Abstract
BACKGROUND
Lumbosacral transitional vertebrae (LSTVs) are congenital anomalies that occur in the spinal segments of L5–S1. These vertebrae result from sacralization of the lowermost lumbar segment or lumbarization of the uppermost sacral segment. When the lowest lumbar vertebra fuses or forms a false joint with the sacrum (pseudoarticulation), it can cause pain and manifest clinically as Bertolotti syndrome.
OBSERVATIONS
A 36-year-old female presented with severe right-sided low-back pain. Computed tomography was unremarkable except for a right-sided Castellvi type IIA LSTV. The pain proved refractory to physical therapy and lumbar epidural spinal injections, but targeted steroid and bupivacaine injection of the pseudoarticulation led to 2 weeks of complete pain relief. She subsequently underwent minimally invasive resection of the pseudoarticulation, with immediate improvement in her low-back pain. The patient continued to be pain free at the 3-year follow-up.
LESSONS
LSTVs alter the biomechanics of the lumbosacral spine, which can lead to medically refractory mechanical pain requiring surgical intervention. Select patients with Bertolotti syndrome can benefit from operative management, including resection, fusion, or decompression of the pathologic joint.
Keywords: Bertolotti syndrome, lumbosacral transitional vertebrae, anomaly, lumbar spine, sacrum, spine surgery, low-back pain
ABBREVIATIONS: 3D = three-dimensional, CT = computed tomography, LSTV = lumbosacral transitional vertebra, MRI = magnetic resonance imaging, RFA = radiofrequency ablation, SPECT = single-photon emission computed tomography
Lumbosacral transitional vertebrae (LSTVs) are reported to occur in 7% to 30% of the population.1 They are congenital anomalies of the lumbosacral junction that comprise a spectrum of pathologies varying from complete sacralization of the lowermost lumbar vertebra to complete lumbarization of the uppermost sacral segment.2 These anomalies have been previously classified by Castellvi and colleagues3 according to morphology and risk of disc herniation at the transitional or cephalad segment (Fig. 1). Prior retrospective data have suggested Castellvi class IA LSTV to be the most prevalent (approximately 15% of patients with LSTV); this category is distinguished by an enlarged lumbar transverse process.4 Progressively higher Castellvi grades denote more intimate association with the sacral alae, with type II lesions having unilateral (IIA) or bilateral (IIB) pseudoarticulation, type III lesions showing complete fusion to the sacrum on one (IIIA) or both (IIIB) sides, and type IV showing pseudoarticulation on one side and full fusion with the sacral ala on the other.1–4
FIG. 1.
Illustration of the Castellvi classification of lumbosacral transitional vertebrae: IA, enlarged L5 transverse process, unilateral; IB, enlarged L5 transverse process, bilateral; IIA, enlarged L5 transverse process contacting sacral ala, forming pseudoarticulation, unilateral; IIB, same as IIA but bilateral; IIIA, enlarged L5 transverse process completely fuses to sacral ala, resembling complete sacralization of L5; IIIB, same as IIIA, but bilateral; IV, unilateral type IIA with a contralateral type IIIA (fusion) on same LSTVs.
The pseudoarticulation/fusion between the L5 transverse process and sacral ala can limit rotation, lateral bending, and flexion/extension movements.4 Such altered biomechanics can in turn create a stress riser in the adjacent level, resulting in mechanical paraxial pain or disc herniation with resultant radicular pain.4 The enlarged L5 transverse process can also cause radicular pain through extraforaminal compression of the exiting root.1,5–7 The confluence of low-back pain and/or radiculopathy in the setting of an LSTV is known as Bertolotti syndrome. Similar to most spinal pathologies, conservative management is considered first-line treatment.8 In a subset of patients, conservative management is insufficient and resection of the pseudoarticulation can be helpful. In the present case, we illustrate the clinical utility of minimally invasive resection of the lumbosacral articulation in a patient with Bertolotti syndrome. We additionally review the contemporary literature to highlight the evidentiary support for various operative techniques in the treatment of Bertolotti syndrome.
Illustrative Case
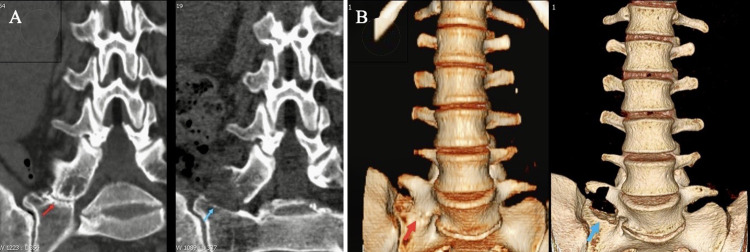
A 36-year-old female presented with persistent, debilitating low-back pain. Lumbar radiographs and computed tomography (CT) were unremarkable except for a right-sided Castellvi type IIA LSTV pseudoarticulation (Fig. 2). Conservative management with physical therapy, lumbar epidural steroid injections, lumbar facet injections, and sacroiliac joint injections provided no improvement in her pain. A combined steroid and bupivacaine injection of the LSTV pseudoarticulation completely relieved her pain for 2 weeks, confirming her diagnosis of Bertolotti syndrome.
