10 studies exceeded 7, while the NOS score for the 25 studies ranged from 5 to 7.
Correlation between Glycolysis Markers and OS in Liver Cancer
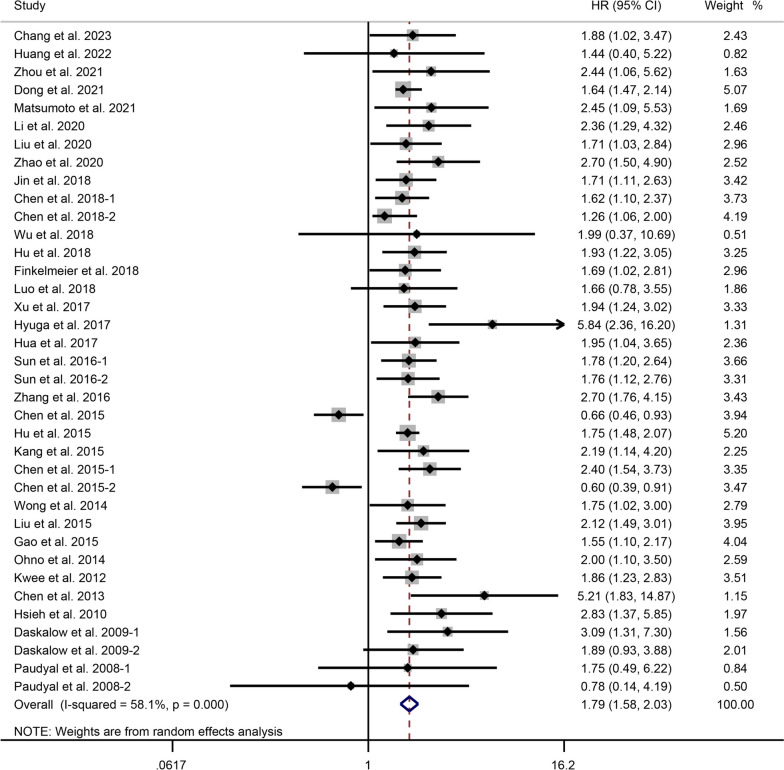
In 32 studies involving 19 glycolysis markers, the association between the expression levels and OS in patients with liver cancer was investigated. The meta-analysis, using a random-effects model (I2 = 57.0%, P < 0.001), revealed that elevated expression of glycolysis markers was significantly associated with worse OS in patients with liver cancer (HR = 1.78, 95% CI: 1.58-2.01, P < 0.001) (Fig. 2).
Fig. 2.
Forest plot showing the correlation between the expression levels of glycolysis markers and OS in patients with liver cancer. A random-effects model was employed. [25–39, 41–58]
Subgroup analysis based on specific glycolysis markers revealed that higher expression of PKM2 (P < 0.001), STMN1 (P = 0.002), MCT4 (P < 0.001), GLUT1 (P = 0.025), HK-2 (P < 0.001), and CA9 (P < 0.001) was significantly correlated with poor OS in liver cancer. However, elevated GLUT2 expression was not significantly associated with OS in patients with liver cancer (P = 0.134). The regional subgroup analysis suggested that high expression levels of glycolytic markers were associated with poorer OS in HCC patients from China (P < 0.001), Japan (P = 0.001), Germany (P < 0.001), and Taiwan (P < 0.001). Subgroup analysis of samples showed that elevated expression of glycolytic markers in tumor tissues (P < 0.001) and serum samples (P = 0.001) was associated with poor prognosis. In the assay-based subgroup analysis, high expression levels of glycolytic markers detected by IHC (P < 0.001) and qRT-PCR (P < 0.001) were associated with poorer OS in HCC patients. In addition, heterogeneity between studies could be attributable to specific glycolysis markers (Table 1). The results revealed that regions, samples, and assays were not the predominant source of heterogeneity (Table 1).
Table 1.
Subgroup analysis of the correlation between the expression levels of glycolysis markers and OS according to the specific glycolysis markers, region, sample, and detection method
| Subgroup | HR (95% CI) | Heterogeneity I2 (%), P |
|---|---|---|
| Indicators: | ||
| MLXIPL | 1.88 (1.02, 3.47) | NA |
| GLUT4 | 1.44 (0.40, 5.20) | NA |
| PKM2 | 1.93 (1.70, 2.18) | I2 = 0.0%, P = 0.704 |
| MAP17 | 1.64 (1.36, 1.98) | NA |
| PFKFB3 | 2.45 (1.09, 5.52) | NA |
| STMN1 | 2.57 (1.43, 4.65) | I2 = 49.6%, P = 0.138 |
| PGM1 | 1.71 (1.11, 2.63) | NA |
| MCT4 | 1.64 (1.30, 2.07) | I2 = 0.0%, P = 0.755 |
| GLUT1 | 1.47 (1.05, 2.05) | I2 = 44.1%, P = 0.181 |
| CDK1 | 1.99 (0.37, 10.70) | NA |
| HK-2 | 2.12 (1.66, 2.71) | I2 = 0.0%, P = 0.604 |
| CA9 | 2.26 (1.47, 3.47) | I2 = 41.1%, P = 0.165 |
| Homer1 | 1.66 (0.78, 3.54) | NA |
| ASCT2 | 1.76 (1.12, 2.76) | NA |
| LDHB | 0.66 (0.46, 0.93) | NA |
| TRIM35 | 0.60 (0.39, 0.92) | NA |
| PGK-1 | 3.09 (1.31, 7.29) | NA |
| GLUT2 | 1.65 (0.86, 3.20) | I2 = 0.0%, P = 0.347 |
| Region: | ||
| China | 1.66 (1.43, 1.94) | I2 = 67.4%, P < 0.001 |
| Japan | 2.37 (1.44, 3.88) | I2 = 28.1%, P = 0.234 |
| Germany | 1.95 (1.34, 2.83) | I2 = 0.0%, P = 0.493 |
| Taiwan | 2.70 (1.64, 4.45) | I2 = 21.5%, P = 0.280 |
| South Korea | 2.19 (1.14, 4.20) | NA |
| Hong Kong | 1.75 (1.02, 3.00) | NA |
| US | 1.86 (1.23, 2.82) | NA |
| Sample: | ||
| Tissue | 1.80 (1.57, 2.05) | I2 = 60.3%, P < 0.001 |
| Serum | 1.82 (1.29, 2.56) | I2 = 0.0%, P = 0.704 |
| Detection method: | ||
| IHC | 1.80 (1.56, 2.07) | I2 = 63.4%, P < 0.001 |
| qRT-PCR | 1.80 (1.30, 2.50) | I2 = 0.0%, P = 0.885 |
| IF | 2.45 (1.09, 5.52) | NA |
| ELISA | 1.69 (1.02, 2.81) | NA |
