Abstract
Background
Worldwide, persons affected by skin Neglected Tropical Diseases (NTDs) may experience stigma and discrimination, which could lead to impaired societal functioning and poor mental wellbeing. Evidence of comorbidity of NTDs and mental health conditions is dominated by Leprosy, largely lacking in post-conflict areas, and rarely disaggregated by sex.
Methods
This cross-sectional survey is the first to explore depression, anxiety, stigma, and quality of life amongst people affected by Lymphatic Filariasis, Buruli Ulcer, Onchocerciasis or Leprosy in the Democratic Republic of the Congo. After a census through active case identification, the survey was completed by 118 persons (response rate 94.4%).
Results
In total, 58.3% of men and 80.0% of women screened positive for major depressive disorder (PHQ-9). Symptoms indicative of generalised anxiety disorder (GAD-7) were displayed by 54.8% of men and 62.2% of women. Being female, having a disability, experiencing stigma and lower physical quality of life were predictors of depression. Anxiety was predicted by age, physical quality of life, disability (for men only) and environmental quality of life (for women only).
Conclusions
Integrated, intersectoral and gender-sensitive initiatives are needed to respond to the many biopsychosocial challenges that persons affected face.
Contexte
Dans le monde entier, les personnes atteintes de maladies tropicales négligées (MTN) peuvent faire l'objet d'une stigmatisation et d'une discrimination, ce qui peut entraîner une altération du fonctionnement de la société et un mauvais bien-être mental. Les preuves de la comorbidité des MTN et des troubles de la santé mentale sont dominées par la lèpre, manquent largement dans les zones post-conflit et sont rarement ventilées par sexe.
Méthodes utilisées
Cette enquête transversale est la première à explorer la dépression, l'anxiété, la stigmatisation et la qualité de vie chez les personnes atteintes de filariose lymphatique, d'ulcère de Buruli, d'onchocercose ou de lèpre en République démocratique du Congo. Après un recensement par identification active des cas, 118 personnes ont répondu à l'enquête (taux de réponse 94,4%).
Résultats
Au total, 58,3% des hommes et 80,0% des femmes ont été dépistés positifs pour un trouble dépressif majeur (PHQ-9). Des symptômes indiquant un trouble anxieux généralisé (GAD-7) ont été observés chez 54,8 % des hommes et 62,2 % des femmes. Le fait d'être une femme, d'avoir un handicap, d'être stigmatisé et d'avoir une qualité de vie physique inférieure était un facteur prédictif de la dépression. L'anxiété était prédite par l'âge, la qualité de vie physique, le handicap (pour les hommes uniquement) et la qualité de vie environnementale (pour les femmes uniquement).
Conclusions
Des initiatives intégrées, intersectorielles et sensibles au genre sont nécessaires pour répondre aux nombreux défis biopsychosociaux auxquels sont confrontées les personnes touchées.
Antecedentes
En todo el mundo, las personas afectadas por Enfermedades Tropicales Desatendidas (ETD) cutáneas pueden sufrir estigmatización y discriminación, lo que podría conducir a un deterioro del funcionamiento social y a un bienestar mental deficiente. La evidencia científica sobre la comorbilidad de las ETD y las afecciones mentales está dominada por la lepra, en general insuficiente en zonas post-conflicto y rara vez se desglosan por sexo.
Métodos
Esta encuesta transversal es la primera que explora la depresión, la ansiedad, el estigma y la calidad de vida entre las personas afectadas por la filariasis linfática, la úlcera de Buruli, la oncocercosis o la lepra en la República Democrática del Congo. Tras un censo mediante identificación activa de casos, la encuesta fue completada por 118 personas (tasa de respuesta del 94,4%).
Resultados
En total, el 58,3% de los hombres y el 80,0% de las mujeres arrojaron resultados positivos para el trastorno depresivo mayor (PHQ-9). El 54,8% de los hombres y el 62,2% de las mujeres presentaban síntomas indicativos de trastorno de ansiedad generalizada (TAG-7). Ser mujer, tener una discapacidad, sufrir estigmatización y una menor calidad de vida física fueron factores predictivos de la depresión. La edad, la calidad de vida física, la discapacidad (sólo en el caso de los hombres) y la calidad de vida ambiental (sólo en el caso de las mujeres) fueron factores predictivos de la ansiedad.
Conclusiones
Se necesitan iniciativas integradas, intersectoriales y con perspectiva de género para responder a los numerosos retos biopsicosociales a los que se enfrentan las personas afectadas.
