Abstract
Background
We examined the relationship between global positioning system (GPS) indicators of community mobility and incident hospitalizations, emergency department (ED) visits, and falls over 1-year in community-dwelling older adults.
Methods
We performed a secondary analysis of a randomized trial investigating a physical therapy intervention to improve mobility in older adults. One hundred and forty-eight participants (mean age: 76.9 ± 6.2 years; 65% female) carried a GPS device following the postintervention visit. Over 1-year, new hospitalizations, falls, and ED visits were reported. GPS indicators of community mobility included the median area and compactness of the standard deviation ellipse (SDE), the median percentage of time spent outside of home (TOH), and median maximum distance from home. Generalized linear models assessed the association between 1-year risk of outcomes and GPS measures adjusted for age, race, gender, body mass index, comorbidity burden, and fall history.
Results
The mean ± standard deviation of the median SDE area was 4.4 ± 8.5 km2, median SDE compactness 0.7 ± 0.2, median percentage TOH 14.4 ± 12.0%, and median maximum distance from home was 38 ± 253 km. Each 5% increase in median percentage TOH was associated with a 24% lower risk of hospitalization (incident rate ratio = IRR = 0.76, 95%CI: 0.61–0.95; p = .01). The association persisted after covariate adjustment (IRR = 0.78, 95%CI: 0.63–0.98; p = .03). No significant associations appeared for any GPS indicators with incident falls or ED visits.
Conclusions
Increased TOH was associated with a lower risk of incident hospitalization over 1 year among community-dwelling older adults. Restricted community mobility may be an indicator of activity limitations related to future health outcomes, but further study is warranted.
Keywords: Emergency department, Falls, Hospitalization, Independent living, Physical therapy
Mobility is essential for participation in everyday activities and independent living. In the United States, over 26% of adults 65 years and older have a mobility disability (1,2). Mobility limitations among older adults can predict subsequent disability, cardiovascular disease, mortality, and increased health care costs (3,4). Community mobility, defined as the ability to move outside of the home including the surrounding neighborhood and extending to regions beyond, can be influenced by a variety of factors (eg, financial, psychosocial, environmental, physical, cognitive, gender, cultural, and biographical influences) (5). Restricted self-reported community mobility is associated with falls and other negative health outcomes among older adults (6,7). Reductions in self-reported community mobility over time have been associated with increased risk for institutionalization and mortality in this age group (8–12). Improvements in clinical performance-based measures (eg, gait speed, 6-minute walk test distance) following exercise interventions are associated with reduced incidence of falls (13). However, improvements in physical capacity, only one component of functional mobility, may not translate to improvements in community mobility (5). Although studies have demonstrated associations between health outcomes and clinical and self-reported measures of mobility, there is limited research investigating associations between health outcomes and objectively measured community mobility in real-world environments.
Measuring mobility is important and can be used to track changes over time and identify the effectiveness of targeted interventions (14,15). Physical aspects of mobility can be measured in clinical settings with the assessment of gait speed or a long distance walk such as the 6-minute walk test (16,17). Mobility can also be assessed via self-report such as the ability to walk a quarter mile or with validated outcome measures (3,18). However, in clinical settings, activity is often measured under ideal circumstances (eg, without environmental barriers typically experienced during everyday activity), and self-reported measures may be prone to recall bias. Alternatively, objective measures of mobility can be obtained through wearable technologies (eg, global positing system [GPS] devices), reducing the risk of recall bias and capturing free-living mobility in real-time (19–21). However, there have been limited studies examining the longitudinal associations between GPS indicators of community mobility and future health outcomes.
The purpose of this study was to examine the relationship between objective, GPS indicators of community mobility and 12-month incidence of falls, hospitalizations, and emergency department (ED) visits among older adults. We hypothesized that participants with greater community mobility would have a lower risk of negative health outcomes during the ensuing period.
Method
This was a secondary analysis using data from the program to improve mobility in aging (PRIMA) study, a randomized clinical trial investigating the effect of timing and coordination training compared to usual care on mobility and physical activity in community-dwelling older adults (22). The study was approved by the University of Pittsburgh Institutional Review Board, and all participants provided written informed consent.
Participants
Participants were included in the study if they were 65 years of age or older, able to ambulate without assistance, had a usual gait speed between 0.6 and 1.2m/s, and had physician clearance to participate. Additional study details are described elsewhere (22,23). Participants were instructed to carry a GPS device for 7 days after the 12-week, postintervention follow-up visit (see section “Measures of Health Outcomes”). For the present analysis, we included participants who had at least 5 days of valid GPS data and completed at least one interactive voice response (IVR) phone call over the 1-year follow-up period. For the time out-of-home (TOH) measure, we further excluded individuals who had less than 20% of time spent inside their home (n = 10). Less than 20% of time spent at home could be an indication of error in data collection or community mobility that is not representative of one’s typical routine (eg, vacation, staying with another person), so we excluded those individuals (24). Demographic and clinical information was collected at the baseline visit, including self-reported fall history (in the past 12 months), Duke comorbidity index (range 0–8, with higher scores indicating greater comorbidity burden), and the Modified Mini-Mental State Examination (3MS) (range 0–100, with higher scores indicating better cognitive function) (25,26).
