Abstract
Objectives:
The aim of this study was to evaluate the prevalence of bifid mandibular canal (BMC) using cone-beam computed tomography (CBCT) and panoramic images through meta-analysis.
Methods:
Databases of Scopus, PubMed, and Web of Science were searched to find the relevant studies. Studies the met the inclusion criteria were selected. Variables of prevalence, side, length and diameter of BMC and sex were assessed. Data was analyzed using STATA software version 17.
Results:
Of the 1164 articles initially selected, 36 were enrolled. A total of 38077 patients were considered. The overall prevalence of BMC was 18.0%. Studies that evaluated CBCT images reported higher prevalence of BMC compared to panoramic images (25.0% vs 3.0%). The prevalence of BMC was higher in men than women and slightly higher in right side than the left side of the jaw, but none of those differences were significant.
Conclusion:
The results have shown a total prevalence of 18.0% for BMC. Detection power of CBCT images were higher than panoramics. There was no significant relation between prevalence of BMC with sex or side of the jaw.
Key Words: Bifid mandibular canal, CBCT, Oral surgery, Panoramic, Systematic review
INTRODUCTION
Mandibular canal (MC) is located bilaterally in the mandibular bone 1. This canal begins in the mandibular foremen in the lingual region and passes through the mandibular angle and leads to the mental foremen. This canal that passes obliquely through the whole mandibular body and bends anterior-posteriorly, contains the inferior alveolar neurovascular bundles 2, 3. Knowing the location and the shape of the MC is crucial for performing surgical procedures on the lower jaw like placing dental implants, osteotomy, tooth extraction or orthognathic surgery 4, 5. Although there is often only one MC on each side of the mandible, different anatomical variations have been observed 6-9.
Most often, the MC is identifiable as a single duct. However, in certain cases, one or more lateral canals may be observed 2. The bifid mandibular canal (BMC) is an anatomical variation found in the ramus or mandibular body, where the MC divides into two branches, and each canal may contain a distinct neurovascular bundle 10. In 1996, Chávez-Lomeli et al. proposed that three different inferior dental nerves fuse together during embryonic maturation to form a single nerve 11. Thus, when the fusion of these three nerves is incomplete, the MCs become bifid and trifid 12. Awareness of the anatomical variations of the MC is of great clinical importance; because it can be helpful in preventing complications from trauma to the BMC during surgery. Traumatic neuroma, paresthesia, anesthesia, bleeding, and bruising are all possible complications 5, 8, 13.
Wide differences have been observed in the results of studies regarding issues such as the prevalence, route, and length of BMCs, which may have been due to the differences in race, sample size, image quality, and interpretation of the researchers14. The prevalence of BMC in studies examining panoramic images has been reported from 0.08% to 0.95%15-17. Detection of the MC and its variations using panoramic radiography may be difficult due to ghost images formed by the superimposition of adjacent and opposite structures of the mandible 6, 8, 18. Due to the limitations of panoramic radiography, the prevalence reported by previous studies may have been lower than the actual value 8. Because in the studies that examined CBCT images, the prevalence of BMC was reported from 9.8% to 65% in CBCT images 4, 8, 18-20.
Despite the importance of correct diagnosis of MC anatomical variations in order to avoid clinical complications, the scope of these variations are not well known yet. Because there is only one systematic review published on this topic 4, the aim of this review was to assess BMC frequency.
METHODS
This systematic review was reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses checklist 21. In addition, this systematic review protocol was completed and registered at the International Prospective Register of Systematic Reviews (PROSPERO CRD42021293310).
Eligibility criteria
The authors selected articles in which the major goal was to assess the anatomical differences of the mandibular canal in humans utilizing evaluation of panoramic, CT, or CBCT images. This research looked at studies that were published in Persian and English. The following articles were excluded: reviews, case reports, editorials, guidelines, letter to the editors, and abstracts from conferences; studies in which the sample included subjects with pathologies in the area around the mandibular nerve, craniofacial syndrome, or previous orthognathic or craniofacial surgery, because these may affect the shape and the mandibular canal, as well as the surrounding bone structures; studies that evaluated other imaging methods such as micro-CT and angiography; studies that evaluated other imaging methods such as micro-CT and angiography; and studies that evaluated in vivo, cadavers or dry skulls 4.