FIG. 2.
A: Coronal CT scans with bone windows illustrating widening of the right L5 transverse process with cortical sclerosis of the inferior aspect and pseudoarticulation with the sacral ala (Castellvi type IIA). The patient presented with significant low-back pain (Bertolotti syndrome) refractory to conservative management and was offered surgical intervention, which included resection of the anomalous transverse process. B: 3D reconstructions of CT illustrating removal/drilling out of the superior sacral alae and inferior right L5 transverse process in the region of the pseudoarticulation.
The patient subsequently underwent resection of the right-sided LSTV pseudoarticulation through a tubular retractor with the assistance of intraoperative image guidance (Fig. 3). Because the main goal of surgery is complete resection of the abnormal pseudoarticulation, intraoperative navigation was exceptionally helpful to ensure this was accomplished. The anatomy of these transitional segments can be confusing, especially if the procedure is performed minimally invasively, and real-time image guidance can keep the surgeon oriented to ensure complete removal of the joint. Although not done in this case, intraoperative CT scanning after resection can also be performed to confirm complete pseudoarticulation resection. The patient was discharged from the hospital on the day of the operation. At the 2-week follow-up, she endorsed near-complete resolution of her presenting low-back pain. At the 3-year postoperative follow-up, she remained completely free of her preoperative back pain.
FIG. 3.

The patient underwent minimally invasive tubular resection of the anomalous transverse process.
Patient Informed Consent
The necessary patient informed consent was obtained in this study.
Discussion
Observations
Here, we present the successful resolution of Bertolotti syndrome in a female in her mid-30s who presented with right Castellvi type IIA pseudoarticulation at the lumbosacral transitional vertebra. Oftentimes, patients with LSTV can be asymptomatic or present with nonspecific low-back pain, as our patient did. This can make the diagnosis challenging, and current diagnostic imaging modalities are subpar in that they will not always demonstrate the presence of any specific pathology. In addition to standard radiography, which is a poor diagnostic modality for LSTV-CT, magnetic resonance imaging (MRI), and single-photon emission computed tomography (SPECT) bone scintigraphy can be used to assess the degenerative changes that may represent the source of a patient’s pain. For example, in a series of 48 patients with Bertolotti syndrome due to Castellvi type II LSTVs, 81% of patients showed increased uptake on SPECT at the site of pseudoarticulation. Although SPECT was not used in the diagnosis and subsequent treatment of our patient, three-dimensional (3D) CT reconstructions aided in the visualization of the pseudoarticulation and planning of the surgical approach. The pseudoarticulation was the only identifiable source of the patient’s pain; therefore, resection of the pseudoarticulation of the bridging transverse process from the LSTV was indicated after conservative treatments had failed. The goal of surgery was to completely decompress the affected neural elements to eliminate the patient’s pain. Resection of the joint provided adequate decompression of the neural elements, as noted by the resolution of the patient’s symptoms at the 3-year follow-up.
Bertolotti syndrome describes the clinical condition of low-back pain in the presence of a lumbosacral pseudoarticulation. The etiology of Bertolotti syndrome is unclear and may be multifactorial in nature. As a result, there is currently no gold standard of care for Bertolotti syndrome, although care generally begins with conservative management.7,9 Surgical intervention may be warranted for refractory cases. To address this, we reviewed the extant literature on the surgical management of Bertolotti syndrome (Table 1).
TABLE 1.
