Abstract
Background
Mental health care is now recognised as essential for people affected by NTDs, but accessible services are rare. This paper presents results of a prevalence study for depression and anxiety among people living with leprosy and lymphatic filariasis, and collation of user perspectives on needs and priorities for a new service.
Methods
Prevalence of mental conditions was carried out with 141 people living with leprosy and lymphatic filariasis and matched controls. Those who screened positive for depression or anxiety were interviewed in a qualitative study to understand their experiences of living with the conditions, and what their priorities would be for services and support. Results contributed to the process of developing a contextually adapted collaborative care model for implementation in the primary care system in Nigeria, using a Theory of Change approach.
Results
We found high rates of depression, anxiety, and reduced wellbeing, with strong correlation across measures. The qualitative study revealed experiences of stigma and exclusion, and concern for financial and economic needs, and a desire for provision of free services and support for livelihoods.
Conclusion
Services should be designed with good understanding of local needs and service user priorities.
Contexte
Les soins de santé mentale sont désormais reconnus comme essentiels pour les personnes touchées par les MTN, mais les services accessibles sont rares. Cet article présente les résultats d'une étude de prévalence de la dépression et de l'anxiété chez les personnes vivant avec la lèpre et la filariose lymphatique, ainsi que la collecte des points de vue des utilisateurs sur les besoins et les priorités d'un nouveau service.
Méthodes utilisées
Une étude de prévalence des troubles mentaux a été menée auprès de 141 personnes vivant avec la lèpre et la filariose lymphatique et de témoins appariés. Celles qui ont été dépistées positives pour la dépression ou l'anxiété ont été interrogées dans le cadre d'une étude qualitative afin de comprendre leur expérience de la vie avec ces maladies et leurs priorités en matière de services et de soutien. Les résultats ont contribué au processus d'élaboration d'un modèle de soins collaboratifs adapté au contexte et destiné à être mis en œuvre dans le système de soins primaires au Nigeria, à l'aide d'une approche fondée sur la théorie du changement.
Résultats
Nous avons constaté des taux élevés de dépression, d'anxiété et de diminution du bien-être, avec une forte corrélation entre les mesures. L'étude qualitative a révélé des expériences de stigmatisation et d'exclusion, des préoccupations concernant les besoins financiers et économiques, ainsi qu'un désir de services gratuits et de soutien aux moyens de subsistance.
Conclusion
Les services doivent être conçus en tenant compte des besoins locaux et des priorités des utilisateurs.
Antecedentes
Actualmente se reconoce que la atención de salud mental es esencial para las personas afectadas por ETD, pero los servicios accesibles son escasos. los servicios accesibles son escasos. Este documento presenta los resultados de un estudio de prevalencia de depresión y ansiedad entre las personas que viven con lepra y filariasis linfática, y las perspectivas de los usuarios sobre las necesidades y prioridades de un nuevo servicio.
Métodos
Se realizó un estudio de prevalencia de trastornos mentales con 141 personas que vivían con lepra y filariasis linfática y controles emparejados. Los que dieron positivo en depresión o ansiedad fueron entrevistados en un estudio cualitativo para conocer sus de vivir con estas enfermedades y cuáles serían sus prioridades en cuanto a servicios y apoyo. servicios y apoyo. Los resultados contribuyeron al proceso de desarrollo de un modelo de atención para su aplicación en el sistema de atención primaria de Nigeria, utilizando un enfoque basado en la Teoría del Cambio.
Resultados
Encontramos altas tasas de depresión, ansiedad y reducción del bienestar, con una fuerte correlación entre las medidas. correlación entre las medidas. El estudio cualitativo reveló experiencias de estigmatización y de estigmatización y exclusión, preocupación por las necesidades financieras y servicios gratuitos y apoyo a los medios de subsistencia.
Conclusión
Los servicios deben diseñarse teniendo en cuenta las necesidades locales y las prioridades de los usuarios de los usuarios.
Keywords: anxiety, depression, leprosy, lymphatic filariasis, mental health, Neglected Tropical Diseases
Introduction
Of the 20 infectious diseases defined by WHO as Neglected Tropical Diseases (NTDs), many have been shown to have a substantial comorbidity with mental and neurological conditions.1 Depression and anxiety are most commonly associated with NTDs. The quality of epidemiological evidence suffers from heterogeneity across multiple small studies but rates of 20% to almost 100% have been reported in various population groups.2
This association is mainly driven by social determinants, with stigma being particularly implicated.3 This link has been postulated to be stronger where there are visible signs of disease, for example in leprosy, lymphatic filariasis (LF) and cutaneous leishmaniasis. This may be increased where disfigurement is on the face and affects women more, while strong relationships are protective.4
There are many common risk factors for mental conditions and NTDs, such as poverty, being part of excluded groups and poor access to healthcare and education. So while comorbidity will be high, common approaches and platforms for care are a logical solution to this increased risk and neglect of care.
In 2021, WHO released the NTD Roadmap (2021–2030),5 which offers a broader holistic perspective on NTDs and emphasises accountability and national leadership.6 New WHO guidance on the integration of mental health and NTDs, subtitled ‘Towards a person-centred approach’,6 borrows from decades of learning in the field of global mental health, applying learning in practical interventions to the NTD field.7
This paper seeks to better characterise the link between NTDs and mental health, quantifying the comorbidity of skin NTDs (leprosy and LF) and depression and anxiety. Nigeria is endemic for both leprosy and LF. Nationally, 17 356 new leprosy cases were notified over 5 y (2010–2014), of whom 9% were children. The leprosy case detection rate during this period was around 2.2/100 000.8 The predicted mean national prevalence of LF was 5.3% using the immunochromatographic test (ICT) and 2.0% for detection of microfilariae.9
We explore, using qualitative methods, the factors that might underlie these links. This is part of the development of an integrated intervention for mental health and NTDs in a typical environment of high NTD endemicity and weak service provision. It represents a structured process of bringing together international normative guidance with local perspectives, so as to appropriately adapt evidence and best practice to local contexts. A linked paper10 describes the findings of a feasibility and acceptability study of the intervention.