Measures of Health Outcomes
After the 12-week, postintervention visit, participants were contacted once per month for a year via an automated IVR phone call inquiring about any new health events in the prior month including falls, ED visits, and hospitalizations (27). They were asked if they had experienced a fall, a visit to the ED for any reason, or a hospitalization for one or more nights in the past 30 days.
GPS Indicators of Community Mobility
Participants were asked to carry a GPS device (iBlue 747A, TSI, Hsinchu, Taiwan or V-990, Columbus, Germany) with them for the 7 days following their 12-week, postintervention visit. The methods used to process the GPS data for this study are described elsewhere (24). The GPS indicators of community mobility for this study included the median standard deviational ellipse (SDE), median percentage TOH, and median maximum distance traveled from home (28). The SDE contains approximately 68% of all GPS data within the ellipse boundary and can be characterized by measuring the area and compactness (ie, shape) of the space (29). Median percentage of time spent outside the TOH buffer (120 meters) and maximum distance from home were used to estimate out-of-home activity (28,30,31).
Statistical Analyses
We used descriptive statistics to summarize the demographic characteristics. The GPS indicators of community mobility were summarized over the 7-day wear period using medians to reduce the influence of outlier travel days on community mobility estimates and better approximate participants’ typical movement patterns during the week.
The GPS indicators of community mobility for the sample were then described using means and standard deviations (SDs). Health events were presented as a rate per 1000 person-months. One-year risk of falls, ED visits, and hospitalization were calculated for each GPS measure (median SDE area, median SDE compactness, median percentage TOH, and median maximum distance from home) using generalized linear models, with event counts as the dependent variable, log(months reported) as an offset, a negative binomial distribution, a log link, and quartile of each GPS measure as a categorical independent variable to account for any potential nonlinear associations. Where a linear association was plausible, we also examined the GPS measure as a continuous independent variable to afford greater statistical sensitivity. Adjusted models included the following covariates: age, race, gender, body mass index, comorbidity index, and fall history. Intervention arm was not included as a covariate because there were no differences in GPS measures of community mobility between arms, and also because the active intervention period did not overlap with the 12-week GPS measurement and follow-up period (32). SAS version 9.4 (SAS Institute, Inc., Cary, NC) was used for statistical analysis.
Results
Baseline Characteristics
The PRIMA study included 249 community-dwelling older adults. Of those, 148 had valid GPS data following the 12-week, postintervention visit and at least 1 IVR phone call. Reasons for a smaller sample at the 12-week postintervention visit have been described elsewhere, with the most common reason being that a device was not distributed due to device failure (n = 56) (32). The mean and SD age of our sample was 76.9 ± 6.2, 64.9% were female, 89.9% were White, and 6.8% were Black (Table 1). Most of the sample had completed college (35.1%) or postgraduate education (47.3%). Half reported living alone (50.7%) and 32.4% reported having a fall in the prior year. The gait speed at baseline was 1.08 ± 0.2 m/s and the 3MS score was 96.4 ± 3.7.
Table 1.
Participant Characteristics and Health Events Over 12 Months (n = 148)
| Mean ± SD or n (%) | |
|---|---|
| Age | 76.9 ± 6.2 |
| Female, n (%) | 96 (64.9) |
| Race, n (%) | |
| Asian | 1 (0.7) |
| Black | 10 (6.8) |
| White | 133 (89.9) |
| Other | 1 (0.7) |
| Refused | 3 (2.0) |
| Living alone, n (%) | 75 (50.7) |
| Education, n (%) | |
| High school | 22 (14.9) |
| College | 52 (35.1) |
| Postgraduate | 70 (47.3) |
| Other | 4 (2.7) |
| Fall in the prior year, n (%) | 48 (32.4) |
| Body mass index | 29.0 ± 5.4 |
| Comorbidity index (0–8) | 2.9 ± 1.3 |
| Gait speed, m/s | 1.08 (0.16) |
| Modified Mini-Mental State Examination (0–100) | 96.4 ± 3.7 |
| GPS measures | |
| Median SDE area, km2 | 4.4 ± 8.5 |
| Median SDE compactness | 0.7 ± 0.2 |
| Median percentage of time out of home, %* | 14.4 ± 12.0 |
| Median maximum distance from home, km | 38.2 ± 252.8 |
| Health events over 12 months | Rate per 1000 person-months |
|---|---|
| Falls | 74.5 |
| Hospitalization | 29.1 |
| Emergency department visit | 38.8 |
Note: Other education includes associate degree or technical/trade school education after high school.
* n = 138 due to exclusion of 10 individuals who spent less than 20% of time spent at home.
At 12 weeks, the average median SDE area was 4.4 ± 8.5 km2, median SDE compactness was 0.7 ± 0.2, median percentage TOH was 14.4 ± 12.0%, and median maximum distance from home was 38.2 ± 252.8 km (Table 1). Over the year following the 12-week visit, falls occurred at a rate of 74.5 per 1000 person-months, hospitalizations 29.1, and ED visits 38.8.