MLXIPL MLX interacting protein like, GLUT4 glucose transporter 4, PKM2 pyruvate kinase M2, MAP17 membrane-associated protein 17, PFKFB3 phosphofructokinase-2/fructose-2,6-bisphosphatase 3, STMN1 stathmin 1, PGM1 phosphoglucomutase 1, MCT4 monocarboxylic acid transporter 4, GLUT1 glucose transporter 1, CDK1 cyclin dependent kinase 1, HK-2 hexokinase 2, CA9 carbonic anhydrase IX, ASCT2, alanine-serine-cysteine transporter 2, LDHB lactate dehydrogenase B, TRIM35, tripartite motif-containing 35, PGK-1 phosphoglycerate kinase-1, GLUT2 glucose transporter 2, HR hazard ratio, IHC immunohistochemistry, qRT-PCR quantitative real time polymerase chain reaction, IF immunofluorescence, ELISA enzyme linked immunosorbent assay
Correlation between Glycolysis Markers and DFS in Liver Cancer
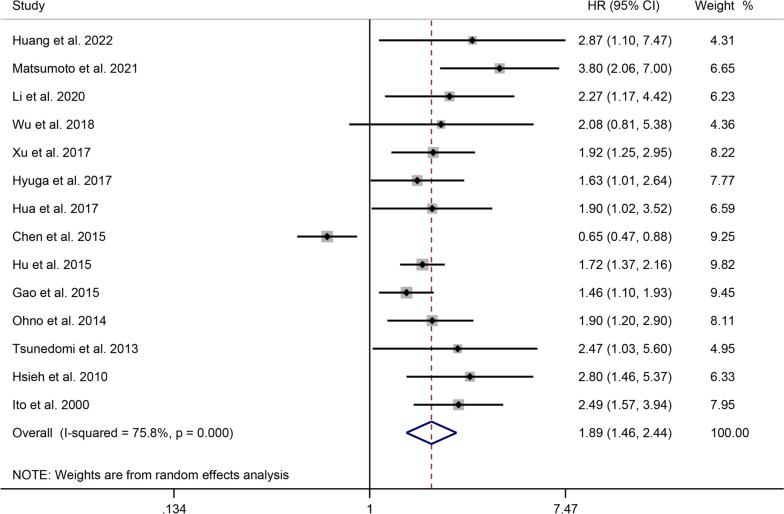
The correlation between glycolysis markers and DFS in HCC patients was investigated in 14 studies, including 1421 patients. High heterogeneity was observed among the studies (I2 = 75.8%, P < 0.001). The pooled HR was 1.89 (95% CI: 1.17-1.81, P = 0.001), indicating that liver cancer patients with elevated expression of glycolysis markers had a shorter DFS (Fig. 3).
Fig. 3.
Forest plot showing the correlation between the expression levels of glycolysis markers and DFS in patients with liver cancer. A random-effects model was employed
High expression of PKM2 (P < 0.001), CA9 (P = 0.005), and MCT4 (P < 0.001) predicted a poor DFS in patients with liver cancer, as determined by subgroup analysis based on specific glycolysis markers. The regional subgroup analysis indicated that high expression levels of glycolytic markers correlated with poorer DFS in China (P = 0.019), Japan (P < 0.001), and Taiwan (P < 0.001). The results of subgroup analysis based on detection methods suggested that high expression levels of glycolytic markers detected using IHC (P < 0.001) and qRT-PCR (P = 0.003) were associated with poor DFS. Furthermore, the heterogeneity between studies can be attributed to changes in glycolytic markers, rather than the study regions or detection methods (Supplementary Table 2).
Correlation between Glycolysis Markers and RFS in Liver Cancer
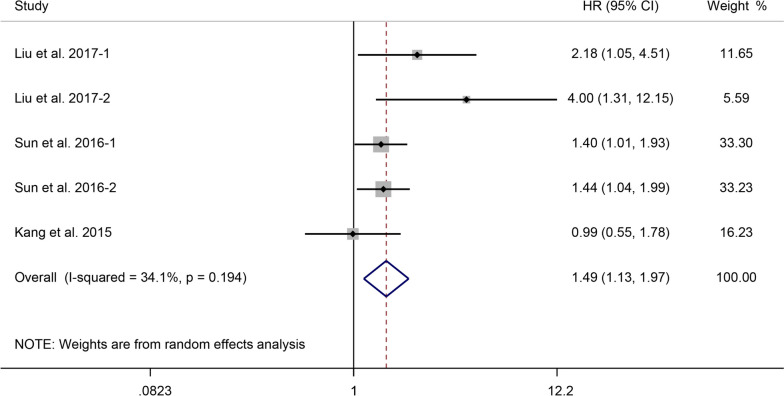
We analyzed data from three studies, including 636 patients, to investigate the correlation between PKM2, GLUT1, ASCT2, and CA9 expression levels and RFS in patients with liver cancer. The pooled results demonstrated moderate heterogeneity (I2 = 34.1%, P = 0.194), and elevated expression levels of these four glycolysis markers were significantly associated with a shorter RFS (HR = 1.49, 95% CI: 1.13-1.97, P = 0.004) (Fig. 4).
Fig. 4.
Forest plot showing the correlation between the expression levels of glycolysis markers and RFS in patients with liver cancer. A random-effects model was employed
A subgroup analysis based on various glycolysis markers revealed that overexpression of PKM2 (P = 0.002) indicated a poor RFS (Supplementary Table 3).
Correlation between Glycolysis Markers and TTR in Liver Cancer
Using data from three studies, we examined the relationship between the expression levels of PGM1, MCT4, GLUT1, and PKM2 and TTR in HCC patients. The pooled results, with low heterogeneity (I2 = 0.0%, P = 0.814), revealed that the high expression of these four glycolysis markers in liver cancer was associated with a higher TTR rate (HR = 1.48, 95% CI: 1.25-1.75, P < 0.001) (Supplementary Figure 1). However, subgroup analyses could not be conducted due to the limited number of studies reporting on TTR.
Sensitivity Analysis
The results of sensitivity analysis showed that our results were robust (Supplementary figure 2, and Supplementary figure 3).
Publication Bias
Begg's and Egger's tests were employed to evaluate publication bias in this meta-analysis. OS (P = 0.059 and P = 0.105, respectively), DFS (P = 0.189 and P = 0.065, respectively), RFS (P = 0.221 and P = 0.307, respectively), and TTR (P = 0.734 and P = 0.070, respectively) showed no significant publication bias.