This research is carried out as a partnership between The Leprosy Mission (TLM) Nigeria, CBM Global and the University of Jos. Local actors working in mental health in Benue State collaborated closely from the outset, for example service-user groups in leprosy and LF, mental health and NTD leads in the Benue State Ministry of Health.
The study has three parts
The first is a quantitative controlled prevalence study incorporating measures of depression, anxiety and well-being among people with leprosy and LF. We also measured the severity of leprosy and LF to examine whether there was a link between the severity of the physical condition and mental health consequences.
The second part is a qualitative study seeking to understand in more detail the social and economic impact of living with NTDs on mental health and well-being, and the priorities of people affected for services.
Finally, we incorporated this information, including the views of service users and carers, as a basis for intervention design through the Theory of Change (ToC) process. This is a method of describing a process of reform by achieving consensus on steps that might lead to a desired change in a particular context. Inherent in this proposed process of change are assumptions about how one step leads to another, which allows research questions to be raised around how interventions might work.11
Methods
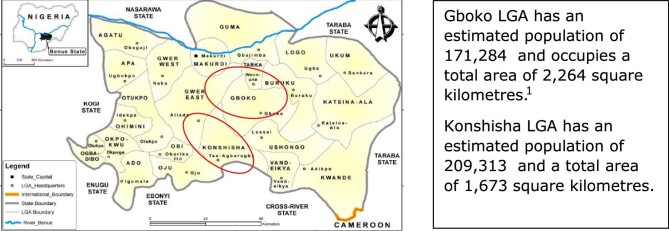
This study was conducted in a total of 12 communities, 6 each in Gboko and Konshisha Local Government Areas (LGAs) in Benue State, Nigeria. Both LGAs are among the 583 endemic LGAs for LF in Nigeria. Also, Benue State has significantly contributed to over 2000 cases of leprosy reported annually in Nigeria for the past decade.12,13 These communities are known to our consortium partners, where persons with LF and leprosy reside in the state. Gboko LGA is mostly urban while Konshisha LGA is more rural. The predominant language in both is Tiv, with farming and trading being the mainstay of the economy.
The area was chosen because TLM and CBM have established partnerships with Benue State health services for NTDs and mental health. The existence of established services for mental health and NTDs (such as Mass Administration of Medicines [MAM] for LF, specialised health centers offering leprosy morbidity management,and a Comprehensive Community Mental Health Programme [CCMHP] in some clinics in the LGA) meant that the new model could be tested relatively quickly, relying on existing infrastructure and human resources for health.
Study design and sample size calculation
The prevalence study utilised a cross-sectional design comparing people affected by LF and leprosy and matched controls. The sample size for the study was estimated using a formula for a comparative study using independent proportions.14 We estimated a minimum sample size of 56 subjects per group, where we used a prevalence of depression of 20% among subjects with LF from a previous study in Nigeria15 and the prevalence of depression among the general population of 3.1% (also in Nigeria).16
We then used a qualitative approach for understanding participants’ perspectives of their experiences of living with an NTD and their priorities for services.
Inclusion criteria and sampling
Men and women with LF and leprosy with visible signs of the conditions (lymphoedema, hydrocele, disfigurement) aged 18 y and above residing in 12 communities within Konshisha and Gboko LGAs were included. Persons residing in the same communities without leprosy and LF matched for age and gender were eligible as controls (through block matching plus or minus 5 y of age).
All men and women who had met the inclusion criteria, resided within the 12 communities of Konshisha and Gboko LGAs of Benue State, and were willing to participate in the study were identified by engaging with existing peer groups of the affected people through the group leaders. Peer-group meetings were subsequently organised by the respective peer-group leaders where further engagement with members was done and all eligible participants were purposively selected and administered the questionnaire.
For the controls, household listing was done in the communities where the study group had been selected and lists of households with eligible participants meeting the age-matching and gender-matching criteria were made, forming the sampling frame. One hundred and forty one (141) households were selected using a simple random sampling technique by balloting from the sampling frame of 208 households following which the eligible controls where picked after consenting for participation in the study. In households with more than one eligible control, a simple random sampling technique by balloting was employed to select one participant. The eligible controls were then administered the questionnaire in their respective locations of choice within the community.
The qualitative component of the study included respondents who screened positive for depression and/or anxiety.
Data collection and analysis
The Patient Health Questionnaire (PHQ-9)17 and Generalised Anxiety Disorder scale (GAD-7)18 are brief screening and severity measures for depression and anxiety, and have been widely used in Nigeria,19 including among people with NTDs.11 Similarly, the WHO-5 Wellbeing Index has been used effectively in a wide variety of contexts and has been shown to be particularly sensitive for depression.20 An interview topic guide was developed for the qualitative study based on literature review and preliminary discussions (Supplementary Data 1).
The data collection instruments were translated into the Tiv language and back-translated into English prior to data collection. Six research assistants were trained on the study protocol and data collection, and tools were pretested on a small number of people, including grading of physical signs of leprosy21 and LF22 using standardised criteria (Supplementary Data 2). These criteria included descriptions of the severity of the physical signs of the conditions, aided by pictorial charts. Prior to the administration of the questionnaires, consent was obtained from all the respondents after receiving information in their own language. Opportunities for accessing support were explained and those screening positive were referred.
Open Data Kit software was used to collect quantitative data, enabling timely quality assessment of data collected.23
A total of 6 focus group discussions (FGDs) were conducted each with between 8 and 10 persons. Three FGDs were conducted with persons with leprosy (two on men and one on women) and three FGDs on LF were conducted with women, as too few men screened positive in each community. The FGDs were conducted in Tiv using voice recorders and keeping field notes.
