Abstract
Background:
Lateral ankle sprain (LAS) is the most common sports-related injury. However, there are currently no published evidence-based criteria to guide the patient’s return to sport (RTS) and this decision is generally time-based. The aim of this study was to assess the psychometric properties of a new score (Ankle-GO) and its predictive ability for RTS at the same level of play after LAS.
Hypothesis:
The Ankle-GO is robust for discriminating and predicting RTS outcomes.
Study Design:
Prospective diagnostic study
Level of Evidence:
Level 2.
Methods:
The Ankle-GO was administered to 30 healthy participants and 64 patients at 2 and 4 months after LAS. The score was calculated as the sum of 6 tests for a maximum of 25 points. Construct validity, internal consistency, discriminant validity, and test-retest reliability were used to validate the score. The predictive value for the RTS was also validated based on the receiver operating characteristic (ROC) curve.
Results:
The internal consistency of the score was good (Cronbach’s alpha coefficient of 0.79) with no ceiling or floor effect. Test-retest reliability was excellent (intraclass coefficient correlation = 0.99) with a minimum detectable change of 1.2 points. The 2-month scores were significantly lower than 4-month and control group scores (7.7 ± 4, 13.9 ± 4.6, and 19.6 ± 3.4 points, respectively, P < 0.01). Ankle-GO values were also significantly higher in patients who returned to their preinjury level at 4 months compared with those who did not (P < 0.01). The predictive value of the 2-month Ankle-GO score was fair for a RTS at the same or higher than preinjury level at 4 months (area under ROC curve, 0.77; 95% CI, 0.65-0.89; P < 0.01).
Conclusion:
The Ankle-GO appears to be a valid and robust score for clinicians to predict and discriminate RTS in patients after LAS.
Clinical Relevance:
Ankle-GO is the first objective score to help in the decision-making of the RTS after LAS. At 2 months, patients with an Ankle-GO score <8 points are unlikely to RTS at the same preinjury level.
Keywords: ankle sprain, decision, functional testing, psychological readiness, return to sport
Acute lateral ankle sprain (LAS) is the most frequent osteoarticular injury, with an estimated incidence of between 2.1 and 3.2 per 1000 inhabitants per year in the general population, 23 and 40% of these are sports related. 16 The reinjury rate can reach 70% in certain groups of athletes, 23 and nearly 40% of patients will develop chronic ankle instability (CAI) in the year after injury.22,42
There are several explanations for this high rate of recurrence and the long-term consequences, including a premature return to sport (RTS). 28
Indeed, there are no validated criteria for an RTS after LAS and the RTS is mainly a time-based decision.51,55 Surprisingly, the word “ankle” cannot be found in the list of sports-related pathology in the expert consensus on the RTS. 2 Even though it is the most frequent sports-related injury, unlike the knee or shoulder,3,25 there is no objective score for the ankle, and no consensus exists on the RTS after LAS or CAI. 55
To help and guide the decision-making process for the management of RTS in these patients, a consensus was reached by the International Ankle Consortium on criteria for the definition and a precise evaluation of LAS to improve management of CAI.19,20 Hertel and Corbett 22 recently added numerous parameters (in particular, functional and psychological) to their model for CAI that should be assessed by practitioners to limit the risk of recurrent sprains.
Another very recent expert consensus retained 16 items, divided into 5 groups based on the Delphi method as objective criteria for the evaluation of RTS. 46 These 5 groups are Pain severity, Ankle impairments, Athlete perception, Sensorimotor control, and Sport/functional performance (PAASS). However, the authors did not propose specific tests to evaluate these items in patients. 46 One recent review of the literature confirmed the value of several functional tests and patient-reported outcome measures in the evaluation of LAS-related deficits and the risk of reinjury during the RTS phase. 35 Postural control deficits (static and dynamic), 11 poor hopping test results 27 as well as low self-reported function by the patient 15 are important risk factors for the development of CAI. Moreover, it is essential to use objective scores that evaluate different aspects of the patient’s psychological state such as self-confidence or fear of reinjury.27,46
Thus, we selected the most reliable and validated tests and cut-off scores found in the literature to distinguish patients with LAS or CAI from healthy persons or copers. 35 Based on these results, our team developed a composite clinical score called “Ankle-GO.”
The first objective of this study was to assess the psychometric properties of Ankle-GO in patients with LAS. The second objective was to evaluate its ability to predict RTS at the same or higher level of play. We hypothesized that Ankle-GO is a valid and reliable score, able to discriminate and predict the level of RTS 4 months after LAS.
Methods
Population
This prospective study included 64 patients (36 women and 28 men, 33.7 ± 13.2 years old) who had suffered a first or recurrent ankle sprain (Table 1). The injury was <1 month before inclusion and resulted from a sudden inversion mechanism that prevented them from participating in sport. Patients were all first examined by the same experienced orthopaedic surgeon at inclusion. Patients with signs of syndesmosis injury were excluded. 33 Only patients who practiced a sport at least once a week and who wished to return to their sport were included. A 4-month prescription for physical rehabilitation was given to the patients on the day of the consultation. The patients then underwent the Ankle-GO test at 2 and 4 months and responded to a question that specifically asked whether they had returned to their preinjury sport. The possible answers were “no”, “yes, but not at the same level of play,” and “yes, at the same or higher level.”
Table 1.
Participants characteristics
| Patients | Controls | |
|---|---|---|
| Sex, n (male/female) | 64 (28/36) | 30 (22/8) |
| Age, y ± SD | 33.7 ± 13.2 | 31.7 ± 13.5 |
| Type of main sport, n (%) | ||
| Pivot contact | 19 (29.7) | 9 (30) |
| Pivot | 22 (34.4) | 14 (46.7) |
| In line | 23 (35.9) | 7 (23.3) |
| Level of practice, n (%) | ||
| Professional | 2 (3.2) | 1 (3.3) |
| Intensive, >6 hours per week | 21 (32.8) | 3 (10) |
| Regular, 2-6 hours per week | 34 (53) | 9 (30) |
| Casual, <2 hours per week | 7 (10.9) | 17 (56.7) |
A control group included 30 subjects (8 women and 22 men, 31.7 ± 13.5 years old) who practiced sports regularly and had no history of lower limb injury (Table 1). Testing was blinded and administered by the same physical therapist who was trained in the evaluation of all functional tests. Patients provided informed consent, and this study received Institutional Ethics Approval (IRB00010835).