Keywords: Democratic Republic of the Congo, mental health, neglected tropical diseases, quality of life, stigma
Introduction
Neglected tropical diseases (NTDs) impose a human, social and economic burden on >1 billion people worldwide. Currently, the WHO recognises a diverse set of 20 communicable and non-communicable diseases and disease groups as NTDs. As ‘diseases of poverty’, NTDs are most endemic in low- and middle-income countries, where they often affect the poorest and most marginalised communities.1 At least 10 NTDs—including leprosy, lymphatic filariasis (LF), Buruli ulcer (BU) and onchocerciasis—initially present with changes and lesions on the skin. Skin NTDs can lead to irreversible, chronic symptoms and the pathology often includes physical disability and permanent disfigurement.2 This, in combination with stigmatisation and discrimination, negatively impacts the ability of many affected people to complete livelihood activities and participate fully in society. Consequently, evidence consistently shows high levels of psychological co-morbidity among populations affected by skin NTDs.3
NTDs and mental health conditions share many common social and structural causes. For example, a recent study in Liberia found that the postconflict environment left people vulnerable to the chronic effects of NTDs as a result of weak health and social systems alongside other general stressors (e.g. precarious livelihoods).4 General stressors may affect all people and create vulnerability to NTD infection and/or mental ill health. However, when mediated by stigma and discrimination, general stressors particularly affect people living with NTDs, creating a risk environment for exacerbated physical morbidity and mental distress.4,5 Frequently, the impact of these experiences is further shaped by intersecting axes of inequity, including age, gender and generation, which influence vulnerability and experience of NTDs, as well as an individual's ability to access care.6 The links between a range of biosocial factors associated with skin NTDs, reduced quality of life (QoL) and emotional well-being are increasingly recognised and supported by empirical evidence in some settings. However, the overall evidence base of the impact of NTDs and their associated physical disabilities and stigma on people's QoL and mental well-being remains patchy. Accurate data are urgently needed to inform advocacy and planning for interventions, services, monitoring and evaluation and funding.7 Currently, the evidence base is particularly sparse in postconflict or conflict-affected settings, mainly dominated by leprosy, and heterogeneous in terms of instruments used for assessment.3,8 In addition, while the literature shows that women affected by NTDs are at a higher risk of poor mental health outcomes,3 sex-disaggregated explorations of the impact of biopsychosocial factors on mental health are largely lacking. Fully understanding the negative psychological and social manifestations of NTDs and how these are shaped by gender is of critical importance when considering hypothesised co-morbidities between mental health and NTDs, particularly as constructions of mental health, often vary significantly between men and women.9
The Democratic Republic of the Congo (DRC) has a high prevalence of several major NTDs, largely resultant from decades of conflict and precarious health infrastructure. Although limited data exist, it is hypothesised that the DRC may have the most leprosy cases in Africa, and the second highest prevalence of LF. Despite NTDs having a huge public health importance in the DRC, little is known about their impacts and successful management strategies.10 Within Kasai Province, DRC, from 2016 to 2019, a violent conflict took place, which at its height led to thousands of deaths and >1 million people being displaced. Although it has largely subsided, the conflict left widespread destruction and destitution, with schools and health centres destroyed, and further exacerbated pre-existing food insecurity and livelihood crises. There is a profound gender crisis in most parts of the province. Many women are de-facto heads of households and providers for their children, because men are often absent in diamond mines and often have multiple wives. Gender-based violence, which was common before the conflict, increased during the conflict as it was used by armed groups on all sides.11 Professional psychosocial services are virtually non-existent. The Leprosy Mission DRC is currently working in Kasai Province and other areas of the DRC to support people affected by leprosy and other skin NTDs, but have identified a critical gap in being able to support the mental health needs of affected people.
In response to these knowledge gaps, this paper quantitatively explores depression and anxiety and their associations with stigma, disability and QoL in people affected by skin NTDs and conflict in Kasai Province, DRC, using a sex-disaggregated analysis. This investigation forms part of a larger, mixed-method study that aims to develop and evaluate a community-based mental health intervention for people affected by skin NTDs. The intervention design process is documented in M. Nganda et al. (manuscript submitted), also within this special supplement.
Materials and Methods
Participants and recruitment
This cross-sectional survey study took place in Ngombe (population: approximately 19 300) and Tshisele (population: approximately 13 600) health areas within Tshikapa Health Zone, Kasai Province, DRC. Four skin NTDs—leprosy, LF, BU and onchocerciasis—are endemic in these areas.12,13 Any person aged >18 y who presented with morbidity associated with any of these diseases was eligible to participate. Data collectors were overseen by staff from the DRC branch of The Leprosy Mission, a global organisation that aims to eradicate leprosy and support those affected. To identify eligible participants, a census of NTD patients in both health areas was completed. Health centre records were searched and a process of active case finding identified a total population of 125 affected people across both health areas. Data collection took place during April 2022. Because of low literacy rates, data collectors described information sheets verbally. Informed consent was recorded, via signature or fingerprint. The survey was administered verbally and directly entered in a tablet using Redcap software (Vanderbilt University, Nashville, Tennessee, USA). A total of 118 people completed the survey (94.4% response rate). Non-respondents refused to participate, had died or had recently moved out of the study area.
Measurements
In addition to questions that captured sociodemographic data, the survey consisted of five questionnaires, most of which were taken from the cross-NTD Morbidity and Disability Toolkit.
The Washington Group Short Set (WGSS) was used to screen for levels of disability. This six-item scale asks participants to what extent they have difficulty seeing, hearing, walking, remembering/concentrating, caring for themselves and communicating.14 The Sari Stigma Scale was used to assess stigma. The scale has 21 items and captures four stigma domains: experienced, internalised and anticipated stigma, as well as disclosure concerns.15 To measure QoL, the WHO-QoL BREF was used. Comprising 26 items, this tool measures the domains of physical health, psychological health, social relationships and environment.16 The Patient Health Questionnaire (PHQ-9) was used to screen for depression. It is made up of nine Likert-scale questions, which align with the Diagnostic and Statistical Manual of Mental Disorders criteria for major depressive disorder.17 The total PHQ-9 score was used to categorise the severity of depression into mild,5–9 moderate,10–14 moderately severe15–19 or severe.20–27 The standard cut-off score of ≥10 was used as being indicative of a major depression disorder. Finally, to measure anxiety, the Generalised Anxiety Disorder Questionnaire (GAD-7) was administered. The total score on this seven-item instrument was used to categorise mild,5–9 moderate10–14 or severe (≥15) anxiety. A score of ≥10 was used as a cut-off score for possible generalised anxiety disorder.18
Questionnaires were translated and back-translated from English into French. Supported by the team, a priest and a teacher from the local communities translated between French and Tshiluba, the national language and back-translated to minimise any discrepancies. The Tshiluba survey was then piloted in the communities before finalisation. A minor adaptation to the PHQ-9 was made to reflect the local context: item 7, ‘Trouble concentrating on things such as reading newspaper and watching television’, was amended to incorporate more relevant examples, specifically ‘listening to radio or church service’.