Information sources and search
PubMed, Scopus, and Web of Science were used to create detailed unique search techniques for each of the electronic databases. Any further references that were overlooked in the electronic database searches were manually sought in the reference lists of the selected papers. From their inception till 20 January 2022, all searches were made in the databases. Duplicate hits were deleted using the EndNote Basic® software (Thompson Reuters, New York, NY). With the help of a health sciences librarian, appropriate truncation and word combinations were chosen and altered for each database search ((“bifid” AND “mandibular” AND (“canal” OR “canals”)) OR (“bifid” AND “mandibular” AND (“nerve” OR “nerves”)) OR (“inferior” AND “alveolar” AND “nerve” AND “branch”) OR (“inferior” AND “alveolar” AND “nerve” AND “segmentation”)).
Study selection
First, two writers (MA and ME) independently assessed all articles’ titles and abstracts. Any articles that did not appear to fit the criteria for inclusion were discarded. Then, full texts were evaluated and screened separately. Disagreements were settled through conversation. When the first two reviewers couldn’t come to an agreement, a third author (AE) was brought in to make the final choice.
Data collection process and data items
Study information (authors, year of publication, and country), sample characteristics (size, gender), diagnostic assessment methods (panoramic, CT, or CBCT), and outcome variables (frequency, sides, mean length, mean diameter) were retrieved from the selected studies by one author (IM). A second author (AM) double-checked all of the information that had been retrieved. Any mistyping was rectified through discussion once more, and a third author (AE) was brought in to make the final decision.
Risk of bias in individual studies
The Meta Analysis of Statistics Assessment and Review Instrument was used to assess the methodology of chosen papers. Two authors (IM and AM) independently examined the quality of each included study by scoring each data item as “yes”, “no”, “unclear” or “not applicable”. Any disagreements between the writers were handled by the third author (AE).
Statistical analysis
A random effect technique was used to derive pooled estimates of bifid prevalence rate and 95% confidence intervals (CIs) overall and by subgroup (CBCT and panoramic). The inverse of the variance of log prevalence was used to weight the studies. The binomial distribution was used to calculate the standard error in each study. The precise binomial and score tests were used to calculate CIs for the original data using STATA’s metaprop program. Because the prevalence rate as a proportion is always a positive figure, and asymmetry in the funnel plot is not related to publication bias, it was not analyzed. The Chi square test and the I2 statistic were used to measure studies’ heterogeneity. The I2 statistic was used to classify heterogeneity: less than 25% indicated a low level of heterogeneity, 25–50% suggested a moderate level, and more than 50% indicated a high one 22. The data were presented using forest plots with a 95% CI by treatment group (CBCT and panoramic). The metareg package in STATA was used to conduct subgroup analysis by group (CBCT and panoramic) and meta-regression analysis including the following covariates: number of sample, year of data collection, mean length of bifid canal, and mean diameter of bifid canal to investigate the main factors influencing prevalence estimation and sources of heterogeneity. Data was analyzed using STATA version 17 (Stata Corporation, College Station, TX, USA) and MedCalc (MedCalc, Ostend, Belgium) software. Statistical significance was defined as a P-value of less than 0.05.
RESULTS
Study Selection
Of the 1164 articles that were initially selected, 433 were duplicate and were excluded. After screening the titles and abstracts, out of the remaining 731 articles, 130 articles were found relevant. In the next phase, according to the exclusion criteria, 98 studies were excluded and finally 36 articles were included in the study. Of these 36 articles, 2 were in Persian and 34 were in English. Study selection process is shown in Figure 1.
Figure 1.
Prisma flow diagram
Study Characteristics
In 36 studies examining the prevalence of BMC included in this systematic review, a total of 38077 patients were considered in these studies and the average number of patients in each study was 1058 patients. The sample size in these studies ranged from 61 23 to 5000 24. These studies were conducted in 17 different countries and the frequency of distribution of these countries were Brazil 4 (11.11%), Iran 4 (11.11%), Turkey 4 (11.11%), China 3 (8.33%), Taiwan 3 (8.33% ), Chile 2 (5.56%), United Kingdom 2 (5.56%), Germany 2 (5.56%), India 2 (5.56%), Korea 2 (5.56%), USA 2 (5.56%), Croatia 1 (2.78%), Egypt 1 (2.78%), Italy 1 (2.78%), Japan 1 (2.78%), Syria 1 (2.78%), and Yemen 1 (2.78%). All of these articles were published in English. Of the 36 studies that examined the prevalence of BMC, 27 examined CBCT studies and 9 panoramic studies.
In addition, the prevalence of BMC based on side, sex, mean length, and mean diameter can be seen in the Table 1. Side was evaluated in 20 studies, gender in 21, mean length in 10, and mean diameter in 11. The mean length was reported from 7.1 to 16.9 mm, and the mean diameter from 0.9 to 2.26 mm. According to the results, the prevalence of BMC on the right and left sides and also between men and women was not statistically significant.
