Abstract
Purpose of Review
To update and concepts for pediatric physeal-sparing patellofemoral stabilization surgery.
Recent Findings
Recent studies have demonstrated positive results in patellofemoral stabilization in pediatric populations with physeal-sparing techniques that limit the potential for physeal damage. Comprehensive analysis remains limited by population and technique heterogeneity.
Summary
Physeal-sparing patellofemoral stabilization, most significantly through physeal-sparing reconstruction of the medial patellofemoral ligament complex remains a viable option for pediatric patients with recurrent patellofemoral instability.
Keywords: MPFL, Patellar instability, Pediatric, Physis
Introduction
The stability of the patellofemoral joint involves a complex interaction of dynamic joint forces extending above and below the knee. Patellofemoral instability often presents as a traumatic occurrence resulting in lateralization of patellar tracking within the trochlear groove and distal femur with flexion, occurring at an incidence of 23.2 per 100,000 person-years, with the highest incidence between ages 14 and 18 [1]. A single occurrence of lateral patellar dislocation has been shown to rupture the medial patellar tissues between 78 and 100% of the time [2–4]. This includes the strongest attachment at the medial patellofemoral ligament (MPFL) as well as additional tissue proximally and distally making up the medial patellofemoral complex (MPFC) of the knee [5, 6•]. While nonoperative management has been shown to have positive outcomes in certain populations, particularly in first-time dislocators [7, 8], risk factors have significantly increased the chances of recurrent patellofemoral instability. These include younger age, trochlear dysplasia, patella alta, rotational or coronal malalignment, or ligamentous laxity [8].
Hundreds of techniques [9] have been described to surgically stabilize the patellofemoral joint (Fig. 1). These have variably addressed a [10••] range of interventions from simple lateral retinacular release [11] to soft tissue reconstruction [12–15], realignment procedures [16], or trochlear reshaping procedures [17], rotational realignment [18, 19], or even the guided growth [20–22]. While isolated soft tissue procedures have shown poor results for patients with bony abnormalities [23, 24], the best approach for each patient, in each individual scenario, has not been clearly defined.
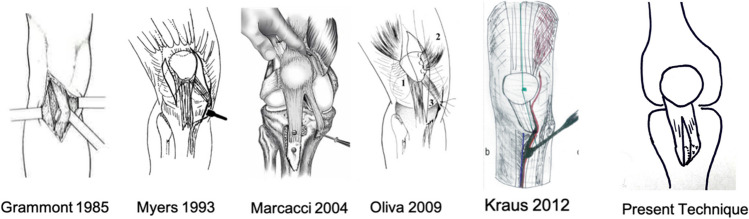
Fig. 1.
Historical techniques of distal extensor mechanism soft tissue realignment
The cornerstone of patellar stabilization procedures remains MPFL reconstruction [25]. Traditional reconstruction in the setting of skeletal immature confers unique risks both at the origin and insertion. On the femur, the MPFL insertion is in close proximity to the distal femoral physis. On the patella, smaller osseous pathways may increase the risk for patellar fracture [26]. More broadly, pediatric patients may have higher levels of activity, and a higher incidence of anatomic predisposing factors such as trochlear dysplasia, patella alta, or increased tibial tubercle – trochlear groove (TT-TG) distance [27••].
Surgical techniques developed to address these challenges are varied. Examples include the use of all-epiphyseal blind-socket femoral tunnel drilling, use of suture anchors [28], pedicled adductor magnus tendon [29, 30], or use of soft tissue pulley at the adductor [31, 32] or medial collateral ligament [33]. To limit complications at the patellar insertion, options may include MQTFL reconstruction [5, 34, 35], or quadriceps turn-down technique [36]. While study heterogeneity has limited the ability to consistently demonstrate a single technique’s superiority, each may highlight important principles in a surgeon’s approach to optimally treating patellar instability in the skeletally immature knee.
Pediatric MPFL Anatomy
Osseous anatomy and proximity to the physis present unique challenges to patellar stabilization in the skeletally immature knee.
The anatomy of the MPFL in relation to the distal femoral physis has been evaluated by several studies [37–44]. Sochacki et al [10••] performed a systematic review of the relationship between the MPFL origin and the distal femoral physis, including seven studies and 298 femurs. Six of seven studies reported the MPFL origin distal to the physis at a mean distance of 6.9 mm. While a guide pin placed at Schottle’s point may appear proximal to the distal extent of the physis on a true lateral view [45, 46], the peripheral flare of the physis in actuality places the insertion within the epiphysis, distally, which provides surgical options for physeal-sparing epiphyseal socket.
To evaluate the clinical outcomes of a blind femoral epiphyseal socket, Upstrom [47] studied 54 patients over nine years with follow-up MRIs or scanograms. Epiphyseal drill holes at the anatomic insertion of the MPFL were found to be 1.9 mm to 12 mm from the physis and epiphyseal sockets resulted in no growth arrests during the study period. Several studies have evaluated the most appropriate trajectory. Irarrazaval [48•] evaluated 80 MRIs with varied trajectories of a 20 mm deep socket and found the worst percent disruption when directed 3 degrees cephalic and 15 degrees posterior, while the safest trajectory was 30–40 degrees distal and 5–35 degrees anterior. Guidelines to aim distally and anteriorly are corroborated by Nguyen [42] who performed a cadaveric study evaluating 8 × 20 mm tunnels and found that if angled less than 10 degrees, 41% violated the growth, while 40% of tunnels that were angled greater than 10 degrees distally would violated the notch if angled less than 10 degrees anterior. The resulting recommendations from this study included the use of an epiphyseal tunnel angled 15–20 degrees both anteriorly and distally. Based on this data, an epiphyseal socket for MPFL reconstruction is a viable option, although surgeons should be aware of the close proximity to the physis and risk of growth arrest.