Data analysis
Data analysis was completed using R software.19 Descriptive analysis was used to present sex-disaggregated data on stigma, QoL, PHQ-9 and GAD-7, with prevalence and 95% CIs calculated using recommended cut-off scores where relevant. Reliability of measurement scales was explored using Cronbach's alpha. Mann–Whitney tests were used to explore differences between sexes in stigma and QoL scores; Z-tests examined differences between proportions of prevalence of depression and anxiety for both sexes. To identify differences between the NTD population and general population, one sample t tests were undertaken, which used the general population prevalence as a fixed value. Multivariable linear regression was applied to examine whether stigma, disability and QoL served as predictors for poor mental health. Interaction effects between these predictors and sex were explored. All variables were entered simultaneously.
Results
Table 1 shows the characteristics of the 118 participants who were identified as having morbidity associated with LF (e.g. lymphoedema) (46.6%), onchocerciasis (e.g. blindness) (26.3%), BU (20.3%) or leprosy (e.g. shortening of extremities) (6.8%). Men constituted the largest proportion of the sample (61.9%). The average age was 49.7 (SD=16.7, range=19–79) y. The largest proportions of men and women worked in agriculture. Approximately 29% of women and 8% of men were unemployed/unable to work. Used as a proxy for disability, 74.0% of men and 75.6% of women reported activity limitations (WGSS≥3). Limitations in the mobility domain were most frequently reported, followed by self-care and concentration difficulties (Supplementary Table 1).
Table 1.
Sample characteristics
| Characteristic | Total, N (%) | Women, N (%) | Men, N (%) |
|---|---|---|---|
| Total | 118 (100) | 45 (38.1) | 73 (61.9) |
| Type of NTD | |||
| Lymphatic filariasis | 55 (46.6) | 20 (44.4) | 35 (47.9) |
| Onchocerciasis | 31 (26.3) | 9 (20.0) | 22 (30.1) |
| Buruli ulcer | 24 (20.3) | 14 (31.1) | 10 (13.7) |
| Leprosy | 8 (6.8) | 2 (4.4) | 6 (8.2) |
| Age | |||
| Mean (in y) | 49.7 (SD 16.7) | 48.4 (SD 16.3) | 50.5 (SD 17.0) |
| Source of income | |||
| Agriculture | 53 (44.9) | 23 (51.1) | 30 (41.1) |
| Day work | 27 (22.9) | 2 (4.4) | 25 (34.2) |
| Small enterprise | 9 (7.6) | 6 (13.3) | 3 (4.1) |
| Private employment | 3 (2.5) | 0 (0) | 3 (4.1) |
| Civil servant | 4 (3.4) | 1 (2.2) | 3 (4.1) |
| Unemployed | 19 (16.1) | 13 (28.9) | 6 (8.2) |
| Other | 3 (2.5) | 0 (0) | 3 (4.1) |
| Disability | |||
| Disability | 88 (74.6) | 34 (75.6) | 54 (74.0) |
Stigma and QoL
The mean stigma score was 39.5 (SD=14.1, 95% CI 36.9 to 42.0) out of a maximum of 63. The Cronbach's alpha for the overall scale was 0.87, indicating a high level of internal consistency. However, reliability was unsatisfactory for the disclosure concerns domain. Although participants reported high levels of stigma in all domains, the mean-per-item scores were highest in the internalised and anticipated stigma domains (Table 2). The five items with the highest scores were also found in these domains, with the majority of patients often/always feeling embarrassed (81.4%); feeling unclean (72.0%); feeling like NTD patients are a nuisance (69.5%); feeling like NTD patients are disgusting (68.6%); or feeling like a bad person (67.8%) (Supplementary Table 2). No significant differences were found between stigma levels reported by men and women.
Table 2.
Levels of stigma and quality of life, sex-disaggregated
| Overall | Mean per item | Men | Women | Mann–Whitney | |
|---|---|---|---|---|---|
| Domain | M (SD) | M (SD) | M (SD) | M (SD) | U test |
|
Stigma (Sari scale)
Total score (max. 63) |
39.46 (14.1) | 39.9 (13.9) | 38.8 (14.4) | U= n.s. | |
| Experienced stigma (max. 21) (α=0.88) |
11.02 (7.3) | 1.57 (1.05) | 11.12 (7.5) | 10.84 (7.2) | U= n.s. |
| Disclosure concerns (max. 12) (α=0.48) |
5.92 (3.3) | 1.48 (0.82) | 5.70 (3.3) | 6.27 (3.3) | U= n.s. |
| Internalised stigma (max. 18) (α=0.70) |
13.55 (4.3) | 2.26 (0.72) | 13.77 (4.4) | 13.20 (4.2) | U= n.s. |
| Anticipated stigma (max. 12) (α=0.73) |
8.97 (3.4) | 2.24 (0.85) | 9.30 (3.2) | 8.44 (3.7) | U= n.s. |
|
Quality of life
(WHO QoL BREF) |
|||||
| Physical (α=0.61) |
33.3 (16.7) | 33.71 (17.3) | 32.54 (15.8) | U=n.s. | |
| Psychological (α=0.30) |
49.4 (18.6) | 55.59 (16.7) | 39.26 (17.2) | U=799.5, p<0.001 | |
| Social (α=0.16) |
55.7 (19.6) | 58.79 (19.5) | 50.74 (18.8) | U=1263.0, p=0.03 | |
| Environmental (α=0.31) |
37.9 (14.0) | 38.78 (15.4) | 36.39 (11.3) | U=n.s. |
Table 2 also presents the mean and SD scores of QoL domains, with women reporting significantly lower psychological and social QoL than men. Further significant differences in individual item responses between sexes are highlighted in Supplementary Table 3. Most men (68.5%) and women (75.6%) rated their QoL as (very) poor. With regard to psychological QoL specifically, 67.1% of men and 73.3% of women stated ‘not at all’ when asked how much they enjoyed their life; 24.7% of men and 48.9% of women reported that they ‘always’ experienced negative feelings. While the reliability of the overall scale was acceptable (α=0.74), it was unsatisfactory for the psychological, social and environmental domains (Table 2).