Construction of the Ankle-GO Score
Ankle-GO is a composite score based on the sum of 7 components for an objective evaluation of the main deficits associated with LAS or CAI and which can result in a risk of reinjury. 35 It was calculated from 4 functional tests: the single-leg stance test (SLS) on a firm surface, the modified star excursion balance test (mSEBT), the side hop test (SHT), and the figure-of-8 test (F8T). In addition, 2 patient self-reported questionnaires were used: the Foot and Ankle Ability Measure, involving 2 subscales evaluating activities in daily life (FAAMadl) and sports (FAAMsport), and the Ankle Ligament Reconstruction-Return to Sport after Injury (ALR-RSI).
The tests were selected for their capacity to distinguish healthy persons and copers from patients with CAI and based on criteria proposed by the PAASS framework, 46 as well as a review of the literature and an expert consensus. 35
Table 2 summarizes all tests and questionnaires as well as their clinimetric properties. The system to calculate points for each item is set out in Table 3 and presented in the following.
Table 2.
Clinical properties of the tests and questionnaires identified by Picot et al 35 to identify patients with CAI
| Tests | Cut-off Score | Reliability, ICC | Minimal Detectable Change | ||
|---|---|---|---|---|---|
| Functional performance testing | SLS | <3 errors | 0.93 | 0.6 errors | |
| mSEBT | COMP | COMP >90% | 0.91-0.93 | 6.70% | |
| ANT | <4.5% or 4 cm | 0.88 | 5.87% | ||
| PM | PM >91% | 0.87 | 7.84% | ||
| PL | PL >91% | 0.88 | 7.55% | ||
| SHT | <10 s | 0.84 | 5.82s | ||
| F8T | <12 s | 0.95 | 4.59s | ||
| PROM | FAAM | Activities of daily living | 95% for both scores | 0.89 | 3.96% |
| Sport | 0.87 | 7.90% | |||
| ALR-RSI | 55% | 0.92 | 10% | ||
ALR-RSI, ankle ligament reconstruction-return to sport after injury; ANT, anterior; CAI, chronic ankle instability; COMP, composite score; FAAM, foot and ankle ability measure; F8T, figure-of-8 test; ICC, intraclass correlation coefficient; mSEBT, star excursion balance test; PL, posterolateral; PM, posteromedial; PROM, patient-reported outcome measure; SHT, side hop test; SLS, single-leg stance test.
Table 3.
List of tests and questionnaires used for the construction of the Ankle-GO score and system to determine the points for each component
| Tests | Test Value | Weight | Maximum Score by Test | |
|---|---|---|---|---|
| SLS | >3 errors | 0 | 3 | |
| 1-3 errors | 1 | |||
| 0 errors | 2 | |||
| No feeling of instability | +1 | |||
| mSEBT | COMP <90% | 0 | 7 | |
| COMP 90-95% | 2 | |||
| COMP >95% | 4 | |||
| ANT >60% | +1 | |||
| PM >90% | +1 | |||
| No feeling of instability | +1 | |||
| SHT | >13 s | 0 | 5 | |
| 10-13 s | 2 | |||
| <10 s | 4 | |||
| No feeling of instability | +1 | |||
| F8T | >18 s | 0 | 3 | |
| 13-18 s | 1 | |||
| <13 s | 2 | |||
| No feeling of instability | +1 | |||
| FAAM | Activities of daily living | <90% | 0 | 2 |
| 90-95% | 1 | |||
| >95% | 2 | |||
| Sport | <80% | 0 | 2 | |
| 80-95% | 1 | |||
| >95% | 2 | |||
| ALR-RSI | <55% | 0 | 3 | |
| 55-63% | 1 | |||
| 63-76% | 2 | |||
| >76% | 3 | |||
ALR-RSI, ankle ligament reconstruction-return to sport after injury; ANT, anterior; COMP, composite score; FAAM, foot and ankle ability measure; F8T, figure-of-8 test; mSEBT, star excursion balance test; PM, posteromedial; PROM, patient-reported outcome measure; SHT, side hop test; SLS, single-leg stance test.
- Self-Reported Questionnaires
- ○ ALR-RSI, 3 points.
This questionnaire measures psychological readiness to RTS among patients with an injured ankle. 45 It includes 12 questions, from 0: No confidence to 10: Fully confident. The global score is obtained by dividing the total score by 1.2 to obtain a percentage. The coding procedure is similar to that for the RTS questionnaire after an anterior cruciate ligament injury or shoulder instability.17,54 This questionnaire was recently validated in French. 1
○ FAAM, 4 points.
This evaluates patient-reported function and is composed of 2 subscales: 21 items for the evaluation of daily activities (FAAMadl) and 8 items for sports (FAAMsport). 8 The patients respond to each item by completing a 5-point scale (0: incapable of performing the exercise to 4: without difficulty) or by responding “Not-applicable” when the activity in question is limited by something other than the foot or ankle. The percentage of each subscale is then determined. The score has been validated for CAI, 8 in French, 4 and as a digital version. 53
- Functional Performance Tests
- ○ SLS on a stable surface, 3 points.