The primary outcome variable in the study was depression (categorised as present or absent). Chi square test was used as a test comparison of the variables between the two groups and the Mann–Whitney U test was employed as the test of difference of the median of well-being, PHQ-9 and GAD-7 scores between the study and control groups. Logistic regression was used to identify predictors of depression using explanatory variables singly at the first level and cumulatively at the second level. Crude and adjusted odds ratios were generated as the point estimates of the effect of the explanatory variables on the presence of depression.
For the qualitative component of the study, NVivo version 12 was used for the content analysis where a priori (items identified in advance) and emergent codes were brought out, recurrent themes identified and a summary of findings made aligned to the objectives of the study.
Results
A total of 282 participants, comprising 141 in the study group (leprosy=73; lymphatic filariasis=68) and 141 in the control group participated in this study. The demographic characteristics of the groups were well matched for age, gender balance and family history of mental illness (Table 1). There were slightly more women compared with men in both groups, and the control group had received slightly higher levels of education and were more likely to be employed.
Table 1.
Demographic characteristics of study participants in the two groups. The study group comprised people identified with visible signs of leprosy of lymphatic filariasis and controls were matched by age, gender and location.
| Study group | Control group | |||
|---|---|---|---|---|
| n=141 | n=141 | |||
| Characteristics | Frequency (%) | Frequency (%) | χ2 | p-value |
| Age (years) | 11 (7.8) | 20 (14.2) | 7.381 | 0.287 |
| 18–27 | 17 (12.1) | 13 (9.2) | ||
| 28–37 | 25 (17.7) | 25 (17.7) | ||
| 38–47 | 23 (16.3) | 26 (18.4) | ||
| 48–57 | 20 (14.2) | 20 (14.2) | ||
| 58–67 | 12 (18.5) | 17 (12.1) | ||
| 68–77 | 33 (23.4) | 20 (14.2) | ||
| ≥78 | ||||
| Gender | ||||
| Female | 82 (58.2) | 82 (58.2) | 0.000 | 1.0 |
| Male | 59 (41.8) | 59 (41.8) | ||
| Marital status | ||||
| Single | 21 (14.9) | 23 (16.3) | 0.738 | 0.864 |
| Married | 75 (53.2) | 78 (55.3) | ||
| Separated/divorced | 10 (7.1) | 7 (5.0) | ||
| Widowed | 35 (24.8) | 33 (23.4) | ||
| Higher educational attainment | ||||
| No formal | 60 (42.6) | 39 (27.7) | 13.823 | 0.003 |
| Primary | 25 (17.7) | 19 (13.5) | ||
| Secondary | 41 (29.1) | 48 (31.6) | ||
| Tertiary | 15 (10.6) | 35 (24.8) | ||
| Employment status | ||||
| Employed | 20 (14.2) | 46 (32.6) | 13.372 | 0.001 |
| Unemployed | 121 (85.8) | 95 (67.4) | ||
| Family history of mental illness | ||||
| Absent | 108 (76.6) | 106 (75.2) | 0.078 | 0.781 |
| Present | 33 (23.4) | 35 (24.8) | ||
Just over half (51.8%) of the participants identified as having leprosy and the rest had LF. The severity gradings of the participants’ conditions are summarised in Table 2. In each case, more people had severe gradings of the conditions, particularly the LF group.
Table 2.
Severity of leprosy and lymphatic filariasis among the study group
| Characteristics | Frequency | Percentage |
|---|---|---|
| Disease condition | ||
| Leprosy | 73 | 51.8 |
| Lymphatic filariasis | 68 | 48.2 |
| Total | 141 | 100.0 |
| Severity of leprosy | ||
| Grade 0 | 22 | 30.1 |
| Grade 1 | 24 | 32.9 |
| Grade 2 | 27 | 37.0 |
| Total | 73 | 100.0 |
| Severity of lymphatic filariasis | ||
| Grade 1 | 10 | 14.7 |
| Grade 2 | 18 | 26.5 |
| Grade 3 | 40 | 58.8 |
| Total | 68 | 100.0 |
Statistically significant variance was found in the median well-being, PHQ-9 and GAD-7 scores in the study. The prevalence of depression was found to be 60.3% in the NTD group and 31.2% in the control group. Among those with depression, the severity of NTDs was similarly distributed (mainly in the mild and moderate levels) (see Table 3). Anxiety disorder was present in 69 (48.9%) of those with NTDs of interest but in only 41 (29.1%) of the control group participants. Well-being was much poorer in participants affected by NTDs than the matched control population.
Table 3.
Status of well-being and prevalence of anxiety and depression using Wellbeing 5, PHQ-9 and Gad-7
| Parameters | Study group n=141 Frequency (%) |
Control group n=141 Frequency (%) |
Χ2 | p-value |
|---|---|---|---|---|
| Well-being | ||||
| Poor | 63 (44.7) | 38 (27.0) | 9.641 | 0.002 |
| Good | 78 (55.3) | 103 (73.0) | ||
| Anxiety | ||||
| Absent | 72 (51.1) | 100 (70.9) | 11.685 | <0.001 |
| Present | 69 (48.9) | 49 (29.1) | ||
| Depression | ||||
| Absent | 56 (39.7) | 97 (68.8) | 24.018 | <0.001 |
| Present | 85 (60.3) | 44 (31.2) | ||
| Depression status | ||||
| Absent | 56 (39.7) | 97 (68.8) | 24.139 | <0.001 |
| Mild | 52 (39.9) | 28 (19.9) | ||
| Moderate | 28 (19.9) | 14 (9.9) | ||
| Severe | 5 (3.5) | 2 (1.4) |
Depression in the study was found to be predicted by the presence of disabling LF with the odds of 9.5 times the control group having adjusted for other factors such as age, level of education, employment status, family history of mental illness, well-being et cetera. The adjusted odds ratio for depression among people with leprosy (again at a level with disfigurement and leading to disabilities) was also high at 2.69. Furthermore, there was a strong correlation between PHQ-9, GAD-7 and WHO-5 Wellbeing Index scores (Table 4). Other demographic, educational and medical factors (other than leprosy or LF) did not show statistically significant correlation.