Table 1.
Prevalence of BMC based on side, sex, mean length, and mean diameter
| Variable | Number of studies | Values | P-value* | |
|---|---|---|---|---|
| Side | Left | 20 | 0.48 † | 0.916 |
| Right | 20 | 0.52 † | ||
| Gender | Men | 21 | 0.514 † | 0.931 |
| Women | 21 | 0.486 † | ||
| Mean length | 10 | 12.38 ± 2.92 ‡ | - | |
| Mean diameter | 11 | 1.64 ± 0.46 ‡ | - | |
† Proportion
‡ Mean ± SD (mm)
* Significant at < 0.05
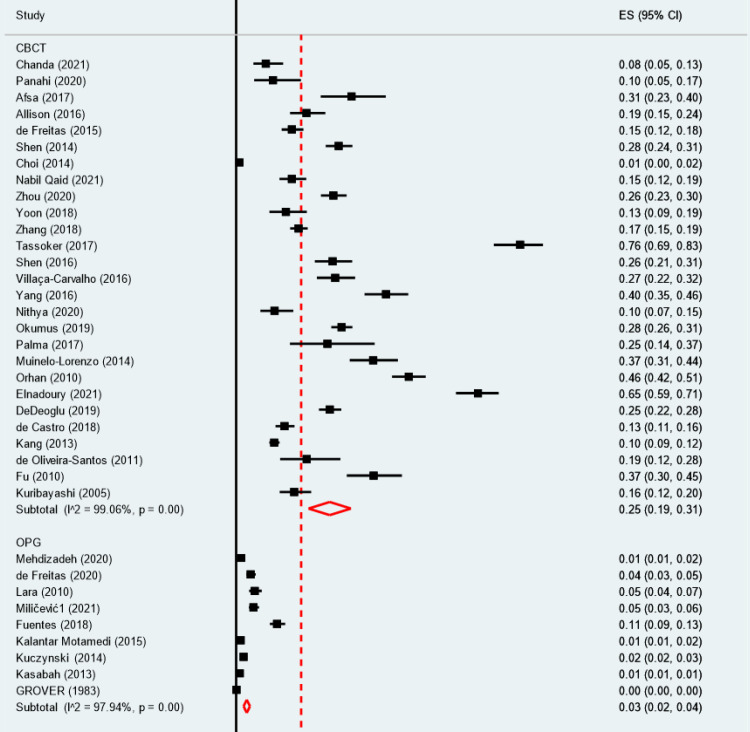
Results of Individual Studies
According to the studies, the lowest and highest prevalence of BMC was related to Grover and Lorton’s study in the United States 24 and Tassoker and Sener’s in Turkey 25 with a prevalence of 0.08% and 76.47%, respectively. In addition, the overall prevalence of BMC was 18.0% (with a 95% CI of 16.0, 19.0). Aggregated prevalence according to CBCT group was 25.0% (with 95% CI of 19.0, 31.0) and according to panoramic group was 3.0% (with 95% CI of 2.0, 4.0). Heterogeneity index was 99.23%, which shows that 99.23% of the differences observed between different studies are due to heterogeneity of studies, and therefore the Random Effect model was used (Table 2).
Table 2.
Estimated prevalence of BMC in CBCT and panoramic studies
| 1st author (year) (reference) | ES | [95% Confidence Interval] | I2 | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| CBCT | Chanda (2021) 34 | 0.08 | 0.05 | 0.13 | |
| Elnadoury (2021) 35 | 0.65 | 0.59 | 0.71 | ||
| Qaid (2021) 36 | 0.15 | 0.12 | 0.19 | ||
| DeDeoglu (2020) 37 | 0.25 | 0.22 | 0.28 | ||
| Nithya (2020) 38 | 0.10 | 0.07 | 0.15 | ||
| Panahi (2020) 39 | 0.10 | 0.05 | 0.17 | ||
| Zhou (2020) 33 | 0.26 | 0.23 | 0.30 | ||
| Okumus (2019) 12 | 0.28 | 0.26 | 0.31 | ||
| de Castro (2018) 40 | 0.13 | 0.11 | 0.16 | ||
| Yoon (2018) 41 | 0.13 | 0.09 | 0.19 | ||
| Zhang (2018) 14 | 0.17 | 0.15 | 0.19 | ||
| Afsa (2017) 42 | 0.31 | 0.23 | 0.40 | ||
| Palma (2017) 23 | 0.25 | 0.14 | 0.37 | ||
| Tassoker (2017) 25 | 0.76 | 0.69 | 0.83 | ||
| Yang (2017) 43 | 0.40 | 0.35 | 0.46 | ||
| Allison (2016) 44 | 0.19 | 0.15 | 0.24 | ||
| Shen (2016) 45 | 0.26 | 0.21 | 0.31 | ||
| Villaça-Carvalho (2016) 46 | 0.27 | 0.22 | 0.32 | ||
| de Freitas (2015) 47 | 0.15 | 0.12 | 0.18 | ||
| Choi (2014) 48 | 0.01 | 0.00 | 0.02 | ||
| Muinelo-Lorenzo (2014) 13 | 0.37 | 0.31 | 0.44 | ||
| Shen (2014) 49 | 0.28 | 0.24 | 0.31 | ||
| Kang (2013) 8 | 0.10 | 0.09 | 0.12 | ||
| de Oliveira-Santos (2012) 17 | 0.19 | 0.12 | 0.28 | ||
| Fu (2010) 15 | 0.37 | 0.30 | 0.45 | ||