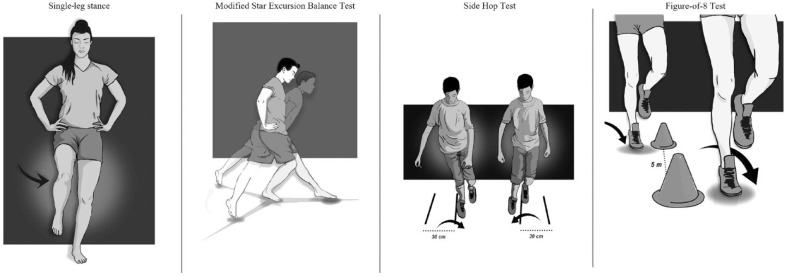
The subject must stand barefoot on 1 leg, with the knee slightly flexed (10°), hands on the hips for 20 seconds with the eyes closed (Figure 1). This test evaluates static postural control based on the participant’s number of errors. 41 One error was recorded for any of the following: lifting hands off hips, moving the thigh into more than 30° of flexion or abduction, lifting the forefoot or heel, remaining out of the testing position for >5 seconds, or opening eyes. The practitioner counted and added up the number of errors on each leg. After 2 learning sessions, the test was performed once on each foot.
Figure 1.
Functional performance tests.
○ mSEBT, 7 points.
This test is used to assess dynamic postural control deficits of the lower limbs, in particular among patients with CAI. 21 Recent practical guidelines were published on performing this test. 36 The patient stands barefoot on the tested foot in the center of a “Y” formed by 3 branches. The subject must reach as far as possible with the opposite leg in the 3 directions: anterior (ANT), posteromedial (PM), and posterolateral (PL), then return to the original position (Figure 1). The trial is refused if the subject takes his/her hands off the hips, if the weightbearing leg moves or if the heel is raised, if the subject loses balance or falls, or transfers their weight onto the nonweightbearing foot. To obtain comparable results, the distances obtained are normalized in relation to the length of the participant’s leg (from the anterior and superior iliac spine to the medial malleolus). After 4 learning trials in each direction for each leg, 3 trials were recorded and averaged.
The composite score (COMP) was then determined for each leg, corresponding to the average of the 3 directions (ANT, PM, and PL).
One point was added if the measurement in the ANT direction was >60% and another point if the measurement in the PM direction of was >90% (Table 3). 43
○ SHT, 5 points.
This test involves hopping laterally and medially as fast as possible 10 times between 2 lines 30 cm apart. 14 The first hop is always toward the outside (Figure 1). If the patient touches the line, that back-and-forth hop is not counted.
○ F8T, 3 points.
This test involves skipping in a figure 8 around 2 posts 5 m apart as fast as possible (Figure 1). 7 The patient has to perform 2 consecutive laps (for a total distance of 20 m).
Because Caffrey et al 7 have clearly shown the importance of assessing feelings of giving way in patients with LAS or CAI, 1 additional point was added for each test if the patient did not experience instability during the tasks.
Statistical Analysis
Ankle-GO was validated according to the international COSMIN (COnsensus-based Standards for the selection of health Measurement INstruments) standards. 31
Floor and Ceiling Effects
The floor or ceiling effects were considered to be present if >15% of the subjects tested obtained the lowest (0 points) or highest (25 points) possible score, respectively.
Internal Consistency
Internal consistency of the 7 components of Ankle-GO were evaluated with the Cronbach’s alpha coefficient. An α value between 0.7 and 0.9 indicated good consistency with no significant risk of redundancy among the items.31,47 The internal consistency was evaluated for the entire score and when a single item was deleted.
Construct Validity (Structural Validity)
The Pearson (r) correlation coefficient was calculated to measure the strength of the association between the individual components in relation to the others, as well as for each component in relation to the total Ankle-GO score. The correlations were considered to be weak (0.3 < r < 0.1), moderate (0.5 < r < 0.3), or strong (r > 0.5). 44
Test-Retest Reliability and Sensitivity to Change
The test-retest reliability identifies whether the score provides the same results when repeated in subjects whose health has not changed. 31 Thus, 15 injured patients underwent the test twice 1 week apart. The test-retest reliability was evaluated with the intraclass correlation coefficient (ICC, 2-way mixed-effects, absolute agreement) and interpreted as “poor” for values <0.5, “moderate” between 0.5 and 0.75, “good” between 0.75 and 0.9, and “excellent” >0.9.26,39 We also determined the standard error of measurement (SEM) and the minimal detectable change (MDC) of the score. The MDC was calculated with the following equation: MDC = 1.96 × √2 × SEM. 24
Discriminant Validity
The discriminant validity was evaluated for all of the items as well as for the Ankle-GO score using a Wilcoxon signed-rank test for paired samples between the results obtained at 2 and 4 months. Ankle-GO was also compared between patients at 4 months and control subjects using independent Student t test. The Ankle-GO scores between patients who resumed at the same or higher level, those who returned at a lower level, and those who did not RTS after 4 months were also compared using a 1-way analysis of variance.
Predictive Validation Process
The predictive validity of the score was evaluated with the receiver operating characteristic (ROC) curve and the Youden index (J = sensitivity + specificity - 1), based on the Ankle-GO at 2 months and RTS status at 4 months. Two predictive analyses were performed. First, the predictive validity of the RTS at the same or higher preinjury level of sport was determined. For this, the RTS was dichotomized as patients who returned to their preinjury level or higher, and those who did not (no RTS, or lower level of sport).
Second, the predictive validity of no RTS was determined. For this analysis, the RTS was divided into patients who did not RTS and those who did, regardless the level of sport.
The area under the curve (AUC) was determined for each predictive analysis. The precision of the score was considered to be null (AUC = 0.5), low (0.5 < AUC < 0.7), fair to good (0.7 ≤ AUC < 0.9), high (0.9 ≤ AUC < 1), or perfect (AUC = 1). All statistical tests were performed with SPSS 12.0 (IBM Corp) software. P ≤ 0.05 was considered to be significant.
Results
The mean raw values as well as the scores for each component of Ankle-GO are presented in Appendix Table A1 (available in the online version of this article). All included patients performed all of the tests at 2 and 4 months, for a completion rate of 100%.
Floor and Ceiling Effects
No floor or ceiling effects were detected, and none of the participants obtained a maximum or minimum score. The minimum total score was 1 point (5 subjects) and the maximum was 23 points (1 subject).
Internal Consistency and Construct Validity
The internal consistency of the scale was good, with a Cronbach’s alpha coefficient of 0.79. Inter-item correlations were also high, with a mean of 0.55 (0.35-0.72). Deletion of items did not significantly decrease or increase the α coefficient (Appendix Table A2, available online).