The MPFL has been shown to insert onto the mid to proximal portion of the patella, approximately 41% down from the superior pole of the patella [49]. Shea [50] performed a cadaveric study of the MPFL insertion on pediatric knees and found the insertion spanned a mean of 41% ( range 24–63%) of the longitudinal width of the patella. In addition, the MPFL itself has been shown to be a component of a broader insertion both above and below the superomedial border of the patella, making up, more broadly, the medial patellofemoral ligament complex (MPFC) [51]. Fibers of the medial structures have been shown to extend to the quadriceps tendon, specifically the vastus intermedius [52] and this has been further supported by pediatric cadaveric studies [50]. Notably, pediatric patients may have added risks secondary to patellar size. Parikh [53] found a 6.5% incidence of patellar fracture with gracilis bone tunnels in the fracture. In turn, several techniques have attempted to utilize this broader patellar and quadriceps tendon insertion to minimize this risk. Options include quadriceps turndown [54], or double-limbed graft with one of two limbs inserted onto the quadriceps tendon [35].
Graft Choice
Both autograft and allograft options have been described and remain viable options for MPFL reconstruction. A systematic review [55] of MPFL reconstructions with both autograft and allograft found no preference based on graft type; however, they did note autograft donor site morbidity. In contrast to studies that have demonstrated inferiority for allograft in ACL reconstruction [56], allograft appears to provide a viable option, and options may include gracilis, semitendinosis, tibialis anterior, or tibialis posterior.
Outcomes of Pediatric MPFL Reconstruction
Although several studies report positive short- and mid-term outcomes [57, 58••], isolated MPFL reconstruction has been shown to have failure rates up to 26% [59]. With varied techniques and patient populations [60] it remains difficult to draw clear superiority of one technique.
In addition, defining failure may be a limitation of historical data, with several studies suggesting that recurrent patellar dislocation may be a limited surrogate for patient outcome. Recent studies include Rueth et al [58••] who presented 101 patients with an average follow-up of 32 months and found only one redislocation, 0.9%. However, only 86% were very satisfied or satisfied with the procedure, and while 86% returned to sport, only 55% achieved a former level of sport. Similarly, Manjunath [61] performed a systematic review and found that only 68% of patients were able to return to play after MPFL reconstruction.
Comprehensive stabilization may seek to address predisposing pathologies such as lateral retinacular tightness, patellar tilt, trochlear dysplasia, patella alta, or increased Q-angle.
Coronal Alignment and Growth Modulation
Coronal plane angular deformity is well-described in the pediatric literature. This has subsequently been associated with increased Q-angle and recurrent patellar instability [62]. Options for growth modulation with open physes include guided growth through percutaneous transphyseal screws [63] or tension band plates [64]. Several studies have demonstrated improved patellar stabilization with correction of coronal alignment, with success rates between 66 and 88% [21, 22, 65]. Nearing skeletal maturity, coronal angular deformity correction requires osteotomy. Wilson [66] presented 11 patients treated with distal femoral valgus osteotomy, achieving a mean of 10.4 degrees of correction, and found 70% of patients achieved good to excellent function and 80% without further episodes of instability. Further studies are needed to understand the importance of intervention in the pediatric population.
Distal Realignment Techniques
For complex adult patellofemoral stabilization, predisposing pathologies such as trochlear dysplasia, increased Q-angle and increased TT-TG distance may be addressed with distal realignment by way tibial tubercle osteotomy [67] (Fig. 1). This procedure typically includes medialization or anteromedialization of the patellar tendon insertion, notably with the potential for increased complication rate, pain, or requiring prolonged rehabilitation [68]. However, in skeletally immature patients with open distal tibial physis, this is contraindicated.
In skeletally immature patients, options may include complete patellar tendon transfer, or Roux-Goldthwaite tendon transfer, which includes transferring the lateral half of the patellar tendon, passing underneath the remaining medial half, and fixing to medial soft tissues [69, 70]. The limitations of Goldthwaite include extensive dissection, complete tendon release, the possibility of inducing patellar tilt (Fig. 3). Below, the authors’ preferred technique which includes partial patellar tendon medialization, concurrent with anatomic, physeal-sparing MPFC reconstruction.
Fig. 3.
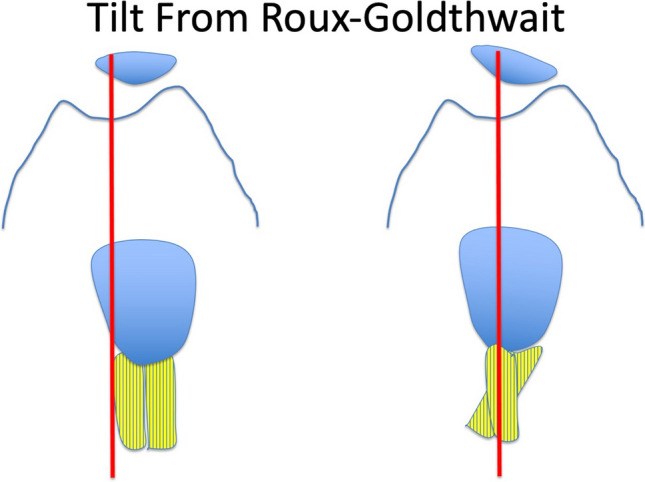
Model of tilt induced from Roux-Goldthwait, in which the lateral half of the patellar tendon insertion is detached and passed underneath attached medial half to create effective extensor mechanism medialization
Authors’ Preferred Technique
We describe our technique for patellar stabilization that includes physeal-sparing MPFC reconstruction, including both the MPFL and MQTFL, as well as physeal respecting distal realignment of the patella tendon insertion. The aim of our technique is to comprehensively address the components to patellofemoral instability in the pediatric patient. Figure 4 represents the combined all-epiphyseal MPFC reconstruction along with a novel extensor realignment involving partial patellar tendon medialization (PPTM).
Fig. 4.
