Abstract
Objectives
Guideline adherence is one of the most important objectives for antibiotic stewardship. The Dutch Working Party on Antibiotic Policy (SWAB) developed an online national guide (SWAB-ID) in 2006. Every Dutch hospital is offered the opportunity to customize the national version to their local context and distribute it through an independent website. We studied user data to see how often the guidelines on therapy, prophylaxis and medication are used.
Methods
Data on usage between 19 June 2020 and 30 June 2022 were extracted through Google Analytics for the national site and the 53 hospitals using a customized version of the national guide. User data were divided into three main groups: users of the national guide SWAB-ID, and users of the sites of general hospitals and university hospitals.
Results
A total of 1 837 126 searches were analysed, of which 1 393 681 (75.9%) concerned therapy, 111 774 (6.1%) prophylaxis and 331 671 (18%) medication. Of these searches, 456 854 (24.9%) were performed on the national site, 950 887 (51.8%) by general hospitals and 429 385 (23.4%) by university hospitals. The most commonly searched tracts among all user groups were lower respiratory tract (21.8%), kidney and urinary tract (16.6%) and skin and soft tissues (11.8%). The most commonly searched conditions were community-acquired pneumonia (15.3%), cystitis (13.5%) and sepsis (11.3%). The top ranked pages on medication differed for the three categories of users.
Conclusions
The SWAB-ID antimicrobial guide is used extensively by both general and university hospitals. The online guide can help in prescribing therapy according to the guideline.
Introduction
An estimated 17%–57% of hospital treatments with antibiotics are in fact unnecessary or inappropriate.1–3 Antibiotic stewardship programmes have been developed to optimize hospital antibiotic use, which can be defined by several quality indicators.4,5 One of these quality indicators is described as follows: ‘empirical antibiotic therapy is prescribed according to the guideline’. Adhering to the guideline has been shown to be associated with a reduction in treatment failure, hospital length of stay, costs and mortality.6
In the Netherlands, having a hospital antimicrobial guide is mandatory. Since the advent of the internet, electronic resources have become important tools for obtaining information and improving antimicrobial programmes in everyday practice.7–9 An online national antimicrobial guide was then created in 2006 by the Dutch Working Party on Antibiotic Policies (SWAB): SWAB-ID (www.swabid.nl).10 The recommendations on treatment and prophylaxis of infectious diseases in hospitals are evidence-based where possible or, in the absence of published guidelines, offer several equivalent alternatives based on the antimicrobial policies in the nine Dutch hospitals that have an infectious diseases or medical microbiology residency programme. The online national antimicrobial guide is accessible for everyone and content of the guide is frequently evaluated and updated when new guidelines are released. In addition, every hospital in the Netherlands is offered the opportunity to customize the national version to their local context and resources and distribute it through an independent website, which is linked to the national site. These local versions of the guide can be facilitated for a small annual fee. Antimicrobial guide updates are provided by the national editorial board, but need to be released by the local administrator.
To our knowledge, no other country has a similar national antibiotic guide with local derivatives. We have previously shown that hospitals using a local version of SWAB-ID customized to the local environment have a more comprehensive and guideline-compliant antibiotic policy than hospitals that have chosen to fully design their own guide.11 With current technology enabling insight into user data, we examined the use of various SWAB-ID sections over time and whether there are differences in usage patterns between the national site and its derived local versions.
Methods
The board of SWAB was notified about the intended study and we were granted full access to the data after careful description of the study and guaranteeing anonymization of data. Data were extracted through Google Analytics, in accordance with the European General Data Protection Regulation.12
Data collection and outcomes
First, a list was made of all local, customizable versions of the online SWAB-ID antimicrobial guide, with the number of hospitals that made use of that specific version. We included Dutch hospitals providing adult patient care. Children’s hospitals, hospitals with outpatient care only and versions of the guide used for demonstration purposes were excluded. For observing changes in time, we included data from 19 June 2020 until 30 June 2022. We included only hospitals that had been using the online antimicrobial guide for at least 1 year.
We studied the following categories within the online antimicrobial guide: therapy (specified per tract, the various clinical syndromes or anatomical locations, and if applicable causative agents), prophylaxis (i.e. surgical prophylaxis, endocarditis, immunocompromised hosts, post-exposition and treatment of latent TB) and medication (i.e. antibacterial, antifungal, antiparasitic, antiviral and other). The latter contains information regarding safety margins for dosing, dosage when there is ‘increased dosage’ sensitivity, dosage adjusted to kidney function etc.
As of June 2022, the national SWAB-ID antimicrobial guide consisted of 242 unique web pages with advice on therapy, prophylaxis or medication. Since local hospitals are able to customize the national version according to local needs, including the description of conditions, the description of one single therapy condition may vary (e.g. ‘community-acquired pneumonia—aspiration’ versus ‘aspiration pneumonia’). We therefore assembled a list of 53 therapy conditions with uniform terminology (e.g. ‘osteomyelitis’ without differentiating between acute or chronic) in our database. We selected conditions considered to be the most prevalent based on expert opinion (J.M.P., E.C.S.) (Table S1, available as Supplementary data at JAC-AMR Online). For community-acquired pneumonia (CAP), we distinguished consultation of therapy advice for ‘unknown pathogens’ from those for pathogen-directed therapy, to explore the hypothesis that the antibiotic guide is consulted more often for empirical rather than pathogen-directed therapy. The sections on prophylaxis and medication are usually not locally customized, and the description of these sections are therefore more uniform across sites.