Test-Retest Reliability
The ICC2,1 for repeated measures was 0.99 for the Ankle-GO score, with a corresponding SEM of 0.41 points and an MDC of 1.2 points, which represents the minimum change required to be 95% confident that real clinical change has occurred.
Discriminant Validity
There was a significant difference among the Ankle-GO results in patients at 2 and 4 months and in control subjects (Table 4).
Table 4.
Results obtained in relation to RTS at 2 and 4 months
| 2 Months | 4 Months | |||||||
|---|---|---|---|---|---|---|---|---|
| Same or Higher Level (n = 0) | Lower Level (n = 15) | No Sport (n = 49) |
P | Same or Higher Level (n = 32) | Lower Level (n = 20) | No Sport (n = 12) | P | |
| Ankle-GO | NA | 10.3 ± 3.6c | 7.1 ± 4.1 | <0.01 | 17.2 ± 3.5 a | 12.4 ± 4.1 | 9.3 ± 3 | <0.01 |
| FAAMadl, % | NA | 92.1 ± 5.4c | 82.9 | 0.03 | 96.8 ± 4.4 a | 92.4 ± 5.9 c | 86.2 ± 10.5 | <0.01 |
| FAAMsport, % | NA | 73.8 ± 13.1 | 55.4 ± 22.9 | <0.01 | 89.3 ± 10.4 a | 75.9 ± 17 c | 62.5 ± 19.4 | <0.01 |
| ALR-RSI, % | NA | 60.3 ± 13.8c | 40.3 ± 21 | <0.01 | 80.9 ± 15.5 a | 58.8 ± 18.1 | 50.4 ± 21 | <0.01 |
| SLS, errors | NA | 2.7 ± 2.5 | 3.7 ± 3 | 0.25 | 1.6 ± 1.9 | 1.9 ± 1.8 | 2.2 ± 1.8 | 0.67 |
| mSEBT COMP, % | NA | 84.6 ± 6.4c | 78.7 ± 7 | <0.01 | 86.8 ± 6.5 b | 83.7 ± 7 | 81.4 ± 7 | 0.04 |
| mSEBT ANT, % | NA | 65 ± 4.7c | 59.4 ± 6.5 | <0.01 | 68.5 ± 4.9 b | 67.8 ± 5 | 65.1 ± 6.7 | 0.03 |
| mSEBT PM, % | NA | 95.3 ± 9.4c | 91.7 ± 8.3 | 0.16 | 96.9 ± 7.7 | 94.7 ± 7.7 | 92.7 ± 8.2 | 0.26 |
| mSEBT PL, % | NA | 93.4 ± 8.9 | 85.3 ± 10.2 | <0.01 | 93.6 ± 9.3 | 92.1 ± 11.9 | 88 ± 10.6 | 0.29 |
| SHT, s | NA | 20.4 ± 9.6 | 22.6 ± 11.5 | 0.51 | 11.3 ± 3.8 b | 14.3 ± 7.4 | 16.8 ± 5.6 | 0.01 |
| F8T, s | NA | 17 ± 5 | 22.1 ± 10 | 0.06 | 12.5 ± 2.5 b | 14.5 ± 4.8 | 17.1 ± 6.9 | 0.01 |
adl, activities of daily living; ALR-RSI, ankle ligament reconstruction-RTS after injury; FAAM, foot and ankle ability measure; F8T, figure-of-8 test; mSEBT, modified star excursion balance test; NA, not applicable since no patient returned to sport at the same level at 2 months; PL, posterolateral; PM, posteromedial; SHT, side hop test; SLS, single-leg stance.
Significant difference between “same or higher level” and “lower level.”
Significant difference between “same or higher level” and “no sport.”
Significant difference between “lower level” and “no sport.”
Predictive Ability of Returning to Preinjury Level of Sport or Higher
Of the 64 patients included in the study, 32 (50%) returned to the preinjury level of sport at 4 months (Table 4). The capacity of Ankle-GO at 2 months to predict RTS at preinjury level at 4 months was good (AUC = 0.77; 95% CI, 0.64-0.88; P < 0.01). A Youden index of 0.38 was observed for a score of 8 points, which corresponds to a sensitivity of 72% and a specificity of 66% (Figure 2).
Figure 2.
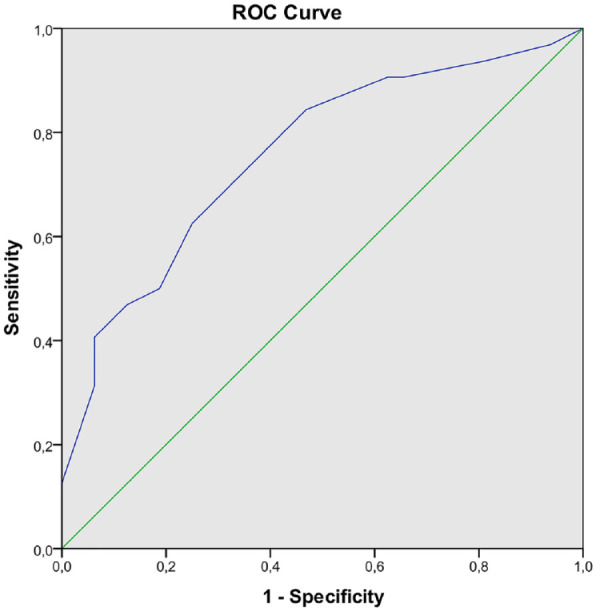
ROC curve for Ankle-GO score for predicting return to preinjury level of sport or higher. ROC, receiver operating characteristic.
Predictive Ability for not Returning to Sport
Of the 64 patients included in the study, 12 (19%) did not RTS at 4 months (Table 4). The capacity of Ankle-GO at 2 months to predict no RTS at 4 months, regardless of the level of sport, was also good (AUC = 0.77; 95% CI, 0.65-0.89; P < 0.01). A Youden index of 0.44 was observed for a score of 7 points, which corresponded to a sensitivity of 67% and a specificity of 92% (Figure 3).
