Abstract
Background
Concerns about increased suicidal attempts, especially by self-poisoning as a consequence of Coronavirus disease 2019 (COVID-19) pandemic have been raised worldwide.
Aim of the study
This study aimed to evaluate the rate and pattern of suicide attempts and deaths by self-poisoning among patients admitted to Tanta University Poisoning Control Center one year before and following COVID-19 pandemic declaration in Egypt. It was conducted on the medical records of 3,200 poisoned patients, from March 2019 to February 2021. Demographic, toxicological data and patients’ outcomes were collected.
Results
During the pandemic year, 63.8% of total admitted patients alleged suicidal self-poisoning. Adults significantly decreased from 59% to 52.3%, while adolescents significantly increased from 34.6% to 41.7%. Monthly numbers of admitted suicidal self-poisoned patients significantly decreased during the lockdown but significantly increased from 7% to 26.5%, during the peak of the second wave of the pandemic as well as suicidal deaths (increased from 1.9% to 21.2%). Suicidal self-poisoning in females increased late in the pandemic year and suicidal self-poisoning deaths were significantly reported from rural areas (P = 0.025). The delay time was significantly longer, length of hospital stay was significantly shorter, intensive care unit admission rates and suicidal deaths were significantly increased during the pandemic year (P < 0.001, 0.026, <0.001, <0.001, respectively). Phosphides were the most commonly used poison for committing suicide and suicidal deaths during this year.
Conclusion
Psychological support should be directed to females and adolescents, especially from rural areas in Egypt to help reduce suicidal attempts and deaths by self-poisoning during any future pandemics and lockdowns.
Keywords: suicidal self-poisoning, COVID-19, lockdown, intensive care unit admission, pesticides, poison control center
Introduction
The Coronavirus disease 2019 (COVID-19) outbreak was recognized as a pandemic by World Health Organization (WHO; Geneva, Switzerland) in March 2020, with widespread lockdown regulations worldwide to prevent disease progression.1 In Egypt, the appearance of the first COVID-19 case was announced on February 14, 2020, forcing the Egyptian government to implement a partial lockdown on March 19, 2020.2,3
These lockdown regulations have resulted in social isolation, economic uncertainty, and increased rates of psychiatric disturbances, ranging from mild anxiety to severe depression with suicidal attempts, in different populations worldwide.4,5 Moreover, a previous study in the United States documented a significant association between stress exposure and anxiety disorders resulting from personal isolation and panic fear from COVID-19 infection and suicidal attempts during the pandemic period.6 Furthermore, some studies documented increased rates of suicide attempts from the start of the pandemic.7,8 Other studies showed increased rates of suicide attempts by the end of the first year of the pandemic or during the second wave.9,10 While, data on deaths by suicide during the lockdown are deficient, possibly due to insufficient studies or too small samples included.11
Although there are many ways to commit suicide, self-poisoning is still one of the most common methods for committing suicide due to its ease of achievement and low suffering.12 In the United States, suicidal self-poisoning is considered the most commonly used way of attempting suicide among youths,13 while in the United Kingdom, it represents approximately 25% of total suicides.14 This problem is worsening with a steady increase in suicide deaths by self-poisoning in developing countries.15 In Egypt, there are a large number of patients admitted to different poison control centers due to suicidal self-poisoning.16,17 The number of these patients is underestimated regarding the actual risk of suicide due to denial or fear of stigma in Egyptian society. Although these patients are likely to be managed and discharged, the main problem remains neglected, and no actual solutions are taken to prevent the risk of future suicide attempts.18
Based on the behavioral changes during the COVID-19 pandemic, it was noted that there were dramatic increases in the rate of acute suicidal poisoned cases admitted to various poison centers worldwide.19–21 Early in the pandemic, all medical attention was focused on treating individuals with COVID-19 and preventing the spread of the disease in the general population. Less attention was paid to the psychiatric consequences of the COVID-19 crisis.8 However, the WHO tried to provide an outline to support patients and the public with the assistance of mental health professionals and psychiatrists against the possible effects of the pandemic on mental health and suicide.4
The effect of the COVID-19 pandemic is still going on. Despite the release of strict measures and regulations, the economic status of different populations worldwide is still affected. People are still living in fear of new strains emerging with possible disease waves hitting the world again. Therefore, research on the relationship between the COVID-19 pandemic and suicidal acts can help the healthcare systems to adapt rapidly to any future threats.11 Additionally, more studies on long-term trends in suicides and the relevant socioeconomic factors during the COVID-19 pandemic are warranted.22 Moreover, studying the effect of the COVID-19 pandemic on the incidence of suicidal self-poisoning over extended periods in Egypt is still limited and less objective.23 Hence, this study aimed to evaluate the rate and pattern of suicide attempts and deaths by self-poisoning among patients admitted to Tanta University Poisoning Control Center (TUPCC), Tanta University Hospitals, Egypt, one year before and one year following the COVID-19 pandemic declaration in Egypt.