Table 4.
Logistic regression of predictors of depression
| Factors | COR 95% (CI) | p-value | AOR 95% (CI) | p-value |
|---|---|---|---|---|
| Age (years) | 1.01 (0.994–1.017) | 0.393 | 1.01 (0.979–1.039) | 0.556 |
| Gender | ||||
| Female | 1.51 (0.936–2.439) | 0.091 | 2.02 (0.738–5.508) | 0.172 |
| Male | Ref | |||
| Marital status | ||||
| Single | 0.50 (0.229–1.077) | 0.076 | 0.43 (0.061–2.985) | 0.388 |
| Married | 0.60 (0.337–1.065) | 0.081 | 0.52 (0.145–1.895) | 0.325 |
| Separated | 0.70 (0.242–2.038) | 0.515 | 0.95 (0.122–7.447) | 0.963 |
| Widowed | Ref | |||
| Highest educational attainment | ||||
| Non-formal | 3.71 (1.757–7.819) | 0.001 | 0.85 (0.195–3.730) | 0.832 |
| Primary | 3.12 (1.312–7.408) | 0.010 | 1.79 (0.445–7.228) | 0.411 |
| Secondary | 2.03 (0.947–4.329) | 0.690 | 2.68 (0.755–9.507) | 0.127 |
| Tertiary | Ref | |||
| Employment status | ||||
| Unemployed | 1.07(0.614–1.853) | 0.819 | 1.53 (0.513–4.540) | 0.447 |
| Employed | Ref | |||
| Family history of mental illness | ||||
| Absent | 0.33 (0.186–0.585) | <0.001 | 0.46 (0.168–1.258) | 0.130 |
| Present | Ref | |||
| Family history of other medical conditions | ||||
| Absent | 0.58 (0.359–0.926) | 0.023 | 0.45 (0.192–1.071) | 0.071 |
| Present | Ref | |||
| Disease condition | ||||
| Leprosy | 2.67 (1.492–4.785) | 0.001 | 2.69 (0.972–7.459) | 0.057 |
| LF | 4.31 (2.330–7.985) | <0.001 | 9.50 (3.160–28.583) | <0.001 |
| Control | Ref | |||
| Well-being score | 0.75 (0.709–0.801) | <0.001 | 0.85 (0.780–0.917) | <0.001 |
| GAD-7 score | 1.82 (1.599–2.062) | <0.001 | 1.65 (1.374–1.068) | <0.001 |
COR = crude odds ratio, AOR = adjusted odds ratio, LF= lymphatic filariasis, Ref = reference.
In the qualitative aspect of the study, people with NTDs expressed concern for financial and economic needs, including free treatment. Respondents experienced social exclusion, discrimination, rejection, self-stigmatisation and emotional distress. In addition, several study respondents described suicidal ideation.
Social impacts of leprosy and LF
Social exclusion and discrimination
Common responses revealed social exclusion by members of families and the community: ‘This disease has separated me from people, I used to attend gatherings of all sorts and have fun but now not possible and so disheartening’ and ‘Our community members lack pleasure and joy to associate with us’. Statements such as ‘For me, this disease inhibited me from going to school’ indicated the degree of exclusion from key opportunities in their communities. Some experienced high levels of aggression and violence: ‘I had to pack and go to Kogi state because they burnt everywhere we were staying.’
Rejection from social roles
Respondents described rejection and an inability to fulfill expected social roles, including marriage: ‘It has affected me because the ladies that I wanted to marry decided to cut off from me because of this condition.’ Another respondent linked this directly to their disease symptoms: ‘when the swelling increased and I couldn't go close to people he left me and moved in with another woman.’
Self-stigmatisation
Many respondents experienced self-stigmatisation: ‘For some of us, we avoid even to mingle with people because you are different from others.’ Many restricted social participation as a result: ‘For some [of] us, we avoid even to mingle with people because you are different from others and by so doing, when you return to your room, you feel so sad.’
Economic effects of living with leprosy and LF
Difficulty in earning a living and loss of business
Having leprosy and LF was described as hindering the ability to earn a living: ‘These diseases have made us unable to engage in economic activities as much as we would have loved to.’ Even farming (the most common occupation in rural communities) can be difficult due to physical impairment: ‘I have also been prevented from working on my farm by this sickness especially when the ground is cold, as my entire body feels pain and not only the leg.’
Some who were previously engaged in business had to stop due to health challenges: ‘Even when I engage in hair making trade, the pain stops me from continuing hence I can hardly do anything.’ Social exclusion also reduced opportunities for economic activities: ‘I had to even stop trading as no one was patronizing me anymore.’
Mental health consequences of NTDs
Emotional distress, anxiety and depression
Common responses indicated that respondents were emotionally distressed as a result of the way they were treated by others because of NTD-related disabilities: ‘This has affected me so much that some nights I am unable to sleep because the people I used to carry out activities with have deserted me.’ Also: ‘I left the place angry and crying home, I wept for 3 days; I was so sad and angry.’
In some cases, these symptoms were recognised as being related to mental health: ‘All these experiences have bothered me so much that I have started acting like one with mental issues,’ though often respondents saw such distress as simply a natural consequence of the way they were treated or an inevitable consequence of their physical suffering.
Some respondents spoke about suicide ideation, despite this being a taboo topic in the local culture: ‘I have been wishing for death but it's not coming’ and ‘When people asked me, I told them I just want to die and end this suffering.’