Discussion
HCC is a global disease with significant consequences. Early detection is crucial for effective HCC management because it not only improves patient prognosis but also preserves valuable societal resources [60]. The rewiring of energy metabolism is a defining feature of cancer, with aerobic glycolysis playing a crucial role in promoting cancer cell proliferation, invasion, and migration [7, 61]. Various tumor types have been observed to exhibit dysregulation of glucose metabolism, most notably through aerobic glycolysis. This meta-analysis examined the relationship between glycolysis markers and survival outcomes in HCC patients.
Within the field of oncology, significant attention has been dedicated to studying metabolic changes in cancer. Following our inclusion criteria, we identified 36 studies examining the effect of glycolytic marker levels on the prognosis of HCC patients. Our findings demonstrated that increased expression of glycolytic markers was associated with decreased OS, DFS, RFS, and TTR in HCC patients. These results are consistent with the findings of the majority of the studies included in our analysis. In addition, subgroup analysis of distinct glycolysis markers revealed a relationship between PKM2, STMN1, MCT4, GLUT1, HK-2, CA9, and GLUT2 and the clinical outcome of HCC patients.
PKM2, a crucial rate-limiting enzyme in glycolysis, is highly active in the latter stages of the glycolytic pathway [13]. It is predominantly expressed in differentiated tissues, such as adipose tissue, lung tissue, and retinal tissue, as well as in cells with high rates of nucleic acid synthesis, such as proliferating cells, embryonic cells, and tumor cells [62, 63]. The concentration of pyruvate directly influences lactate production. PKM2 serves a vital role in tumorigenesis by catalyzing the conversion of phosphoenolpyruvate to pyruvate and releasing energy [64]. Numerous studies have reported that overexpression of PKM2 is correlated with an unfavorable prognosis and chemotherapy resistance in various tumor types [27]. Consistent with previous findings, increased PKM2 expression in HCC patients was associated with decreased OS, DFS, and RFS. In addition, PKM2-induced phosphorylation of histone H3 in HCC promotes the transcription of programmed death-ligand 1 (PD-L1) via epidermal growth factor (EGF). This leads to immunosuppression and tumor development within the HCC tumor microenvironment [65].
STMN1 is essential for regulating microtubule motility and is implicated in cancer cell division and proliferation [66]. Published studies have consistently reported that elevated STMN1 expression is associated with poorer survival in various cancers, including head and neck squamous cell carcinoma, gallbladder carcinoma, esophageal squamous cell carcinoma, breast cancer, and endometrial carcinoma. In addition, Zhang et al. demonstrated that eight glycolysis-related genes, namely AURKA (aurora kinase A), CDK1, CENPA, DEPDC1 (DEP domain containing 1), HMMR (hyaluronan-mediated motility receptor), KIF20A (kinesin family member 20A), PFKFB4 (6-Phosphofructo-2-Kinase/Fructose-2,6-Biphosphatase 4), and STMN1, are correlated with both OS and DFS in patients with HCC, which is consistent with our findings [67].
Lactic acid has been identified as a major energy source in cancer [68]. MCT4 is responsible for transporting pyruvate, lactate, and ketones as a monocarboxylate transporter [69]. It exports monocarboxylates accompanied by protons [70]. MCT4 is frequently upregulated in various malignancies, and its increased expression correlates with a poor prognosis. In liver cancer, abnormal MCT4 expression has been associated with early recurrence and a poor prognosis after radical resection [38]. This meta-analysis supports previous research findings, indicating that MCT4 can serve as both a therapeutic target and a prognostic marker for hepatocellular carcinoma [48].
The GLUT family, which consists of 14 members, plays a crucial role in the uptake of glucose and facilitates the transportation of glucose and related hexoses into cells [12]. Glucose is the primary energy source for cells and satisfies the elevated energy requirements of cancer cells involved in various biochemical processes [71, 72]. Multiple varieties of cancer have been linked to an upregulation of the glucose transporter GLUT1, which has a high affinity for glucose [73]. Amann et al. demonstrated that GLUT1 is essential for the proliferation and migration of HCC cells [74]. Consistent with previous research, our findings indicate that elevated GLUT1 expression is associated with decreased overall survival in liver cancer patients and can serve as a prognostic indicator for the disease [44]. In contrast to GLUT1, GLUT2 has a comparatively low affinity for glucose, mannose, galactose, and fructose, but a high affinity for glucosamine [75, 76]. Two investigations conducted in 2017 and 2022 demonstrated that GLUT2 is not only a negative prognostic factor in HCC but also a diagnostic imaging target for the disease [57, 77]. However, our meta-analysis revealed no correlation between the expression levels of GLUT2 and the overall survival of patients with HCC. This observation could be attributed to the limited number of studies and sample sizes in the analysis.
HK-2, the rate-limiting enzyme in the first stage of glycolysis, is essential for converting glucose to glucose-6-phosphate [78]. Overexpression of HK-2 frequently occurs in various tumors, resulting in enhanced glucose metabolism, resistance to cell apoptosis, and tumor-invading capacity. The regulatory function of HK-2 in cancer cells is complex. HK-2 overexpression initially increases glycolytic flux. HK-2 also translocates to the mitochondrial outer membrane, binds to the voltage-dependent anion channel (VDAC) porin, and inhibits apoptosis by preventing the formation of the mitochondrial permeability transition pore [79, 80]. Given HK-2's dual function in cancer cells, it is an attractive target for anticancer therapies. According to a study by Kwee et al. [55], HK-2 expression has biological and prognostic significance in HCC and may serve as an independent predictor of HCC survival. Our results also corroborate this theory, demonstrating that elevated levels of HK-2 expression are linked to reduced overall survival in HCC patients.
This meta-analysis demonstrated that elevated CA9 expression was associated with OS and DFS in HCC patients. A transmembrane protein, CA9, with an extracellular catalytic domain, CA9, is regulated by HIF-1 and plays a role in pH regulation under hypoxic conditions, such as hypoxia, acidosis, and oncogenic alterations [37]. As an adaptive response to hypoxia, the upregulation of CA9 in tumors significantly contributes to the malignant transformation of cancer and precancerous lesions [81, 82]. Hyuga et al. observed that CA9 is a crucial predictor of a poor prognosis after radical resection of liver cancer and can enhance the malignant potential of HCC cells by regulating epithelial-mesenchymal transition [41]. Genetic variation in the 3' untranslated region (3'UTR) of CA9 regulates the expression of CA9 and the progression of cancer, and serves as a novel determinant and target for HCC metastasis and prognosis, according to a study conducted in Taiwan [42].