Prevalence of depression and anxiety
As seen in Table 3, the mean PHQ-9 score was 13.23 (SD=6.97, range 0 to 26). Internal consistency was good (α=0.81). Using a cut-off score of ≥10, more women (80.0%) were classed as having symptoms indicative of major depressive disorder than men (58.3%). A significant association between sex and depression was found (χ2(1)=5.85, p=0.016). Notably, 45.8% of men and 66.7% of women (χ2(1)=4.84, p=0.028) reported having thoughts about being better off dead or harming themselves. A comparison with reported mental health prevalence data from the general population in the same area (M. Seekles et al., manuscript submitted) showed that PHQ-9 scores were significantly higher in the NTD population for both men (M=7.59 vs M=12.11, t(71)=5.10, p<0.001) and women (M=9.52 vs M=15.02, t(44)=6.55, p<0.001).
Table 3.
Mental health outcomes, sex-disaggregated
| Overall | Men (n=73) | Women (n=45) | |||||
|---|---|---|---|---|---|---|---|
| MH outcome | Mean (SD) | % (N) | Mean (SD) | % (N) | Mean (SD) | % (N) | |
| Depression (PHQ-9) (n=117) | |||||||
| Mean (SD) | 13.23 (6.97) | 12.11 (0.89) | 15.02 (5.64) | U=1243.5, p=0.035 | |||
| Major depression (≥10) | 66.7 (78) | 58.3 (42) | 80.0 (36) | χ2(1)=5.85, p=0.016 | |||
| None (0–4) | 15.4 (18) | 21.9 (16) | 4.4 (2) | ||||
| Mild (5–9) | 17.9 (21) | 19.2 (14) | 15.6 (7) | ||||
| Moderate (10–14) | 20.4 (24) | 19.2 (14) | 22.2 (10) | ||||
| Moderately severe (15–19) | 23.1 (27) | 16.4 (12) | 33.3 (15) | ||||
| Severe (20–27) | 23.1 (27) | 21.9 (16) | 24.4 (11) | ||||
| Anxiety (GAD-7) (n=118) | |||||||
| Mean (SD) | 10.61 (5.25) | 10.19 (5.5) | 11.29 (4.76) | U=n.s. | |||
| Anxiety (≥10) | 57.6 (68) | 54.8 (40) | 62.2 (28) | χ2=n.s. | |||
| None (0–4) | 18.6 (22) | 26.0 (19) | 6.7 (3) | ||||
| Mild (5–9) | 23.7 (28) | 19.2 (14) | 31.1 (14) | ||||
| Moderate (10–14) | 28.8 (34) | 27.4 (20) | 31.1 (14) | ||||
| Severe (>15) | 28.8 (34) | 27.4 (20) | 31.1 (14) | ||||
The mean GAD-7 score was 10.61 (SD=5.25, range 0 to 20) and 57.6% of patients displayed symptoms of moderate or severe anxiety (scoring ≥10) indicative of general anxiety disorder; univariate analysis revealed no significant difference in anxiety scores between men and women. Internal consistency for the GAD-7 was acceptable (α=0.75). Mean GAD-7 scores were significantly higher than those reported in the general population for men (M=10.19 vs M=6.69, t(71)=5.43, p<0.001) and women (M=11.29 vs M=7.41, t(44)=5.46, p<0.001).
Several multivariable linear regression models were run to explore biopsychosocial predictors (including age, sex, disability, employment status, total stigma score and QoL domains) of mental distress (depression and anxiety), and the moderating effects of sex. Table 4 presents an overview of relevant models (for a full list of all models, see Supplementary Tables 4 and 5). Being female, having a disability, experiencing higher stigma and lower physical QoL were found to be significant predictors of depression. No interactions were found between sex and disability, stigma and QoL. Anxiety was significantly predicted by higher age and lower physical QoL. Significant interaction effects showed that disability only predicted increased anxiety for men; women experienced high anxiety levels regardless of disability (Figure 1). Further, lower environmental QoL only predicted anxiety for women. Further regression analysis showed that an association between social QoL and anxiety in these models was merely due to the modelling strategy.
Table 4.
