ABSTRACT
Traditional ferroptosis activators typically suppress antitumor immunity. Our discovery shows that N6F11, a small molecule compound, can selectively induce ferroptosis by targeting TRIM25-mediated GPX4 degradation in cancer cells while sparing immune cells. This breakthrough establishes a safe and effective strategy to enhance ferroptosis-driven antitumor immunity.
KEYWORDS: Drug discovery, ferroptosis, GPX4, immunotherapy, TRIM25
The tumor microenvironment (TME) is a highly intricate and dynamic system that undergoes continuous transformations. While the specific composition of the TME can vary based on the type of tumor, it consistently encompasses vital components, such as immune cells, stromal cells, blood vessels, and the extracellular matrix.1 The TME plays a pivotal role in shaping the development and progression of tumors. It can either impede the infiltration and functioning of immune cells or, conversely, stimulate anti-tumor immune responses, as evidenced by the remarkable progress achieved with immune checkpoint inhibitors in patient treatment.2
However, conventional anti-cancer drugs are typically administered systemically, affecting not only tumor cells, but also altering the behavior of immune cells. For instance, numerous studies have shown that traditional ferroptosis inducers, such as erastin and RSL3, directly target the glutathione peroxidase 4 (GPX4) antioxidant pathway.3 This dual impact results in the demise of tumor cells, but also causes harm to immune cells.4–8 Consequently, a significant challenge in the field of oncology is to discover methods or drugs that selectively eliminate tumor cells while preserving the functionality of immune cells. In our recent study, we unveiled a novel strategy for inducing ferroptosis that selectively targets tumor cells without compromising the activity of immune cells (Figure 1).9
Figure 1.
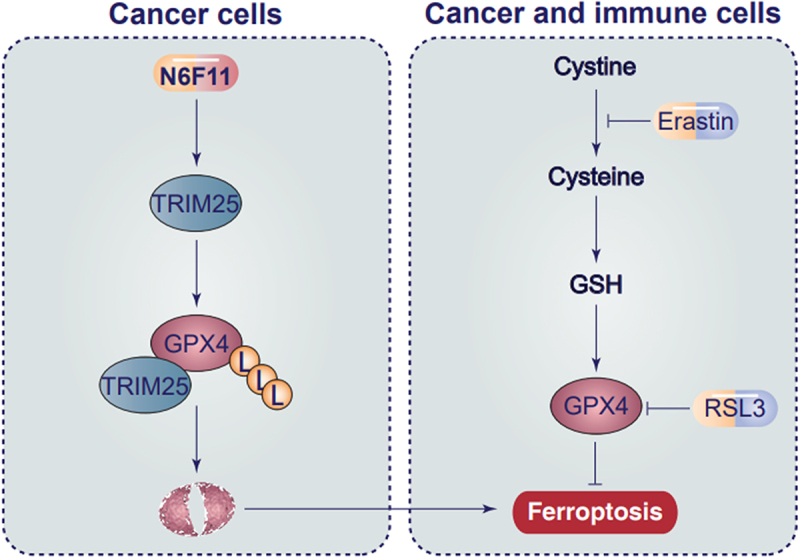
Selective role of N6F11 in inducing ferroptosis in cancer cells. Unlike traditional ferroptosis activators erastin and RSL3, N6F11 can trigger TRIM25-dependent GPX4 degradation in cancer cells, rather than in immune cells.
In our research, we initiated the screening of a library of over 4000 small-molecule compounds using In-Cell Western assays (also known as cell-based enzyme-linked immunosorbent assay). These compounds had unknown targets, and our objective was to identify inhibitors of GPX4 protein expression in PANC1 cells, a well-established human pancreatic ductal adenocarcinoma (PDAC) cell line widely utilized in drug response studies. Our screening approach, followed by subsequent traditional protein and gene expression techniques, revealed that a compound named N6F11 can effectively inhibit GPX4 protein expression in various human and mouse cancer cell lines. Notably, N6F11‘s mechanism of action differs from widely used ferroptosis activators. Unlike RSL3 and erastin, N6F11 does not directly bind to GPX4 or induce glutathione depletion, respectively.
Second, we demonstrated that N6F11 functions as a novel GPX4 degrader by activating the ubiquitin/proteasome system (UPS), rather than the autophagy pathway. In contrast, erastin and RSL3 have been previously shown to cause GPX4 degradation through selective or nonselective autophagy activation. Further investigations through immunoprecipitation-mass spectrometry experiments identified specific GPX4 binding proteins, including several E3 ubiquitin ligases, early in the N6F11 treatment process. Subsequent RNAi and CRISPR-Cas9 knockout experiments pinpointed tripartite motif containing 25 (TRIM25) as the key E3 ligase responsible for N6F11-induced GPX4 degradation. Structural mutations and in vitro thermal stability experiments provided evidence that TRIM25 interacts with GPX4 through its PS domain, while N6F11 directly binds to TRIM25 on the RING domain to initiate this process.