Figure 3.
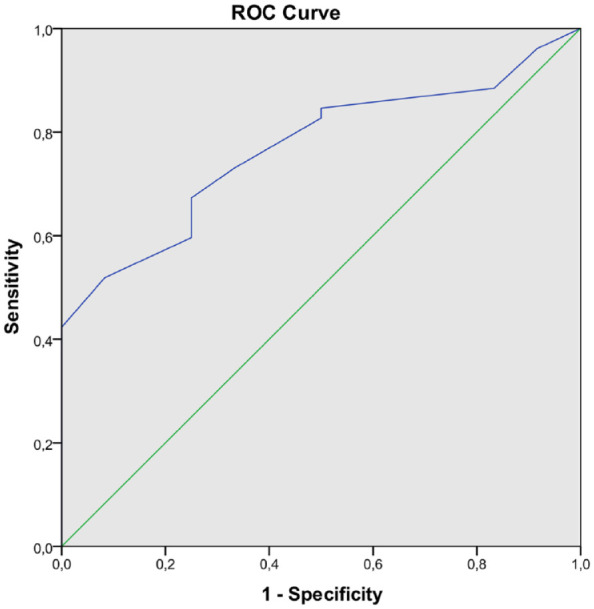
ROC curve for Ankle-GO score for predicting no RTS. ROC, receiver operating characteristic; RTS, return to sport.
Discussion
The purpose of this study was to develop and validate a new clinical composite score to assess patients who suffered LAS during the RTS continuum. We also aimed to evaluate its ability to predict RTS at the same or higher level of play.
The results showed that the test-retest reliability of the Ankle-GO was excellent, with no ceiling or floor effects. Clinical sensitivity to change is important to take into account when evaluating patients along the RTS continuum. We therefore determined the SEM and MDC, which were found to have a very good sensitivity to change. In comparison, the SEM and MDC in a similar score for anterior cruciate ligament reconstruction were 3 times higher than in the Ankle-GO (1.2 vs 0.41 and 3.3 vs 1.2 for SEM and MDC, respectively). 3
The internal consistency of Ankle-GO was also optimal (0.7 < Cronbach’s alpha <0.9) providing high inter-relatedness without redundancy among items. 47 Discriminant validity of the test was also good since it allows healthy persons to be distinguished from those who returned to sport or not. The scores at 2 months were also significantly lower than those at 4 months.
One important result of this prospective study is the good ability of the Ankle-GO score at 2 months to predict RTS at 4 months at the same preinjury level or higher. Clinically, this means that patients who do not reach a score of 8 points at 2 months are unlikely to return to their preinjury level of sport at 4 months. Moreover, patients with a score <7 points at 2 months have a low probability of returning to sport. This predictive capacity is highly important for practitioners, since they can adjust the rehabilitation at 2 months on the basis of patient’s deficits/capacities. In addition, it should help to prevent the risk of a premature RTS by using objective criteria rather than time-based decisions and therefore decreased the risk of recurrences.10,46,51 Indeed, approximately 90% of athletes who suffered from a first or recurrent LAS returned to participation within a week even though it takes 6 to 12 weeks for the ligaments to heal. 28
It is interesting to note that even patients who returned to sport at the same preinjury level or higher at 4 months had scores that were significantly lower than those of the control group (Tables 4 and A1). In particular, the ALR-RSI score was markedly lower than in controls (80.9% vs 96.1%), which could be a sign that there is a strong fear of reinjury, even in subjects who RTS at the same level.48,54 Nevertheless, their scores were higher than those who successfully returned to sport after ligament reconstruction (regardless the level of practice) or patients who underwent a modified Broström-Gould procedure (68.8% and 61.9%, respectively).37,45 These results confirmed the importance to assess psychological readiness to RTS during rehabilitation in patients suffering from LAS.22,46
The composite mSEBT score was also significantly lower in patients with an RTS at the same or higher preinjury level than that in healthy subjects (86.8% vs 91.9%, respectively). This value is close to the cut-off score identified by Butler et al, 6 who showed that the risk of lower limb injury was increased when the COMP score was <89.6%. Finally, the FAAMsport was also significantly lower in patients who RTS at the same or higher preinjury level compared with healthy participants (89.3% vs 99%) and <95%, which corresponds to the threshold proposed to define a “coper.” 22
Several elements can explain the good reliability, validity, and predictive capacity of the Ankle-GO for the RTS. First, all items were selected according to their ability to assess deficits among patients with LAS or CAI based on an expert consensus report, 46 and recent systematic reviews of the literature on RTS.51,55 The tests used were also selected according to their frequency of use, complementarity, and the level of scientific evidence. 35 Thus, the Ankle-GO score includes various functional tests (SLS, mSEBT, SHT, F8T), self-reported functional questionnaires (FAAMadl and FAAMsport), and an evaluation of the patient’s psychological status (ALR-RSI) to provide a global overview of patients deficits. All these elements are considered as risk factors for reinjury after LAS.11,15,27,46 The weight of each test was adapted in relation with the level of evidence, which explains, for example, the high number of points assigned to mSEBT.21,36,38,40 Second, threshold values were also chosen for each item based on the results in the literature (cut-off scores and MDC) of the different tests.35,43 The evaluation of instability reported by the subject when performing functional tests is crucial in the evaluation of ankle instability. 7 Thus, besides objective performance, points were also added if the patient did not experience any feeling of instability during the tests.
Finally, the Ankle-GO score was designed in a manner similar to that of other composite tests for RTS after knee and shoulder stabilization.3,25 However, the strength of this study is its prospective design, allowing the capacity of the Ankle-GO at 2 months to predict RTS at preinjury level at 4 months to be evaluated. To our knowledge, this is the first score identifying and discriminating patients who will RTS at the same or higher preinjury level from those who will not.