Users were divided into three main groups: users of the national SWAB-ID site, and users of a local version of the online antimicrobial guide in general hospitals and in university hospitals.
Statistical analysis
We defined a web session as each time the national or a local site was accessed. To describe search characteristics, we calculated the total number of searches (defined as the sum of page views within the total number of web sessions) and total number of searches according to the day of the week. These statistics were reported overall and according to page category (i.e. therapy, prophylaxis, medication). To describe the volume of searches over time, we calculated the total number of searches per month.
We then performed more specific analysis on search content by summarizing the distribution of the 20 selected tracts, 20 selected conditions (most common of the 53 predefined terms, Table S1), 6 selected prophylaxis categories, and 5 selected medication categories searched over the entire study period. Since the size of a hospital could influence the frequency of antimicrobial guide usage, we also adjusted percentages using direct standardization across hospitals, which were weighted by the proportion of beds in the hospital over the total number of beds in the sample.
Finally, we estimated the frequency of specific searches over time using Poisson regression. The total number of searches for a given category was modelled across interval months, while the total number of searches overall (per month) was constrained to one. For each category, the modelled search frequencies were plotted by months and a line was fitted using kernel-weighted local polynomial smoothing.
We carried out analyses in the overall sample and stratified on user group. Statistical analysis was performed using STATA (v15.1, College Station, TX, USA). The large number of entries rendered most comparisons highly overpowered, hence we did not perform any formal statistical testing.
Results
The national guide SWAB-ID entails a single national website and 37 local, customizable versions. Currently, 60 of 76 Dutch non-paediatric hospitals are affiliated with SWAB-ID. This includes 54 of 69 general hospitals and 6 of 7 university hospitals. Included in the present study are 35 local, customizable versions of the guide, covering 53 hospitals that used SWAB-ID for at least 1 year prior to start of data collection.
Description of included searches
Of the 982 887 web sessions retrieved, we excluded 62 297 since they were from outside the Netherlands (n = 27 648), were from sites that had participated for less than 1 year (n = 13 087), were used for demonstration purposes (n = 94), concerned children’s hospitals and hospitals with outpatient care only (n = 21 400) or were from non-hospital-related sources (n = 68). The remaining 920 590 web sessions contained 1 837 126 searches, which were used in analysis and of which 1 393 681 (75.9%) were related to therapy, 111 774 (6.1%) to prophylaxis and 331 671 (18%) to medication. Of these searches, the majority were performed by users from general hospitals (n = 950 887; 51.8%), followed by the national site (n = 456 854; 24.9%) and university hospitals (n = 429 385; 23.4%).
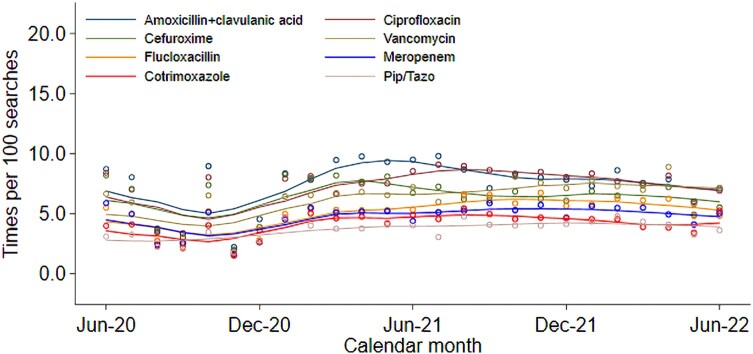
Searches over time
Figure 1 displays the number of searches from 19 June 2020 until 30 June 2022 per month for the national SWAB-ID guide, as well as for the general and university hospitals. The number of affiliated hospitals (53) did not change during this time. The overall number of searches per month fluctuated during the first year of our study, varying between 25 000 and 175 000 searches per month. In the second year, starting June 2021, this total stabilized to around 70 000 searches per month. The ratio between the number of monthly searches of the national SWAB-ID guide, general and university hospitals remained consistent.
Figure 1.
Number of monthly searches, from 19 June 2020 to 30 June 2022.
The distribution of searches during the week is shown in Table 1. During weekdays the number of searches was on average constant; on Saturdays and Sundays the number of searches was lower.
Table 1.
Distribution of searches during the week
| Day | n | % |
|---|---|---|
| Sunday | 104.203 | 5.67 |
| Monday | 367.545 | 19.99 |
| Tuesday | 306.712 | 16.68 |
| Wednesday | 339.557 | 18.47 |
| Thursday | 314.943 | 17.13 |
| Friday | 310.328 | 16.88 |
| Saturday | 95.007 | 5.17 |
Searches related to therapy (tracts)
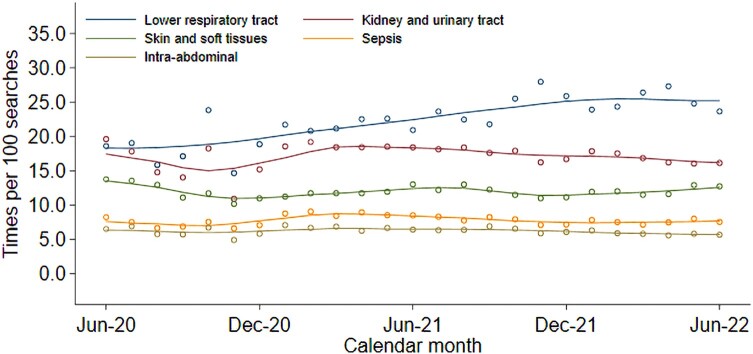
Table 2 displays the distribution of searches on therapy, given for each of the 20 tracts. The most commonly searched tracts were lower respiratory tract (n = 303 948 searches; 21.8%), kidney and urinary tract (n = 231 775 searches; 16.6%), and skin and soft tissue (n = 164 834 searches; 11.8%). This ranking was comparable for all three main user groups except among university hospital users, where the third most consulted tract was sepsis (n = 32 682 searches; 10.7%). When adjusted for the number of beds per healthcare institute, sepsis also ranked third among general hospital users (n = 55 270 searches; 7.6% unadjusted, 11.9% adjusted).