Selection of multivariable linear regression models for predictors of depression and anxiety
| Anxiety (n=118) | ||||
|---|---|---|---|---|
| Depression (n=117) Model 1 | Model 1 | Model 2 | Model 3 | |
| Predictor | b (SE) | b (SE) | b (SE) | b (SE) |
| Intercept | 5.48 (4.58) | 10.31 (3.58) | 8.60 (3.53) | 7.98 (3.61) |
| Age | −0.05 (0.04) | −0.06 (0.03)** | −0.08 (0.03)*** | −0.06 (0.03)** |
| Employed (ref: no) | 1.96 (1.69) | 0.36 (1.32) | 0.99 (1.30) | 0.12 (1.29) |
| Disability (ref: no) | 4.60 (1.44)*** | 3.33 (1.11)*** | 5.54 (1.34)*** | 3.58 (1.09)*** |
| Sex (ref: male) | 3.22 (1.35)** | 1.09 (1.06) | 5.33 (1.83)*** | 8.06 (2.91)*** |
| Stigma | 0.11 (0.05)** | 0.03 (0.04) | 0.04 (0.04) | 0.03 (0.04) |
| QoL: Physical | −0.08 (0.04)* | −0.08 (0.03)** | −0.07 (0.03)** | −0.08 (0.03)** |
| Qol: Psychological | 0.03 (0.04) | −0.003 (0.03) | −0.01 (0.03) | 0.01 (0.03) |
| QoL: Social | 0.04 (0.03) | 0.05 (0.03)* | 0.05 (0.03)* | 0.05 (0.03)** |
| QoL: Environmental | −0.01 (0.05) | −0.02 (0.04) | −0.003 (0.04) | 0.02 (0.04) |
| Disability*Sex | −5.94 (2.13)*** | |||
| QoL: Environmental*Sex | −0.18 (0.07)** | |||
***p<0.001; **p<0.01; *p<0.05.
Figure 1.
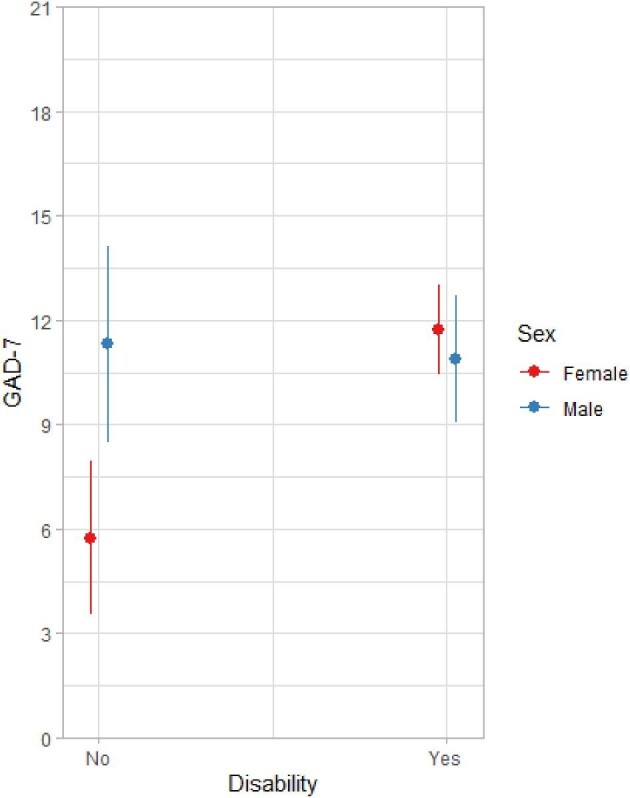
Interaction effect between disability and sex for anxiety.
Because of the small sample size of leprosy patients, NTD type was not added as a predictor in the regression models. As seen in Table 5, levels of depression and anxiety among leprosy patients appear lower than those in people affected by other NTDs.
Table 5.
Mental health outcomes by disease type
| PHQ-9 | GAD-7 | |
|---|---|---|
| Type of NTD | M (SD) | M (SD) |
| Lymphatic filariasis (n=54) | 13.87 (6.9) | 10.84 (5.3) |
| Onchocerciasis (n=31) | 13.13 (6.9) | 10.65 (5.2) |
| Buruli ulcer (n=24) | 13.75 (7.2) | 11.42 (5.3) |
| Leprosy (n=8) | 7.75 (5.1) | 6.25 (3.2) |
Discussion
Overall, the data portray a challenging situation, with reports of high levels of stigma, low QoL and high prevalence rates of depression and anxiety among people affected by skin NTDs in Kasai Province. The mean PHQ-9 score was 13.2 and 67% of participants fit the screening classification for major depressive disorder. Approximately 85% of our sample reported at least mild depressive symptoms. With regard to anxiety, the mean GAD-7 score was 10.6 and 57.6% of respondents were classed as having symptoms indicative of generalised anxiety disorder. These figures are noticeably higher than most previous studies with people affected by skin NTDs in other sub-Saharan countries. For example, two studies that also used the PHQ-9 in patients with podoconiosis or lower limb lymphoedema in Cameroon20 and Rwanda21 found mean scores of 3.5 (with 3.6% ≥10) and 7.4 (with 33.3% ≥10), respectively. Studies that used different measures with BU patients in Benin22 and Ghana23 and LF patients in Nigeria24 reported prevalence rates of 32%, 27% and 20%, respectively. A study in Togo reported levels that were more similar to those in our study, with 70% of lymphoedema patients at risk of depression.25 Three studies that assessed anxiety in leprosy patients in Nigeria and BU patients in Benin found prevalence rates of approximately 19%.22,26,27 Stigma levels were higher than those found in Ethiopian leprosy and LF patients28 and Indonesian leprosy patients,29 who reported average scores of 24 and 22, respectively. Irrespective of these differences, our study and those conducted elsewhere emphasise the critical need for the development of strategies that can support the mental well-being of people affected by NTDs. In the DRC context, our findings suggest that affected people may self-stigmatise more than they are stigmatised by the wider community, although high levels of experienced stigma were also reported. A significant association between higher levels of depression and an increased level of stigma might, in part, explain the high prevalence of depression in our sample. This signifies the need for the development of context-specific stigma reduction interventions that work specifically with people affected by NTDs and the wider community, to address the multiple domains of stigma that are negatively impacting mental health. Our findings are consistent with multiple studies that have shown that skin NTDs and their related symptoms predispose those affected to stigma and other biopsychosocial problems that harm QoL.3
Comparisons with the general population in the province found lower QoL and higher levels of mental distress among NTD-affected people (M. Seekles et al., manuscript submitted). These levels of distress were also higher than those found in other populations in other areas of the DRC.30–33 Still, the small number of identified studies in the DRC reported higher prevalence rates than most of the above NTD studies in other sub-Saharan countries. The broader social and structural drivers of health in Kasai as well as the recent insurgence of conflict in this area may explain this finding. Our participants face multiple burdens of being affected by an NTD, but also living in a postconflict setting with high rates of poverty, insecurity and gender inequitable attitudes. Thus, considering the broader context of our participants’ lives in the interpretation of our findings is critically important. Our data indicate that biosocial factors may impact the mental health of men