| Kuribayashi (2010) 50 | 0.16 | 0.12 | 0.20 | ||
| Orhan (2010) 6 | 0.46 | 0.42 | 0.51 | ||
| Sub-total | Random pooled ES | 0.25 | 0.19 | 0.31 | 99.06% |
| Panoramic | Miličević (2021) 51 | 0.05 | 0.03 | 0.06 | |
| Mehdizadeh (2020) 52 | 0.01 | 0.01 | 0.02 | ||
| de Freitas (2020) 2 | 0.04 | 0.03 | 0.05 | ||
| Fuentes (2019) 1 | 0.11 | 0.09 | 0.13 | ||
| Kalantar Motamedi (2015) 53 | 0.01 | 0.01 | 0.02 | ||
| Kuczynski (2014) 3 | 0.02 | 0.02 | 0.03 | ||
| Kasabah (2013) 54 | 0.01 | 0.01 | 0.01 | ||
| Lara (2010) 55 | 0.05 | 0.04 | 0.07 | ||
| Grover (1983) 24 | 0.0008 | 0.0002 | 0.001 | ||
| Sub-total | Random pooled ES | 0.03 | 0.02 | 0.04 | 97.94% |
| Overall | Random pooled ES | 0.18 | 0.16 | 0.19 | 99.23% |
The forest plot diagram of the aggregated prevalence of BMC categorized into CBCT and panoramic groups and also as a whole, is shown in Figure 2. The midpoint of each line segment estimates the prevalence percentage and length of line segments indicates a 95% prevalence interval in each study. The rhombus symbol indicates the prevalence of BMC in general and separately for CBCT and panoramic.
Figure 2.
Forest plot diagram of aggregated prevalence of BMC in two groups of CBCT and panoramic
DISCUSSION
The differences and variations in the shape of the MC are very important for maxillofacial surgeons, especially during osteotomy surgeries 26. Inferior alveolar nerve (IAN) block is the most common and important injection method in dentistry. But unfortunately, the probability of failure, even with the correct injection is very high (about 15-20%) 27. The failure of mandibular anesthesia can be attributed to the high density of the alveolar plate, limited access to the IAN, the anatomical diversity of this area, and the presence of additional nerves adjacent to the mandibular teeth 28. Therefore, although the presence of unilateral or bilateral mandibular bifid canals is very rare, it is important to diagnose this anatomical condition before mandibular surgeries 29.The studies included in this study were from a total of 17 countries, most of which are related to Iran, Brazil and Turkey. In general, the prevalence of BMC was 18% among all of the studies, with the lowest and highest prevalence of BMC related to studies of Grover from the United States 24 and Tassoker from Turkey 25 with a prevalence of 0.08% and 76.47%, respectively. The reason for this difference could be due to differences in the statistical population and racial effects on anatomical indicators such as BMC.