Table 2.
Distribution of searches on therapy, per tract
| Total (n = 1 394 850)a | National site (N = 359 489) | University hospitals (N = 304 613) | General hospitals (N = 730 748) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Tract | n | Unadj % | n | Unadj % | n | Unadj % | Adjb % | n | Unadj % | Adjb % |
| Bone and joint | 71 470 | 5.12 | 14 647 | 4.1 | 17 654 | 5.8 | 6.2 | 39 169 | 5.4 | 6.1 |
| CNS | 49 734 | 3.57 | 11 855 | 3.3 | 16 707 | 5.5 | 7.2 | 21 172 | 2.9 | 4.7 |
| Ear, nose and sinus | 18 288 | 1.31 | 7401 | 2.1 | 3848 | 1.3 | 1.6 | 7039 | 1.0 | 1.4 |
| Eye | 22 250 | 1.60 | 6119 | 1.7 | 6302 | 2.1 | 3.4 | 9829 | 1.3 | 2.8 |
| Gastrointestinal infections | 77 896 | 5.58 | 27 611 | 7.7 | 14 181 | 4.7 | 5.8 | 36 104 | 4.9 | 5.5 |
| Heart and thorax | 38 881 | 2.79 | 6206 | 1.7 | 14 075 | 4.6 | 4.1 | 18 600 | 2.5 | 2.4 |
| HIV-related and other opportunistic infections | 24 112 | 1.73 | 7855 | 2.2 | 5721 | 1.9 | 1.9 | 10 536 | 1.4 | 2.4 |
| ICU carec | 2749 | 0.20 | 0 | 0 | 2749 | 0.9 | 1.4 | 0 | 0 | 0 |
| Intra-abdominal infections | 85 197 | 6.11 | 18 102 | 5.0 | 18 817 | 6.2 | 7.6 | 48 278 | 6.6 | 4.7 |
| Kidney and urinary tract | 231 775 | 16.62 | 53 095 | 14.8 | 41 875 | 13.7 | 9.5 | 136 805 | 18.7 | 12.2 |
| Lower respiratory tract | 303 948 | 21.79 | 67 025 | 18.6 | 65 537 | 21.5 | 14.5 | 171 386 | 23.5 | 15.6 |
| Mouth and upper respiratory tract | 44 126 | 3.16 | 16 393 | 4.6 | 9223 | 3.0 | 4.4 | 18 510 | 2.5 | 3.8 |
| Mycobacterial infections | 399 | 0.03 | 0 | 0 | 350 | 0.1 | 0.2 | 49 | 0 | 0 |
| Sepsisd | 106 794 | 7.66 | 18 842 | 5.2 | 32 682 | 10.7 | 8.7 | 55 270 | 7.6 | 11.9 |
| Skin and soft tissues | 164 834 | 11.82 | 50 670 | 14.1 | 27 291 | 9.0 | 8.2 | 86 873 | 11.9 | 11.7 |
| STDs, sexual organs, obstetrics | 63 954 | 4.59 | 23 220 | 6.5 | 8539 | 2.8 | 4.0 | 32 195 | 4.4 | 5.0 |
| Systemic fungal infections | 36 846 | 2.64 | 13 898 | 3.9 | 7631 | 2.5 | 2.0 | 15 317 | 2.1 | 2.7 |
| Tropical and parasitic infections | 44 800 | 3.21 | 15 578 | 4.3 | 8325 | 2.7 | 7.9 | 20 897 | 2.9 | 6.7 |
| TB | 2697 | 0.19 | 972 | 0.3 | 384 | 0.1 | 0.1 | 1341 | 0.2 | 0.3 |
| Viral infectionsc | 2931 | 0.21 | 0 | 0 | 2722 | 0.9 | 1.3 | 209 | 0 | 0 |
Adj, adjusted; unadj, unadjusted; STD, sexual transmitted disease.
aOf the 1 394 850 pages in the ‘therapy’ rubric, 1169 could not be analysed as the tract search term was unclear.
bAdjusted for number of beds in healthcare institutions; only applies to university and general hospitals.
cSubcategory not included in the national site, but used by a number of websites/healthcare institutions.
dDefinition based on the term used to search for specific tracts.
Figure 2 shows the overall distribution of the five most commonly searched tracts over time. There is a clearly visible increase in the number of searches starting November 2020 regarding the lower respiratory tract. This coincided with the second COVID-19 wave in the Netherlands. Figure S1 displays the search for these five tracts over time for the national SWAB-ID guide (a), university (b) and general hospitals (c).
Figure 2.
Distribution of the five most searched tracts over time.