Expressed priorities in relation to services
Basic needs and economic empowerment
Common responses revealed the need for money to enable the affordability of food and to take care of the family: ‘If you have enough money, you'll buy good food for you and your family’ and ‘What would most improve my life is to be physically sound and also have places to work instead of struggling endlessly to make ends meet.’ Respondents stated that if the facilities were to provide them with money, it would improve their quality of life by meeting basic needs and being able to engage in livelihood activities: ‘I pray to God to help me and give me a husband or money so that I can purchase a generator and a refrigerator to sell items and use the money for my upkeep, that way, I will be glad.’
Respondents also expressed a desire for free self-care products like toiletries to be provided: ‘So, if I have a small hospital that I can get money to eat and buy soap to bath that will be enough for me.’ Some respondents pointed to the fact that free treatment used to be provided but has stopped, making treatment unaffordable: ‘Since I was young, I have been receiving treatment here for free. I never used to pay money but now money is required, so since I have nothing, how do I get well.’
The ToC and integrated service model
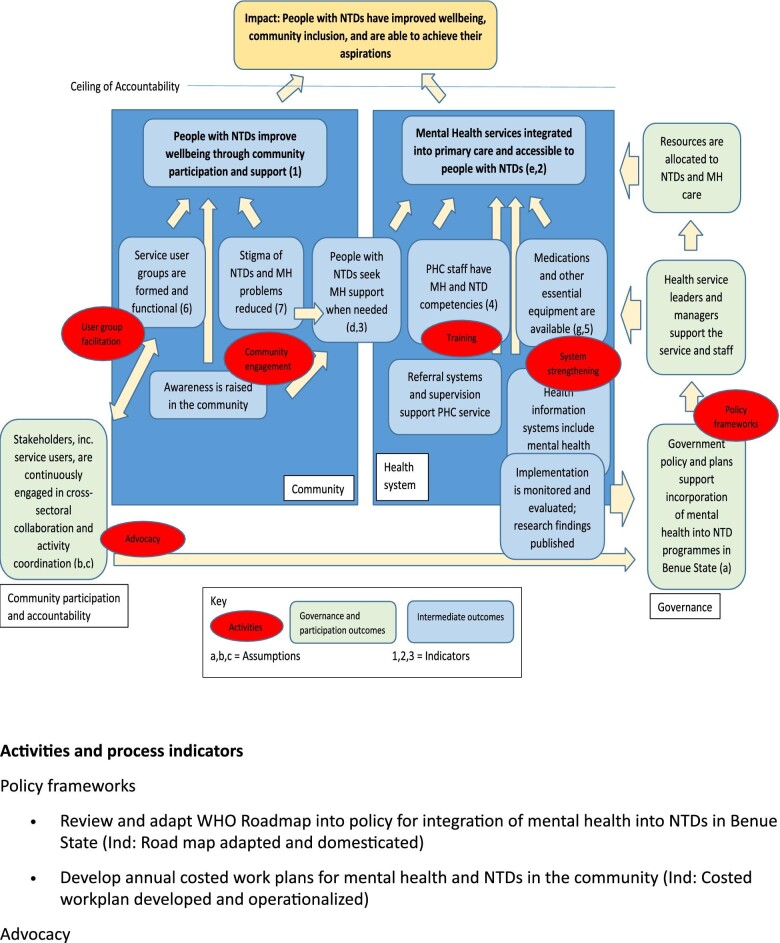
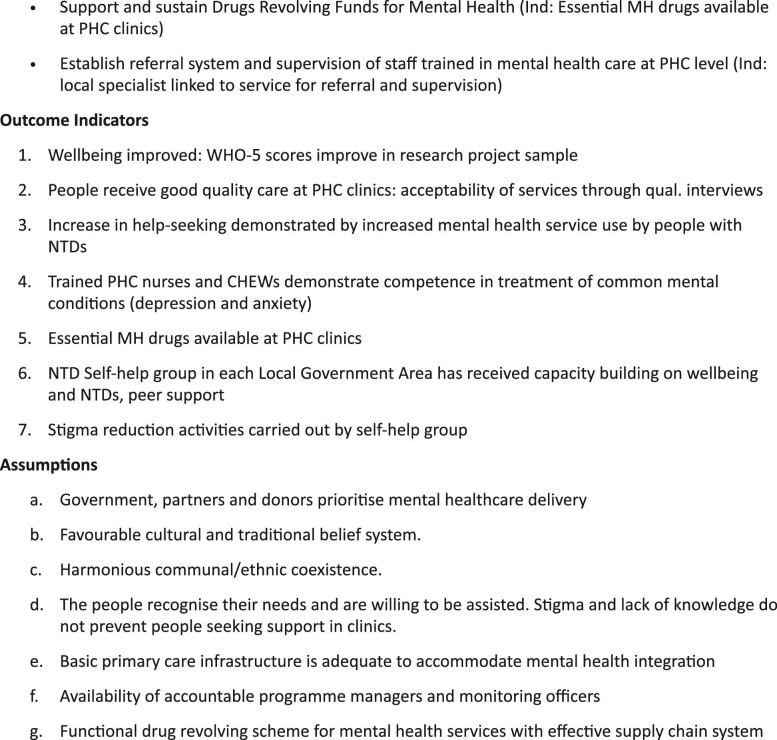
The ToC workshop was held by the study team and stakeholders in Benue State in February 2021. The participants for the 3-d workshop included state and local government (Gboko and Konshisha) NTD and mental health focal persons, primary healthcare workers, community leaders, representatives of persons affected by leprosy and LF, and family members. Following the workshop, the ToC map (Figure 2) was reviewed by a group of key stakeholders in an online workshop, including other researchers in mental health and NTDs (many from the NTD NGO Network), World Health Organisation NTD and Mental Health departments, and the Task Force for Global Health.
Figure 2.
Theory of Change for integration of mental health (MH) into NTD care and support. The ceiling of accountability refers to the point beyond which the intervention itself cannot claim attribution for the impact.