With the development of cancer research, the metabolic reprogramming of tumors is now recognized as a promising therapeutic target, leading to significant advances in anticancer treatment. In this meta-analysis, we evaluated the effect of alterations in glycolysis markers expression on the prognosis of patients with liver cancer. The results indicated that glycolysis markers, including PKM2, STMN1, MCT4, GLUT1, HK-2, CA9, and GLUT2, can serve as potential prognostic biomarkers and therapeutic targets for liver cancer. Future research should investigate the role of glycolysis markers in the differentiation, migration, invasion, and stemness of tumor cells. These findings have significant implications for the development of novel prognostic biomarkers and the advancement of adjuvant therapies for liver cancer.
Limitations
First, we found significant heterogeneity among studies related to OS and DFS. Despite employing random-effects models for analysis and performing subgroup analysis to investigate the sources of heterogeneity, these effects could not be completely eliminated or explained. Significant heterogeneity suggested that study results need to be treated with caution. In addition, due to the lack of standardized cutoff values for various glycolysis markers, different studies included in our analysis might have used different cutoff values, which might have a potential impact on our results. Furthermore, the majority of the patient data included in this study originated from research conducted on Asian populations. This introduces the possibility of group selection bias and limits the applicability of the conclusions to other populations. Additionally, the data selected for the meta-analysis could be subject to potential publication bias. Although neither Begg's test nor Egger's test showed significant publication bias, the majority of the studies we included reported positive results. Finally, the included studies lacked crucial information regarding survival outcomes. Even though we estimated HR and their corresponding 95% CIs by extracting data from Kaplan-Meier survival curves, it was vital to note that these calculated values were inherently less precise than those directly provided by the original studies.
Conclusions
This meta-analysis demonstrated that the high expression of glycolysis markers was strongly associated with decreased OS, DFS, RFS, and TTR in liver cancer patients. Higher expression levels of PKM2, STMN1, MCT4, GLUT1, HK-2, and CA9 were significantly associated with reduced OS, as determined by subgroup analysis based on specific glycolysis markers. Patients with high expression levels of PKM2, CA9, and MCT4 were predicted to have a poorer DFS. Furthermore, elevated PKM2 expression was associated with reduced RFS in patients with liver cancer.
Supplementary Information
Additional file 1: Supplementary figure 1. Forest plot showing the correlation between the expression levels of glycolysis markers and TTR in patients with liver cancer. A random-effects model was employed.
Additional file 2: Supplementary figure 2. Sensitivity analysis between the expression levels of glycolysis markers and OS.
Additional file 3: Supplementary figure 3. Sensitivity analysis between the expression levels of glycolysis markers and DFS (A), RFS (B) and TTR (C).
Additional file 4: Supplementary Table 1. Overview and characteristics of the eligible studies.
Additional file 5: Supplementary Table 2. Subgroup analysis of the correlation between the expression levels of glycolysis markers and DFS according to the specific glycolysis markers, region, and detection method.
Additional file 6: Supplementary Table 3. Subgroup analysis of the correlation between the expression levels of glycolysis markers and RFS according to the specific glycolysis markers.
Acknowledgements
None.
Abbreviations
- OS
overall survival
- DFS
disease-free survival
- RFS
recurrence-free survival
- TTR
time to recurrence
- HR
hazard ratio
- CI
confidence interval
- HCC
hepatocellular carcinoma
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-analyses
- ENO1
Enolase 1
- LDH5
lactate dehydrogenase 5
- DPYSL4
dihydropyrimidinase-like 4
- CENPA
centromeric protein A
- MLXIPL
MLX interacting protein like
- GLUT4
glucose transporter 4
- PKM2
pyruvate kinase M2
- MAP17
membrane-associated protein 17
- PFKFB3
phosphofructokinase-2/fructose-2,6-bisphosphatase 3
- STMN1
stathmin 1
- PGM1
phosphoglucomutase 1
- MCT4
monocarboxylic acid transporter 4
- GLUT1
glucose transporter 1
- CDK1
cyclin dependent kinase 1
- HK-2
hexokinase 2
- CA9
carbonic anhydrase IX
- ASCT2
alanine-serine-cysteine transporter 2
- LDHB
lactate dehydrogenase B
- TRIM35
tripartite motif-containing 35
- CKA
choline kinase alpha
- PGK-1
phosphoglycerate kinase-1
- GLUT2
glucose transporter 2
- ABCB6
ATP-binding cassette subfamily B member 6
- CDC2
cyclin-dependent kinase 1
- Homer1
Homer protein homolog 1
- NOS
Newcastle-Ottawa Scale
- IHC
immunohistochemistry
- qRT-PCR
quantitative real time polymerase chain reaction
- IF
immunofluorescence
- ELISA
enzyme linked immunosorbent assay
- PD-L1
programmed death-ligand 1
- EGF
epidermal growth factor
- AURKA
aurora kinase A
- DEPDC1
DEP domain containing 1
- HMMR
hyaluronan-mediated motility receptor
- KIF20A
kinesin family member 20A
- PFKFB4
6-Phosphofructo-2-Kinase/Fructose-2,6-Biphosphatase 4
- VDAC
voltage-dependent anion channel
- 3'UTR
3' untranslated region
Authors’ contributions
WBQ and PR conceived of the study and participated in its design. WBQ and PR conducted the systematic literature review. WBQ and PR performed data analyses. S.S. drafted the article. WBQ and PR critically revised the article. All authors have read and approved the final version of the article. All authors have read and approved the final manuscript.
Funding
This paper is supported by the Basic and Applied Basic Research Foundation of Guangdong Province (Grant No. 2021B1515140062) and the Basic and Applied Basic Research Foundation of Guangdong Province (Grant No. 201950715024926).