Falls
There were no significant associations between GPS indicators of community mobility and falls except in the unadjusted analysis of maximum distance from home (Table 2). Those in the second median maximum distance from home quartile had a 59% lower incidence of falls (incidence rate ratio [IRR] = 0.41, 95% CI: 0.18–0.94; p = .04) compared to those in the fourth (highest quartile). However, this finding was not significant after the covariate adjustment. In the adjusted model only, those in the third median SDE area quartile had a lower risk of falls (IRR = 0.39, 95% CI: 0.16–0.94; p = .04) compared to those in the fourth quartile.
Table 2.
Association of GPS Measures and Incident Falls Over 12 Months
| Unadjusted | Adjusted | |||||
|---|---|---|---|---|---|---|
| IRR | 95% CI | p | IRR | 95% CI | p | |
| Median SDE Area | ||||||
| Quartile 1 versus 4 | 0.80 | 0.36–1.81 | 0.60 | 1.14 | 0.54–2.40 | 0.73 |
| Quartile 2 versus 4 | 1.29 | 0.62–2.66 | 0.50 | 1.18 | 0.59–2.37 | 0.63 |
| Quartile 3 versus 4 | 0.55 | 0.23–1.28 | 0.17 | 0.39* | 0.16–0.94 | 0.04 |
| Median SDE compactness | ||||||
| Quartile 1 versus 4 | 1.69 | 0.72–4.00 | 0.23 | 1.12 | 0.48–2.60 | 0.80 |
| Quartile 2 versus 4 | 1.47 | 0.63–3.43 | 0.38 | 1.56 | 0.69–3.55 | 0.29 |
| Quartile 3 versus 4 | 1.99 | 0.87–4.53 | 0.10 | 2.29* | 1.05–5.00 | 0.04 |
| Median % of time outside of home | ||||||
| Continuous (per 5%) | 1.06 | 0.94–1.20 | 0.37 | 1.01 | 0.90–1.14 | 0.86 |
| Quartile 1 versus 4 | 0.78 | 0.36–1.72 | 0.54 | 0.88 | 0.42–1.85 | 0.73 |
| Quartile 2 versus 4 | 0.81 | 0.38–1.72 | 0.59 | 0.89 | 0.44–1.81 | 0.75 |
| Quartile 3 versus 4 | 0.97 | 0.46–2.04 | 0.93 | 0.90 | 0.44–1.87 | 0.79 |
| Median maximum distance from home | ||||||
| Quartile 1 versus 4 | 0.87 | 0.41–1.85 | 0.71 | 1.54 | 0.72–3.30 | 0.27 |
| Quartile 2 versus 4 | 0.41* | 0.18–0.94 | 0.03 | 0.58 | 0.26–1.28 | 0.18 |
| Quartile 3 versus 4 | 0.59 | 0.28–1.25 | 0.17 | 0.93 | 0.43–1.99 | 0.85 |
Notes: Adjusted models included the following covariates: age, gender, race, BMI, Duke Comorbidity Index, Fall history. CI = confidence interval; IRR = incident rate ratio; SDE = standard deviational ellipse.
* p < .05.
Hospitalizations
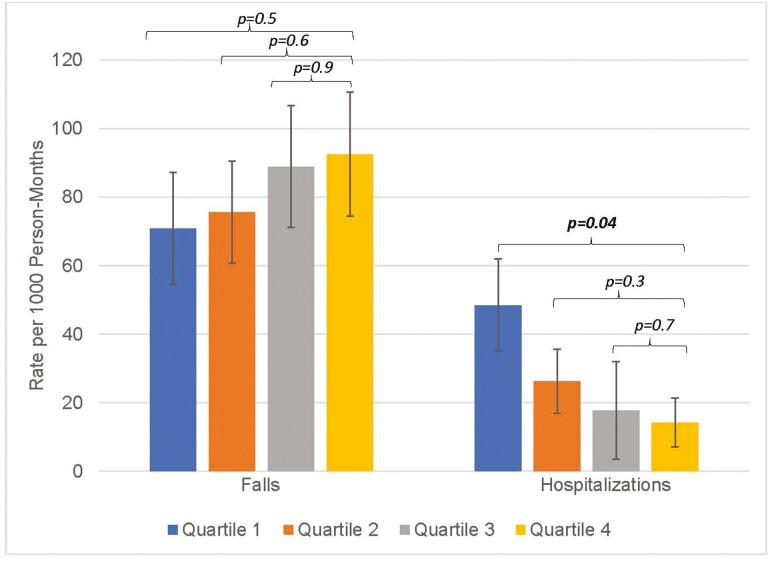
Each 5% increase in median percentage TOH was associated with a 24% lower risk of hospitalization (IRR = 0.76, 95%CI: 0.61–0.95; p = .01; Table 3). The relationship persisted in models adjusted for covariates (IRR = 0.78, 95%CI: 0.63–0.98; p = .03). Participants in the first quartile of percent TOH had greater rates of hospitalization over 12 months compared to those in the fourth quartile (IRR = 3.47, 95%CI: 1.06–11.43; p = .04) in the unadjusted model (Figure 1). Those in the second and third percentage of time spent outside of home quartiles also had a greater risk of hospitalization compared to those in the highest quartile, although the results were not statistically significant.