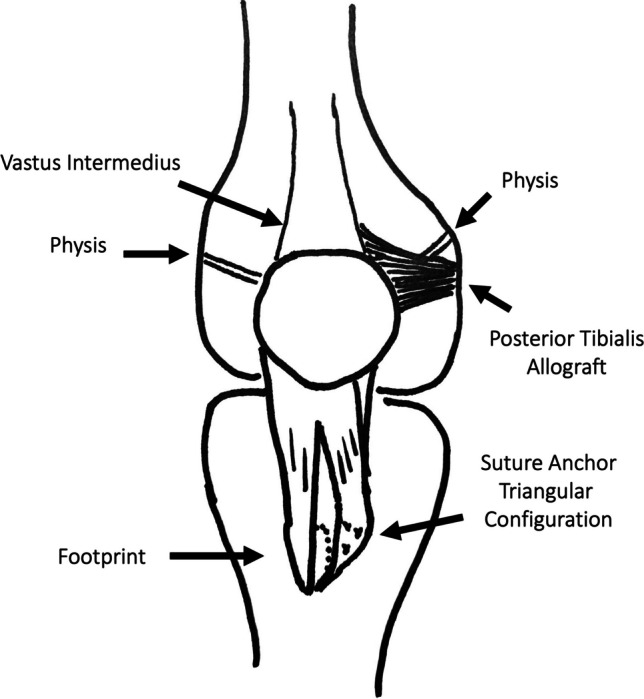
Model of author’s preferred technique of extraphyseal MPFC reconstruction with partial patellar tendon medialization (PPTM) (right knee). The posterior tibialis allograft is placed distal to the medial flare of the distal femoral physis and inserts on the proximal third of the patella and the distal vastus intermedius. This anatomically reconstructs both the MPFL and the MQTFL. The vastus medialis and the vastus lateralis are not pictured. The PPTM utilizes a triangular configuration of suture anchors placed with fixation to the elevated medial footprint, tied with a modified Krakow technique
MPFC Reconstruction
Following initial arthroscopic evaluation, MPFC reconstruction is performed. The present technique reconstructs both the medial patellofemoral ligament (MPFL) and medial quadriceps tendon femoral ligament (MQTFL) using single-strand posterior tibialis tendon allograft.
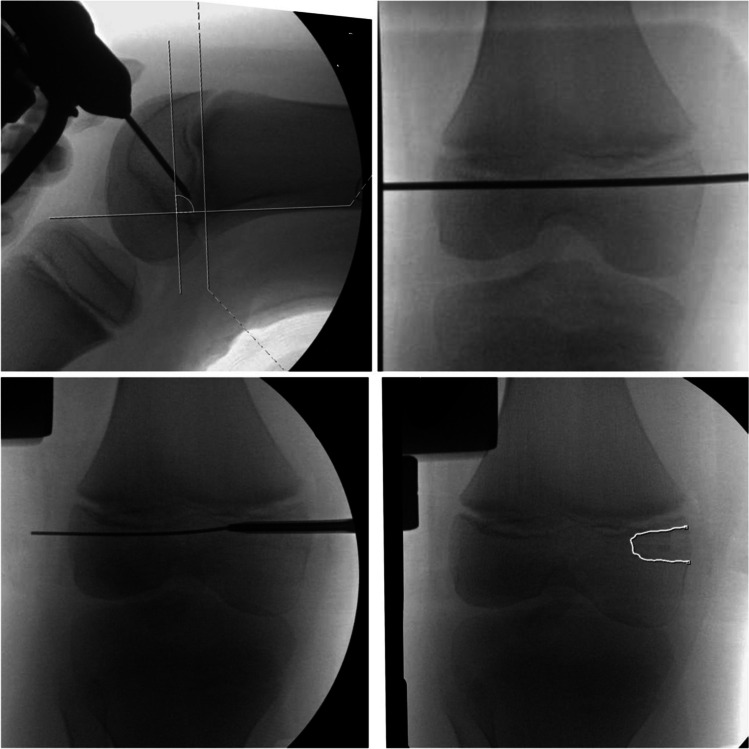
In skeletally immature patients, the femoral insertion is secured first. The narrowed (distal) end of a posterior tibialis allograft is placed at the femoral origin of the MPFL, between the adductor tubercle and medial epicondyle. This is be identified with direct palpation as well as identification of Schottle’s point [71] on a true lateral radiograph. In skeletally-immature patients, this point appears close to the level of the physis on the lateral view [45]. However, on an anteroposterior view or notch view, this point will be shown to be in fact distal to the physis, which flares proximally from its center towards the periphery of the metaphysis [47, 71]. This flaring allows all-epiphyseal femoral tunnel placement when indicated to prevent tunnel drilling across the physis. This is performed using an epiphyseal socket, a tenodesis anchor with a closed eyelet, as has been described in detail previously [14, 47, 72].
As an alternative to a blind socket, a trans-epiphyseal guide pin may be placed starting at Schottle’s point and passing across the epiphysis. Care must be taken to not disrupt the physis proximally, the notch distally, or the trochlea anteriorly (Fig. 2**). Notably, on a true lateral radiograph, Schottle’s point may appear directly in line with the physis, whereas an anteroposterior (AP) view will demonstrate it is distal to the medial flare of the physis, which lies proximal to the true insertion of Schottle’s point. Physeal-sparing MPFC reconstruction is be indicated in patients with significant growth remaining with neutral or varus coronal alignment.
Fig. 2.
demonstrates trans-epiphyseal guidepin placement for all-epiphyseal MPFL femoral socket. This may be performed with careful attention to anatomic MPFC insertion distal to the medial flare of the distal femoral physis
Disruption of the medial distal femoral physis could result in progressive genu varum, which may be protective against patellar instability in the setting of genu valgum, or in patients closer to skeletal maturity. Therefore, traditional transphyseal drilling may be an intended procedural step to effectively induce hemiepiphysiodesis towards the end of growth. However, in this, overcorrection may also be a concern. Our preference is to perform physeal-sparing reconstruction when a patient has neutral alignment and two or more years of growth remaining. However, universal indications for all-epiphyseal versus transphyseal MPFC reconstruction have not been established.