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Ethical approval was not needed because this is a meta-analysis.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Valery PC, Laversanne M, Clark PJ, Petrick JL, McGlynn KA, Bray F. Projections of primary liver cancer to 2030 in 30 countries worldwide. Hepatology. 2018;67:600–611. doi: 10.1002/hep.29498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics. CA Cancer J Clin. 2012;65(2015):87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 3.Kim HS, El-Serag HB. The Epidemiology of Hepatocellular Carcinoma in the USA. Curr Gastroenterol Rep. 2019;21:17. doi: 10.1007/s11894-019-0681-x. [DOI] [PubMed] [Google Scholar]
- 4.Sohn W, Lee HW, Lee S, Lim JH, Lee MW, Park CH, Yoon SK. Obesity and the risk of primary liver cancer: A systematic review and meta-analysis. Clin Mol Hepatol. 2021;27:157–174. doi: 10.3350/cmh.2020.0176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.L. European Association For The Study Of The, R. European Organisation For, C. Treatment Of EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012;56:908–943. doi: 10.1016/j.jhep.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 6.Wu H, Pan L, Gao C, Xu H, Li Y, Zhang L, et al. Quercetin Inhibits the Proliferation of Glycolysis-Addicted HCC Cells by Reducing Hexokinase 2 and Akt-mTOR Pathway. Molecules. 2019;24:1993. [DOI] [PMC free article] [PubMed]
- 7.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 8.Iansante V, Choy PM, Fung SW, Liu Y, Chai JG, Dyson J, Del Rio A, D'Santos C, Williams R, Chokshi S, Anders RA, Bubici C, Papa S. PARP14 promotes the Warburg effect in hepatocellular carcinoma by inhibiting JNK1-dependent PKM2 phosphorylation and activation. Nat Commun. 2015;6:7882. doi: 10.1038/ncomms8882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hsu PP, Sabatini DM. Cancer cell metabolism: Warburg and beyond. Cell. 2008;134:703–707. doi: 10.1016/j.cell.2008.08.021. [DOI] [PubMed] [Google Scholar]
- 10.Byun JK, Choi YK, Kang YN, Jang BK, Kang KJ, Jeon YH, Lee HW, Jeon JH, Koo SH, Jeong WI, Harris RA, Lee IK, Park KG. Retinoic acid-related orphan receptor alpha reprograms glucose metabolism in glutamine-deficient hepatoma cells. Hepatology. 2015;61:953–964. doi: 10.1002/hep.27577. [DOI] [PubMed] [Google Scholar]
- 11.Zhao Y, Butler EB, Tan M. Targeting cellular metabolism to improve cancer therapeutics. Cell Death Dis. 2013;4:e532. doi: 10.1038/cddis.2013.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Avril N, Menzel M, Dose J, Schelling M, Weber W, Janicke F, Nathrath W, Schwaiger M. Glucose metabolism of breast cancer assessed by 18F-FDG PET: histologic and immunohistochemical tissue analysis. J Nucl Med. 2001;42:9–16. [PubMed] [Google Scholar]
- 13.Yu M, Chen S, Hong W, Gu Y, Huang B, Lin Y, Zhou Y, Jin H, Deng Y, Tu L, Hou B, Jian Z. Prognostic role of glycolysis for cancer outcome: evidence from 86 studies. J Cancer Res Clin Oncol. 2019;145:967–999. doi: 10.1007/s00432-019-02847-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Iizuka K, Bruick RK, Liang G, Horton JD, Uyeda K. Deficiency of carbohydrate response element-binding protein (ChREBP) reduces lipogenesis as well as glycolysis. Proc Natl Acad Sci U S A. 2004;101:7281–7286. doi: 10.1073/pnas.0401516101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cao Y, Zhang X, Wang L, Yang Q, Ma Q, Xu J, Wang J, Kovacs L, Ayon RJ, Liu Z, Zhang M, Zhou Y, Zeng X, Xu Y, Wang Y, Fulton DJ, Weintraub NL, Lucas R, Dong Z, Yuan JX, Sullivan JC, Meadows L, Barman SA, Wu C, Quan J, Hong M, Su Y, Huo Y. PFKFB3-mediated endothelial glycolysis promotes pulmonary hypertension. Proc Natl Acad Sci U S A. 2019;116:13394–13403. doi: 10.1073/pnas.1821401116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rider MH, Bertrand L, Vertommen D, Michels PA, Rousseau GG, Hue L. 6-phosphofructo-2-kinase/fructose-2,6-bisphosphatase: head-to-head with a bifunctional enzyme that controls glycolysis. Biochem J. 2004;381:561–579. doi: 10.1042/BJ20040752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jiang L, Zhao L, Bi J, Guan Q, Qi A, Wei Q, He M, Wei M, Zhao L. Glycolysis gene expression profilings screen for prognostic risk signature of hepatocellular carcinoma. Aging (Albany NY). 2019;11:10861–10882. doi: 10.18632/aging.102489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moher D, Liberati A, Tetzlaff J, Altman DG, Prisma Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 19.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, Prisma-P Group Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16. doi: 10.1186/1745-6215-8-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 22.Han CL, Meng GX, Ding ZN, Dong ZR, Chen ZQ, Hong JG, Yan LJ, Liu H, Tian BW, Yang LS, Xue JS, Li T. The Predictive Potential of the Baseline C-Reactive Protein Levels for the Efficiency of Immune Checkpoint Inhibitors in Cancer Patients: A Systematic Review and Meta-Analysis. Front Immunol. 2022;13:827788. doi: 10.3389/fimmu.2022.827788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Abdelmalak J, Tan N, Con D, Eslick G, Majeed A, Kemp W, et al. The Effect of Aspirin Use on Incident Hepatocellular Carcinoma-An Updated Systematic Review and Meta-Analysis. Cancers (Basel). 2023;15:3518. [DOI] [PMC free article] [PubMed]
- 24.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chang X, Tian C, Jia Y, Cai Y, Yan P. MLXIPL promotes the migration, invasion, and glycolysis of hepatocellular carcinoma cells by phosphorylation of mTOR. BMC Cancer. 2023;23:176. doi: 10.1186/s12885-023-10652-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huang Y, Xian L, Liu Z, Wei L, Qin L, Xiong Y, Hu L, Zhou S, Fu Q, Li B, Qin Y. AMPKalpha2/HNF4A/BORIS/GLUT4 pathway promotes hepatocellular carcinoma cell invasion and metastasis in low glucose microenviroment. Biochem Pharmacol. 2022;203:115198. doi: 10.1016/j.bcp.2022.115198. [DOI] [PubMed] [Google Scholar]