Literature review of studies reporting outcomes of different operative management techniques for the treatment of low back pain in Bertolotti’s syndrome
| Authors & Year | No. of Patients | Mean Age in Yrs (range) | No. of Females/Total | Operative Management (no. of cases) | Pain Outcomes (no. of cases) | Conclusion |
|---|---|---|---|---|---|---|
| Jonsson et al., 198914 |
11 |
39 (13–76) |
6/11 |
LSTV open resection |
Complete resolution (7), significant improvement (2), unchanged from preop levels (2) |
LSTV resection in patients w/ temporary pain relief of lower back pain after anesthetizing joint articulation is worthwhile procedure |
| Santavirta et al., 199316 |
16 |
34 (27–58) |
11/16 |
Posterolat fusion (8), LSTV open resection (8) |
Improvement (10), patients required 2nd operation (6; 3/6 fusions) |
Surgical treatment w/ resection or fusion in Bertolotti’s syndrome should be attempted in select cases that failed conservative management |
| Abe et al., 199717 |
1 |
37 |
0/1 |
Ant decompression w/ resection of bone spur using wide muscle-splitting extraperitoneal approach |
Good relief of low back pain & radiculopathy obtained |
Selective radiculography provided optimal diagnostic value as method of exam for far-out foraminal stenosis; ant approach to decompression of far-out foraminal stenosis below LSTV is simple & effective treatment |
| Brault et al., 200115 |
1 |
17 |
1/1 |
Resection of anomalous lumbosacral articulation |
Symptom free at last FU |
Low back pain may occur from facet contralat to unilat LSTV, even in young patients; resection of anomalous articulation can provide excellent results due to unloading of force on symptomatic facet |
| Ichihara et al., 200420 |
1 |
34 |
1/1 |
Pst decompression by LSTV open resection |
Complete resolution |
Pst decompression is easy, safe, & useful method of treatment for radicular pain caused by a Bertolotti joint when conservative management failed |
| Ugokwe et al., 200823 |
1 |
40 |
0/1 |
Minimally invasive resection of anomalous, enlarged transverse process at caudal-most lumbar vertebra involved in pseudoarticulation at sacral ala |
97% resolution of pain at 6-mo FU |
Minimally invasive approaches can be as effective as conventional approaches to treat LSTV while minimizing trauma associated w/ surgical exposure |
| Miyoshi et al., 201124 |
1 |
29 |
0/1 |
Pst decompression by osteophyte resection |
Complete resolution |
Pst decompression is effective form of management for radicular pain caused by foraminal stenosis secondary to LSTV |
| Weber and Ernestus, 201121 |
1 |
53 |
1/1 |
Lat foraminal & extraforaminal nerve root decompression |
No low back or radicular pain & no radiographic signs of instability at 12 mos |
Extraforminal impingement originating from below transitional vertebra in Castellvi type IIA and IIB can be relieved by lat foraminal & extraforaminal radicular decompression |
| Shibayama et al., 201122 |
1 |
46 |
1/1 |
Extraforaminal decompression of rt L6 nerve root involving removal of lower part of enlarged transverse process & upper part of sacral ala |
At 30-mo FU, VAS score had decreased 10 points; JOA score increased from 10 to 25 |
Clinical presentation of intractable sciatica-like pain could arise from impingement of nerve root extraforaminally by compression caused by transverse process |
| Kikuchi et al., 201318 |
2 |
61.5 (53–70) |
1/2 |
Ant decompression by osteophyte resection |
Complete resolution (2) |
L5 extraforaminal stenosis below LSTV causes nerve entrapment more ant to L5 nerve than in other pathologies, so ant decompression results in more complete decompression |
| Malham et al., 201319 |
2 |
38 (27–49) |
1/2 |
Ant retroperitoneal LSTV resection |
Significant improvement (2) |
Ant approach for pseudoarthrectomy in treatment of Bertolotti’s syndrome is safe & effective approach for long-term symptomatic relief |
| Takata et al., 201425 |
1 |
45 |
1/1 |
Minimally invasive microendoscopic LSTV resection & discectomy |
Complete resolution |
Minimally invasive LSTV resection is effective for treatment of low back pain associated w/ Bertolotti’s syndrome |
| Li et al., 20147 |
7 |
43.3 (26–63) |
4/7 |
Minimally invasive tubular LSTV resection |
Complete resolution (3), improvement (2), initial improvement followed by recurrence (2) |
Minimally invasive surgical approach for LSTV resection is effective for pain resolution in patients w/ Bertolotti’s syndrome w/ pain refractive to conventional therapy |
| Babu et al., 201729 |
2 |
27.5 (17–38) |
2/2 |
LSTV O-arm neuronavigational resection |
Complete resolution (2) |
Excellent outcomes achieved w/ navigation guidance approach to locate & completely resect LSTVs in 2 patients |
| Ju et al., 201726 |
61 |
53 ± 12 |
42/61 |
Combined resection of L5 transverse process & decompression of L4 nerve root |
Average 4.68-point decrease in VAS score across all patients (7.54 preop, 2.86 postop) |
When pain relieved by anesthetic block of pseudoarticulation or selective L4 exiting nerve root, bisectional cutting of base of transverse process of L5 using paraspinal route can be effective treatment for Bertolotti’s |
| Adams et al., 201831 |
1 |
37 |
1/1 |
Nonsegmental pedicle screw instrumentation w/ low-profile screws on rt side w/ fusion using allograft & rh-BMP2 bone graft substitute |
Complete resolution of preop symptoms from rare Castellvi type IV LSTV at 2-wk FU |
Patients w/ symptoms consistent w/ Bertolotti’s syndrome should be considered for surgical treatment even if they have Castellvi type III or IV LSTV |
| Louie et al., 201930 |
2 |
15 (14–16) |
2/2 |
Resection of L5 transverse process |