The mandibular dental canal is of special biological importance as part of the mandible, which contains neurovascular bundles. It is essential to have sufficient information about the route, topography and variations observed in radiography 30. Knowing the length of the canal and especially its location in different parts of the path and knowing the main points of change in direction of the canal helps dentists in recognizing high risk areas. This issue is especially important in oral surgeries, endodontic procedures, placement of dental implants, etc. 31, 32. It was found in this meta-analysis that the mean length of BMC was 12.38 ± 2.92 mm and the mean diameter of the BMC was 1.64 ± 0.46 mm. The lowest length of BMC was reported in the study of Muinelo-Lorenzo et al. 13 with a mean of 7.1 ± 3.7 and the highest value of this parameter was reported 14.1 mm (standard deviation not reported) in the study of Orhan et al. 6. The lowest diameter of BMC was related to the study of Fu et al. 15 with a mean of 0.9 mm (standard deviation not reported) and the highest value of this parameter was 2.26 mm (standard deviation was not reported) to Zhou et al. 33.The overall prevalence of BMC in the studies that evaluated CBCT images was 25%, which is higher than studies that evaluated panoramic radiographs. This difference can be due to two reasons. The first reason is the difference in the nature of radiographs, including the dimension, resolution and measurement accuracy. The second reason is the difference in the number of articles studied (27 articles used CBCT method and 9 articles used panoramic method). Before performing any surgery, it is very important to pay attention to the anatomical structures of the operation area and determine their exact position. By providing appropriate radiography of the patient and determining the location of these structures, the occurrence of complications during and after surgery is significantly reduced. Diagnosis of a disease based on its radiographic image requires accurate knowledge of radiographic signs and natural structures. This diagnosis cannot be made without considering the variations and changes in natural anatomical structures 5, 8.
In a meta-analysis study by Haas et al. 4 , the mean prevalence of bifid and retromolar canals was generally 4.2%, which is almost similar to the present study. Also, the prevalence of these canals on CBCT radiography was 16.25%, which is slightly lower than the present study. This difference could be due to the aggregation of data related to two variations of bifid and retromolar canals.
One of the limitations of this study, which is related to the nature of meta-analysis studies, is the lack of access to all studies performed in this scope.
CONCLUSION
The prevalence of BMC is higher in men than women and this rate is slightly higher on the right than the left side of the mandible, none of which was statistically significant. The total prevalence of bifid canal was 18%, detected 25% in CBCT images and 3% in panoramic images.
DATA AVAILABILITY
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
FUNDING STATEMENT
This systematic review did not have any funding resources.
CONFLICT OF INTEREST
The authors declare no conflicts of interest regarding publication of this paper.
ACKNOWLEDGEMENTS
The authors would like thank the Student Research Committee of Mashhad University of Medical Sciences for their financial support of this project.
References
- 1.Fuentes R, Arias A, Farfán C, et al. Morphological variations of the mandibular canal in digital panoramic radiographs: a retrospective study in a Chilean population. J Korean Assoc Oral Maxillofac Surg. 2019;78(1):163–70. doi: 10.5603/FM.a2018.0058. [DOI] [PubMed] [Google Scholar]
- 2.de Freitas GB, de Morais Silva PG, dos Santos JA, Júnior LRCM, Bernardon P. Prevalence and classification of anatomical variations of mandibular canal in panoramic radiographies. J Health Sci. 2020;10(2):133–8. [Google Scholar]
- 3.Kuczynski A, Kucharski W, Franco A, Westphalen FH, de Lima AAS, Fernandes Â. Prevalence of bifid mandibular canals in panoramic radiographs: a maxillofacial surgical scope. Surg Radiol Anat. 2014;36(9):847–50. doi: 10.1007/s00276-014-1298-2. [DOI] [PubMed] [Google Scholar]