and women differently. For men, anxiety was predicted by having a disability and correlated with physical QoL, while for women anxiety was high regardless of disability. Instead, it correlated with environmental QoL, which includes aspects of personal safety, financial security and access to health services, among others. In addition, women experienced higher levels of depression than men. Although our study was unable to disentangle the causal pathways of mental health challenges and we did not measure experiences and consequences of conflict (e.g. post-traumatic stress disorder) or gender inequitable attitudes (e.g. gender-based violence), we know that these factors are independently related to poor mental health.34 Co-occurrence of these factors can contribute to increased vulnerability to NTD- and mental health-related morbidity and mortality; complex pathways that have also been identified in other postconflict settings, for example, in Liberia.4 While our data suggest that having an NTD is a risk factor for mental health conditions, the relationship between NTDs and mental health is likely bi-directional.3 Intersectoral, person-centred integrated support that targets a broad range of shared social determinants for NTDs and mental health, in addition to caring for those affected,35 is therefore recommended. The WHO intervention pyramid for integrating NTDs and mental health should guide the development of such a system of support.35 When using data such as those presented here to plan for service delivery, it is important to consider that self-reported and symptom-based measurement tools may overestimate the prevalence rates of depression and anxiety by 1.5 to 2 times.36 Many participants who screen positive may instead be displaying normal, temporary responses to stressful circumstances that do not require treatment. Community-based initiatives—such as peer support groups and stigma-reduction activities—may be able to alleviate some distress, although further research into this is needed.3,37 However, even when halving the current prevalence rates, the data in this paper still highlight a pressing need for increased holistic, professional psychosocial service delivery at primary, secondary and/or tertiary levels of care.
We believe that through our active case-finding efforts, we have successfully surveyed a large proportion of people living with NTDs in the area, resulting in a representative sample. Because many people affected are not necessarily known to the formal health system, we believe that this is a significant strength of the study. As was our sex-disaggregated analysis, which provided further evidence of the differential impact of biopsychosocial factors on men and women. As a limitation, the survey did not capture the severity of disease or time since onset. If we had measured this, we might have been able to better explain the finding that leprosy patients appeared to have lower levels of disability, depression and anxiety than those affected by other NTDs. We believe that this may be due to the well-established work of The Leprosy Mission in the area, which means that leprosy patients are potentially identified, treated and supported at an earlier stage along the disease pathway than those living with other NTDs. Another surprising finding is that we found no correlation between the psychological QoL domain and the PHQ-9 or GAD-7 scores, which raised questions regarding the validity of the tools. Internal consistency of the PHQ-9 and GAD-7 was acceptable, but low for the domains of the WHO-QoL-BREF—and much lower than reported during WHO development of the tool.16 A study in Colombia also found that the latter questionnaire was not easily understood by a majority of participants.38 However, a study among Ebola survivors in the DRC found good internal consistency for the domains.39 While the tools in this study were recommended in the NTD toolkit and adapted following a translation and piloting process, evidence of cultural transferability of these tools remains limited. An in-depth quantitative examination of validity of the tools (using data from NTD-affected people and the general population) is currently underway and will hopefully shed further light on this.
Conclusion
People affected by skin NTDs in Kasai Province, DRC, report a low QoL and high levels of stigma, depression and anxiety. An integrated, intersectoral and gender-sensitive response is needed to address the many biopsychosocial challenges that this population faces.
Supplementary Material
Acknowledgements
The authors would like to thank Dr Lucas Sempe for his support with data analysis. In addition, we would like to thank Benoit Tshishiku, Clement Mukendi, Antoinette Mbokashanga, Naomie Sengu, Atishimen Bakamba, Florance Ntumba, Dimuenayi Marcelo, Garcia Chita, Clement Kande and Didier Mubudi for their contributions to the data collection process.
Contributor Information
Maaike L Seekles, Liverpool School of Tropical Medicine, Department of International Public Health, Pembroke Place, Liverpool L3 5QA, UK.
Jacob K Kadima, The Leprosy Mission DRC, Kinshasa, Democratic Republic of the Congo.
Yan Ding, Liverpool School of Tropical Medicine, Department of International Public Health, Pembroke Place, Liverpool L3 5QA, UK.
Christian B Bulambo, The Leprosy Mission DRC, Kinshasa, Democratic Republic of the Congo.