- 27.Zhou B, Lu D, Wang A, Cui J, Zhang L, Li J, Fan L, Wei W, Liu J, Sun G. Endoplasmic reticulum stress promotes sorafenib resistance via miR-188-5p/hnRNPA2B1-mediated upregulation of PKM2 in hepatocellular carcinoma. Mol Ther Nucleic Acids. 2021;26:1051–1065. doi: 10.1016/j.omtn.2021.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Matsumoto K, Noda T, Kobayashi S, Sakano Y, Yokota Y, Iwagami Y, Yamada D, Tomimaru Y, Akita H, Gotoh K, Takeda Y, Tanemura M, Umeshita K, Doki Y, Eguchi H. Inhibition of glycolytic activator PFKFB3 suppresses tumor growth and induces tumor vessel normalization in hepatocellular carcinoma. Cancer Lett. 2021;500:29–40. doi: 10.1016/j.canlet.2020.12.011. [DOI] [PubMed] [Google Scholar]
- 29.Dong F, Li R, Wang J, Zhang Y, Yao J, Jiang SH, Hu X, Feng M, Bao Z. Hypoxia-dependent expression of MAP17 coordinates the Warburg effect to tumor growth in hepatocellular carcinoma. J Exp Clin Cancer Res. 2021;40:121. doi: 10.1186/s13046-021-01927-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhao R, Li L, Yang J, Niu Q, Wang H, Qin X, Zhu N, Shi A. Overexpression of Pyruvate Kinase M2 in Tumor Tissues Is Associated with Poor Prognosis in Patients with Hepatocellular Carcinoma. Pathol Oncol Res. 2020;26:853–860. doi: 10.1007/s12253-019-00630-3. [DOI] [PubMed] [Google Scholar]
- 31.Liu YP, Pan LL, Kong CC. Stathmin 1 promotes the progression of liver cancer through interacting with YAP1. Eur Rev Med Pharmacol Sci. 2020;24:7335–7344. doi: 10.26355/eurrev_202007_21900. [DOI] [PubMed] [Google Scholar]
- 32.Li TE, Wang S, Shen XT, Zhang Z, Chen M, Wang H, Zhu Y, Xu D, Hu BY, Wei R, Zheng Y, Dong QZ, Qin LX. PKM2 Drives Hepatocellular Carcinoma Progression by Inducing Immunosuppressive Microenvironment. Front Immunol. 2020;11:589997. doi: 10.3389/fimmu.2020.589997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wu CX, Wang XQ, Chok SH, Man K, Tsang SHY, Chan ACY, Ma KW, Xia W, Cheung TT. Blocking CDK1/PDK1/beta-Catenin signaling by CDK1 inhibitor RO3306 increased the efficacy of sorafenib treatment by targeting cancer stem cells in a preclinical model of hepatocellular carcinoma. Theranostics. 2018;8:3737–3750. doi: 10.7150/thno.25487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Luo P, Feng X, Jing W, Zhu M, Li N, Zhou H, Worley PF, Chai H, Tu J. Clinical and Diagnostic Significance of Homer1 in hepatitis B virus-induced Hepatocellular Carcinoma. J Cancer. 2018;9:683–689. doi: 10.7150/jca.22279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jin GZ, Zhang Y, Cong WM, Wu X, Wang X, Wu S, Wang S, Zhou W, Yuan S, Gao H, Yu G, Yang W. Phosphoglucomutase 1 inhibits hepatocellular carcinoma progression by regulating glucose trafficking. PLoS Biol. 2018;16:e2006483. doi: 10.1371/journal.pbio.2006483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hu ML, Wang XY, Chen WM. TGF-beta1 upregulates the expression of lncRNA UCA1 and its downstream HXK2 to promote the growth of hepatocellular carcinoma. Eur Rev Med Pharmacol Sci. 2018;22:4846–4854. doi: 10.26355/eurrev_201808_15620. [DOI] [PubMed] [Google Scholar]
- 37.Finkelmeier F, Canli O, Peiffer KH, Walter D, Tal A, Koch C, Pession U, Vermehren J, Trojan J, Zeuzem S, Piiper A, Greten FR, Grammatikos G, Waidmann O. Circulating hypoxia marker carbonic anhydrase IX (CA9) in patients with hepatocellular carcinoma and patients with cirrhosis. PLoS One. 2018;13:e0200855. doi: 10.1371/journal.pone.0200855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen HL, OuYang HY, Le Y, Jiang P, Tang H, Yu ZS, He MK, Tang YQ, Shi M. Aberrant MCT4 and GLUT1 expression is correlated with early recurrence and poor prognosis of hepatocellular carcinoma after hepatectomy. Cancer Med. 2018;7:5339–5350. doi: 10.1002/cam4.1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Xu Q, Tu J, Dou C, Zhang J, Yang L, Liu X, Lei K, Liu Z, Wang Y, Li L, Bao H, Wang J, Tu K. HSP90 promotes cell glycolysis, proliferation and inhibits apoptosis by regulating PKM2 abundance via Thr-328 phosphorylation in hepatocellular carcinoma. Mol Cancer. 2017;16:178. doi: 10.1186/s12943-017-0748-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu Y, Wu H, Mei Y, Ding X, Yang X, Li C, Deng M, Gong J. Clinicopathological and prognostic significance of PKM2 protein expression in cirrhotic hepatocellular carcinoma and non-cirrhotic hepatocellular carcinoma. Sci Rep. 2017;7:15294. doi: 10.1038/s41598-017-14813-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hyuga S, Wada H, Eguchi H, Otsuru T, Iwgami Y, Yamada D, Noda T, Asaoka T, Kawamoto K, Gotoh K, Takeda Y, Tanemura M, Umeshita K, Doki Y, Mori M. Expression of carbonic anhydrase IX is associated with poor prognosis through regulation of the epithelial-mesenchymal transition in hepatocellular carcinoma. Int J Oncol. 2017;51:1179–1190. doi: 10.3892/ijo.2017.4098. [DOI] [PubMed] [Google Scholar]
- 42.Hua KT, Liu YF, Hsu CL, Cheng TY, Yang CY, Chang JS, Lee WJ, Hsiao M, Juan HF, Chien MH, Yang SF. 3'UTR polymorphisms of carbonic anhydrase IX determine the miR-34a targeting efficiency and prognosis of hepatocellular carcinoma. Sci Rep. 2017;7:4466. doi: 10.1038/s41598-017-04732-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang ZF, Feng XS, Chen H, Duan ZJ, Wang LX, Yang D, Liu PX, Zhang QP, Jin YL, Sun ZG, Liu H. Prognostic significance of synergistic hexokinase-2 and beta2-adrenergic receptor expression in human hepatocelluar carcinoma after curative resection. BMC Gastroenterol. 2016;16:57. doi: 10.1186/s12876-016-0474-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sun HW, Yu XJ, Wu WC, Chen J, Shi M, Zheng L, Xu J. GLUT1 and ASCT2 as Predictors for Prognosis of Hepatocellular Carcinoma. PLoS One. 2016;11:e0168907. doi: 10.1371/journal.pone.0168907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Liu WR, Tian MX, Yang LX, Lin YL, Jin L, Ding ZB, Shen YH, Peng YF, Gao DM, Zhou J, Qiu SJ, Dai Z, He R, Fan J, Shi YH. PKM2 promotes metastasis by recruiting myeloid-derived suppressor cells and indicates poor prognosis for hepatocellular carcinoma. Oncotarget. 2015;6:846–861. doi: 10.18632/oncotarget.2749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kang HJ, Kim IH, Sung CO, Shim JH, Yu E. Expression of carbonic anhydrase 9 is a novel prognostic marker in resectable hepatocellular carcinoma. Virchows Arch. 2015;466:403–413. doi: 10.1007/s00428-014-1709-0. [DOI] [PubMed] [Google Scholar]