Pain & functional status improved w/in 6 wks & continued through last FU |
Resection of l5 transverse process fused to sacral ala can reduce pain & improve overall function; even in young patients, surgical intervention should be considered to mitigate yrs of chronic pain & additional degenerative change |
| Mikula et al., 20226 |
27 |
40 ± 16 |
18/27 |
Fusion (9) vs resection (18) |
No statistically significant difference in short-term pain improvement (< 6 mos) btwn fusion & resection groups, but fusion provided superior long-term (> 12 mos) pain improvement |
Patients w/ Bertolotti syndrome who underwent fusion across LSTV had higher rate of long-term pain improvement vs patients who underwent resection of LSTV pseudoarticulation |
| Chang et al., 202232 |
1 |
39 |
0/1 |
Minimally invasive microscopic tubular articular resection w/ C-arm guidance |
Free of pain/symptoms at 2-yr postoperative FU |
Simple resection of pseudoarticulation is most effective surgical treatment in patient w/ degeneration of anomalous articulation or facet joint above LSTV; decompression of nerve root effective for patients w/ radiculopathy who respond to selective nerve root-block procedure; fusion may be indicated when there is coexisting joint instability w/ increased motion |
| Stein et al., 202333 | 1 | 57 | 1/1 | Minimally invasive endoscopic LSTV resection | Sustained improvement | Endoscopic resection of anomalous LSTV is effective treatment for refractory Bertolotti’s syndrome, w/ extensive resection along entire length of LSTV providing more complete pain relief |
ant = anterior; FU = follow-up; pst = posterior; VAS = visual analog scale; JOA = Japanese Orthopedic Association.
Conservative Management
Conservative therapy can include a combination of oral analgesics, physical therapy, and alternative therapies.9 A local anesthetic and steroid injections serve as the next tier in management and can also offer diagnostic guidance.10 As demonstrated in the present case, when injection of the pseudoarticulation results in significant pain relief, the surgeon is provided with reasonable evidence that stabilization or resection of the articulation may lead to long-term benefit. Several other case reports have demonstrated the benefit of pseudoarticulation injection in this patient population. Barkhane et al.11 used lidocaine/triamcinolone acetate injections into the lumbosacral articulations of a 65-year-old male with Castellvi type IIB with robust relief of symptoms continuing through the 6-month follow-up.
Zhang and Cheng12 likewise successfully used targeted injections for the management of five patients presenting with Bertolotti syndrome and Castellvi type II/III malformations. Of the four patients with follow-up, all experienced ≥50% reduction in their pain and were able to continue with nonoperative management.12 Glémarec et al.13 subsequently published confirmatory findings in a comparative study of 15 patients with Bertolotti syndrome who had undergone injection with a lidocaine/corticosteroid combination or saline. Patients in the interventional arm had significantly greater pain relief at the 4- and 12-week follow-up, whereas patients in the placebo group did not.13
As in the present case, injection may fail to provide robust long-term benefit, but the creation of even short-term benefit is diagnostically valuable, as it suggests the pseudoarticulation may be a driver of the chief complaint. Jönsson et al.14 published one of the earliest series showing this, using lidocaine injections in 10 patients with Castellvi type II LSTV and more than 1 year of pain. Patients subsequently underwent resection of the L5 transverse process contributing to the pathologic pseudoarticulation. Of these patients, 8 had pain relief at the last follow-up and 7 were pain free (median follow-up 13 months), leading the authors to recommend transverse process resection as definitive management for patients with Bertolotti syndrome who had shown a response to local anesthesia of the pseudoarticulation.
Although most patients whose condition fails conservative treatment will eventually undergo surgery, another option to consider is radiofrequency ablation (RFA), a minimally invasive technique that can be trialed prior to invasive surgical procedures. Interestingly, it was previously reported that a case refractory to conservative management (including injections) underwent L4–5 facet RFA but experienced only incomplete pain relief. Another injection was trialed, again providing only temporary pain relief. Normally, this would seem to indicate that surgery may be warranted. However, RFA was trialed a second time and proved successful in alleviating the patient’s pain, suggesting that it may represent a potential alternative to surgery for select patients.
Surgical Management: Resection Versus Fusion
For patients whose condition has failed nonoperative management (including a trial of nonopioid analgesics, physical therapy, and/or steroid injections), surgery could lead to significant symptomatic improvement.10 There are two predominant approaches to surgical management for Bertolotti syndrome: fusion of the abnormal segment and resection of the pathologic joint. In the present case, an instance of Castellvi type II disease, similar to the cases reported by Jönsson et al.,14 resection of the pseudoarticulation can result in significant pain relief potentially due to the restoration of lumbosacral junction biomechanics to a seminormal state.15,16 In the present case, the patient had robust symptomatic improvement that was maintained even at the 3-year follow-up.