Searches related to therapy (conditions)
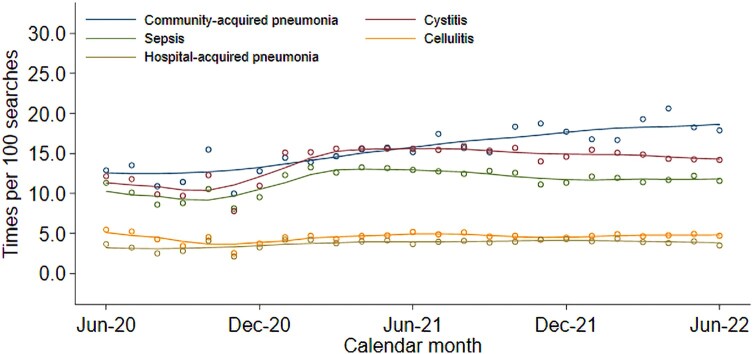
Table 3 displays the distribution of the 20 most commonly searched therapy conditions, out of our 53 previously selected conditions with uniform terms (Table S1). These 20 conditions represented 1 119 013 searches, which is 80% of the total number of therapy searches. The most commonly searched conditions were CAP (n = 213 314 searches; 15.3%), cystitis (n = 188 193 searches; 13.5%), sepsis (n = 157 588 searches; 11.3%), cellulitis (n = 61 842 searches; 4.4%) and hospital-acquired pneumonia (n = 50 894 searches; 3.6%). This ranking was mostly driven by the large number of searches from general hospitals (Table 3). Meningitis ranked tenth and fifth among national users and users from university hospitals (n = 7530 and n = 13 311 searches, respectively), while not even in the first 10 conditions searched by general hospital users. Figure 3 shows the overall distribution of the five most commonly searched conditions over time. There is a steady increase in the number of searches on CAP after December 2020. For both cystitis and sepsis we observed an increase in the number of consultations starting in 2021. Figure S2 displays the five most commonly searched conditions over time for the national SWAB-ID guide (a), university (b) and general hospitals (c).
Table 3.
Distribution of the 20 most commonly searched therapy conditions
| Total (N = 1 394 850)a | National site (N = 359 489) | University hospitals (N = 304 613) | General hospitals (N = 730 748) | |||||
|---|---|---|---|---|---|---|---|---|
| Condition | n | % | n | % | n | % | n | % |
| Arthritis | 22 995 | 1.6 | 5850 | 1.6 | 4465 | 1.5 | 12 680 | 1.7 |
| Candida infection | 36 213 | 2.6 | 12 802 | 3.6 | 8165 | 2.7 | 15 246 | 2.1 |
| CAPb | 213 314 | 15.3 | 52 024 | 14.5 | 35 738 | 11.7 | 125 552 | 17.2 |
| Cellulitis | 61 842 | 4.4 | 17 850 | 5.0 | 10 353 | 3.4 | 33 639 | 4.6 |
| Cholangitis | 24 335 | 1.7 | 3990 | 1.1 | 5413 | 1.8 | 13 907 | 1.9 |
| Cholecystitis | 13 550 | 1.0 | 5015 | 1.4 | 1807 | 0.6 | 8642 | 1.2 |
| Cystitis | 188 193 | 13.5 | 45 724 | 12.7 | 25 592 | 8.4 | 116 877 | 16.0 |
| Diabetic foot | 14 546 | 1.0 | 3604 | 1.0 | 2301 | 0.8 | 8641 | 1.2 |
| Endocarditis | 31 608 | 2.3 | 4819 | 1.3 | 10 763 | 3.5 | 16 026 | 2.2 |
| Erysipelas | 44 938 | 3.2 | 13 070 | 3.6 | 6134 | 2.0 | 25 734 | 3.5 |
| Gastroenteritis | 41 898 | 3.0 | 14 459 | 4.0 | 7820 | 2.6 | 19 457 | 2.7 |
| Hospital-acquired pneumonia | 50 894 | 3.6 | 12 869 | 3.6 | 13 881 | 4.6 | 24 144 | 3.3 |
| Meningitis | 33 808 | 2.4 | 7530 | 2.1 | 13 311 | 4.4 | 12 967 | 1.8 |
| Osteomyelitis | 29 854 | 2.1 | 6831 | 1.9 | 7820 | 2.6 | 15 203 | 2.1 |
| Peritonitis | 25 051 | 1.8 | 4550 | 1.3 | 6918 | 2.3 | 13 583 | 1.9 |
| PID | 16 161 | 1.2 | 4396 | 1.2 | 2815 | 0.9 | 8950 | 1.2 |
| Prostatitis | 17 410 | 1.2 | 3229 | 0.9 | 5590 | 1.8 | 8591 | 1.2 |
| Pyelonephritis | 43 936 | 3.1 | 5387 | 1.5 | 8512 | 2.8 | 30 037 | 4.1 |
| Sepsisc | 157 588 | 11.3 | 31 898 | 8.9 | 42 872 | 14.1 | 82 818 | 11.3 |
| Urosepsis/UTI | 50 879 | 3.6 | 13 056 | 3.6 | 10 137 | 3.3 | 27 686 | 3.8 |
PID, pelvic inflammatory disease; UTI, urinary tract infection.
aOf the 1 394 850 pages in the ‘therapy’ rubric, 1169 could not be analysed as the condition search term was unclear. Only the 20 most commonly searched conditions are presented in the table.
bNumber (%) of searches of CAP where the pathogen was unknown: total, n = 135 929 (63.7%); national site, n = 26 307 (50.6%); university hospitals, n = 24 840 (69.5%); general hospitals, n = 84 782 (67.5%).
cDefinition based on any search term containing ‘sepsis’ or ‘bacteraemia’.