Once secured to the femur, the flared end of the graft will be in an extracapsular fashion a medial and proximal parapatellar incision in preparation for patellar fixation. The patellar insertion is prepared by a 2.5 cm incision just lateral to the medial border of the patella. The thick medial parapatellar retinaculum can distort the medial border of the patella and attention is directed to sharply dissecting down to bone along the medial patella, elevating a small initial flap of periosteum overlying the anterior bone (Fig. 3). Proximally in the incision, the distal quadriceps tendon is identified. A 1 cm incision is made through the medial quadriceps tendon in order to elevate the vastus medialis obliquus (VMO) as a full-thickness flap. In our experience, this facilitates later VMO advancement and assists in the identification of the potential space between the first and second layers of the knee for graft passage. The VMO and medial retinacular flap are elevated, with careful cauterization along medial patella remaining outside the capsular layer. The articular margin of the medial patellar facet can often be palpated through the thinnerπ capsule once the thick overlying tissue is elevated, without direct visualization which would require arthrotomy.
The patellar insertion of the MPFL has been reported previously extensively in the literature [50, 73]. Recent studies have expanded the understanding of the medial soft tissue constraints of the patella and our technique combines recreation of the MPFL as well as the MQTFL proximal insertion onto the vastus lateralis [6•].
Patellar fixation (Fig. 4) is performed with two-three suture anchors placed at the proximal 60% of the medial border of the patella, anterior to the articular cartilage surface. The anchors are oriented in an anterolateral direction, to be directed away from the cartilage surface of the patella. A third attachment is placed at the vastus intermedius tendon, just proximal to the insertion on the superior pole of the patella, beneath the vastus medialis muscle belly. This recreates the anatomic flared insertion of the MPFC along the proximal patella and quadriceps tendon. In addition to anatomically reconstructing the entire extent of the MPFC patellar insertion, this technique minimizes the risk of patellar fracture that has been reported in up to 6.5% [26] of MPFL reconstructions in younger, smaller patients using full patellar drill holes and graft passage. During fixation, the knee is placed at 50 degrees of knee flexion to engage and ‘center’ the patella within the trochlea, and modified Krakow sutures (Fig. 5) are placed through the appropriate points of the graft. This allows secure fixation without overtensioning. Initially, single knots be placed to check patellar tracking through the knee range of motion. These may be untied if altered tension is desired, or reinforced with alternating half-hitches to finalize fixation.
Fig. 5.
demonstrates the planned surgical incisions (A), intraoperative visualization of patellar tendon footprint insertion (B), finalized construct following suture anchor fixation (C), and postsurgical scars (D)
Partial Patellar Tendon Medialization
Following MPFC reconstruction, a 2.5 cm incision is made over the distal fourth of the palpated patellar tendon and its insertion at the tibial tubercle (Fig. 6). A self-retaining retractor is placed and similar to the parapatellar incision is utilized to mobilize the incision to identify proximally and distally, limiting the necessary extent of skin incision. Sharp dissection through the skin and subcutaneous tissue is performed with attention to identify any crossing branches of the infrapatellar branch of the saphenous nerve. The paratenon is incised, and the medial and lateral borders of the distal patellar tendon are confirmed and a midline incision is made sharply through the distal tendon to the level of the cortical bone and periosteum. This extends proximally and distally to release the patellar tendon footprint slightly above the most proximal attachments of the patella tendon to the tibia tubercle. The patellar tendon inserts at the level of the tibial tubercle, with strong anterior attachments to the anterior tibial periosteum. Proximally, the retropatellar fat pad is left intact. An allis clamp facilitates lifting of the medial tendon and a sharp 15-blade knife is utilized to cleanly elevate the medial 50% of the patella tendon footprint off the tubercle. Particularly in younger patients, the patella tendon is contiguous with a very thick and substantial layer of periosteum, which although elevated off the anterior aspect of the tibia, allows the periosteal sleeve to remain securely attached to the tibia distally. The goal of this elevation is to elevate the patella tendon adequately to allow 10–15 mm of medialization of the patellar tendon footprint without disruption of the distal attachment of the footprint (Fig. 4C). Approximately 15 mm of proximo-distal footprint peel typically permits approximately 8-15 mm of medialization. The lateral half of the patella tendon is left completely intact and attached to the tibia. Again, the distal periosteal attachment and even the most distal footprint fibers of the medial half of the footprint remain intact.
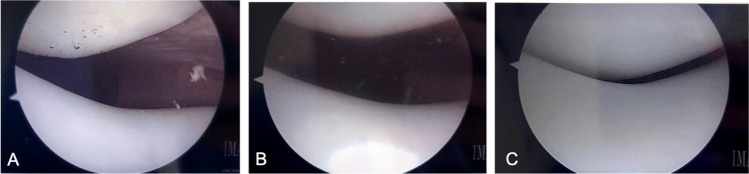
Fig. 6.
Sequential arthroscopic visualization of the patellofemoral joint A before patellar reconstruction, B after comprehensive patellofemoral stabilization, and C dynamic evaluation of knee flexion to 30 degrees showing centralized tracking of the patella within the trochlea
Once the elevation of the footprint is sufficient to permit medialization, suture anchors (FiberTak, Arthrex) are placed in a triangular pattern in order to medialize the medial patellar tendon footprint. This is arranged with the apex pointing medially. Three suture anchors are placed and passed sequentially to medialize the medial patellar tendon footprint. Sutures are passed in a modified-Krackow suture configuration and tied on the undersurface of the tendon, placing the knots below the tendon/periosteal sleeve elevation layer.
The tibial incision is closed in layers. Prior to closure of the medial parapatellar incision, the vastus medialis native MPFL layer is advanced and secured in a standard fashion. Arthroscopy is performed to ensure appropriate post-operative patellar tracking. The patella should engage smoothly in the central trochlea at approximately 25 to 30 degrees of knee flexion without patellar tilt of overtensioning that may cause medial patellofemoral arthrosis (Fig. 6). Approximately two quadrants of lateral patellar mobility should be expected with stress while knee is extended.
Conclusion
Approaches to pediatric patellofemoral stabilization utilize common principles of patellar stabilization within the context of smaller patient size, the presence of open physes, and the potential for increased risk factors for treatment failure. A careful understanding of the relevant anatomy may permit anatomic reconstruction of the medial patellofemoral complex, while nonanatomic procedures such as distal realignment through partial patellar tendon medialization may allow surgeons to comprehensively address relevant pathologies. Patellar stabilization remains viable for skeletally immature patients with recurrent patellofemoral instability.