Other series have looked at pseudoarticulation resection and decompression of the compressed lumbar nerve root in Bertolotti syndrome.7 The basis for this treatment stems from the observation that radiculopathy is the presenting symptom for more than 70% of individuals affected by Bertolotti syndrome, with compression caused by the extraforaminal bulk of the L5-sacroilial pseudoarticulation/fusion mass.8 As mentioned previously, Jönsson et al.14 noted complete pain relief in 70% of their patients who had experienced transient symptom relief after local anesthesia of the pseudoarticulation. Abe et al.17 subsequently described the case of a 37-year-old male with back and left leg pain secondary to extraforaminal stenosis by a Castellvi type IIb pseudoarticulation with associated osteophyte formation compressing the exiting L5 root. The patient underwent a left-sided extraperitoneal approach with resection of the osteophyte; he endorsed complete relief of symptoms through the 1-year follow-up. Kikuchi et al.18 similarly utilized an anterior extraperitoneal approach for L5 root decompression and resection of the L5 transverse process osteophyte in a person with Bertolotti syndrome and a left-sided Castellvi type IIA LSTV. As in the case reported by Abe et al.,17 the patient had complete pain relief through the 1-year follow-up. More recently, Malham et al.19 also utilized an anterior retroperitoneal approach for pseudoarthrectomy and extraforaminal decompression in two patients with medically refractory low-back pain and Castellvi type IIA LSTV. At the 2-year follow-up, both had continued robust pain relief, had returned to work, and were engaged in low impact exercise.19
However, posterior approaches seem to have become increasingly popular relative to anterior approaches, likely due to the familiar positioning and reduced risk of bowel injury. Ichihara et al.19 described their use of a posterior paramedian approach for resection of the pseudoarticulation in a patient with Bertolotti syndrome secondary to a Castellvi type IIB LSTV with left L5 root compression. The patient had robust improvement in pain that continued through the 2-year follow-up. Weber and Ernestus21 and Shibayama et al.22 likewise reported success with open and minimally invasive approaches for extraforaminal decompression of the root, noting continued pain relief at the 1-year and 30-month follow-ups. Similarly Ugokwe et al.,23 Miyoshi et al.,24 and Takata et al.25 reported successful pain reduction through the 1-year follow-up after resection of the pseudoarticulation.
Subsequently, Li and colleagues7 reported on a series of seven patients with Bertolotti syndrome who had undergone minimally invasive resection of the pathologic pseudoarticulation for extraforaminal decompression; all had full or partial relief of pain preoperatively with trigger point injection. All patients experienced improvement in their low-back pain, and six experienced improvements in their radicular pain component; only two patients had recurrence of either component, and three patients remained pain free at the last follow-up.
Contemporaneously, Ju and colleagues published their experience with a similar approach in 61 patients with Bertolotti syndrome and Castellvi type I/II LSTV using an open L5 transverse processectomy for decompression of the L4 nerve root.26 Both groups experienced significant pain relief, though the relief was greater in patients whose pain had been relieved by a preoperative L4 nerve root block versus injection of the pseudoarticulation itself.
As noted by some of the aforementioned studies, including those by Li et al.7 and Jönsson et al.,14 decompression may not result in robust benefit for a subset of patients. For these patients, the main symptom driver may be the altered biomechanics of the lumbosacral junction as opposed to extraforaminal compression. Santavirta et al.16 compared the outcomes of two interventions in their series of 16 patients, 8 of whom underwent transverse processectomy and 8 of whom underwent posterolateral fusion. The authors reported equipoise between the interventions in terms of low-back pain improvement and improvement in functionality on the Oswestry pain scale. Both operatively treated groups had better pain outcomes relative to those of conservatively managed controls, but Oswestry Disability Index outcomes were similar. It was noted that fusion patients had disc degeneration more frequently than resection patients, leading others to recommend transverse processectomy for patients whose condition failed conservative management.
Mikula et al.6 additionally compared outcomes following fusion and decompression alone in 27 patients treated for Bertolotti syndrome. Although short-term (<6 months) pain improvement was similarly high in both groups (78% vs 100%), patients who underwent fusion had a significantly higher likelihood (78% vs 28%) of reporting long-term (>12 months) pain relief. Aside from these two studies, there appears to be a dearth of evidence comparing decompression and fusion for Bertolotti syndrome. However, a recent cadaveric study by Golubovsky et al.27 suggests the optimal surgical approach may depend upon the status of the lumbar motion segments immediately cephalad to the LSTV. Using a sample of seven cadaveric spines, the authors tested the biomechanics of the spines in five states: 1) the intact state, 2) an LSTV-mimic state wherein a 3D-printed surrogate of the LSTV pseudoarticulation was affixed to the cadaveric spine with bone cement so that it emulated the spine of an actual patient with Bertolotti syndrome, 3) the LSTV-mimic state with an L5–S1 instrumented fusion, 4) the LSTV-mimic state with an L4–S1 fusion, and 5) the LSTV-mimic state with an L4–5 fusion. The LSTV-mimic spine had significantly decreased lateral bending and axial rotation range of motion relative to the intact spine but increased lateral bending motion at L2–3. The L4–S1 and L4–5 fusion constructs both showed significantly greater flexion/extension, axial rotation, and lateral bending motion at the L3–4 and L2–3 motion segments. These data suggest that fusion of the caudal lumbar segments in LSTV patients create stress risers at the more cephalad segments, which may predispose them to more rapid degeneration. Nevertheless, they did decrease bending moments of the L5–S1 segment. Consequently, the authors argued in favor of resection alone for isolated LSTV with relatively healthy adjacent segments to reduce the risk that future surgical intervention would be required. But for patients with multilevel degenerative changes also meriting surgical intervention or where there is existing instability at the L5–S1 (LSTV) segment, instrumented fusion may create superior outcomes.