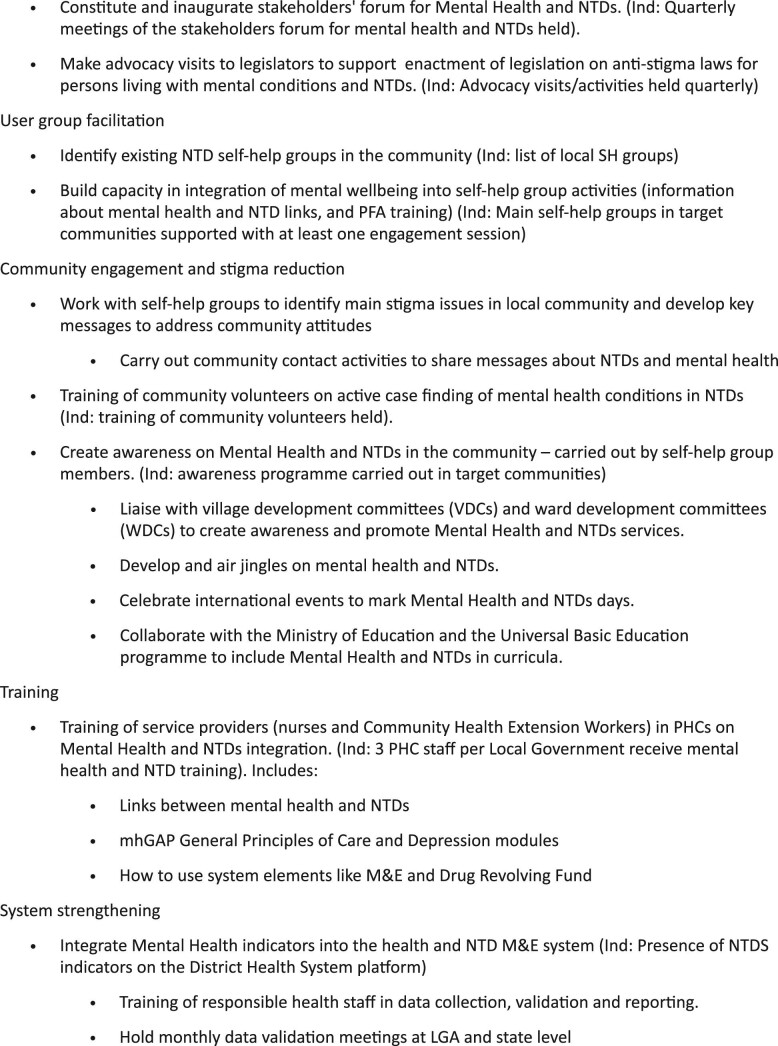
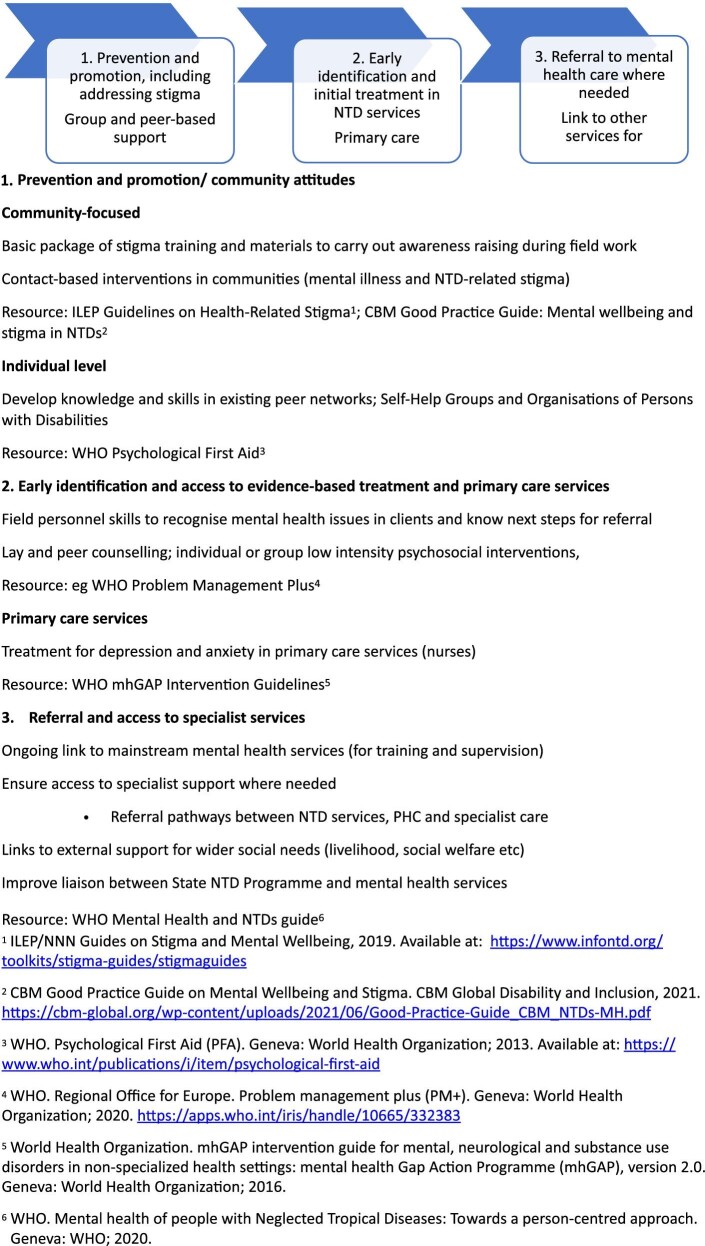
From this ToC and international normative guidance, an intervention model was derived (Figure 3). At the community level, the stakeholders advocated awareness creation to reduce associated stigma and for people with NTDs to be able to access mental health support without barriers. The critical role of the government in the formation of policy and plans and in resource allocation for NTDs and mental health was also noted. In order to bridge the gap in mental health and NTD services, capacity building for primary healthcare workers to acquire mental health and NTD competencies was recommended.