- 4.Haas LF, Dutra K, Porporatti AL, et al. Anatomical variations of mandibular canal detected by panoramic radiography and CT: a systematic review and meta-analysis. Dentomaxillofac Radiol. 2016;45(2):20150310. doi: 10.1259/dmfr.20150310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Öztürk A, Tayman A, Potluri A. Observation of double mandibular canals and types of bifid canals in dry skulls. Balk J Dent Med. 2020;24(2):107–12. [Google Scholar]
- 6.Orhan K, Aksoy S, Bilecenoglu B, Sakul BU, Paksoy CS. Evaluation of bifid mandibular canals with cone-beam computed tomography in a Turkish adult population: a retrospective study. Surg Radiol Anat. 2011 Aug;33(6):501–7. doi: 10.1007/s00276-010-0761-y. [DOI] [PubMed] [Google Scholar]
- 7.Rashsuren O, Choi J-W, Han W-J, Kim E-K. Assessment of bifid and trifid mandibular canals using cone-beam computed tomography. Imaging Sci Dent. 2014;44(3):229–36. doi: 10.5624/isd.2014.44.3.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kang J-H, Lee K-S, Oh M-G, et al. The incidence and configuration of the bifid mandibular canal in Koreans by using cone-beam computed tomography. Imaging Sci Dent. 2014;44(1):53–60. doi: 10.5624/isd.2014.44.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Correr GM, Iwanko D, Leonardi DP, Ulbrich LM, Araujo MRd, Deliberador TM. Classification of bifid mandibular canals using cone beam computed tomography. Braz Oral Res. 2013;27:510–6. doi: 10.1590/S1806-83242013000600011. [DOI] [PubMed] [Google Scholar]
- 10.Naitoh M, Hiraiwa Y, Aimiya H, et al. Bifid mandibular canal in Japanese. Implant Dent. 2007 Mar;16(1):24–32. doi: 10.1097/ID.0b013e3180312323. [DOI] [PubMed] [Google Scholar]
- 11.Chávez-Lomeli M, Mansilla Lory J, Pompa J, Kjaer I. The human mandibular canal arises from three separate canals innervating different tooth groups. J Dent Res. 1996;75(8):1540–4. doi: 10.1177/00220345960750080401. [DOI] [PubMed] [Google Scholar]
- 12.Okumuş Ö, Dumlu A. Prevalence of bifid mandibular canal according to gender, type and side. J Dent Sci. 2019 Jun;14(2):126–33. doi: 10.1016/j.jds.2019.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Muinelo-Lorenzo J, Suárez-Quintanilla J, Fernández-Alonso A, Marsillas-Rascado S, Suárez-Cunqueiro M. Descriptive study of the bifid mandibular canals and retromolar foramina: cone beam CT vs panoramic radiography. Dentomaxillofac Radiol. 2014;43(5):20140090. doi: 10.1259/dmfr.20140090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang Y-Q, Zhao Y-N, Liu D-G, Meng Y, Ma X-C. Bifid variations of the mandibular canal: cone beam computed tomography evaluation of 1000 Northern Chinese patients. Oral Surg Oral Med Oral Pathol Oral Radiol. 2018;126(5):271–8. doi: 10.1016/j.oooo.2018.06.008. [DOI] [PubMed] [Google Scholar]
- 15.Fu E, Peng M, Chiang CY, Tu HP, Lin YS, Shen EC. Bifid mandibular canals and the factors associated with their presence: a medical computed tomography evaluation in a Taiwanese population. Clin Oral Implants Res. 2014 Feb;25(2):64–7. doi: 10.1111/clr.12049. [DOI] [PubMed] [Google Scholar]
- 16.Kim M, Yoon S, Park H, et al. A false presence of bifid mandibular canals in panoramic radiographs. Dentomaxillofac Radiol. 2011;40(7):434–8. doi: 10.1259/dmfr/87414410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.de Oliveira-Santos C, Souza PHC, de Azambuja Berti-Couto S, et al. Assessment of variations of the mandibular canal through cone beam computed tomography. Clin Oral Investig. 2012;16(2):387–93. doi: 10.1007/s00784-011-0544-9. [DOI] [PubMed] [Google Scholar]
- 18.Naitoh M, Hiraiwa Y, Aimiya H, Ariji E. Observation of bifid mandibular canal using cone-beam computerized tomography. Int J Oral Maxillofac Implants. 2009 Jan-Feb;24(1):155–9. [PubMed] [Google Scholar]
- 19.Karamifar K, Shahidi S, Tondari A. Bilateral bifid mandibular canal: report of two cases. Indian J Dent Res. 2009;20(2):235–7. doi: 10.4103/0970-9290.52889. [DOI] [PubMed] [Google Scholar]
- 20.Neves FS, Nascimento MCC, Oliveira ML, Almeida SM, Bóscolo FN. Comparative analysis of mandibular anatomical variations between panoramic radiography and cone beam computed tomography. Oral Maxillofac Surg. 2014;18(4):419–24. doi: 10.1007/s10006-013-0428-z. [DOI] [PubMed] [Google Scholar]