Ultimately, selection of the treatment approach should be guided by sound clinical judgement and the specific presentation of the patient. For patients whose primary complaint is isolated low-back pain—as was the case for the patient described in this report—treatment directed at the pseudoarticulation is normally a reasonable course of action. As we report, complete pain relief can be obtained in part due to the restoration of normal motion and the reduction of mechanical low-back pain. Additionally, it is thought that the pseudoarticulation contains abnormal nociceptors that signal along the medial branch pathway to produce the sensation of low-back pain in a manner similar to pseudoarthrosis-induced back pain.28 As such, resection of the pseudoarticulation effectively destroys and removes the nociceptors responsible for generating low-back pain. In select patients, fusion can also prove effective as a treatment for Bertolotti syndrome because it eliminates the motion that activates the pseudoarticulation nociceptors. This is similar to fusing a pseudarthrosis to achieve pain relief. The decision to perform joint resection without fusion in the illustrative case we describe was also based on the state of the native L5–S1 disc. If the disc had exhibited signs of significant deterioration with poor quality facet joints, concomitant fusion could have been considered.28 However, for young patients and patients with healthy discs and facet joints, fusion is generally not necessary.
Transverse processectomy, on the other hand, may be most suitable for patients with leg pain similar to foraminal stenosis–induced radiculopathy.26 In Bertolotti syndrome, instead of foraminotomy to decompress the root at the foramen, decompression of the extraforaminal nerve requires removal of the large articulation (i.e., resection of the transverse process). Altogether, because Bertolotti syndrome with leg pain is a rare condition, with its treatment rarer still, there is only level III evidence to support this rationale. However, as our review of the literature demonstrates, sound clinical decision-making that is based on each patient’s unique clinical presentation generally improves pain scores and overall quality of life in those experiencing Bertolotti syndrome.
Limitations
The present study has several limitations. First, the literature review is based on limited case series comprised of retrospective data. These are subject to selection bias in that good surgical candidates are more likely to be offered surgery, as well as institutional biases wherein the preference for resection versus fusion of the LSTV may be dictated by standard institutional practices. Reported pain and functional outcomes are also difficult to compare in the aggregate, because of the variability in reporting across publications. Last, most reported cases have only 1 to 2 years of follow-up. This limited follow-up and the difficulty in generalization that stems from the small sample size can likely be addressed through a prospective multicenter collaboration that examines standardized pain and functional outcomes.
Lessons
Lumbosacral transitional vertebrae alter the biomechanics of the lumbosacral junction and can cause extraforaminal compression of the lower lumbar roots, leading patients to present with radicular and/or axial pain components. Herein, we report the case of a 36-year-old female with medically refractory back pain-predominant Bertolotti syndrome, who underwent minimally invasive resection of her pseudoarticulation with robust pain relief through her 3-year follow-up. Image guidance with intraoperative navigation can be exceptionally helpful during resection due to the potential for disorientating transitional anatomy. Pseudoarticulation resection appears to be the favored operative strategy for patients with medically refractory disease, though limited evidence suggests that fusion may offer superior outcomes for select patients.
Further delineation of the best indications for surgical management and a comparison of fusion and pseudoarticulation resection are merited and will likely benefit from a prospective multicenter trial.
Acknowledgments
We would like to thank Stephen Graepel for their excellent illustrative contribution to the present work.
Author Contributions
Conception and design: Brown, Pham. Acquisition of data: Brown, Nguyen, Pham. Analysis and interpretation of data: Brown, Nguyen. Drafting the article: Brown, Pennington, Shahin, Nguyen. Critically revising the article: all authors. Reviewed submitted version of manuscript: Brown, Pennington, Pham. Approved the final version of the manuscript on behalf of all authors: Brown. Study supervision: Brown, Pham.