Table 3.
Association of GPS Measures and Incident Hospitalizations Over 12 Months
| Unadjusted | Adjusted | |||||
|---|---|---|---|---|---|---|
| IRR | 95% CI | p | IRR | 95% CI | p | |
| Median SDE area | ||||||
| Quartile 1 versus 4 | 2.44 | 0.88–6.76 | 0.09 | NE | NE | NE |
| Quartile 2 versus 4 | 1.05 | 0.34–3.18 | 0.94 | NE | NE | NE |
| Quartile 3 versus 4 | 0.62 | 0.17–2.30 | 0.47 | NE | NE | NE |
| Median SDE compactness | ||||||
| Quartile 1 versus 4 | 0.78 | 0.22–2.77 | 0.70 | NE | NE | NE |
| Quartile 2 versus 4 | 1.92 | 0.67–5.50 | 0.22 | NE | NE | NE |
| Quartile 3 versus 4 | 1.04 | 0.33–3.27 | 0.94 | NE | NE | NE |
| Median % of time outside of home | ||||||
| Continuous (per 5%) | 0.76* | 0.61–0.95 | 0.01 | 0.78* | 0.63–0.98 | 0.03 |
| Quartile 1 versus 4 | 3.47* | 1.06–11.43 | 0.04 | 2.75 | 0.85–8.92 | 0.09 |
| Quartile 2 versus 4 | 1.85 | 0.52–6.52 | 0.34 | 1.85 | 0.55–6.25 | 0.32 |
| Quartile 3 versus 4 | 1.25 | 0.32–4.94 | 0.75 | 0.95 | 0.25–3.62 | 0.94 |
| Median maximum distance from home | ||||||
| Quartile 1 versus 4 | 1.68 | 0.68–4.15 | 0.26 | NE | NE | NE |
| Quartile 2 versus 4 | 0.20* | 0.04–0.96 | 0.04 | NE | NE | NE |
| Quartile 3 versus 4 | 0.62 | 0.22–1.75 | 0.36 | NE | NE | NE |
Note: Adjusted models included the following covariates: age, gender, race, BMI, Duke Comorbidity Index, Fall history. CI = confidence interval; IRR = incident rate ratio; NE = not estimable due to model convergence issues; SDE = standard deviational ellipse.
* p < .05.
Figure 1.
Rates of falls and hospitalizations per 1000 person-months over 12 months by median percentage of time outside of home quartile. Participants in quartile 1 had a greater risk of incident hospitalizations over 12 months compared to participants in quartile 4.
Participants in the second quartile for median maximum distance from home had an 80% lower risk of hospitalizations compared with those in the highest quartile (IRR = 0.20, 95% CI: 0.04–0.96; p = .04). However, this finding could not be assessed in adjusted models.
Emergency Department Visits
There were no significant associations between GPS metrics of community mobility and ED visits (Table 4). All p’s > .10 with the exception of those in the second quartile versus highest quartile for maximum distance from home in the unadjusted model (p = .07).
Table 4.
Association of GPS Measures and Incident Emergency Department Visits Over 12 Months
| Unadjusted | Adjusted | |||||
|---|---|---|---|---|---|---|
| IRR | 95% CI | p | IRR | 95% CI | p | |
| Median SDE area | ||||||
| Quartile 1 versus 4 | 1.02 | 0.38–2.74 | 0.96 | 1.29 | 0.49–3.37 | 0.61 |
| Quartile 2 versus 4 | 1.02 | 0.40–2.62 | 0.97 | 1.46 | 0.58–3.65 | 0.42 |
| Quartile 3 versus 4 | 0.78 | 0.28–2.20 | 0.64 | 1.12 | 0.38–3.36 | 0.83 |
| Median SDE compactness | ||||||
| Quartile 1 versus 4 | 1.62 | 0.56–4.72 | 0.38 | 1.52 | 0.54–4.31 | 0.43 |
| Quartile 2 versus 4 | 1.78 | 0.64–4.93 | 0.27 | 1.44 | 0.54–3.86 | 0.46 |
| Quartile 3 versus 4 | 1.29 | 0.45–3.71 | 0.64 | 1.46 | 0.53–4.03 | 0.46 |
| Median % of time outside of home | ||||||
| Continuous (per 5%) | 1.02 | 0.87–1.21 | 0.78 | 1.01 | 0.87–1.18 | 0.85 |
| Quartile 1 versus 4 | 0.95 | 0.34–2.61 | 0.91 | 0.85 | 0.32–2.26 | 0.74 |
| Quartile 2 versus 4 | 0.83 | 0.30–2.28 | 0.72 | 0.86 | 0.34–2.19 | 0.75 |
| Quartile 3 versus 4 | 1.69 | 0.67–4.24 | 0.26 | 1.29 | 0.55–3.01 | 0.56 |
| Median maximum distance from home | ||||||
| Quartile 1 versus 4 | 0.84 | 0.34–2.07 | 0.71 | 1.02 | 0.41–2.55 | 0.97 |
| Quartile 2 versus 4 | 0.37 | 0.13–1.08 | 0.07 | 0.48 | 0.17–1.36 | 0.17 |
| Quartile 3 versus 4 | 0.65 | 0.27–1.61 | 0.35 | 0.89 | 0.35–2.24 | 0.80 |
Notes: Adjusted models included the following covariates: age, gender, race, BMI, Duke Comorbidity Index, Fall history. CI = confidence interval; IRR = incident rate ratio; SDE = standard deviational ellipse.