The completion rate of 100% shows that the applicability of this score is good. Indeed, Ankle-GO is easy to perform in daily clinical practice, and does not require any particular material, is simple and rapid to administer (<30 minutes), and could thus be easily accessible for practitioners. Each of the self-reported questionnaires have already been validated in English and French,1,4,8,37,45 and the FAAM in numerous other languages,9,18,34,52 facilitating their use and the diffusion of Ankle-GO. To simplify its practical use, we have developed a free application (Ankle-GO) that automatically calculates the patient’s score for each item and the final result.
Limitations
The severity of ligament injuries was not taken into account, which could have likely created a major inclusion bias. However, that made it possible to evaluate the use of Ankle-GO in the entire population of patients with LAS. Diagnosis of the sprain was based only on a clinical examination by an experienced surgeon. While no other paraclinical diagnostic examinations were performed, patients presenting with clinical signs of syndesmosis injury were excluded due to the large differences in term of rates and time to RTS related to high ankle sprains.12,13,30,32,33 Although motivation is a highly important factor in the RTS, as shown in a recent study on anatomic ankle ligament reconstruction, 5 this was not evaluated in our study. However, only patients declaring that they wished to RTS during the initial consultation were included in the study. Also, included patients were heterogeneous (age, BMI, level of play, type of sport), which can influence the RTS rate. 51 Finally, we did not control the type of physical therapy that patients received. This is a weak point in the study because the rehabilitation sessions certainly differed. However, it is important to consider the recent guidelines of the International Ankle Consortium, which clearly recommend physical therapy on a case-by-case basis depending on the specific individual deficits of each patient. Thus, by definition, these sessions will be different for each patient, as they are individualized. 10 In addition, we have included both recurrent and primary ankle injury. Indeed, our goal was to generalize the test and make it applicable to all patients, because the literature does not report any difference in the time to RTS between these 2 groups. 28 Cartilage injury and/or residual pain can persist for up to 1 year and influence RTS.29,46,50 This factor was not taken into account when calculating Ankle-GO.
Moreover, the fact that the evaluator was not the physical therapists who conducted the rehabilitation (blind assessment) should be considered a strength in the present study, as it prevented certain biases during testing.
We did not control who was in charge of clearing patients for RTS, and patients returned to sports mainly when they felt ready in accordance with their practitioners. Indeed, there are currently no standard criteria to inform RTS decisions for patients with a LAS. This confirms the importance of building new scores and evaluating their robustness help practitioners in the decision making process for RTS.
The number of patients in this study was limited (n = 64) but none were lost to follow-up, and there was a completion rate of 100%. According to the high rate of recurrences in LAS, longer follow-up would allow to evaluate the rate of reinjury or identify coper patients to refine the Ankle-GO test cut-off score for RTS.
It is also worth noting that there is significant confusion in the terminology of RTS in the literature. 51 Indeed, the consensus article by Ardern et al 2 clearly defined 3 phases in a continuum to be considered for an optimal RTS. First, a return to participation with active rehabilitation, modified training, or practicing a sport at a lower level than the final goal. Then, RTS in which the subject practices his/her sport but not at the desired level of performance. Finally, a return to performance in which the patient is performing at the same or higher preinjury level of play. It is important to note that the Ankle-GO score does not take into account key parameters for the return to performance, such as accomplishing optimal performance under fatigue or performing complex tasks challenging neurocognitive processing capacities (multitasking, disturbed vision, facing an opponent, etc). It therefore seems prudent to consider that this score is probably best adapted to be a basic reference for RTS, rather than a score with a real ceiling to validate the return to performance, especially in high-level sports, or sports at high risk of ankle injury (pivot-contact sports or martial arts, for example). In this case, the notion of the return to the preinjury level of play must be evaluated from the point of view of the patient’s existing skills compared with the skills actually required at the patient’s preinjury level of play. 49
Conclusion
Ankle-GO is a valid and reliable score when assessing patients after LAS during the RTS continuum. This inexpensive clinical tool composed of functional test and self-reported questionnaires seems relevant to discriminate and predict the level of RTS. At 2 months after injury, a patient exhibiting an Ankle-GO score <8 points is unlikely to resume at the same preinjury level at 4 months.
Supplemental Material
Supplemental material, sj-docx-1-sph-10.1177_19417381231183647 for Development and Validation of the Ankle-GO Score for Discriminating and Predicting Return-to-Sport Outcomes After Lateral Ankle Sprain by Brice Picot, Ronny Lopes, Gauthier Rauline, François Fourchet and Alexandre Hardy in Sports Health
Footnotes
The following authors declared potential conflicts of interest: R.L. has received royalties from Serf Extremity, PODONOV, and Implant Service Orthopedie, and consulting fees and honoraria from Arthrex. A.H. has received consulting fees from Arthrex.