References
- 1. Sekharappa V, Amritanand R, Krishnan V, David KS. Lumbosacral transition vertebra: prevalence and its significance. Asian Spine J. 2014;8(1):51–58. doi: 10.4184/asj.2014.8.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Quinlan JF, Duke D, Eustace S. Bertolotti’s syndrome. A cause of back pain in young people. J Bone Joint Surg Br. 2006;88(9):1183–1186. doi: 10.1302/0301-620X.88B9.17211. [DOI] [PubMed] [Google Scholar]
- 3. Castellvi AE, Goldstein LA, Chan DP. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine (Phila Pa 1976) 1984;9(5):493–495. doi: 10.1097/00007632-198407000-00014. [DOI] [PubMed] [Google Scholar]
- 4. Ahn SS, Chin DK, Kim SH, Kim DW, Lee BH, Ku MG. The clinical significance of lumbosacral transitional vertebrae on the surgical outcomes of lumbar discectomy: a retrospective cohort study of young adults. World Neurosurg. 2017;99:745–750. doi: 10.1016/j.wneu.2016.05.073. [DOI] [PubMed] [Google Scholar]
- 5. Shin EH, Cho KJ, Kim YT, Park MH. Risk factors for recurrent lumbar disc herniation after discectomy. Int Orthop. 2019;43(4):963–967. doi: 10.1007/s00264-018-4201-7. [DOI] [PubMed] [Google Scholar]
- 6. Mikula AL, Lakomkin N, Ransom RC, et al. Operative treatment of Bertolotti syndrome: resection versus fusion. World Neurosurg. 2022;165:e311–e316. doi: 10.1016/j.wneu.2022.06.042. [DOI] [PubMed] [Google Scholar]
- 7. Li Y, Lubelski D, Abdullah KG, Mroz TE, Steinmetz MP. Minimally invasive tubular resection of the anomalous transverse process in patients with Bertolotti’s syndrome: presented at the 2013 Joint Spine Section Meeting: clinical article. J Neurosurg Spine. 2014;20(3):283–290. doi: 10.3171/2013.11.SPINE13132. [DOI] [PubMed] [Google Scholar]
- 8. Porter NA, Lalam RK, Tins BJ, Tyrrell PNM, Singh J, Cassar-Pullicino VN. Prevalence of extraforaminal nerve root compression below lumbosacral transitional vertebrae. Skeletal Radiol. 2014;43(1):55–60. doi: 10.1007/s00256-013-1750-0. [DOI] [PubMed] [Google Scholar]
- 9. Avimadje M, Goupille P, Jeannou J, Gouthière C, Valat JP. Can an anomalous lumbo-sacral or lumbo-iliac articulation cause low back pain? A retrospective study of 12 cases. Rev Rhum Engl Ed. 1999;66(1):35–39. [PubMed] [Google Scholar]
- 10. Mitra R, Carlisle M. Bertolotti’s syndrome: a case report. Pain Pract. 2009;9(2):152–154. doi: 10.1111/j.1533-2500.2008.00253.x. [DOI] [PubMed] [Google Scholar]
- 11. Barkhane Z, Belaaroussi S, Foudail M, Mehdi F. Bilateral bertolotti’s syndrome: A case report of an uncommon presentation of chronic low back pain in an elder patient. Cureus. 2022;14(7):e26569. doi: 10.7759/cureus.26569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zhang R, Change J. Interventional management of chronic low back pain associated with Bertolotti’s syndrome: report of case series. Ann Clin Case Rep. 2017;2:1348. [Google Scholar]
- 13. Glémarec J, Varin S, Cozic C, et al. Efficacy of local glucocorticoid after local anesthetic in low back pain with lumbosacral transitional vertebra: a randomized placebo-controlled double-blind trial. Joint Bone Spine. 2018;85(3):359–363. doi: 10.1016/j.jbspin.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 14. Jönsson B, Strömqvist B, Egund N. Anomalous lumbosacral articulations and low-back pain. Evaluation and treatment. Spine (Phila Pa 1976) 1989;14(8):831–834. doi: 10.1097/00007632-198908000-00009. [DOI] [PubMed] [Google Scholar]
- 15. Brault JS, Smith J, Currier BL. Partial lumbosacral transitional vertebra resection for contralateral facetogenic pain. Spine (Phila Pa 1976) 2001;26(2):226–229. doi: 10.1097/00007632-200101150-00020. [DOI] [PubMed] [Google Scholar]
- 16. Santavirta S, Tallroth K, Ylinen P, Suoranta H. Surgical treatment of Bertolotti’s syndrome. Follow-up of 16 patients. Arch Orthop Trauma Surg. 1993;112(2):82–87. doi: 10.1007/BF00420261. [DOI] [PubMed] [Google Scholar]
- 17. Abe E, Sato K, Shimada Y, Okada K, Yan K, Mizutani Y. Anterior decompression of foraminal stenosis below a lumbosacral transitional vertebra. A case report. Spine (Phila Pa 1976) 1997;22(7):823–826. doi: 10.1097/00007632-199704010-00023. [DOI] [PubMed] [Google Scholar]