Declarations
Conflict of Interest
Kevin Shea serves on the medical advisory board for nView and Sarcio.
Tyler Stavinoha declares that he has no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Sanders TL, Pareek A, Hewett TE, Stuart MJ, Dahm DL, Krych AJ. Incidence of first-time lateral patellar dislocation: a 21-year population-based study. Sports Health. 10(2):146–151. 10.1177/1941738117725055. [DOI] [PMC free article] [PubMed]
- 2.Askenberger M, Arendt EA, Ekström W, Voss U, Finnbogason T, Janarv P-M. Medial patellofemoral ligament injuries in children with first-time lateral patellar dislocations: a magnetic resonance imaging and arthroscopic study. Am J Sports Med. 2016;44(1):152–158. doi: 10.1177/0363546515611661. [DOI] [PubMed] [Google Scholar]
- 3.Balcarek P, Ammon J, Frosch S, et al. Magnetic resonance imaging characteristics of the medial patellofemoral ligament lesion in acute lateral patellar dislocations considering trochlear dysplasia, patella alta, and tibial tuberosity-trochlear groove distance. Arthroscopy. 2010;26(7):926–935. doi: 10.1016/j.arthro.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 4.Zhang G-Y, Zheng L, Shi H, Ji B-J, Feng Y, Ding H-Y. Injury patterns of medial patellofemoral ligament after acute lateral patellar dislocation in children: correlation analysis with anatomical variants and articular cartilage lesion of the patella. Eur Radiol. 2017;27(3):1322–1330. doi: 10.1007/s00330-016-4473-5. [DOI] [PubMed] [Google Scholar]
- 5.Joseph SM, Fulkerson JP. Medial quadriceps tendon femoral ligament reconstruction technique and surgical anatomy. Arthrosc Tech. 2019;8(1):e57–e64. doi: 10.1016/j.eats.2018.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.• Tanaka MJ, Voss A, Fulkerson JP. The anatomic midpoint of the attachment of the medial patellofemoral complex. J Bone Jt Surg - Am Vol. 2016;98(14):1199-1205. 10.2106/JBJS.15.01182. Study found midpoint of the medial patellofemoral ligament complex was found at or proximal to the superior articular pole of the patella, and a mean of 2.3% of the patellar articular length distal to the superior pole. [DOI] [PubMed]
- 7.Monson J, Arendt EA. Rehabilitative protocols for select patellofemoral procedures and nonoperative management schemes. Sports Med Arthrosc. 2012;20(3):136–144. doi: 10.1097/JSA.0b013e318263db1c. [DOI] [PubMed] [Google Scholar]
- 8.Mcconnell J, Phty B, Dip G, Ther M. Rehabilitation and nonoperative treatment of patellar instability. 2007;15(2):95-104. [DOI] [PubMed]
- 9.Weeks KD, Fabricant PD, Ladenhauf HN, Green DW. Surgical options for patellar stabilization in the skeletally immature patient. Sports Med Arthrosc. 2012;20(3):194–202. doi: 10.1097/jsa.0b013e3182631707. [DOI] [PubMed] [Google Scholar]
- 10.•• Sochacki KR, Shea KG, Varshneya K, et al. Relationship of the medial patellofemoral ligament origin on the distal femur to the distal femoral physis: a systematic review. Am J Sports Med. 2021;49(1):261-266. 10.1177/0363546520904685. Study provides a systematic review of seven articles evaluating the relation of the MPFL insertion to the distal femoral physis. [DOI] [PubMed]
- 11.Fulkerson JP, Schutzer SF. After failure of conservative treatment for painful patellofemoral malalignment: lateral release or realignment? Orthop Clin North Am. 1986;17(2):283–288. http://www.ncbi.nlm.nih.gov/pubmed/3714212. [PubMed]
- 12.Mj T, Mj B, Jt A, Jp F, Aj C. Complications of medial patellofemoral ligament reconstruction: common technical errors and factors for success. 2012;87:1-8 [DOI] [PubMed]
- 13.Espregueira-mendes J, Ph D, Andrade R, et al. Patellofemoral ligament and medial quadriceps tendon e femoral ligament. Arthrosc Tech. 2019;8(5):e481–e488. doi: 10.1016/j.eats.2019.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ellis Jr HB, Dennis G, Wilson PL. Patellofemoral instability in the skeletally immature patient: a review and technical description of medial patellofemoral ligament reconstruction in patients with open physes. Am J Orthop (Belle Mead, NJ). 2018;47(12). [DOI] [PubMed]
- 15.Nelitz M, Dreyhaupt J, Reichel H, Woelfle J, Lippacher S. Anatomic Reconstruction of the medial patellofemoral ligament in children and adolescents with open growth plates surgical technique and clinical outcome. 58–63. 10.1177/0363546512463683. [DOI] [PubMed]
- 16.Dejour D, Coultre B Le. Osteotomies in patello-femoral instabilities. 2007;15(1):39-46. [DOI] [PubMed]
- 17.Hiemstra LA, Kerslake S, Kupfer N, Lafave MR. Generalized joint hypermobility does not influence clinical outcomes following isolated MPFL reconstruction for patellofemoral instability. Knee Surg Sport Traumatol Arthrosc. 2019;27(11):3660–3667. doi: 10.1007/s00167-019-05489-0. [DOI] [PubMed] [Google Scholar]
- 18.Tian G, Yang G, Zuo L, Li F, Wang F. Femoral derotation osteotomy for recurrent patellar dislocation. Arch Orthop Trauma Surg. 2020;140(12):2077–2084. doi: 10.1007/s00402-020-03598-x. [DOI] [PubMed] [Google Scholar]
- 19.Nelitz M, Dreyhaupt J, Williams SRM, Dornacher D. Combined supracondylar femoral derotation osteotomy and patellofemoral ligament reconstruction for recurrent patellar dislocation and severe femoral anteversion syndrome: surgical technique and clinical outcome. Int Orthop. 2015;39(12):2355–2362. doi: 10.1007/s00264-015-2859-7. [DOI] [PubMed] [Google Scholar]