Discussion
We found that individuals with a greater percentage of TOH had a reduced risk of hospitalization in the ensuing 12-month period. We did not find any additional meaningful associations between other GPS metrics of community mobility and falls, hospitalizations, or ED visits after adjusting for covariates. Spending time outside of the home may allow for more opportunities to engage in social, cognitive, and physical activities. Greater time spent inside the home may indicate more sedentary behavior (33,34), which is associated with an increased risk of hospitalization and other negative health outcomes (35–37). Greater time spent inside the home may also be an indicator of poorer health status, which could increase the risk of future hospitalizations.
Percentage TOH specifically quantifies duration of community mobility (28) and greater TOH measured using GPS has been associated with better cognitive and physical function measures among older adults (38). In contrast, the area and compactness of the SDE and maximum distance from home characterize mobility space and extent (28). Given the current findings were specific to percentage TOH, timing and duration of mobility may be important indicators for potential mobility limitations and risk of future hospitalizations. Nevertheless, others have also found that GPS indicators of the space and extent of community mobility, such as distance traveled as a pedestrian and number of journeys, were associated with better perceived health and physical function, cognitive and psychological functioning, and balance performance (36,37,39). Given the associations of GPS metrics with a variety of clinic-based physical function and cognitive measures, restrictions in community mobility may precede declines in physical or cognitive performance or serve as an indicator for poorer health status, which would subsequently lead to increased risk for negative health outcomes among community-dwelling older adults.
Kennedy et al. found that a reduction in self-reported life space is associated with higher odds of hospitalization and ED visits over the course of a 3-year study (38). Reductions in self-reported life space are also associated with increased risk for falls and incidence of injurious falls over a 6-month period (6,40). Therefore, the association between changes in self-reported community mobility and negative health outcomes, including hospitalizations, ED visits, and falls has been well-established (7,8,38,40).
In a recent review, it was noted that fall history and incident falls in relation to GPS measures of community mobility have been understudied (20). In a study investigating patterns of falling among individuals with glaucoma, researchers found no association between fall status over a year and time away from home measured with GPS (41). Ahmed et al. found an association between falls and a decrease in self-reported life-space mobility over 4 years (6). In the present study, although not statistically significant, there was some preliminary evidence in descriptive statistics to suggest that individuals who spend more time away from home may have more falls (Figure 1). This may indicate exposure to additional risks for falls as well as benefits in terms of reduced hospitalization risk. Similar results have been found among older men with those who had low physical activity and poor physical performance having an increased risk of falls as well as those who had better physical activity and performance (42). However, this observation must be interpreted cautiously as it is not supported by statistical significance, except in one adjusted model. The association between objectively measured community mobility and falls should be more rigorously examined in future work to establish if limitations in community mobility may be an early indicator of underlying health issues or preclinical mobility limitations that may increase fall risk.
There is some evidence that disability prevention programs, physical therapy, community health and wellness, and physical activity interventions have a positive effect on life space and community mobility measured through self-report and GPS (43–45). Addressing limitations in community mobility may in turn reduce risk of the negative outcomes associated with a restricted life space. Future work should focus on the development of interventions targeting improvements in community mobility, participation in daily activities, and life roles. Interventions to improve community mobility will likely be multifaceted in nature and include behavioral, physical, and educational interventions to address the complex interactions of factors associated with life-space mobility (44,46). However, improvements in community mobility may begin with small behavioral changes. Clinicians can encourage increased daily mobility among community-dwelling older adults by suggesting activities such as walking to the mailbox and back, walking to visit a neighbor, or walking a pet in the neighborhood.
Strengths and Limitations
Our study had limitations and strengths. It should be noted that the community-dwelling older adults included in this study were mostly White, highly educated, and cognitively intact, which may limit generalizability to the general older adult population (23). The analysis included all falls that were reported during the 12-month follow-up period, and we do not know if they occurred indoors or outdoors. However, the use of monthly IVR phone calls to regularly assess incident health outcomes reduced the length of time over which the participants were asked to recall health events. Participants using GPS devices may not have been compliant on all days of the wear period, which would result in an underestimation of community mobility. However, we attempted to correct this by excluding those with less than 5 days of wear time. In addition, 7 days of wear time is relatively short and may not capture typical community mobility for all individuals. The number of events was relatively small, especially for the hospitalization outcome, which precluded fitting a model that included covariates with some GPS measures. In addition, we were unable to determine the underlying reasons for the reduced percentage of TOH, which may be risk factors for increased risk of hospitalization. We also did not adjust our models for prior episodes of hospitalizations, as there were only 3 participants who reported a hospitalization in the 3 months prior to our analytic baseline. The parent trial had not collected specific reasons for hospitalizations and ED visits that could have explained the differential findings, and we speculate the former may be due to more illnesses while the latter may be attributable to injuries. Finally, our report contains an unplanned secondary analysis of data from a clinical trial. Further studies are needed for more definitive conclusions.