Figure 3.
Simple intervention model drawn from Theory of Change.
Limitations of the study
The short time frame of the research project meant that some of the system changes prioritised by the participants that require longer-term implementation could not be carried out. On the other hand, our choice of a location with strong existing relationships with the government and health service enabled us to mobilise existing resources (like a drug revolving fund run by the existing CCMHP). Given the core importance of sustainability, it is a weakness that we are unable to run the service for long enough to evaluate long-term impacts, though some assessment of this will be made in the evaluation, along with process indicators to assess systems change.
This research had the strength of close engagement with community stakeholders and people affected by NTDs, seeking to address their priorities in the process of the application of international normative guidance. The need to conform to the realities of local resource availability should lead to a feasible model but this means many expressed aspirations of service providers and users could be met, for example free services or the social security provision that were stated as a priority. This was a limitation of this intervention and study, and there was a relative lack of focus on understanding or addressing the needs and contribution of families and carers in relation to economic security or in relation to attitudes and stigma.
Discussion
We confirmed existing evidence showing a substantial increase in the prevalence of depression and anxiety in people with NTDs. The prevalence of depression measured in matched controls was surprisingly high, which may reflect either social deprivation in these communities or potentially a measurement affect. However, people affected by leprosy and LF still have significantly elevated rates of depression and anxiety and lower well-being scores. We found a strong correlation between PHQ-9, GAD-7 and WHO-5 Wellbeing Index, implying that a single measure might be an effective and practical screening tool for identification of those who require more support.
People affected by NTDs reported substantial social and economic impacts of living with NTDs, mediated by population beliefs, stigma and discrimination. This also extended to families and carers, who also experienced the economic hardship and social stigma associated with living with these conditions. These experiences and stigma from communities hostile to those with LF and leprosy share many characteristics found in other studies.24,25 This reaffirmed the importance of not only providing services, but also addressing population beliefs and stigma, as other studies have shown that stigma can result in avoidance of services.26
The expressed priorities for services centered on practical support for addressing financial needs, made worse by the recent reduction in practical and financial support previously available in the form of self-care items, and free healthcare. This was often expressed at the family level, rather than simply affecting individuals.
We found that this process enabled international evidence and normative guidance to be tailored to be appropriate and impactful in a local context, particularly being sensitive to user priorities. We feel that this process of seeking participant priorities and including a ToC process can be used elsewhere to align emerging international evidence with local needs. The finding that the measures we used correlated strongly means that a single basic measure (e.g. well-being) could be utilised as an efficient screen or measure of progress or change. While there is value in developing such tailored services, it remains the case that wider economic realities and stigmatising attitudes have a substantial impact that is difficult to mitigate with service provision alone. Greater focus on these social determinants, including wider family and community factors, is also likely to be important alongside service reform alone. We would concur with previous calls for future research in NTDs to include a broader perspective on the mental health and social aspects of these conditions,27 given the substantial increased impact on people's lives, beyond physical symptoms alone (Figures 1–3).
Figure 1.
Study area: Gboko and Konshisha Local Government Areas, Benue State, Nigeria.
Supplementary Material
Acknowledgements
The authors are grateful to the many people with lived experience of LF and leprosy who participated in the research, as well as staff of the health system in Benue State.
Contributor Information
Julian Eaton, CBM Global, and Centre for Global Mental Health, London School of Hygiene and Tropical Medicine, London, WC1E 7HT, UK.
Tolulope Afolaranmi, Department of Community Medicine, University of Jos, Plateau State, Nigeria.
Paul Tsaku, The Leprosy Mission Nigeria, Fort Royal Homes Estate, 12 King's Drive, 900102 Lugbe, Abuja, Nigeria.
Emeka Nwefoh, CBM Global Country Office, 8 Huambo Crescent, Wuse 7, 904101 Abuja, Nigeria.
Philip Ode, CBM Global Country Office, 8 Huambo Crescent, Wuse 7, 904101 Abuja, Nigeria; CBM UK, Cambridge, CB5 8HY, UK.
Theresa Baird, CBM UK, Cambridge, CB5 8HY, UK.
Pius Sunday, The Leprosy Mission Nigeria, Fort Royal Homes Estate, 12 King's Drive, 900102 Lugbe, Abuja, Nigeria.
Taiwo Obindo, Department of Psychiatry, University of Jos, Plateau State 930001, Nigeria.
Authors’ contributions
JE, EN, TB, TA and TO conceived the study and designed the study protocol; TO, EN, PO, JE and PT carried out the ToC workshop and training; TA, TO, JE and PT carried out analysis and all authors drafted the manuscript. All authors read and approved the final manuscript. JE and TO are guarantors of the paper.
Funding
This research is supported by the Coalition for Operational Research on NTDs (COR-NTD) [grant number NTD-SC #214D] through support from the UK Foreign, Commonwealth and Development Office.
Competing interests
JE and PAT are Guest Editors of this supplement but had no role in the review of this manuscript.
Ethical approval
Ethical approval was obtained from Jos University Teaching Hospital institutional human research ethics committee [JUTH/DCS/IREC/127/XXXI/2194] and Benue State University Teaching Hospital institutional human research ethics committee [BSUTH/MKD/HREC/2020/002] prior to the commencement of the study. In addition, we ensured that the state authorities were close collaborators in the research, as well as local organisations of people with leprosy and LF.
Data availability statement
The data underlying this article are available in the article and in its online supplementary material in analysed form. Raw data are available on reasonable request from the authors.