Figure 3.
Distribution of the five most commonly searched therapy conditions over time.
Searches related to prophylaxis
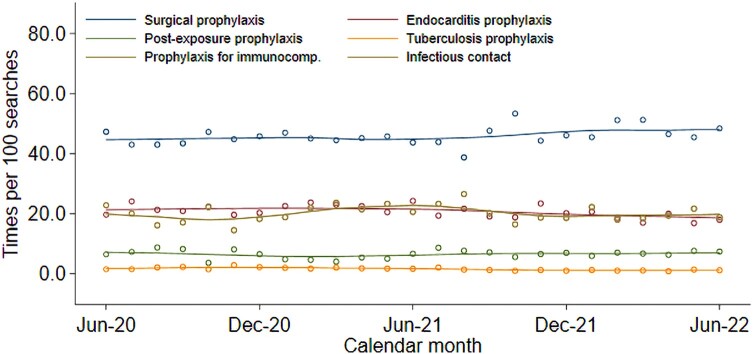
Table 4 shows the distribution of searches on prophylaxis for each of the six categories. The most commonly searched advice concerned surgical prophylaxis (n = 50 978 searches; 45.6%), endocarditis prophylaxis (n = 23 089 searches; 20.7%) and prophylaxis in immunocompromised hosts (n = 21 702 searches; 19.4%). For the national guide, endocarditis prophylaxis ranked first (n = 11 462 searches; 40.3%).
Table 4.
Distribution of searches on prophylaxis
| Total (N = 111 774)a | National site (N = 28 475) | University hospitals (N = 36 013) | General hospitals (N = 47 286) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Prophylaxis type | n | Unadj % | n | Unadj % | n | Unadj % | Adjb % | n | Unadj % | Adjb % |
| Surgical | 50 978 | 45.6 | 9981 | 35.1 | 14 924 | 41.4 | 50.0 | 26 073 | 55.1 | 51.0 |
| Endocarditis | 23 089 | 20.7 | 11 462 | 40.3 | 3866 | 10.7 | 10.0 | 7761 | 16.4 | 16.7 |
| Post-exposure | 7456 | 6.7 | 2019 | 7.1 | 1759 | 4.9 | 8.7 | 3678 | 7.8 | 8.5 |
| TB contact | 1882 | 1.7 | 843 | 3.0 | 252 | 0.7 | 1.0 | 787 | 1.7 | 2.4 |
| Immunocompromised | 21 702 | 19.4 | 2532 | 8.9 | 13 472 | 37.4 | 18.3 | 5698 | 12.1 | 10.9 |
| Close contact | 5709 | 5.1 | 1637 | 5.7 | 1037 | 2.9 | 8.3 | 3035 | 6.4 | 9.8 |
Adj, adjusted; unadj: unadjusted. Post-exposure refers to prophylaxis after drowning, animal bites, HIV/hepatitis exposure. Close contact refers to prophylaxis after close contact with invasive group A streptococci, invasive Haemophilus influenzae type B, whooping cough or meningococci cases.
aOnly the six most commonly used terms are presented and thus 958 web sessions were not included in the table.
bAdjusted for number of beds in healthcare institutions; applies to university and general hospitals.
Figure 4 shows the distribution of the searches over time. Figure S3 displays the search for these subtypes over time for the national SWAB-ID guide (a), university (b) and general hospitals (c). Over time the number of searches per month show only small fluctuations.
Figure 4.
Distribution of the searches on prophylaxis categories over time.
Searches related to medication
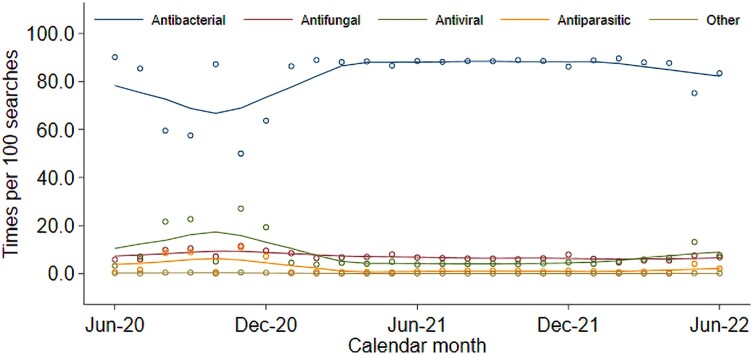
Table 5 displays the distribution of searches on medication for each of the five categories. The most commonly searched advices concerned antibacterials (n = 250 158 searches; 75.4%). The ranking across users were comparable (Table 5), also when adjusted for the number of beds in university and general hospitals.
Table 5.
Distribution of searches on medication, per category
| Total (N = 331 671) | National site (N = 68 890) | University hospitals (N = 88 759) | General hospitals (N = 174 022) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Medication type | n | % | n | Unadj % | n | Unadj % | Adja % | n | Unadj % | Adja % |
| Antibacterial | 250 158 | 75.4 | 55 409 | 80.4 | 69 452 | 78.2 | 62.9 | 125 297 | 72.0 | 64.8 |
| Antifungal | 26 745 | 8.1 | 4632 | 6.7 | 7974 | 9.0 | 10.2 | 14 139 | 8.1 | 8.7 |
| Antiviral | 40 254 | 12.1 | 6456 | 9.4 | 9079 | 10.2 | 19.8 | 24 719 | 14.2 | 17.4 |
| Antiparasitic | 13 850 | 4.2 | 2291 | 3.3 | 2151 | 2.4 | 6.9 | 9408 | 5.4 | 8.7 |
| Other | 664 | 0.2 | 102 | 0.1 | 103 | 0.1 | 0.3 | 459 | 0.3 | 0.4 |
aAdjusted for number of beds in healthcare institutes; only applies to university and general hospitals.