- 21.Moher D, Liberati A, Tetzlaff J, Altman D. Reprint-preferred reporting items for systematic reviews and met-analyses: the PRISMA statemet. Phys Ther. 2009;89:873–80. [PubMed] [Google Scholar]
- 22.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta‐analysis. Stat Med. 2002;21(11):1539–58. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 23.Palma LF, Buck AF, Kfouri F, Blachman IT, Lombardi LA, Cavalli MA. Evaluation of retromolar canals on cone beam computerized tomography scans and digital panoramic radiographs. Oral Maxillofac Surg. 2017 Sep;21(3):307–12. doi: 10.1007/s10006-017-0632-3. [DOI] [PubMed] [Google Scholar]
- 24.Grover PS, Lorton L. Bifid Mandibular Nerve as a Possible Cause of Inadequate Anesthesia in the Mandible. J Oral Maxillofac Surg. 1983;41(3):177–9. doi: 10.1016/0278-2391(83)90076-9. [DOI] [PubMed] [Google Scholar]
- 25.Tassoker M, Sener S. Investigation of the Prevalence of Retromolar Canals: A Cone Beam CT Study. Int J Morphol. 2017 Dec;35(4):1298–302. [Google Scholar]
- 26.Genc T, Duruel O, Kutlu HB, Dursun E, Karabulut E, Tözüm T. Evaluation of anatomical structures and variations in the maxilla and the mandible before dental implant treatment. Dent Med Probl. 2018;55(3):233–40. doi: 10.17219/dmp/94303. [DOI] [PubMed] [Google Scholar]
- 27.Shahi S, Rahimi S, Yavari HR, Ghasemi N, Ahmadi F. Success Rate of 3 Injection Methods with Articaine for Mandibular First Molars with Symptomatic Irreversible Pulpitis: A CONSORT Randomized Double-blind Clinical Trial. J Endod. 2018;44(10):1462–6. doi: 10.1016/j.joen.2018.07.010. [DOI] [PubMed] [Google Scholar]
- 28.Aggarwal V, Singla M, Miglani S, Kohli S. Comparative evaluation of mental incisal nerve block, inferior alveolar nerve block, and their combination on the anesthetic success rate in symptomatic mandibular premolars: a randomized double-blind clinical trial. J Endod. 2016;42(6):843–5. doi: 10.1016/j.joen.2016.02.015. [DOI] [PubMed] [Google Scholar]
- 29.Rouas P, Nancy J, Bar D. Identification of double mandibular canals: literature review and three case reports with CT scans and cone beam CT. Dentomaxillofac Radiol. 2007;36(1):34–8. doi: 10.1259/dmfr/27374727. [DOI] [PubMed] [Google Scholar]
- 30.Bogdán S, Huszar T, Joób AF, Németh Z, Pataky L, Barabás J. The clinical importance of the mandibular canal course variations. Fogorvosi szemle. 2006;99(4):169–73. [PubMed] [Google Scholar]
- 31.Güler A, Sumer M, Sumer P, Biçer I. The evaluation of vertical heights of maxillary and mandibular bones and the location of anatomic landmarks in panoramic radiographs of edentulous patients for implant dentistry. J Oral Rehabil. 2005;32(10):741–6. doi: 10.1111/j.1365-2842.2005.01499.x. [DOI] [PubMed] [Google Scholar]
- 32.Gomes ACA, do Egito Vasconcelos BC, de Oliveira Silva ED, de França Caldas Jr A, Neto ICP. Sensitivity and specificity of pantomography to predict inferior alveolar nerve damage during extraction of impacted lower third molars. J Oral Maxillofac Surg. 2008;66(2):256–9. doi: 10.1016/j.joms.2007.08.020. [DOI] [PubMed] [Google Scholar]
- 33.Zhou X, Gao X, Zhang J. Bifid mandibular canals: CBCT assessment and macroscopic observation. Surg Radiol Anat. 2020 Sep;42(9):1073–9. doi: 10.1007/s00276-020-02489-5. [DOI] [PubMed] [Google Scholar]
- 34.Chanda S, Manoj R, Ramaswami E, Santosh V, Waghmare M, Vahanwala S. Anatomical variations of mandibular canal using cone-beam computed tomography-A retrospective study. J Indian Acad Oral Med Radiol. 2021 Apr-Jun;33(2):183–8. [Google Scholar]
- 35.Elnadoury EA, Gaweesh YSE, Abu El Sadat SM, Anwar SK. Prevalence of bifid and trifid mandibular canals with unusual patterns of nerve branching using cone beam computed tomography. Odontology. 2021 Jul;:110:203–11. doi: 10.1007/s10266-021-00638-9. [DOI] [PubMed] [Google Scholar]
- 36.Qaid N, Aldilami A, Al-Jawfi K, Shamala A. Prevalence and morphological assessment of bifid mandibular canal using cone beam computed tomography among a group of yemeni adults. J Indian Acad Oral Med Radiol. 2021;33(3):242–7. [Google Scholar]
- 37.Dedeoglu N, Duman SB. Prevalence of Bifid Mandibular Canals in Turkish Eastern Anatolia Population: A Retrospective Study. J Clin Diagn Res. 2020 Feb;14(2):13–7. [Google Scholar]