Joy J Kim, Effect: Hope, Program Team, Markham, ON L3R 6G1, Canada.
Junior K Kukola, The Leprosy Mission DRC, Kinshasa, Democratic Republic of the Congo.
Pierre O L Omumbu, The Leprosy Mission DRC, Kinshasa, Democratic Republic of the Congo.
Raphael M Mulamba, The Leprosy Mission DRC, Kinshasa, Democratic Republic of the Congo.
Motto Nganda, Liverpool School of Tropical Medicine, Department of International Public Health, Pembroke Place, Liverpool L3 5QA, UK.
Stephanie M Ngenyibungi, University of Kinshasa, Department of Psychology, Kinshasa H8J56PX, Democratic Republic of Congo.
Florent L Ngondu, Ministry of Health, Leprosy Programme, Kinshasa, M8R29W2, Democratic Republic of Congo.
Louis P Sabuni, The Leprosy Mission DRC, Kinshasa, Democratic Republic of the Congo.
Laura Dean, Liverpool School of Tropical Medicine, Department of International Public Health, Pembroke Place, Liverpool L3 5QA, UK.
Authors’ contributions
The authors wish it to be known that, in their opinion, MLS and JK Kadima should be regarded as joint first authors. LD and LPS conceived the study; LD, LPS, JK Kadima, YD, JJK, CBB, JK Kukola, POL, MN, FLN and RMM designed the study protocol; JK Kadima, CBB, JK Kukola, POL, RMM, SMN and LPS coordinated the data collection; MLS, JK Kadima, YD and LD completed the analysis and interpretation of these data. MLS and JK Kadima drafted the manuscript; LD critically revised the manuscript for intellectual content. All the authors commented on and contributed to draft revisions, read and approved the final manuscript. MLS, JK Kadima and LD are guarantors of the paper.
PPI Statement
This publication is one outcome from a community-based participatory research study. This means that community members and people with lived experience (peer-researchers) of NTDs and mental health conditions were involved in study design, data collection and analysis. Findings were shared back to peer researchers to support with interpretation and intervention development, as described in M. Nganda et al. (forthcoming, also in this supplement).
Funding
This work was supported by Effect: Hope (no grant number available), who provided financial and technical support.
Competing interests
LD is Guest Editor of this supplement but had no role in the review of this manuscript.
Ethical approval
Ethical approval for this study was obtained from the Congolese National Health Ethics Committee (reference number: 269/CNES/BN/PMMF/2021) and the Liverpool School of Tropical Medicine (reference number: 21-053).
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
- 1. WHO . Ending the neglect to attain the Sustainable Development Goals: A road map for neglected tropical diseases 2021-2030. Geneva: World Health Organisation; 2021.
- 2. WHO . Ending the neglect to attain the sustainabile development goals: A strategic framework for integrated control and management of skin-related neglected tropical diseases. Geneva: World Health Organisation; 2022.
- 3. Kosch, orke M, Al-Haboubi YH, Tseng P-Cet al. Mental health, stigma, and neglected tropical diseases: A review and systematic mapping of the evidence. Front Trop Dis. 2022;3. 10.3389/fitd.2022.808955 [DOI] [Google Scholar]
- 4. Dean L, Theobald S, Nallo Get al. A syndemic born of war: Combining intersectionality and structural violence to explore the biosocial interactions of neglected tropical diseases, disability and mental distress in Liberia. PLOS Glob Public Health. 2022;2(6):e0000551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Litt E, Baker MC, Molyneux D. Neglected tropical diseases and mental health: A perspective on comorbidity. Trends Parasitol. 2012;28(5):195–201. [DOI] [PubMed] [Google Scholar]
- 6. Ozano K, Dean L, Yoshimura M, MacPherson Eet al. A call to action for universal health coverage: Why we need to address gender inequities in the neglected tropical disease community. PloS NTDs. 2020. 10.1371/journal.pntd.0007786 [DOI] [PMC free article] [PubMed]
- 7. van ‘t Noordende AT, Kuiper H, Ramos AN Jret al. Towards a toolkit for cross-neglected tropical disease morbidity and disability assessment. Int Health. 2016;8(suppl_1):i71–81. [DOI] [PubMed] [Google Scholar]
- 8. Bailey F, Eaton J, Jidda Met al. Neglected tropical diseases and mental health: Progress, partnerships, and integration. Trends Parasitol. 2019;35(1):23–31. [DOI] [PubMed] [Google Scholar]
- 9. WHO . Report of the Global Partners' meeting on Neglected Tropical Diseases: 2007 - a Turning Point, Geneva, Switzerland, 17-18 April 2007. Geneva, Switzerland: World Health Organization;2007. [Google Scholar]
- 10. Rimoin AW, Hotez PJ. NTDs in the heart of darkness: The Democratic Republic of Congo's unknown burden of neglected tropical diseases. PLoS Negl Trop Dis. 2013;7(7):e2118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Corps M. Congo's Kasaï Provinces Conflict Assessment: Current dynamics and potential interventions. USA: Mercy Corps; 2019. https://www.mercycorps.org/sites/default/files/2020-03/Kasai_conflict_assessment.pdf
- 12. Ministère de la Santé D-PNDEdlL . Rapport Epidémiologique lèpre. Kinshasa: Ministere de la Sante; 2019.
- 13. Ministère de la Santé D-PNdlclmtN . Plan stratégique de lutte contre les maladies tropicales Négligées à chimiothérapie préventive. Kinshasa: Ministere de la Sante; 2016.