- 47.Hu W, Lu SX, Li M, Zhang C, Liu LL, Fu J, Jin JT, Luo RZ, Zhang CZ, Yun JP. Pyruvate kinase M2 prevents apoptosis via modulating Bim stability and associates with poor outcome in hepatocellular carcinoma. Oncotarget. 2015;6:6570–6583. doi: 10.18632/oncotarget.3262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gao HJ, Zhao MC, Zhang YJ, Zhou DS, Xu L, Li GB, Chen MS, Liu J. Monocarboxylate transporter 4 predicts poor prognosis in hepatocellular carcinoma and is associated with cell proliferation and migration. J Cancer Res Clin Oncol. 2015;141:1151–1162. doi: 10.1007/s00432-014-1888-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chen Z, Lu X, Wang Z, Jin G, Wang Q, Chen D, Chen T, Li J, Fan J, Cong W, Gao Q, He X. Co-expression of PKM2 and TRIM35 predicts survival and recurrence in hepatocellular carcinoma. Oncotarget. 2015;6:2538–2548. doi: 10.18632/oncotarget.2991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chen R, Zhou X, Yu Z, Liu J, Huang G. Low Expression of LDHB Correlates With Unfavorable Survival in Hepatocellular Carcinoma: Strobe-Compliant Article. Medicine (Baltimore). 2015;94:e1583. doi: 10.1097/MD.0000000000001583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wong CC, Au SL, Tse AP, Xu IM, Lai RK, Chiu DK, Wei LL, Fan DN, Tsang FH, Lo RC, Wong CM, Ng IO. Switching of pyruvate kinase isoform L to M2 promotes metabolic reprogramming in hepatocarcinogenesis. PLoS One. 2014;9:e115036. doi: 10.1371/journal.pone.0115036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ohno A, Yorita K, Haruyama Y, Kondo K, Kato A, Ohtomo T, Kawaguchi M, Marutuska K, Chijiiwa K, Kataoka H. Aberrant expression of monocarboxylate transporter 4 in tumour cells predicts an unfavourable outcome in patients with hepatocellular carcinoma. Liver Int. 2014;34:942–952. doi: 10.1111/liv.12466. [DOI] [PubMed] [Google Scholar]
- 53.Tsunedomi R, Iizuka N, Yoshimura K, Iida M, Tsutsui M, Hashimoto N, Kanekiyo S, Sakamoto K, Tamesa T, Oka M. ABCB6 mRNA and DNA methylation levels serve as useful biomarkers for prediction of early intrahepatic recurrence of hepatitis C virus-related hepatocellular carcinoma. Int J Oncol. 2013;42:1551–1559. doi: 10.3892/ijo.2013.1854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chen YL, Uen YH, Li CF, Horng KC, Chen LR, Wu WR, Tseng HY, Huang HY, Wu LC, Shiue YL. The E2F transcription factor 1 transactives stathmin 1 in hepatocellular carcinoma. Ann Surg Oncol. 2013;20:4041–4054. doi: 10.1245/s10434-012-2519-8. [DOI] [PubMed] [Google Scholar]
- 55.Kwee SA, Hernandez B, Chan O, Wong L. Choline kinase alpha and hexokinase-2 protein expression in hepatocellular carcinoma: association with survival. PLoS One. 2012;7:e46591. doi: 10.1371/journal.pone.0046591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hsieh SY, Huang SF, Yu MC, Yeh TS, Chen TC, Lin YJ, Chang CJ, Sung CM, Lee YL, Hsu CY. Stathmin1 overexpression associated with polyploidy, tumor-cell invasion, early recurrence, and poor prognosis in human hepatoma. Mol Carcinog. 2010;49:476–487. doi: 10.1002/mc.20627. [DOI] [PubMed] [Google Scholar]
- 57.Daskalow K, Pfander D, Weichert W, Rohwer N, Thelen A, Neuhaus P, Jonas S, Wiedenmann B, Benckert C, Cramer T. Distinct temporospatial expression patterns of glycolysis-related proteins in human hepatocellular carcinoma. Histochem Cell Biol. 2009;132:21–31. doi: 10.1007/s00418-009-0590-4. [DOI] [PubMed] [Google Scholar]
- 58.Paudyal B, Paudyal P, Oriuchi N, Tsushima Y, Nakajima T, Endo K. Clinical implication of glucose transport and metabolism evaluated by 18F-FDG PET in hepatocellular carcinoma. Int J Oncol. 2008;33:1047–1054. [PubMed] [Google Scholar]
- 59.Ito Y, Takeda T, Sakon M, Monden M, Tsujimoto M, Matsuura N. Expression and prognostic role of cyclin-dependent kinase 1 (cdc2) in hepatocellular carcinoma. Oncology. 2000;59:68–74. doi: 10.1159/000012140. [DOI] [PubMed] [Google Scholar]
- 60.Zhang X, Wu LN, Li XQ, Luo X, Liu SW, Zhang L, Nawaz S, Ma LN, Ding XC. Whether the Golgi protein 73 could be a diagnostic serological marker in hepatocellular carcinoma: a meta analysis. BMC Gastroenterol. 2023;23:85. doi: 10.1186/s12876-023-02685-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lis P, Dylag M, Niedzwiecka K, Ko YH, Pedersen PL, Goffeau A, et al. The HK2 Dependent "Warburg Effect" and Mitochondrial Oxidative Phosphorylation in Cancer: Targets for Effective Therapy with 3-Bromopyruvate. Molecules. 2016;21:1730. [DOI] [PMC free article] [PubMed]
- 62.Zhang Q, Zheng S, Liu Q, Liu T, Tuerxun A, Yang L, Han X, Lu X. Prognostic significance of pyruvate kinase M2 expression in esophageal squamous cell carcinoma and its meta-analysis, Transl. Cancer Res. 2021;10:2643–2652. doi: 10.21037/tcr-21-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Xu D, Liang J, Lin J, Yu C. PKM2: A Potential Regulator of Rheumatoid Arthritis via Glycolytic and Non-Glycolytic Pathways. Front Immunol. 2019;10:2919. doi: 10.3389/fimmu.2019.02919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Clower CV, Chatterjee D, Wang Z, Cantley LC, Vander Heiden MG, Krainer AR. The alternative splicing repressors hnRNP A1/A2 and PTB influence pyruvate kinase isoform expression and cell metabolism. Proc Natl Acad Sci U S A. 2010;107:1894–1899. doi: 10.1073/pnas.0914845107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wang X, Liang C, Yao X, Yang RH, Zhang ZS, Liu FY, Li WQ, Pei SH, Ma J, Xie SQ, Fang D. PKM2-Induced the Phosphorylation of Histone H3 Contributes to EGF-Mediated PD-L1 Transcription in HCC. Front Pharmacol. 2020;11:577108. doi: 10.3389/fphar.2020.577108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Belletti B, Baldassarre G. Stathmin: a protein with many tasks. New biomarker and potential target in cancer. Expert Opin Ther Targets. 2011;15:1249–1266. doi: 10.1517/14728222.2011.620951. [DOI] [PubMed] [Google Scholar]