Figure 5 shows the distribution of the searches over time. Figure S4 displays the searches over time for the national SWAB-ID guide (a), university (b) and general hospitals (c).
Figure 5.
Distribution of the searches on medication categories over time.
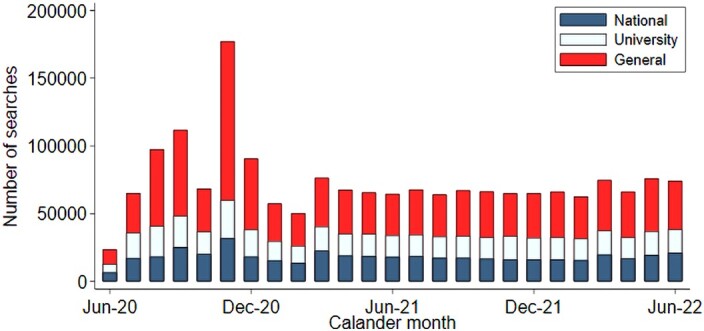
Table 6 displays the distribution of searches on medication for the 10 most searched drugs. Most common searched were amoxicillin/clavulanic acid (n = 20 996 searches; 6.3%), ciprofloxacin (n = 19 842 searches; 6.0%) and cefuroxime (n = 17 836 searches; 5.4%). The ranking across the three user groups differed slightly (Table 6). In general hospitals amoxicillin/clavulanic acid (6.2%), cefuroxime (6.2%) and ciprofloxacin (6.2%) were most often searched, while in university hospitals vancomycin (8.6%), meropenem (5.9%) and piperacillin/tazobactam (5.4%) were most often searched.
Table 6.
Distribution of searches on medication, per drug
| Total (N = 331 671) | National site (N = 68 890) | University hospitals (N = 88 759) | General hospitals (N = 174 022) | |||||
|---|---|---|---|---|---|---|---|---|
| Medication type | n | % | n | % | n | % | n | % |
| Amoxicillin | 10 426 | 3.1 | 2598 | 3.8 | 2512 | 2.8 | 5316 | 3.1 |
| Amoxicillin/clavulanic acid | 20 996 | 6.3 | 5496 | 8.0 | 4677 | 5.3 | 10 823 | 6.2 |
| Cefuroxime | 17 836 | 5.4 | 3376 | 4.9 | 365 | 4.1 | 10 810 | 6.2 |
| Ciprofloxacin | 19 842 | 6.0 | 4568 | 6.6 | 4577 | 5.2 | 10 697 | 6.2 |
| Clindamycin | 10 293 | 3.1 | 4742 | 6.9 | 1595 | 1.8 | 3956 | 2.3 |
| Flucloxacillin | 14 294 | 4.3 | 3631 | 5.3 | 3967 | 4.5 | 6696 | 3.9 |
| Meropenem | 13 393 | 4.0 | 2234 | 3.2 | 5214 | 5.9 | 5945 | 3.4 |
| Piperacillin/tazobactam | 10 763 | 3.3 | 1616 | 2.4 | 4745 | 5.4 | 4402 | 2.5 |
| Co-trimoxazole | 11 871 | 3.6 | 3122 | 4.5 | 3365 | 3.8 | 5384 | 3.1 |
| Vancomycin | 17 518 | 5.3 | 2462 | 3.6 | 7617 | 8.6 | 7439 | 4.3 |
Only the 10 most common searched drugs are given in the table.
Figure 6 shows the distribution of the searches on the eight most searched drugs over time. Figure S5 displays the search for these drugs over time for the national SWAB-ID guide (a), university (b) and general hospitals (c). Overall, an increase in searches on amoxicillin/clavulanic acid is seen around October 2020, which could be related to the increase in searches on lower respiratory tract (Figure 2) and CAP (Figure 3). In university hospitals vancomycin was consistently the most consulted medication type (Figure S5b).
Figure 6.
Distribution of the searches on specific drugs over time.
Discussion
In this study, we presented user data of the online national antimicrobial guide with customized local versions, as designed by SWAB. Included in the present study were 35 local versions of the guide that used SWAB-ID for at least 1 year prior to start of data collection, covering 53 of the 76 Dutch hospitals. At present (October 2023), 65/76 (86%) of Dutch hospitals are affiliated with SWAB-ID. Our current findings show that the online guides are frequently used. The total number of page views was stable over time but decreased during the weekends. More than half of the total number of searches were performed by users of the customized sites from general hospitals. We conclude that the online guides are an important source for Dutch physicians in prescribing therapy according to the guidelines.
Our study shows that the online antimicrobial guides are most often consulted for advice on therapy. The most commonly searched tracts among all user groups were the lower respiratory tract, kidney and urinary tract, and skin and soft tissues. The most commonly searched conditions were CAP, sepsis, cystitis and gastroenteritis. This seems to parallel everyday practice in the hospitals, as national Dutch data report that in 2019 approximately 30 000 patients were admitted with pneumonia, 24 500 with a urinary tract infection and 9500 with cellulitis/erysipelas.13 The increase of the number of guideline consultations for lower respiratory tract and CAP during the winter in 2020 could be related to the second COVID-19 wave.