Third, our in vitro experiments have shown that TRIM25 is predominantly expressed in cancer cells, rather than in immune cells. The induction of TRIM25-dependent GPX4 degradation through N6F11 does not exhibit toxicity toward immune cells, including T cells, natural killer cells, neutrophils, and dendritic cells. This unique selectivity of N6F11 prompted us to compare its activity with that of IKE, an analog of erastin known for its metabolic stability in vivo. In a subcutaneous tumor animal model using immunocompromised nude mice, IKE demonstrated greater anticancer activity than N6F11. However, N6F11 exhibited strong anticancer activity compared to IKE in immunocompetent C57BL/6J mice. To further assess its effectiveness, we employed orthotopic and spontaneous PDAC models, which are typically unresponsive to immune checkpoint inhibitors due to their low immunogenicity. Combining N6F11 with anti-CD274 (also known as PD-L1) significantly inhibited PDAC tumor growth in these advanced PDAC models. This inhibition was found to be dependent on CD8+ T cells and high mobility group box 1 (HMGB1), a mediator of immunological cell death.10
In summary, our findings have established a safe and efficient strategy for enhancing ferroptosis-driven antitumor immunity in PDAC models. While these results are promising, several aspects require further investigation. Although N6F11 has demonstrated efficacy at nanomolar concentrations in specific cancer cells, the most effective concentration in most cancer cells appears to be in the micromolar range. This discrepancy needs to be addressed through pharmacological optimization to enhance its activity. Additionally, there is a lack of pharmacokinetic data for N6F11 in vivo, necessitating future studies to determine its half-life and tissue distribution. Furthermore, additional research is needed to determine whether other TRIM25-targeted molecules are involved in ferroptosis-related antitumor immunity.
Funding Statement
J.Liu is supported by grants from National Natural Science Foundation of China (32200594 and 82372152). J. Li is supported by grants from National Natural Science Foundation of China (82102806).
Disclosure statement
No potential conflict of interest was reported by the authors.
Author contributions
All authors contributed to the writing and agreed on the submission.
References
- 1.Binnewies M, Roberts EW, Kersten K, Chan V, Fearon DF, Merad M, Coussens LM, Gabrilovich DI, Ostrand-Rosenberg S, Hedrick CC, et al. Understanding the tumor immune microenvironment (TIME) for effective therapy. Nat Med. 2018;24(5):541–3. doi: 10.1038/s41591-018-0014-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Galluzzi L, Humeau J, Buque A, Zitvogel L, Kroemer G.. Immunostimulation with chemotherapy in the era of immune checkpoint inhibitors. Nat Rev Clin Oncol. 2020;17(12):725–741. doi: 10.1038/s41571-020-0413-z. [DOI] [PubMed] [Google Scholar]
- 3.Chen X, Kang R, Kroemer G, Tang D. Broadening horizons: the role of ferroptosis in cancer. Nat Rev Clin Oncol. 2021;18(5):280–296. doi: 10.1038/s41571-020-00462-0. [DOI] [PubMed] [Google Scholar]
- 4.Kim R, Hashimoto A, Markosyan N, Tyurin VA, Tyurina YY, Kar G, Fu S, Sehgal M, Garcia-Gerique L, Kossenkov A, et al. Ferroptosis of tumour neutrophils causes immune suppression in cancer. Nature. 2022;612(7939):338–346. doi: 10.1038/s41586-022-05443-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xu S, Chaudhary O, Rodriguez-Morales P, Sun X, Chen D, Zappasodi R, Xu Z, Pinto AFM, Williams A, Schulze I, et al. Uptake of oxidized lipids by the scavenger receptor CD36 promotes lipid peroxidation and dysfunction in CD8+ T cells in tumors. Immunity. 2021;54(7):1561–1577.e7. doi: 10.1016/j.immuni.2021.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ma X, Xiao L, Liu L, Ye L, Su P, Bi E, Wang Q, Yang M, Qian J, Yi Q. CD36-mediated ferroptosis dampens intratumoral CD8+ T cell effector function and impairs their antitumor ability. Cell Metab. 2021;33(5):1001–1012.e5. doi: 10.1016/j.cmet.2021.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Poznanski SM, Singh K, Ritchie TM, Aguiar JA, Fan IY, Portillo AL, Rojas EA, Vahedi F, El-Sayes A, Xing S, et al. Metabolic flexibility determines human NK cell functional fate in the tumor microenvironment. Cell Metab. 2021;33(6):1205–1220.e5. doi: 10.1016/j.cmet.2021.03.023. [DOI] [PubMed] [Google Scholar]
- 8.Han L, Bai L, Qu C, Dai E, Liu J, Kang R, Zhou D, Tang D, Zhao Y. PPARG-mediated ferroptosis in dendritic cells limits antitumor immunity. Biochem Biophys Res Commun. 2021;576:33–39. doi: 10.1016/j.bbrc.2021.08.082. [DOI] [PubMed] [Google Scholar]
- 9.Li J, Liu J, Zhou Z, Wu R, Chen X, Yu C, Stockwell B, Kroemer G, Kang R, Tang D. Tumor-specific GPX4 degradation enhances ferroptosis-initiated antitumor immune response in mouse models of pancreatic cancer. Sci Transl Med. 2023;15(720):eadg3049. doi: 10.1126/scitranslmed.adg3049. [DOI] [PubMed] [Google Scholar]
- 10.Galluzzi L, Vitale I, Warren S, Adjemian S, Agostinis P, Martinez AB, Chan TA, Coukos G, Demaria S, Deutsch E, et al. Consensus guidelines for the definition, detection and interpretation of immunogenic cell death. J Immunother Cancer. 2020;8(1):e000337. doi: 10.1136/jitc-2019-000337. [DOI] [PMC free article] [PubMed] [Google Scholar]