- 38.Nithya J, Aswath N. Assessing the Prevalence and Morphological Characteristics of Bifid Mandibular Canal Using Cone-Beam Computed Tomography - A Retrospective Cross-Sectional Study. J Clin Imaging Sci. 2020;10:30. doi: 10.25259/JCIS_67_2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Panahi S, Moradi Seifabad Z, Sabz G. Frequency of Bifid Mandibular Canals and it’s Relationship with Third Molar Teeth in Cone Beam Computed Tomography (CBTT) Armaghane Danesh. 2020;25(2):256–63. [Google Scholar]
- 40.de Castro MAA, Barra SG, Vich MOL, Abreu MHG, Mesquita RA. Mandibular canal branching assessed with cone beam computed tomography. La radiologia medica. 2018;123(8):601–8. doi: 10.1007/s11547-018-0886-3. [DOI] [PubMed] [Google Scholar]
- 41.Yoon TYH, Robinson DK, Estrin NE, Tagg DT, Michaud RA, Dinh TN. Utilization of cone beam computed tomography to determine the prevalence and anatomical characteristics of bifurcated inferior alveolar nerves. Gen Dent. 2018 Jul-Aug;66(4):22–6. [PubMed] [Google Scholar]
- 42.Afsa M, Rahmati H. Branching of mandibular canal on cone beam computed tomography images. Singapore Dent J. 2017;38:21–5. doi: 10.1016/j.sdj.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 43.Yang X, Lyu C, Zou D. Bifid Mandibular Canals Incidence and Anatomical Variations in the Population of Shanghai Area by Cone Beam Computed Tomography. J Comput Assist Tomogr. 2017 Jul/Aug;41(4):535–40. doi: 10.1097/RCT.0000000000000561. [DOI] [PubMed] [Google Scholar]
- 44.Allison JR, Carr A. A prevalence study of bifid mandibular canals using cone beam computed tomography. Oral Surg. 2017;10(4):55–61. [Google Scholar]
- 45.Shen EC, Fu E, Peng M, Hsieh YD, Tu HP, Fu MW. Bifid mandibular canals and their cortex thicknesses: A comparison study on images obtained from cone-beam and multislice computed tomography. J Dent Sci. 2016 Jun;11(2):170–4. doi: 10.1016/j.jds.2016.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Villaça-Carvalho MF, Manhães LR Jr, de Moraes ME, Lopes SL. Prevalence of bifid mandibular canals by cone beam computed tomography. Oral Maxillofac Surg. 2016 Sep;20(3):289–94. doi: 10.1007/s10006-016-0569-y. [DOI] [PubMed] [Google Scholar]
- 47.de Freitas GB, de Freitas e Silva A, Morais LA, Felippe Silva MB, da Silva TCG, Manhães Júnior LRC. Incidence and classification of bifid mandibular canals using cone beam computed tomography. Braz J Oral Sci. 2015;14(4):294–8. [Google Scholar]
- 48.Choi Y-Y, Han S-S. Double mandibular foramen leading to the accessory canal on the mandibular ramus. Surg Radiol Anat. 2014;36(9):851–5. doi: 10.1007/s00276-014-1310-x. [DOI] [PubMed] [Google Scholar]
- 49.Shen E-C, Fu E, Ming-Jen Fu M, Peng M. Configuration and corticalization of the mandibular bifid canal in a Taiwanese adult population: a computed tomography study. Int J Oral Maxillofac Implants. 2014;29(4):893–7. doi: 10.11607/jomi.3435. [DOI] [PubMed] [Google Scholar]
- 50.Kuribayashi A, Watanabe H, Imaizumi A, Tantanapornkul W, Katakami K, Kurabayashi T. Bifid mandibular canals: cone beam computed tomography evaluation. Dentomaxillofac Radiol. 2010 May;39(4):235–9. doi: 10.1259/dmfr/66254780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Miličević A, Salarić I, Đanić P, et al. Anatomical Variations of the Bifid Mandibular Canal on Panoramic Radiographs in Citizens from Zagreb, Croatia. Acta Stomatol Croat. 2021 Sep;55(3):248–55. doi: 10.15644/asc55/3/2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mehdizadeh M, Nateghi N, Vahedian M, Biuki N. Prevalence of Different Types of the Bifid Mandibular Canal and its Relationship with the Position and Width of the Main Canal in the Panoramic Radiographs. Qom Univ Med Sci J. 2020;14(7):12–8. [Google Scholar]
- 53.Kalantar Motamedi MH, Navi F, Sarabi N. Bifid mandibular canals: prevalence and implications. J Oral Maxillofac Surg. 2015 Mar;73(3):387–90. doi: 10.1016/j.joms.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 54.Kasabah S, Modellel Y. Classification of bifid mandibular canals in the Syrian population using panoramic radiographs. Clin Anat. 2014 Jan;:19 Suppl 3:178–83. [PubMed] [Google Scholar]
- 55.Lara JS, Quezada AS, Valenzuela JSP, Schilling L, Schilling Q, San Pedro V. Mandibular canal duplication prevalence, digital panoramic radiography analysis. Int J Odontostomatol. 2010;4:207–13. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.