References
- 1. Bailey F, Eaton J, Jidda Met al. . Neglected tropical diseases and mental health: Progress, partnerships, and integration. Trends Parasitol. 2019;35(1):23–31. [DOI] [PubMed] [Google Scholar]
- 2. Litt E, Baker MC, Molyneux D. Neglected tropical diseases and mental health: A perspective on comorbidity. Trends Parasitol. 2012;28(5):195–201. [DOI] [PubMed] [Google Scholar]
- 3. Trania J-F, Ballard E, Peñac J. Stigma of persons with disabilities in Afghanistan: Examining the pathways from stereotyping to mental distress. Soc Sci Med. 2016;153:258–65. [DOI] [PubMed] [Google Scholar]
- 4. Abdulmalik J, Nwefoh E, Obindo Jet al. . Emotional difficulties and experiences of stigma among persons with lymphatic filariasis in Plateau State, Nigeria. Health Hum Rights. 2018;20(1):27. [PMC free article] [PubMed] [Google Scholar]
- 5. WHO . Ending the neglect to attain the Sustainable Development Goals: A road map for neglected tropical diseases 2021–2030. Geneva: World Health Organization; 2020. [Google Scholar]
- 6. WHO . Mental health of people with Neglected Tropical Diseases: Towards a person-centred approach. Geneva: WHO; 2020. [Google Scholar]
- 7. Patel V, Saxena S, Lund Cet al. . The Lancet Commission on global mental health and sustainable development. Lancet. 2018;392(10157):1553–98. [DOI] [PubMed] [Google Scholar]
- 8. Daniel OJ, Adejumo OA, Oritogun KSet al. . Spatial distribution of leprosy in Nigeria. Lepr Rev. 2016;87(4):476–85. [PubMed] [Google Scholar]
- 9. Eneanya OA, Fronterre C, Anagbogu Iet al. . Mapping the baseline prevalence of lymphatic filariasis across Nigeria. Parasites Vectors. 2019;12(1):1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Obindo T, Eaton J, Tsaku Pet al. . Integrated services for Neglected Tropical Diseases and mental health: Pilot study assessing acceptability, feasibility and attitudes in Benue State. Nigeria Int Health. (submitted) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. De Silva MJ, Breuer E, Lee Let al. . Theory of change: A theory-driven approach to enhance the Medical Research Council's framework for complex interventions. Trials. 2014;15(1):1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Neglected tropical disease elimination programme, national guidelines for lymphatic filariasis assessment with a framework for human capacity development. Neglected Tropical Diseases Division, Department of Public Health, Federal Ministry of Health, Abuja, Nigeria, 2019. [Google Scholar]
- 13. World Health Organization . Global Health Observatory. Geneva: World Health Organization; 2022. Available from: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/number-of-new-leprosy-cases [Accessed January 2023]. [Google Scholar]
- 14. Ibrahim T. Sample size determination: In research methodology and dissertation writing for health and allied health professionals. 1st ed. Abuja, Nigeria: Cress Global Link Limited; 2009. [Google Scholar]
- 15. Obindo J, Abdulmalik J, Nwefoh Eet al. . Prevalence of depression and associated clinical and socio-demographic factors in people living with lymphatic filariasis in Plateau State, Nigeria. PLoS Negl Trop Dis. 2017;11(6): e0005567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gureje O, Uwakwe R, Oladeji Bet al. . Depression in adult Nigerians: Results from the Nigerian Survey of Mental Health and Well-being. J Affect Disord. 2010;120(1-3):158–64. [DOI] [PubMed] [Google Scholar]
- 17. Martin A, Rief W, Klaiberg Aet al. . Validity of the brief patient health questionnaire mood scale (PHQ-9) in the general population. Gen Hosp Psychiatry. 2006;28(1):71–7. [DOI] [PubMed] [Google Scholar]
- 18. Spitzer RL, Kroenke K, Williams JBWet al. . GAD-7: A brief measure for assessing generalized anxiety disorder. Arch Intern Med. 2006;166:1092–7. [DOI] [PubMed] [Google Scholar]
- 19. Adewuya AO, Atilola O, Ola BAet al. . Current prevalence, comorbidity and associated factors for symptoms of depression and generalised anxiety in the Lagos State Mental Health Survey (LSMHS), Nigeria. Compr Psychiatry. 2018;81:60–5. [DOI] [PubMed] [Google Scholar]
- 20. Topp CW, Østergaard SD, Sondergaard Set al. . The WHO-5 Well-Being Index: A systematic review of the literature. Psychother Psychosom. 2015;84(3):167–76. [DOI] [PubMed] [Google Scholar]
- 21. Brandsma JW, Brakel WV. WHO ‘disability’ grading: Operational definitions. Lepr Rev. 2003;74(4):366–73. [PubMed] [Google Scholar]
- 22. Pani SP, Srividya A. Clinical manifestations of bancroftian filariasis with special reference to lymphoedema grading. Indian J Med Res. 1995;102:114–8. [PubMed] [Google Scholar]
- 23.[accessed January 2023]. https://opendatakit.org/
- 24. Caprioli T, Martindale S, Mengiste Aet al. . Quantifying the socio-economic impact of leg lymphoedema on patient caregivers in a lymphatic filariasis and podoconiosis co-endemic district of Ethiopia. PLoS Negl Trop Dis. 2020;14(3):e0008058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Somar PM, Waltz MM, van Brakel WH. The impact of leprosy on the mental wellbeing of leprosy-affected persons and their family members–a systematic review. Glob Mental Health. 2020;7:e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Perera M, Whitehead M, Molyneux Det al. . Neglected patients with a neglected disease? A qualitative study of lymphatic filariasis. PLoS Negl Trop Dis. 2007. ;1(2): e128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ton TG, Mackenzie C, Molyneux DH. The burden of mental health in lymphatic filariasis. Infect Dis Poverty. 2015;4(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available in the article and in its online supplementary material in analysed form. Raw data are available on reasonable request from the authors.