- 67.Zhang L, Li Y, Dai Y, Wang D, Wang X, Cao Y, Liu W, Tao Z. Glycolysis-related gene expression profiling serves as a novel prognosis risk predictor for human hepatocellular carcinoma. Sci Rep. 2021;11:18875. doi: 10.1038/s41598-021-98381-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Muramatsu T, Miyauchi T. Basigin (CD147): a multifunctional transmembrane protein involved in reproduction, neural function, inflammation and tumor invasion. Histol Histopathol. 2003;18:981–987. doi: 10.14670/HH-18.981. [DOI] [PubMed] [Google Scholar]
- 69.Halestrap AP, Price NT. The proton-linked monocarboxylate transporter (MCT) family: structure, function and regulation. Biochem J. 1999;343(Pt 2):281–299. doi: 10.1042/bj3430281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Halestrap AP. The SLC16 gene family - structure, role and regulation in health and disease. Mol Aspects Med. 2013;34:337–349. doi: 10.1016/j.mam.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 71.Wang Y, Li Y, Jiang L, Ren X, Cheng B, Xia J. Prognostic value of glycolysis markers in head and neck squamous cell carcinoma: a meta-analysis. Aging (Albany NY). 2021;13:7284–7299. doi: 10.18632/aging.202583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Islam RA, Hossain S, Chowdhury EH. Potential Therapeutic Targets in Energy Metabolism Pathways of Breast Cancer. Curr Cancer Drug Targets. 2017;17:707–721. doi: 10.2174/1568009617666170330150458. [DOI] [PubMed] [Google Scholar]
- 73.Yu M, Yongzhi H, Chen S, Luo X, Lin Y, Zhou Y, Jin H, Hou B, Deng Y, Tu L, Jian Z. The prognostic value of GLUT1 in cancers: a systematic review and meta-analysis. Oncotarget. 2017;8:43356–43367. doi: 10.18632/oncotarget.17445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Amann T, Maegdefrau U, Hartmann A, Agaimy A, Marienhagen J, Weiss TS, Stoeltzing O, Warnecke C, Scholmerich J, Oefner PJ, Kreutz M, Bosserhoff AK, Hellerbrand C. GLUT1 expression is increased in hepatocellular carcinoma and promotes tumorigenesis. Am J Pathol. 2009;174:1544–1552. doi: 10.2353/ajpath.2009.080596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mardones L, Ormazabal V, Romo X, Jana C, Binder P, Pena E, Vergara M, Zuniga FA. The glucose transporter-2 (GLUT2) is a low affinity dehydroascorbic acid transporter. Biochem Biophys Res Commun. 2011;410:7–12. doi: 10.1016/j.bbrc.2011.05.070. [DOI] [PubMed] [Google Scholar]
- 76.Wu L, Fritz JD, Powers AC. Different functional domains of GLUT2 glucose transporter are required for glucose affinity and substrate specificity. Endocrinology. 1998;139:4205–4212. doi: 10.1210/endo.139.10.6245. [DOI] [PubMed] [Google Scholar]
- 77.Kim YH, Jeong DC, Pak K, Han ME, Kim JY, Liangwen L, Kim HJ, Kim TW, Kim TH, Hyun DW, Oh SO. SLC2A2 (GLUT2) as a novel prognostic factor for hepatocellular carcinoma. Oncotarget. 2017;8:68381–68392. doi: 10.18632/oncotarget.20266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chen Y, Yang H, Chen S, Lu Z, Li B, Jiang T, Xuan M, Ye R, Liang H, Liu X, Liu Q, Tang H. SIRT1 regulated hexokinase-2 promoting glycolysis is involved in hydroquinone-enhanced malignant progression in human lymphoblastoid TK6 cells. Ecotoxicol Environ Saf. 2022;241:113757. doi: 10.1016/j.ecoenv.2022.113757. [DOI] [PubMed] [Google Scholar]
- 79.Krasnov GS, Dmitriev AA, Lakunina VA, Kirpiy AA, Kudryavtseva AV. Targeting VDAC-bound hexokinase II: a promising approach for concomitant anti-cancer therapy. Expert Opin Ther Targets. 2013;17:1221–1233. doi: 10.1517/14728222.2013.833607. [DOI] [PubMed] [Google Scholar]
- 80.Cheung EC, Ludwig RL, Vousden KH. Mitochondrial localization of TIGAR under hypoxia stimulates HK2 and lowers ROS and cell death. Proc Natl Acad Sci U S A. 2012;109:20491–20496. doi: 10.1073/pnas.1206530109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ditte P, Dequiedt F, Svastova E, Hulikova A, Ohradanova-Repic A, Zatovicova M, Csaderova L, Kopacek J, Supuran CT, Pastorekova S, Pastorek J. Phosphorylation of carbonic anhydrase IX controls its ability to mediate extracellular acidification in hypoxic tumors. Cancer Res. 2011;71:7558–7567. doi: 10.1158/0008-5472.CAN-11-2520. [DOI] [PubMed] [Google Scholar]
- 82.Wykoff CC, Beasley NJ, Watson PH, Turner KJ, Pastorek J, Sibtain A, Wilson GD, Turley H, Talks KL, Maxwell PH, Pugh CW, Ratcliffe PJ, Harris AL. Hypoxia-inducible expression of tumor-associated carbonic anhydrases. Cancer Res. 2000;60:7075–7083. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplementary figure 1. Forest plot showing the correlation between the expression levels of glycolysis markers and TTR in patients with liver cancer. A random-effects model was employed.
Additional file 2: Supplementary figure 2. Sensitivity analysis between the expression levels of glycolysis markers and OS.
Additional file 3: Supplementary figure 3. Sensitivity analysis between the expression levels of glycolysis markers and DFS (A), RFS (B) and TTR (C).
Additional file 4: Supplementary Table 1. Overview and characteristics of the eligible studies.
Additional file 5: Supplementary Table 2. Subgroup analysis of the correlation between the expression levels of glycolysis markers and DFS according to the specific glycolysis markers, region, and detection method.
Additional file 6: Supplementary Table 3. Subgroup analysis of the correlation between the expression levels of glycolysis markers and RFS according to the specific glycolysis markers.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.