The study was strengthened by the relatively large sample size and the use of GPS technology which allows for objective measurement and decreases the risk of recall bias associated with self-report. In addition, the participants in this study had a wide range of physical functions evidenced by the 6-Minute Walk Test, Figure-of-8 Walk, and gait speed measures. The GPS metrics utilized in this study allowed us to capture multiple dimensions of community mobility (ie, duration, timing, space, extent) and the longitudinal study design allowed us to measure how community mobility relates to incident health events.
Conclusion
Greater time spent outside of home as measured by GPS was associated with reduced risk of future hospitalization in community-dwelling older adults over a year. This finding highlights the potential usefulness of GPS indicators of community mobility timing to identify early risk for negative health outcomes among community-dwelling older adults. GPS technology offers an objective way to track changes in mobility over time and identify potential risks for negative health outcomes. With advances in technology, using wearable devices would allow for remote monitoring of mobility patterns with the potential for reduced burden on clinicians and patients. Our findings are to be considered preliminary due to the limitations mentioned above. Future work should focus on (i) larger purpose-built studies to elicit definitive conclusions and (ii) employing longitudinal GPS indicators of community mobility to identify if declines over time are associated with adverse health outcomes. Information gleaned from these studies will allow for the development of targeted interventions to improve community mobility and potentially decrease the risk of negative health outcomes among community-dwelling older adults.
Acknowledgments
We thank the participants for giving their time to this study.
Contributor Information
Pamela M Dunlap, Department of Physical Therapy, University of Pittsburgh, Pittsburgh, Pennsylvania, USA.
Breanna M Crane, Department of Mental Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, USA.
Subashan Perera, Division of Geriatric Medicine and Department of Biostatistics, University of Pittsburgh, Pittsburgh, Pennsylvania, USA.
Kyle D Moored, Department of Mental Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, USA.
Michelle C Carlson, Department of Mental Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, USA.
Jennifer S Brach, Department of Physical Therapy, University of Pittsburgh, Pittsburgh, Pennsylvania, USA.
Brooke N Klatt, Department of Physical Therapy, University of Pittsburgh, Pittsburgh, Pennsylvania, USA.
Andrea L Rosso, Department of Epidemiology, University of Pittsburgh, Pittsburgh, Pennsylvania, USA.
Lewis A Lipsitz, (Medical Sciences Section).
Funding
This work was supported by the National Institute on Aging at the National Institutes of Health through research grants (R01 AG045252, K24 AG057728, R01 AG057671, P30 AG024827, T32-AG027668 [B.M.C.], T32-AG000247 [B.M.C.], T32-AG000181 [K.D.M.].
Conflict of Interest
None.
Author Contributions
Study concept and design: A.L.R, P.M.D., J.S.B. Acquisition of subjects and/or data: J.S.B., A.L.R. Analysis and interpretation of data: B.M.C., K.D.M., S.P., A.L.R., M.C.C., P.M.D, B.N.K., Preparation of manuscript: all authors.
Sponsor’s Role
The sponsor did not have a role in the design, methods, subject recruitment, data collections, analysis or preparation of paper.
References
- 1. Okoro CA, Hollis ND, Cyrus AC, Griffin-Blake S.. Prevalence of disabilities and health care access by disability status and type among adults—United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(32):882–887. 10.15585/mmwr.mm6732a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bergen G, Stevens MR, Burns ER.. Falls and fall injuries among adults aged ≥65 years–United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65(37):993–998. 10.15585/mmwr.mm6537a2 [DOI] [PubMed] [Google Scholar]
- 3. Hardy SE, Kang Y, Studenski SA, Degenholtz HB.. Ability to walk 1/4 mile predicts subsequent disability, mortality, and health care costs. J Gen Intern Med. 2011;26(2):130–135. 10.1007/s11606-010-1543-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Newman AB, Simonsick EM, Naydeck BL, et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. JAMA. 2006;295(17):2018–2026. 10.1001/jama.295.17.2018 [DOI] [PubMed] [Google Scholar]
- 5. Webber SC, Porter MM, Menec VH.. Mobility in older adults: a comprehensive framework. Gerontologist. 2010;50(4):443–450. 10.1093/geront/gnq013 [DOI] [PubMed] [Google Scholar]
- 6. Ahmed T, Curcio C-L, Auais M, et al. Falls and life-space mobility: longitudinal analysis from the international mobility in aging study. Aging Clin Exp Res. April 8, 2020;33:303–310. 10.1007/s40520-020-01540-0 [DOI] [PubMed] [Google Scholar]