- 20.Lin KM, Fabricant PD. CORR synthesis: can guided growth for angular deformity correction be applied to management of pediatric patellofemoral instability? Clin Orthop Relat Res. 2020;478(10):2231–2238. doi: 10.1097/CORR.0000000000001311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kearney SP, Mosca VS. Selective hemiepiphyseodesis for patellar instability with associated genu valgum. J Orthop. 2015;12(1):17–22. doi: 10.1016/j.jor.2015.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Parikh SN, Redman C, Gopinathan NR. Simultaneous treatment for patellar instability and genu valgum in skeletally immature patients: a preliminary study. J Pediatr Orthop Part B. 2019;28(2):132–138. doi: 10.1097/BPB.0000000000000546. [DOI] [PubMed] [Google Scholar]
- 23.Huntington LS, Webster KE, Devitt BM, Scanlon JP, Feller JA. Factors associated with an increased risk of recurrence after a first-time patellar dislocation: a systematic review and meta-analysis. Am J Sports Med. 2020;48(10):2552–2562. doi: 10.1177/0363546519888467. [DOI] [PubMed] [Google Scholar]
- 24.Sappey-Marinier E, Sonnery-Cottet B, O’Loughlin P, et al. Clinical outcomes and predictive factors for failure with isolated MPFL reconstruction for recurrent patellar instability: a series of 211 reconstructions with a minimum follow-up of 3 years. Am J Sports Med. 2019;47(6):1323–1330. doi: 10.1177/0363546519838405. [DOI] [PubMed] [Google Scholar]
- 25.Stupay KL, Swart E, Shubin Stein BE. Widespread implementation of medial patellofemoral ligament reconstruction for recurrent patellar instability maintains functional outcomes at midterm to long-term follow-up while decreasing complication rates: a systematic review. Arthroscopy. 2015;31(7):1372–1380. doi: 10.1016/j.arthro.2014.12.029. [DOI] [PubMed] [Google Scholar]
- 26.Parikh SN, Wall EJ. Patellar fracture after medial patellofemoral ligament surgery: a report of five cases. J Bone Jt Surg Ser A. 2011;93(17):1–8. doi: 10.2106/JBJS.J.01558. [DOI] [PubMed] [Google Scholar]
- 27.•• Hobson T, Mortensen A, Tomasevich K, Adeyemi T, Aoki S, Quinlan N. MPFL reconstruction in the pediatric population: does skeletal maturity matter? Orthop J Sport Med. 2021;9(7_suppl4):2325967121S0023. 10.1177/2325967121s00233. This study provides a retrospective review comparing pediatric to adult patellar stabilization procedures and found a higher incidence of trochlear dysplasia (88% versus 63%) and a revision rate in the pediatric cohort of 23%.
- 28.Hidalgo Perea S, Shannon SR, Green DW. Medial patellofemoral ligament reconstruction with open physes. Clin Sports Med. 2022;41(1):97–108. doi: 10.1016/j.csm.2021.07.004. [DOI] [PubMed] [Google Scholar]
- 29.Sillanpää PJ, Mäenpää HM, Mattila VM, Visuri T, Pihlajamäki H. A mini-invasive adductor magnus tendon transfer technique for medial patellofemoral ligament reconstruction: a technical note. Knee Surg Sports Traumatol Arthrosc. 2009;17(5):508–512. doi: 10.1007/s00167-008-0713-9. [DOI] [PubMed] [Google Scholar]
- 30.Avikainen VJ, Nikku RK, Seppänen-Lehmonen TK. Adductor magnus tenodesis for patellar dislocation. Technique and preliminary results. Clin Orthop Relat Res. 1993;(297):12–16. http://www.ncbi.nlm.nih.gov/pubmed/8242919. [PubMed]
- 31.Monllau JC, Masferrer-Pino À, Ginovart G, Pérez-Prieto D, Gelber PE, Sanchis-Alfonso V. Clinical and radiological outcomes after a quasi-anatomical reconstruction of medial patellofemoral ligament with gracilis tendon autograft. Knee Surg Sports Traumatol Arthrosc. 2017;25(8):2453–2459. doi: 10.1007/s00167-015-3934-8. [DOI] [PubMed] [Google Scholar]
- 32.Pérez-Prieto D, Capurro B, Gelber PE, et al. The anatomy and isometry of a quasi-anatomical reconstruction of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2017;25(8):2420–2423. doi: 10.1007/s00167-015-3865-4. [DOI] [PubMed] [Google Scholar]
- 33.Deie M, Ochi M, Sumen Y, Yasumoto M, Kobayashi K, Kimura H. Reconstruction of the medial patellofemoral ligament for the treatment of habitual or recurrent dislocation of the patella in children. J Bone Joint Surg Br. 2003;85(6):887–890. http://www.ncbi.nlm.nih.gov/pubmed/12931813. [PubMed]
- 34.Joseph SM, Fulkerson JP, Tanaka MJ, et al. Editorial commentary: the best medial patellofemoral reconstruction may include components of both quadriceps and patellar attachments. Arthrosc J Arthrosc Relat Surg. 2019;36(2):1677–1678. doi: 10.1016/j.arthro.2020.02.034. [DOI] [PubMed] [Google Scholar]
- 35.Spang RC, Tepolt FA, Paschos NK, Redler LH, Davis EA, Kocher MS. Combined reconstruction of the medial patellofemoral ligament (MPFL) and medial quadriceps tendon-femoral ligament (MQTFL) for patellar instability in children and adolescents: Surgical technique and outcomes. J Pediatr Orthop. 2019;39(1):e54–e61. doi: 10.1097/BPO.0000000000001259. [DOI] [PubMed] [Google Scholar]
- 36.Fisher M, Singh S, Samora WP, Beran MC, Klingele KE. Outcomes of MPFL reconstruction utilizing a quadriceps turndown technique in the adolescent/pediatric population. J Pediatr Orthop. Published online April 23, 2021. 10.1097/BPO.0000000000001836. [DOI] [PubMed]