The most commonly searched medication category was by far antibacterial, with the drugs amoxicillin/clavulanic acid, ciprofloxacin, cefuroxime and vancomycin as the four most common. These findings are largely in line with NethMap, the annual report on consumption of antimicrobial agents in the Netherlands, which provides DDD/100 patient-days and DDD/100 admissions in hospitalized patients: in 2021 amoxicillin/clavulanate, piperacillin/tazobactam, second- and third-generation cephalosporins and fluoroquinolones were the most used antibiotics in hospitals.14 Explanations for the discrepancies between most commonly searched medication and consumption could be that the current guidelines maintain a fixed dose of 2 g ceftriaxone. The simplicity of the dosage is easy to memorize and therefore probably needs less consulting of the guide by physicians. Dosing of vancomycin is more individualized, apparently requiring more frequent consultation.
NethMap further differentiates between university hospitals, large teaching hospitals and general hospitals. University hospitals have a higher use of vancomycin and carbapenems. The use of antibiotic classes within large teaching hospitals and general hospitals is comparable and higher for second-generation cephalosporins compared with university hospitals.14 These differences are reflected in the searches from the various types of hospitals.
The main strength of our study is that we analysed a large amount of data over an extended period of time, which allowed evaluation of possible seasonal effects. Second, our data covers the majority of Dutch hospital beds, as 53 of 76 (70%) general and university Dutch hospitals used local versions of SWAB-ID at the time of the study. To prevent any influence of the size of the hospital, we also adjusted percentages for the number of beds per institution. Finally, we are unaware of any other country with a similar online national antibiotic guide with locally customized versions. To our knowledge, no other studies have also been performed on the rate of guideline consultation. Taken together, these data provide unique insight into how often and which guidelines are used.
There are several limitations to our study. First, these data do not provide us with information regarding actual prescribing practices. Second, user data in NethMap are based on data from a selection of hospitals in the Netherlands that differs from the selection of hospitals affiliated with SWAB-ID. However, given the high percentage of hospitals in the Netherlands that are covered by the SWAB and by NethMap, these selections largely overlap. Third, we have no user characteristics. For example, the guide could be used more often by medical interns and residents at the start of their training compared with experienced attending physicians, as has been shown in other studies.15–17 Lastly, the fact that many pages on therapy, medication or prophylaxis are less often or hardly ever consulted does not make them superfluous, because we are unable to distinguish whether a low number of views reflects the frequency of such conditions in daily practice or that these pages are underutilized.
In conclusion, our study has identified frequent rates of consultation across a wide variety of guidelines on therapy, prophylaxis and medication. The benefits of prescribing therapy according to the guideline are clear; nevertheless, several studies have shown that there is much room for improvement regarding adherence to this stewardship objective.6,18–21 The fact that the customized, local versions were consulted in the majority suggests the value of an option to customize the national version to the local situation; however, it has to be acknowledged that the lack of difference in resistance rates across our country would be unlikely to justify local adaptations.14 The next logical step would be for healthcare institutions to incorporate guidelines into the local electronic medication prescribing system to function as a clinical decision-support tool. By offering a prescribing suggestion for a specific therapy indication based on locally endorsed, up-to-date and evidence-based information we can improve the quality of antibiotic prescribing.
Supplementary Material
Acknowledgements
Dr Roel Verkooijen was involved in the conception of this study. Regretfully he passed away on 10 May 2020.
Contributor Information
Emelie C Schuts, Department of Internal Medicine, Division of Infectious Diseases, Amsterdam UMC, University of Amsterdam, Meibergdreef 9, 1105 AZ Amsterdam, The Netherlands.
Anders Boyd, Department of Infectious Diseases, Public Health Service Amsterdam, Amsterdam, The Netherlands; Stichting HIV Monitoring, Amsterdam, The Netherlands.
Stephanie Natsch, Department of Pharmacy, Radboud University Medical Center, Nijmegen, The Netherlands.
Arjen Veenman, Integrated Disease Management Corporation (IDMC), Nijmegen, The Netherlands.
Jan M Prins, Department of Internal Medicine, Division of Infectious Diseases, Amsterdam UMC, University of Amsterdam, Meibergdreef 9, 1105 AZ Amsterdam, The Netherlands.
SWAB-ID Study Group:
Dr Hannelore I Bax, Drs Eefje de Jong, Dr Merel M C Lambregts, Dr Maurine A Leverstein-van Hall, Dr Paul D van der Linden, Dr Damian C Melles, Dr Stephanie Natsch, Drs Fre W Sebens, Dr Tom F Wolfs, and Prof Dr Jan M Prins
Members of the SWAB-ID Study Group (Editorial Board)
Dr Hannelore I. Bax, Drs Eefje de Jong, Dr Merel M. C. Lambregts, Dr Maurine A. Leverstein-van Hall, Dr Paul D. van der Linden, Dr Damian C. Melles, Dr Stephanie Natsch, Drs Fre W. Sebens, Dr Tom F. Wolfs, Prof. Dr Jan M. Prins (editor-in-chief).
Funding
Current study: none. SWAB is funded by the National Institute for Public Health and the Environment (RIVM-CIb), the Netherlands.
Transparency declarations
None to declare.
Supplementary data
Figures S1 to S5 and Table S1 are available as Supplementary data at JAC-AMR Online.