- 7. Lo AX, Brown CJ, Sawyer P, Kennedy RE, Allman RM.. Life-space mobility declines associated with incident falls and fractures. J Am Geriatr Soc. 2014;62(5):919–923. 10.1111/jgs.12787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kennedy RE, Sawyer P, Williams CP, et al. Life-space mobility change predicts 6-month mortality. J Am Geriatr Soc. 2017;65(4):833–838. 10.1111/jgs.14738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mackey DC, Cauley JA, Barrett-Connor E, Schousboe JT, Cawthon PM, Cummings SR; Osteoporotic Fractures in Men Research Group. Life-space mobility and mortality in older men: a prospective cohort study. J Am Geriatr Soc. 2014;62(7):1288–1296. 10.1111/jgs.12892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Watanabe D, Yoshida T, Yamada Y, et al. Dose-response relationship between life-space mobility and mortality in older Japanese adults: a prospective cohort study. J Am Med Dir Assoc. 2022Nov;23(11):1869.e7–1869.e18. 10.1016/j.jamda.2022.04.017 [DOI] [PubMed] [Google Scholar]
- 11. Mackey DC, Lui L-Y, Cawthon PM, Ensrud K, Yaffe K, Cummings SR.. Life-space mobility and mortality in older women: prospective results from the study of osteoporotic fractures. J Am Geriatr Soc. 2016;64(11):2226–2234. 10.1111/jgs.14474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sheppard KD, Sawyer P, Ritchie CS, Allman RM, Brown CJ.. Life-space mobility predicts nursing home admission over 6 years. J Aging Health. 2013;25(6):907–920. 10.1177/0898264313497507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Shuman V, Coyle PC, Perera S, Van Swearingen JM, Albert SM, Brach JS.. Association between improved mobility and distal health outcomes. J Gerontol A Biol Sci Med Sci. 2020;75(12):2412–2417. 10.1093/gerona/glaa086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA. 2011;305(1):50–58. 10.1001/jama.2010.1923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Perera S, Patel KV, Rosano C, et al. Gait speed predicts incident disability: a pooled analysis. J Gerontol A Biol Sci Med Sci. 2016;71(1):63–71. 10.1093/gerona/glv126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Harada ND, Chiu V, Stewart AL.. Mobility-related function in older adults: assessment with a 6-minute walk test. Arch Phys Med Rehabil. 1999;80(7):837–841. 10.1016/s0003-9993(99)90236-8 [DOI] [PubMed] [Google Scholar]
- 17. Cesari M, Kritchevsky SB, Penninx BWHJ, et al. Prognostic value of usual gait speed in well-functioning older people—results from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2005;53(10):1675–1680. 10.1111/j.1532-5415.2005.53501.x [DOI] [PubMed] [Google Scholar]
- 18. Peel C, Sawyer Baker P, Roth DL, Brown CJ, Brodner EV, Allman RM.. Assessing mobility in older adults: the UAB Study of Aging Life-Space Assessment. Phys Ther. 2005;85(10):1008–1119. 10.1093/ptj/85.10.1008 [DOI] [PubMed] [Google Scholar]
- 19. Boissy P, Blamoutier M, Brière S, Duval C.. Quantification of free-living community mobility in healthy older adults using wearable sensors. Front Public Health. 2018;6:216. 10.3389/fpubh.2018.00216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Suri A, VanSwearingen J, Dunlap P, Redfern MS, Rosso AL, Sejdić E.. Facilitators and barriers to real-life mobility in community-dwelling older adults: a narrative review of accelerometry- and global positioning system-based studies. Aging Clin Exp Res. March 11, 2022;34:1733–1746. 10.1007/s40520-022-02096-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chung J, Sargent L, Brown R, Gendron T, Wheeler D.. GPS tracking technologies to measure mobility-related behaviors in community-dwelling older adults: a systematic review. J Appl Gerontol. 2020;40:547–557. 10.1177/0733464820979801 [DOI] [PubMed] [Google Scholar]
- 22. Brach JS, VanSwearingen JM, Gil A, et al. Program to improve mobility in aging (PRIMA) study: Methods and rationale of a task-oriented motor learning exercise program. Contemp Clin Trials. 2020;89:105912. 10.1016/j.cct.2019.105912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Brach JS, Perera S, Shuman V, et al. Effect of timing and coordination training on mobility and physical activity among community-dwelling older adults: a randomized clinical trial. JAMA Netw Open. 2022;5(5):e2212921. 10.1001/jamanetworkopen.2022.12921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Crane BM, Moored KD, Rosso AL, Carlson MC.. Using GPS technologies to examine community mobility in older adults. J Gerontol A Biol Sci Med Sci. 2023May 11;78(5):811–820. 10.1093/gerona/glac185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rigler SK, Studenski S, Wallace D, Reker DM, Duncan PW.. Co-morbidity adjustment for functional outcomes in community-dwelling older adults. Clin Rehabil. 2002;16(4):420–428. 10.1191/0269215502cr515oa [DOI] [PubMed] [Google Scholar]
- 26. Teng EL, Chui HC.. The Modified Mini-Mental State (3MS) examination. J Clin Psychiatry. 1987;48(8):314–318. [PubMed] [Google Scholar]