- 37.Shea KG, Polousky JD, Jacobs JC, et al. The relationship of the femoral physis and the medial patellofemoral ligament in children. Am J Sports Med. 2016;44(11):2833–2837. doi: 10.1177/0363546516656366. [DOI] [PubMed] [Google Scholar]
- 38.Shea KG, Grimm NL, Belzer J, Burks RT, Pfeiffer R. The relation of the femoral physis and the medial patellofemoral ligament. Arthrosc J Arthrosc Relat Surg. 2010;26(8):1083–1087. doi: 10.1016/j.arthro.2009.12.020. [DOI] [PubMed] [Google Scholar]
- 39.Lee BJ, Christino MA, Eberson CP. Adolescent patellar osteochondral fracture following patellar dislocation. Published online 2013:1856–1861. 10.1007/s00167-012-2179-z. [DOI] [PubMed]
- 40.Shea KG, Polousky JD, Jacobs JC, et al. The relationship of the femoral physis and the medial patellofemoral ligament in children: a cadaveric study. J Pediatr Orthop. 2014;34(8):808–813. doi: 10.1097/BPO.0000000000000165. [DOI] [PubMed] [Google Scholar]
- 41.Nelitz M, Dornacher D, Dreyhaupt J, Reichel H, Lippacher S. The relation of the distal femoral physis and the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2011;19(12):2067–2071. doi: 10.1007/s00167-011-1548-3. [DOI] [PubMed] [Google Scholar]
- 42.Nguyen CV, Farrow LD, Liu RW, Gilmore A. Safe drilling paths in the distal femoral epiphysis for pediatric medial patellofemoral ligament reconstruction. Am J Sports Med. 2017;45(5):1085–1089. doi: 10.1177/0363546516677795. [DOI] [PubMed] [Google Scholar]
- 43.Farrow LD, Alentado VJ, Abdulnabi Z, Gilmore A, Liu RW. The relationship of the medial patellofemoral ligament attachment to the distal femoral physis. Am J Sports Med. 2014;42(9):2214–2218. doi: 10.1177/0363546514539917. [DOI] [PubMed] [Google Scholar]
- 44.Bishop ME, Black SR, Nguyen J, Mintz D, Stein BS. A simple method of measuring the distance from the schöttle point to the medial distal femoral physis with MRI. Orthop J Sport Med. 2019;7(4):1–6. doi: 10.1177/2325967119840713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shea KG, Grimm NL, Belzer J, Burks RT, Pfeiffer R. The relation of the femoral physis and the medial patellofemoral ligament. Arthrosc J Arthrosc Relat Surg. 2010;26(8):1083–1087. doi: 10.1016/j.arthro.2009.12.020. [DOI] [PubMed] [Google Scholar]
- 46.Ellis HB, Dennis G, Wilson PL. Patellofemoral instability in the skeletally immature patient: a review and technical description of medial patellofemoral ligament reconstruction in patients with open physes. Am J Orthop (Belle Mead NJ). 2018;47(12). 10.12788/ajo.2018.0110. [DOI] [PubMed]
- 47.Uppstrom TJ, Price M, Black S, Gausden E, Haskel J, Green DW. Medial patellofemoral ligament (MPFL) reconstruction technique using an epiphyseal femoral socket with fluoroscopic guidance helps avoid physeal injury in skeletally immature patients. Knee Surg Sport Traumatol Arthrosc. 2019;27(11):3536–3542. doi: 10.1007/s00167-019-05412-7. [DOI] [PubMed] [Google Scholar]
- 48.• Irarrázaval S, Besa P, Fernández F, et al. Anterior and distal tunnel orientation for anatomic reconstruction of the medial patellofemoral ligament is safer in patients with open growth plates. Knee Surg Sport Traumatol Arthrosc. 2021;29(6):1822-1829. 10.1007/s00167-020-06229-5. This study provided MRI evaluation of the ideal femoral tunnel orientation in the setting of skeletal immaturity. The safest zone was obtained hwen aiming 30 to 40 degrees distal and 5 to 35 degrees anterior, regardless of sex. [DOI] [PubMed]
- 49.LaPrade MD, Kennedy MI, Wijdicks CA, LaPrade RF. Anatomy and biomechanics of the medial side of the knee and their surgical implications. Sports Med Arthrosc. 2015;23(2):63–70. doi: 10.1097/JSA.0000000000000054. [DOI] [PubMed] [Google Scholar]
- 50.Shea KG, Polousky JD, Jacobs JC, et al. The patellar insertion of the medial patellofemoral ligament in children: a cadaveric study. J Pediatr Orthop. 2015;35(4):e31–e35. doi: 10.1097/BPO.0000000000000399. [DOI] [PubMed] [Google Scholar]
- 51.Christian DR, Redondo ML, Cancienne JM, et al. Differential contributions of the quadriceps and patellar attachments of the proximal medial patellar restraints to resisting lateral patellar translation. Arthrosc J Arthrosc Relat Surg. 2020;36(6):1670–1676. doi: 10.1016/j.arthro.2020.01.058. [DOI] [PubMed] [Google Scholar]
- 52.Tanaka MJ, Cosgarea AJ. Medial patellofemoral ligament reconstruction. Oper Tech Knee Surg Second Ed. 2018;20(3):295–303. doi: 10.1016/B978-0-323-46292-1.00032-0. [DOI] [Google Scholar]
- 53.Parikh SN, Wall EJ. Patellar fracture after medial patellofemoral ligament surgery: a report of five cases. J Bone Joint Surg Am. 2011;93(17):e97(1–8). 10.2106/JBJS.J.01558. [DOI] [PubMed]
- 54.Fisher M, Singh S, Samora WP, Beran MC, Klingele KE. Outcomes of MPFL reconstruction utilizing a quadriceps turndown technique in the adolescent/pediatric population. J Pediatr Orthop. 2021;41(7):E494–E498. doi: 10.1097/BPO.0000000000001836. [DOI] [PubMed] [Google Scholar]
- 55.McNeilan RJ, Everhart JS, Mescher PK, Abouljoud M, Magnussen RA, Flanigan DC. Graft choice in isolated medial patellofemoral ligament reconstruction: a systematic review with meta-analysis of rates of recurrent instability and patient-reported outcomes for autograft, allograft, and synthetic options. Arthroscopy. 2018;34(4):1340–1354. doi: 10.1016/j.arthro.2017.11.027. [DOI] [PubMed] [Google Scholar]