- 18. Kikuchi K, Abe E, Miyakoshi N, et al. Anterior decompression for far-out syndrome below a transitional vertebra: a report of two cases. Spine J. 2013;13(8):e21–e25. doi: 10.1016/j.spinee.2013.02.033. [DOI] [PubMed] [Google Scholar]
- 19. Malham GM, Limb RJ, Claydon MH, Brazenor GA. Anterior pseudoarthrectomy for symptomatic Bertolotti’s syndrome. J Clin Neurosci. 2013;20(12):1762–1766. doi: 10.1016/j.jocn.2013.02.018. [DOI] [PubMed] [Google Scholar]
- 20. Ichihara K, Taguchi T, Hashida T, Ochi Y, Murakami T, Kawai S. The treatment of far-out foraminal stenosis below a lumbosacral transitional vertebra: a report of two cases. J Spinal Disord Tech. 2004;17(2):154–157. doi: 10.1097/00024720-200404000-00013. [DOI] [PubMed] [Google Scholar]
- 21. Weber J, Ernestus RI. Transitional lumbosacral segment with unilateral transverse process anomaly (Castellvi type 2A) resulting in extraforaminal impingement of the spinal nerve: a pathoanatomical study of four specimens and report of two clinical cases. Neurosurg Rev. 2010;34(2):143–150. doi: 10.1007/s10143-010-0300-7. [DOI] [PubMed] [Google Scholar]
- 22. Shibayama M, Ito F, Miura Y, Nakamura S, Ikeda S, Fujiwara K. Unsuspected reason for sciatica in Bertolotti’s syndrome. J Bone Joint Surg Br. 2011;93(5):705–707. doi: 10.1302/0301-620X.93B5.26248. [DOI] [PubMed] [Google Scholar]
- 23. Ugokwe KT, Chen TL, Klineberg E, Steinmetz MP. Minimally invasive surgical treatment of Bertolotti’s syndrome: case report. Neurosurgery. 2008;62(5 suppl 2):ONSE454–ONSE456. doi: 10.1227/01.neu.0000326034.77585.88. [DOI] [PubMed] [Google Scholar]
- 24. Miyoshi Y, Yasuhara T, Date I. Posterior decompression of far-out foraminal stenosis caused by a lumbosacral transitional vertebra—case report. Neurol Med Chir (Tokyo) 2011;51(2):153–156. doi: 10.2176/nmc.51.153. [DOI] [PubMed] [Google Scholar]
- 25. Takata Y, Sakai T, Higashino K, et al. Minimally invasive microendoscopic resection of the transverse process for treatment of low back pain with Bertolotti’s syndrome. Case Rep Orthop. 2014;2014:613971. doi: 10.1155/2014/613971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ju CI, Kim SW, Kim JG, Lee SM, Shin H, Lee HY. Decompressive L5 transverse processectomy for Bertolotti’s syndrome: a preliminary study. Pain Physician. 2017;20(6):E923–E932. [PubMed] [Google Scholar]
- 27. Golubovsky JL, Colbrunn RW, Klatte RS, et al. Development of a novel in vitro cadaveric model for analysis of biomechanics and surgical treatment of Bertolotti syndrome. Spine J. 2020;20(4):638–656. doi: 10.1016/j.spinee.2019.10.011. [DOI] [PubMed] [Google Scholar]
- 28. Kotsenas AL. Imaging of posterior element axial pain generators: facet joints, pedicles, spinous processes, sacroiliac joints, and transitional segments. Radiol Clin North Am. 2012;50(4):705–730. doi: 10.1016/j.rcl.2012.04.008. [DOI] [PubMed] [Google Scholar]
- 29. Babu H, Lagman C, Kim TT, Grode M, Johnson JP, Drazin D. Intraoperative navigation-guided resection of anomalous transverse processes in patients with Bertolotti’s syndrome. Surg Neurol Int. 2017;8:236. doi: 10.4103/sni.sni_173_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Louie CE, Hong J, Bauer DF. Surgical management of Bertolotti’s syndrome in two adolescents and literature review. Surg Neurol Int. 2019;10:135. doi: 10.25259/SNI-305-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Adams R, Herrera-Nicol S, Hawks C, Sobotka S, Jenkins AL. Treatment optimization for patients with Bertolotti’s syndrome. J Am Coll Surg. 2019;2294(suppl 2):e39. [Google Scholar]
- 32. Chang CJ, Chiu YP, Ji HR, Chu CH, Chiu CD. Surgical interventions for Bertolotti’s syndrome: case report and review of unsatisfactory cases in the literature. BMC Surg. 2022;22(1):36. doi: 10.1186/s12893-022-01498-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Stein E, Panjeton GD, Kumar S. Endoscopic resection of pseudoarticulation as a treatment for Bertolotti’s syndrome. Cureus. 2023;15(1):e33397. doi: 10.7759/cureus.33397. [DOI] [PMC free article] [PubMed] [Google Scholar]