- 27. Albert SM, King J, Keene RM.. Assessment of an interactive voice response system for identifying falls in a statewide sample of older adults. Prev Med. 2015;71:31–36. 10.1016/j.ypmed.2014.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Fillekes MP, Giannouli E, Kim E-K, Zijlstra W, Weibel R.. Towards a comprehensive set of GPS-based indicators reflecting the multidimensional nature of daily mobility for applications in health and aging research. Int J Health Geogr. 2019;18(1):17. 10.1186/s12942-019-0181-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hirsch JA, Winters M, Clarke P, McKay H.. Generating GPS activity spaces that shed light upon the mobility habits of older adults: a descriptive analysis. Int J Health Geogr. 2014;13:51. 10.1186/1476-072X-13-51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Tung JY, Rose RV, Gammada E, et al. Measuring life space in older adults with mild-to-moderate Alzheimer’s disease using mobile phone GPS. Gerontology. 2014;60(2):154–162. 10.1159/000355669 [DOI] [PubMed] [Google Scholar]
- 31. Harada K, Lee S, Lee S, Bae S, Harada K, Shimada H.. Changes in objectively measured outdoor time and physical, psychological, and cognitive function among older adults with cognitive impairments. Arch Gerontol Geriatr. 2018;78:190–195. 10.1016/j.archger.2018.06.003 [DOI] [PubMed] [Google Scholar]
- 32. Dunlap PM, Crane BM, Perera S, et al. Effects of a physical therapist intervention on GPS indicators of community mobility in older adults: a secondary analysis of a randomized controlled trial. Phys Ther. 2023Aug 1;103(8):pzad071. 10.1093/ptj/pzad071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hurvitz PM, Moudon AV, Kang B, Fesinmeyer MD, Saelens BE.. How far from home? The locations of physical activity in an urban U.S. setting. Prev Med. 2014;69:181–186. 10.1016/j.ypmed.2014.08.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Pasanen S, Halonen JI, Pulakka A, et al. Contexts of sedentary time and physical activity among ageing workers and recent retirees: cross-sectional GPS and accelerometer study. BMJ Open. 2021;11(5):e042600. 10.1136/bmjopen-2020-042600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Jain P, Bellettiere J, Glass N, et al. The relationship of accelerometer-assessed standing time with and without ambulation and mortality: the WHI OPACH study. J Gerontol A Biol Sci Med Sci. 2021;76(1):77–84. 10.1093/gerona/glaa227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Dohrn I-M, Welmer A-K, Hagströmer M.. Accelerometry-assessed physical activity and sedentary time and associations with chronic disease and hospital visits—a prospective cohort study with 15 years follow-up. Int J Behav Nutr Phys Act. 2019;16(1):125. 10.1186/s12966-019-0878-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Biswas A, Oh PI, Faulkner GE, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. 2015;162(2):123–132. 10.7326/M14-1651 [DOI] [PubMed] [Google Scholar]
- 38. Kennedy RE, Williams CP, Sawyer P, et al. Life-space predicts health care utilization in community-dwelling older adults. J Aging Health. 2019;31(2):280–292. 10.1177/0898264317730487 [DOI] [PubMed] [Google Scholar]
- 39. McInnes L, Jones E, Rochester L, et al. Mobility in community dwelling older adults: predicting successful mobility using an instrumented battery of novel measures. J Frailty Aging. 2020;9(2):68–73. 10.14283/jfa.2019.35 [DOI] [PubMed] [Google Scholar]
- 40. Lo AX, Rundle AG, Buys D, et al. Neighborhood disadvantage and life-space mobility are associated with incident falls in community-dwelling older adults. J Am Geriatr Soc. 2016;64(11):2218–2225. 10.1111/jgs.14353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Garzon C, Mihailovic A, Jian-Yu E, et al. Evaluation of away-from-home excursion patterns after falling among individuals with glaucoma: a longitudinal study. BMC Geriatr. 2022;22(1):101. 10.1186/s12877-022-02788-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Orwoll ES, Fino NF, Gill TM, et al. ; Osteoporotic Fractures in Men (MrOS) Study Research Group. The relationships between physical performance, activity levels, and falls in older men. J Gerontol A Biol Sci Med Sci. 2019;74(9):1475–1483. 10.1093/gerona/gly248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Liu M, Xue Q-L, Gitlin LN, et al. Disability prevention program improves life-space and falls efficacy: a randomized controlled trial. J Am Geriatr Soc. 2021;69(1):85–90. 10.1111/jgs.16808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Crist K, Jankowska MM, Schipperijn J, et al. Change in GPS-assessed walking locations following a cluster-randomized controlled physical activity trial in older adults, results from the MIPARC trial. Health Place. 2021;69:102573. 10.1016/j.healthplace.2021.102573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Fairhall N, Sherrington C, Kurrle SE, Lord SR, Lockwood K, Cameron ID.. Effect of a multifactorial interdisciplinary intervention on mobility-related disability in frail older people: randomised controlled trial. BMC Med. 2012;10:120. 10.1186/1741-7015-10-120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Dunlap PM, Rosso AL, Zhu X, Klatt BN, Brach JS.. The association of mobility determinants and life space among older adults. J Gerontol A Biol Sci Med Sci. 2021;77:2320–2328. 10.1093/gerona/glab268 [DOI] [PMC free article] [PubMed] [Google Scholar]