- 56.Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, MOON Consortium, Spindler KP. Risk Factors and predictors of subsequent acl injury in either knee after ACL reconstruction: prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015;43(7):1583–1590. 10.1177/0363546515578836. [DOI] [PMC free article] [PubMed]
- 57.Nelitz M, Dreyhaupt J, Reichel H, Woelfle J, Lippacher S. Anatomic reconstruction of the medial patellofemoral ligament in children and adolescents with open growth plates: Surgical technique and clinical outcome. Am J Sports Med. 2013;41(1):58–63. doi: 10.1177/0363546512463683. [DOI] [PubMed] [Google Scholar]
- 58.•• Rueth M-J, Koehl P, Schuh A, Goyal T, Wagner D. Return to sports and short-term follow-up of 101 cases of medial patellofemoral ligament reconstruction using gracilis tendon autograft in children and adolescents. Arch Orthop Trauma Surg. Published online February 16, 2022. 10.1007/s00402-022-04365-w. This study evlauated short term results and return to sport for 101 isolated MPFL reconstructions using gracilis autograft. 84% of patients were satisfied or very satisfied with their surgery. Complication rate was 2.9% and redislocation rate was 0.9% at short-term follow-up. [DOI] [PubMed]
- 59.Shah JN, Howard JS, Flanigan DC, Brophy RH, Carey JL, Lattermann C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012;40(8):1916–1923. doi: 10.1177/0363546512442330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tompkins MA, Arendt EA. Patellar instability factors in isolated medial patellofemoral ligament reconstructions - what does the literature tell us?: a systematic review. Am J Sports Med. 2015;43(9):2318–2327. doi: 10.1177/0363546515571544. [DOI] [PubMed] [Google Scholar]
- 61.Manjunath AK, Hurley ET, Jazrawi LM, Strauss EJ. Return to play after medial patellofemoral ligament reconstruction: a systematic review. Am J Sports Med. 2021;49(4):1094–1100. doi: 10.1177/0363546520947044. [DOI] [PubMed] [Google Scholar]
- 62.Dickschas J, Harrer J, Bayer T, Schwitulla J, Strecker W. Correlation of the tibial tuberosity-trochlear groove distance with the Q-angle. Knee Surg Sports Traumatol Arthrosc. 2016;24(3):915–920. doi: 10.1007/s00167-014-3426-2. [DOI] [PubMed] [Google Scholar]
- 63.Khoury JG, Tavares JO, McConnell S, Zeiders G, Sanders JO. Results of screw epiphysiodesis for the treatment of limb length discrepancy and angular deformity. J Pediatr Orthop. 2007;27(6):623–628. doi: 10.1097/BPO.0b013e318093f4f4. [DOI] [PubMed] [Google Scholar]
- 64.Stevens PM. Guided growth for angular correction: a preliminary series using a tension band plate. J Pediatr Orthop. 27(3):253–259. 10.1097/BPO.0b013e31803433a1. [DOI] [PubMed]
- 65.Lin KM, Thacher RR, Apostolakos JM, Heath MR, Mackie AT, Fabricant PD. implant-mediated guided growth for coronal plane angular deformity in the pediatric patient with patellofemoral instability. Arthrosc Tech. 2021;10(3):e913–e924. doi: 10.1016/j.eats.2020.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wilson PL, Black SR, Ellis HB, Podeszwa DA. Distal femoral valgus and recurrent traumatic patellar instability : is an isolated varus producing distal femoral osteotomy a treatment option ? 2018;00(00):1–6. 10.1097/BPO.0000000000001128. [DOI] [PubMed]
- 67.Sherman SL, Erickson BJ, Cvetanovich GL, et al. Tibial tuberosity osteotomy: indications, techniques, and outcomes. Am J Sports Med. 2014;42(8):2006–2017. doi: 10.1177/0363546513507423. [DOI] [PubMed] [Google Scholar]
- 68.Erickson BJ, Nguyen J, Gasik K, Gruber S, Brady J, Shubin Stein BE. Isolated medial patellofemoral ligament reconstruction for patellar instability regardless of tibial tubercle–trochlear groove distance and patellar height: outcomes at 1 and 2 Years. Am J Sports Med. 2019;47(6):1331–1337. doi: 10.1177/0363546519835800. [DOI] [PubMed] [Google Scholar]
- 69.Trivellas M, Arshi A, Beck JJ. Roux-Goldthwait and Medial Patellofemoral ligament reconstruction for patella realignment in the skeletally immature patient. Arthrosc Tech. 2019;8(12):e1479–e1483. doi: 10.1016/j.eats.2019.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Marsh JS, Daigneault JP, Sethi P, Polzhofer GK. Treatment of recurrent patellar instability with a modification of the Roux-Goldthwait technique. J Pediatr Orthop. 2006;26(4):461–465. doi: 10.1097/01.bpo.0000217711.34492.48. [DOI] [PubMed] [Google Scholar]
- 71.Huston KL, Okoroafor UC, Kaar SG, Wentt CL, Saluan P, Farrow LD. ¨ ttle Technique Evaluation of the Scho in the Pediatric Knee. Published online 2017:1–5. 10.1177/2325967117740078. [DOI] [PMC free article] [PubMed]
- 72.Haskel JD, Uppstrom TJ, Gausden EB, Green DW. Low risk of physeal damage from a medial patellofemoral ligament (MPFL) reconstruction technique that uses an epiphyseal socket in children. Orthop J Sport Med. 2015;3(7):1. doi: 10.1177/2325967115S00038. [DOI] [Google Scholar]
- 73.Philippot R, Chouteau J, Wegrzyn J, Testa R, Fessy MH, Moyen B. Medial patellofemoral ligament anatomy: implications for its surgical reconstruction. Knee Surg Sport Traumatol Arthrosc. 2009;17(5):475–479. doi: 10.1007/s00167-009-0722-3. [DOI] [PubMed] [Google Scholar]