References
- 1. Behar P, Wagner MB, Freitas I et al. Assessing the antimicrobial prescription request process in a teaching hospital in Brazil: regulations and training. Braz J Infect Dis 2000; 4: 76–85. [PubMed] [Google Scholar]
- 2. Davey P, Marwick CA, Scott CL et al. Interventions to improve antibiotic prescribing practices for hospital inpatients. Cochrane Database Syst Rev 2017; issue 2: CD003543. 10.1002/14651858.CD003543.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dellit TH, Owens RC, McGowan JE Jr et al. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis 2007; 44: 159–77. 10.1086/510393 [DOI] [PubMed] [Google Scholar]
- 4. Barlam TF, Cosgrove SE, Abbo LM et al. Implementing an antibiotic stewardship program: guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis 2016; 62: e51–77. 10.1093/cid/ciw118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. van den Bosch CM, Geerlings SE, Natsch S, et al. Quality indicators to measure appropriate antibiotic use in hospitalized adults. Clin Infect Dis 2015; 60: 281–91. 10.1093/cid/ciu747 [DOI] [PubMed] [Google Scholar]
- 6. Schuts EC, Hulscher M, Mouton JW et al. Current evidence on hospital antimicrobial stewardship objectives: a systematic review and meta-analysis. Lancet Infect Dis 2016; 16: 847–56. 10.1016/S1473-3099(16)00065-7 [DOI] [PubMed] [Google Scholar]
- 7. Agwu AL, Lee CK, Jain SK et al. A world wide web-based antimicrobial stewardship program improves efficiency, communication, and user satisfaction and reduces cost in a tertiary care pediatric medical center. Clin Infect Dis 2008; 47: 747–53. 10.1086/591133 [DOI] [PubMed] [Google Scholar]
- 8. MacDougall C, Polk RE. Antimicrobial stewardship programs in health care systems. Clin Microbiol Rev 2005; 18: 638–56. 10.1128/CMR.18.4.638-656.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pagani L, Gyssens IC, Huttner B et al. Navigating the web in search of resources on antimicrobial stewardship in health care institutions. Clin Infect Dis 2009; 48: 626–32. 10.1086/596762 [DOI] [PubMed] [Google Scholar]
- 10. van Vonderen MG, Gyssens IC, Hartwig NG et al. Optimalisation of the antibiotic policy in The Netherlands. XI. The national electronic antibiotic guide ‘SWAB-ID’ for use in hospitals. Ned Tijdschr Geneeskd 2006; 150: 2560–4. [PubMed] [Google Scholar]
- 11. Schuts EC, van den Bosch CM, Gyssens IC et al. Adoption of a national antimicrobial guide (SWAB-ID) in The Netherlands. Eur J Clin Pharmacol 2016; 72: 249–52. 10.1007/s00228-015-1969-x [DOI] [PubMed] [Google Scholar]
- 12. Data Protection Authority, Ministry of Health, Welfare and Sport . Right to privacy in a digital world. https://autoriteitpersoonsgegevens.nl/en.
- 13. CBS, Statline. Ziekenhuisopnamen en -Patiënten; Diagnose-indeling ICD-10 (3-teken niveau). 2019. https://opendata.cbs.nl/#/CBS/nl/dataset/84069NED/table? ts=1660057504243.
- 14. NethMap. Consumption of Antimicrobial Agents and Antimicrobial Resistance Among Medically Important Bacteria in the Netherlands in 2021/MARAN 2022. Monitoring of Antimicrobial Resistance and Antibiotic Usage in Animals in the Netherlands in 2021. 2022. https://www.rivm.nl/publicaties/nethmap-2022-consumption-of-antimicrobial-agents.
- 15. Skodvin B, Aase K, Charani E et al. An antimicrobial stewardship program initiative: a qualitative study on prescribing practices among hospital doctors. Antimicrob Resist Infect Control 2015; 4: 24. 10.1186/s13756-015-0065-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Barlow G, Nathwani D, Myers E et al. Identifying barriers to the rapid administration of appropriate antibiotics in community-acquired pneumonia. J Antimicrob Chemother 2008; 61: 442–51. 10.1093/jac/dkm462 [DOI] [PubMed] [Google Scholar]
- 17. Mol PG, Rutten WJ, Gans RO et al. Adherence barriers to antimicrobial treatment guidelines in teaching hospital, The Netherlands. Emerg Infect Dis 2004; 10: 522–5. 10.3201/eid1003.030292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Arnold FW, LaJoie AS, Brock GN et al. Improving outcomes in elderly patients with community-acquired pneumonia by adhering to national guidelines: Community-Acquired Pneumonia Organization International cohort study results. Arch Intern Med 2009; 169: 1515–24. 10.1001/archinternmed.2009.265 [DOI] [PubMed] [Google Scholar]
- 19. Wathne JS, Harthug S, Kleppe LKS et al. The association between adherence to national antibiotic guidelines and mortality, readmission and length of stay in hospital inpatients: results from a Norwegian multicentre, observational cohort study. Antimicrob Resist Infect Control 2019; 8: 63. 10.1186/s13756-019-0515-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Spoorenberg V, Hulscher ME, Akkermans RP et al. Appropriate antibiotic use for patients with urinary tract infections reduces length of hospital stay. Clin Infect Dis 2014; 58: 164–9. 10.1093/cid/cit688 [DOI] [PubMed] [Google Scholar]
- 21. Huijts SM, van Werkhoven CH, Boersma WG et al. Guideline adherence for empirical treatment of pneumonia and patient outcome. Treating pneumonia in The Netherlands. Neth J Med 2013; 71: 502–7. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.