References
- 1. Ajaka N, Bouché P-A, Dagher M, Lopes R, Bauer T, Hardy A. The French Ankle Ligament Reconstruction - Return to Sport after Injury (ALR-RSI-Fr) is a valid scale for the French population. J Exp Orthop. 2022;9(1):27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ardern CL, Glasgow P, Schneiders A, et al. 2016 Consensus statement on return to sport from the First World Congress in Sports Physical Therapy, Bern. Br J Sports Med. 2016;50(14):853-864. [DOI] [PubMed] [Google Scholar]
- 3. Blakeney WG, Ouanezar H, Rogowski I, et al. Validation of a composite test for assessment of readiness for return to sports after anterior cruciate ligament reconstruction: the K-STARTS test. Sports Health. 2018;10(6):515-522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Borloz S, Crevoisier X, Deriaz O, Ballabeni P, Martin RL, Luthi F. Evidence for validity and reliability of a French version of the FAAM. BMC Musculoskelet Disord. 2011;12:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bouveau V, Housset V, Chasset F, Bauer T, Hardy A. Return to sports: rate and time after arthroscopic surgery for chronic lateral ankle instability. Orthop Traumatol Surg Res. 2022;108(7):103398. [DOI] [PubMed] [Google Scholar]
- 6. Butler RJ, Lehr ME, Fink ML, Kiesel KB, Plisky PJ. Dynamic balance performance and noncontact lower extremity injury in college football players: an initial study. Sports Health. 2013;5(5):417-422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Caffrey E, Docherty CL, Schrader J, Klossnner J. The ability of 4 single-limb hopping tests to detect functional performance deficits in individuals with functional ankle instability. J Orthop Sports Phys Ther. 2009;39(11):799-806. [DOI] [PubMed] [Google Scholar]
- 8. Carcia CR, Martin RL, Drouin JM. Validity of the foot and ankle ability measure in athletes with chronic ankle instability. J Athl Train. 2008;43(2):179-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cervera-Garvi P, Ortega-Avila AB, Morales-Asencio JM, Cervera-Marin JA, Martin RR, Gijon-Nogueron G. Cross-cultural adaptation and validation of Spanish version of The Foot and Ankle Ability Measures (FAAM-Sp). J Foot Ankle Res. 2017;10:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Delahunt E, Bleakley CM, Bossard DS, et al. Clinical assessment of acute lateral ankle sprain injuries (ROAST): 2019 consensus statement and recommendations of the International Ankle Consortium. Br J Sports Med. 2018;52(20):1304-1310. [DOI] [PubMed] [Google Scholar]
- 11. Delahunt E, Remus A. Risk Factors for lateral ankle sprains and chronic ankle instability. J Athl Train. 2019;54(6):611-616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. D’Hooghe P, Cruz F, Alkhelaifi K. Return to play after a lateral ligament ankle sprain. Curr Rev Musculoskelet Med. 2020;13(3):281-288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. D’Hooghe P, Grassi A, Alkhelaifi K, et al. Return to play after surgery for isolated unstable syndesmotic ankle injuries (West Point grade IIB and III) in 110 male professional football players: a retrospective cohort study. Br J Sports Med. 2020;54(19):1168-1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Docherty CL, Arnold BL, Gansneder BM, Hurwitz S, Gieck J. Functional-performance deficits in volunteers with functional ankle instability. J Athl Train. 2005;40(1):30-34. [PMC free article] [PubMed] [Google Scholar]
- 15. Doherty C, Bleakley C, Hertel J, Caulfield B, Ryan J, Delahunt E. Recovery from a first-time lateral ankle sprain and the predictors of chronic ankle instability: a prospective cohort analysis. Am J Sports Med. 2016;44(4):995-1003. [DOI] [PubMed] [Google Scholar]
- 16. Doherty C, Delahunt E, Caulfield B, Hertel J, Ryan J, Bleakley C. The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sports Med. 2014;44(1):123-140. [DOI] [PubMed] [Google Scholar]
- 17. Gerometta A, Klouche S, Herman S, Lefevre N, Bohu Y. The Shoulder Instability-Return to Sport after Injury (SIRSI): a valid and reproducible scale to quantify psychological readiness to return to sport after traumatic shoulder instability. Knee Surg Sports Traumatol Arthrosc. 2018;26(1):203-211. [DOI] [PubMed] [Google Scholar]
- 18. González-Sánchez M, Li GZ, Ruiz Muñoz M, Cuesta-Vargas AI. Foot and ankle ability measure to measure functional limitations in patients with foot and ankle disorders: a Chinese cross-cultural adaptation and validation. Disabil Rehabil. 2017;39(21):2182-2189. [DOI] [PubMed] [Google Scholar]
- 19. Gribble PA, Bleakley CM, Caulfield BM, et al. 2016 consensus statement of the International Ankle Consortium: prevalence, impact and long-term consequences of lateral ankle sprains. Br J Sports Med. 2016;50(24):1493-1495. [DOI] [PubMed] [Google Scholar]
- 20. Gribble PA, Delahunt E, Bleakley CM, et al. Selection criteria for patients with chronic ankle instability in controlled research: a position statement of the International Ankle Consortium. J Athl Train. 2014;49(1):121-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gribble PA, Hertel J, Plisky P. Using the star excursion balance test to assess dynamic postural-control deficits and outcomes in lower extremity injury: a literature and systematic review. J Athl Train. 2012;47(3):339-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hertel J, Corbett RO. An updated model of chronic ankle instability. J Athl Train. 2019;54(6):572-588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Herzog MM, Kerr ZY, Marshall SW, Wikstrom EA. Epidemiology of ankle sprains and chronic ankle instability. J Athl Train. 2019;54(6):603-610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hopkins WG. Measures of reliability in sports medicine and science. Sports Med. 2000;30(1):1-15. [DOI] [PubMed] [Google Scholar]
- 25. Juré D, Blache Y, Degot M, et al. The S-STARTS Test: validation of a composite test for the assessment of readiness to return to sport after shoulder stabilization surgery. Sports Health. 2022;14(2):254-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Martin RL, Davenport TE, Fraser JJ, et al. Ankle stability and movement coordination impairments: lateral ankle ligament sprains revision 2021: clinical practice guidelines linked to the International Classification of Functioning, Disability and Health From the Academy of Orthopaedic Physical Therapy of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2021;51(4):CPG1-CPG80. [DOI] [PubMed] [Google Scholar]
- 28. Medina McKeon JM, Bush HM, Reed A, Whittington A, Uhl TL, McKeon PO. Return-to-play probabilities following new versus recurrent ankle sprains in high school athletes. J Sci Med Sport. 2014;17(1):23-28. [DOI] [PubMed] [Google Scholar]