- 14. Madans JH, Loeb ME, Altman BM. Measuring disability and monitoring the UN Convention on the Rights of Persons with Disabilities: The work of the Washington Group on Disability Statistics. BMC Public Health. 2011;11(4):S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dadun, Peters RMH, Van Brakel WHet al. Cultural validation of a new instrument to measure leprosy-related stigma: The SARI Stigma Scale. Lepr Rev. 2017;88(1):23–42. [PubMed] [Google Scholar]
- 16. World Health Organization. Division of Mental H . WHOQOL-BREF : Introduction, Administration, Scoring and Generic Version of the Assessment : Field Trial Version, December 1996. Geneva, Switzerland: World Health Organization;1996. [Google Scholar]
- 17. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Spitzer RL, Kroenke K, Williams JBet al. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med. 2006;166(10):1092–7. [DOI] [PubMed] [Google Scholar]
- 19. Team RC . R: a Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria, 2021. [Google Scholar]
- 20. Semrau M, Davey G, Beng AAet al. Depressive symptoms amongst people with podoconiosis and lower limb lymphoedema of other cause in Cameroon: A cross-sectional study. Trop Med Infect Dis. 2019;4(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Semrau M, Davey G, Bayisenge Uet al. High levels of depressive symptoms among people with lower limb lymphoedema in Rwanda: A cross-sectional study. Trans R Soc Trop Med Hyg. 2020;114(12):974–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kpadonou TG, Alagnidé E, Azanmasso Het al. Psychosocioprofessional and familial becoming of formers Buruli ulcer patients in Benin. Ann Phys Rehabil Med. 2013;56(7):515–26. [DOI] [PubMed] [Google Scholar]
- 23. Amoako YA, Ackam N, Omuojine J-Pet al. Mental health and quality of life burden in Buruli ulcer disease patients in Ghana. Infect Dis Poverty. 2021;10(1):109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Obindo J, Abdulmalik J, Nwefoh Eet al. Prevalence of depression and associated clinical and socio-demographic factors in people living with lymphatic filariasis in Plateau State, Nigeria. PLoS Negl Trop Dis. 2017;11(6):e0005567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Richard SA, Mathieu E, Addiss DGet al. A survey of treatment practices and burden of lymphoedema in Togo. Trans R Soc Trop Med Hyg. 2007;101(4):391–7. [DOI] [PubMed] [Google Scholar]
- 26. Attama CM, Uwakwe R, Onyeama GMet al. Psychiatric morbidity among subjects with leprosy and albinism in South East Nigeria: A comparative study. Ann Med Health Sci Res. 2015;5(3):197–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bakare A. Anxiety and depression: A study of people with leprosy In Sokoto, North- Western Nigeria. J Psychiatry. 2015;s1. [Google Scholar]
- 28. van‘t Noordende AT, Wubie Aycheh M, Tadesse Tet al. A family-based intervention for prevention and self-management of disabilities due to leprosy, podoconiosis and lymphatic filariasis in Ethiopia: A proof of concept study. PLoS Negl Trop Dis. 2021;15(2):e0009167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lusli M, Peters R, van Brakel Wet al. The impact of a rights-based counselling intervention to reduce stigma in people affected by leprosy in Indonesia. PLoS Negl Trop Dis. 2016;10(12):e0005088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Johnson K, Scott J, Rughita Bet al. Association of sexual violence and Human rights violations with physical and mental health in Territories of the Eastern Democratic Republic of the Congo. JAMA. 2010;304(5):553–62. [DOI] [PubMed] [Google Scholar]
- 31. Ngamaba KH, Lombo LS, Makopa IKet al. Are COVID-19’s restrictive measures associated with people's quality of life and the prevalence of anxiety and depression in Kinshasa in the Democratic Republic of Congo? J Public Health Afr. 2022;13(3):1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kaputu-Kalala-Malu C, Musalu EM, Walker Tet al. PTSD, depression and anxiety in Ebola virus disease survivors in Beni town, Democratic Republic of the Congo. BMC Psychiatry. 2021;21(1):342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Scott J, Rouhani S, Greiner Aet al. Respondent-driven sampling to assess mental health outcomes, stigma and acceptance among women raising children born from sexual violence-related pregnancies in eastern Democratic Republic of Congo. BMJ Open. 2015;5(4):e007057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Corley A, Glass N, Remy MMet al. A latent class analysis of gender attitudes and their associations with intimate partner violence and mental health in the Democratic Republic of Congo. Int J Environ Res Public Health. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. WHO . Mental health of people with neglected tropical diseases - towards a person-centred approach. Geneva: World Health Organisation; 2020.
- 36. Charlson F, van Ommeren M, Flaxman Aet al. New WHO prevalence estimates of mental disorders in conflict settings: A systematic review and meta-analysis. Lancet. 2019;394(10194):240–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Chowdhury S, Adekeye O, McRae Aet al. A holistic approach to well-being and neglected tropical diseases: Evaluating the impact of community-led support groups in Nigeria using community-based participatory research. Int Health. 2023;15(Supplement_1):i87–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Fischer J, Jansen B, Rivera Aet al. Validation of a cross-NTD toolkit for assessment of NTD-related morbidity and disability. A cross-cultural qualitative validation of study instruments in Colombia. PLoS One. 2019;14(12):e0223042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kokou-Kpolou CK, Derivois D, Rousseau Cet al. Enacted Ebola stigma and health-related quality of life in Post Ebola epidemic: A psychosocial mediation framework through social support, self-efficacy, and coping. Appl Res Quality of Life. 2022;17(5):2809–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.