- 29. Michels F, Wastyn H, Pottel H, Stockmans F, Vereecke E, Matricali G. The presence of persistent symptoms 12 months following a first lateral ankle sprain: a systematic review and meta-analysis. Foot Ankle Surg. 2022;28(7):817-826. [DOI] [PubMed] [Google Scholar]
- 30. Miller BS, Downie BK, Johnson PD, et al. Time to return to play after high ankle sprains in collegiate football players: a prediction model. Sports Health. 2012;4(6):504-509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mokkink LB, Terwee CB, Patrick DL, et al. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J Clin Epidemiol. 2010;63(7):737-745. [DOI] [PubMed] [Google Scholar]
- 32. Netterström-Wedin F, Bleakley C. Diagnostic accuracy of clinical tests assessing ligamentous injury of the ankle syndesmosis: a systematic review with meta-analysis. Phys Ther Sport. 2021;49:214-226. [DOI] [PubMed] [Google Scholar]
- 33. Netterström-Wedin F, Matthews M, Bleakley C. Diagnostic accuracy of clinical tests assessing ligamentous injury of the talocrural and subtalar joints: a systematic review with meta-analysis. Sports Health. 2022;14(3):336-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Obionu KC, Krogsgaard MR, Hansen CF, Comins JD. Dual-panel translation to Danish and Rasch validation of the Foot and Ankle Ability Measure (FAAM-DK). Foot Ankle Surg. 2022;28(5):588-594. [DOI] [PubMed] [Google Scholar]
- 35. Picot B, Hardy A, Terrier R, Tassignon B, Lopes R, Fourchet F. Which functional tests and self-reported questionnaires can help clinicians make valid return to sport decisions in patients with chronic ankle instability? A narrative review and expert opinion. Front Sports Act Living. 2022;4:902886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Picot B, Terrier R, Forestier N, Fourchet F, McKeon PO. The star excursion balance test: an update review and practical guidelines. Int J Athl Ther Train. 2021;26(6):285-293. [Google Scholar]
- 37. Pioger C, Guillo S, Bouché P-A, et al. The ALR-RSI score is a valid and reproducible scale to assess psychological readiness before returning to sport after modified Broström-Gould procedure. Knee Surg Sports Traumatol Arthrosc. 2022;30(7):2470-2475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Plisky P, Schwartkopf-Phifer K, Huebner B, Garner MB, Bullock G. Systematic review and meta-analysis of the Y-balance test lower quarter: reliability, discriminant validity, and predictive validity. Int J Sports Phys Ther. 2021;16(5):1190-1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice. 3rd ed. Prentice Hall; 2009. [Google Scholar]
- 40. Powden CJ, Dodds TK, Gabriel EH. The reliability of the star excursion balance test and lower quarter Y-balance test in healthy adults: a systematic review. Intl J Sports Phys Ther. 2019;14(5):683-694. [PMC free article] [PubMed] [Google Scholar]
- 41. Riemann B, A. Caggiano N, M. Lephart S. Examination of a clinical method of assessing postural control during a functional performance task. J Sport Rehab. 1999;8(3):171-183. [Google Scholar]
- 42. Rijn RM van, Os AG van, Bernsen RMD, Luijsterburg PA, Koes BW, Bierma-Zeinstra SMA. What is the clinical course of acute ankle sprains? A systematic literature review. Am J Med. 2008;121(4):324-331.e7. [DOI] [PubMed] [Google Scholar]
- 43. Rosen AB, Needle AR, Ko J. Ability of functional performance tests to identify individuals with chronic ankle instability: a systematic review with meta-analysis. Clin J Sport Med. 2019;29(6):509-522. [DOI] [PubMed] [Google Scholar]
- 44. Salkind N. Encyclopedia of Measurement and Statistics. 2007. https://sk.sagepub.com/reference/statistics. Accessed February 4, 2021
- 45. Sigonney F, Lopes R, Bouché P-A, et al. The ankle ligament reconstruction-return to sport after injury (ALR-RSI) is a valid and reproducible scale to quantify psychological readiness before returning to sport after ankle ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2020;28(12):4003-4010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Smith MD, Vicenzino B, Bahr R, et al. Return to sport decisions after an acute lateral ankle sprain injury: introducing the PAASS framework - an international multidisciplinary consensus. Br J Sports Med. 2021;55:1270-1276. [DOI] [PubMed] [Google Scholar]
- 47. Streiner DL. Starting at the beginning: an introduction to coefficient alpha and internal consistency. J Pers Assess. 2003;80(1):99-103. [DOI] [PubMed] [Google Scholar]
- 48. Suttmiller AMB, McCann RS. Injury-related fear in individuals with and without chronic ankle instability: a systematic review. J Sport Rehabil. 2021;30(8):1203-1212. [DOI] [PubMed] [Google Scholar]
- 49. Taberner M, Allen T, Cohen DD. Progressing rehabilitation after injury: consider the ‘control-chaos continuum.’ Br J Sports Med. 2019;53(18):1132-1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Taga I, Shino K, Inoue M, Nakata K, Maeda A. Articular cartilage lesions in ankles with lateral ligament injury. An arthroscopic study. Am J Sports Med. 1993;21(1):120-126; discussion 126-127. [DOI] [PubMed] [Google Scholar]
- 51. Tassignon B, Verschueren J, Delahunt E, et al. Criteria-based return to sport decision-making following lateral ankle sprain injury: a systematic review and narrative synthesis. Sports Med. 2019;49(4):601-619. [DOI] [PubMed] [Google Scholar]
- 52. Uematsu D, Suzuki H, Sasaki S, et al. Evidence of validity for the Japanese version of the foot and ankle ability measure. J Athl Train. 2015;50(1):65-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Uimonen MM, Ponkilainen VT, Toom A, et al. Validity of five foot and ankle specific electronic patient-reported outcome (ePRO) instruments in patients undergoing elective orthopedic foot or ankle surgery. Foot Ankle Surg. 2021;27(1):52-59. [DOI] [PubMed] [Google Scholar]
- 54. Webster KE, Feller JA, Lambros C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys Ther Sport. 2008;9(1):9-15. [DOI] [PubMed] [Google Scholar]
- 55. Wikstrom EA, Mueller C, Cain MS. Lack of consensus on return-to-sport criteria following lateral ankle sprain: a systematic review of expert opinions. J Sport Rehab. 2020;29(2):231-237. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-sph-10.1177_19417381231183647 for Development and Validation of the Ankle-GO Score for Discriminating and Predicting Return-to-Sport Outcomes After Lateral Ankle Sprain by Brice Picot, Ronny Lopes, Gauthier Rauline, François Fourchet and Alexandre Hardy in Sports Health