Patients and methods
Study design and setting
This cross-sectional comparative study was conducted on alleged suicidal self-poisoned patients admitted to TUPCC, Egypt, from the start of March 2019 to the end of February 2021. (One year before and one year following the declaration of the COVID-19 pandemic in Egypt). This Egyptian poison center is the only center serving the region of the Gharbia governate that represented an extent of 1,912 Km2 with a high population density of 2,668/km.2 Moreover, TUPCC provides its medical services to the neighboring governates in and around the Delta region that lack poison center facilities. The Delta region is one of the most densely populated places in Egypt.24
Patients and sampling
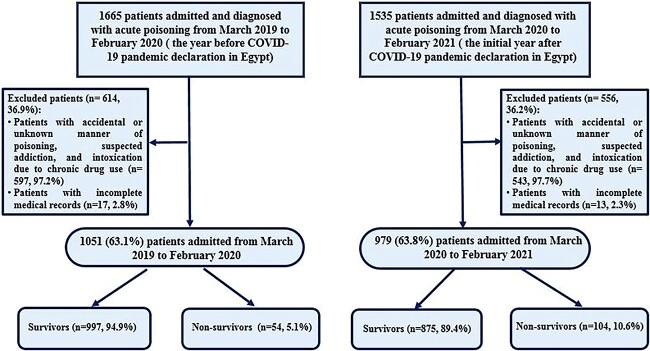
A total of 3,200 Egyptian acutely poisoned patients who were admitted to TUPCC during the study period, were recruited. Among them 2030 were diagnosed with acute suicidal self-poisoning and were included in the study analysis. To evaluate the rate and pattern of suicide attempts and deaths by self-poisoning among patients admitted to TUPCC during the COVID-19 pandemic, the current study included the medical records of 1,051 suicidal poisoned cases admitted to TUPCC in the year preceding the COVID-19 pandemic declaration in Egypt (from the beginning of March 2019 till the end of February 2020), representing 63.1% of all poisoning cases admitted this year. These data were compared to the data of 979 cases who were admitted due to suicidal self-poisoning in the year following the COVID-19 pandemic declaration (from the beginning of March 2020 till the end of February 2021), representing 63.8% of all admitted cases in this period. Furthermore, this study compared the data of 54 suicidal self-poisoning deaths, representing 5.1% of all suicidal self-poisoned patients admitted in the year before the pandemic declaration with the data of 104 suicidal self-poisoning deaths, representing 10.6% of all suicidal self-poisoned patients admitted in the year following the pandemic declaration as illustrated in Fig. 1.
Fig. 1.
Flowchart of eligibility criteria of patients who were admitted to Tanta University Poison Control Center (TUPCC) and included in this study.
Inclusion and exclusion criteria
The medical records of all patients presented with acute suicidal self-poisoning during the study period were included. Diagnosis of poisoning in TUPCC is established according to the International Classification of Diseases and is confirmed by the clinical manifestations and laboratory investigations. All confirmed, diagnosed cases were documented in the database. Diagnosis of suicidal self-poisoning is based on the history taken from patients or their attendants in the case of mentally disabled patients. In addition, suicidal self-poisoning could be easily detected as some patients in the database had been reported for previous suicide attempts. Other rare cases bear signs of previous suicide attempts by other methods, such as cutting wrists. The type of poison is identified by referring to the report of the patients or their attendants. Some cases bring the container of toxin so could be detected easily.
The causative agents were categorized as aluminum and zinc phosphides, organophosphorus compounds, carbamates, pyrethroids, corrosives, hydrocarbons, alcohols, Central Nervous System (CNS) depressants, antipsychotics, antidepressants, anticonvulsants, cardiovascular drugs, anti-diabetic drugs, paracetamol and xanthine derivatives.
Exclusion criteria included patients exposed to accidental or unknown manner of poisoning, suspected addiction, and intoxication due to chronic drug use, as well as those with missed data affecting the study.
Data collection tools
Demographic data including age, gender, and residence (i.e. urban or rural) and toxicological data including type of the taken poison, whether it is single or multiple ingestion, and the delay time (elapsed time from intake to hospital admission) were collected from the admission file records. The patients were classified according to their age as follows: children seven to 14 years; adolescents >14–19 years; adults >19–60 years; and older adults aged over 60 years.
The length of the hospital stay, the need for Intensive Care Unit (ICU) admission and /or mortality were also recorded and analyzed as the patients’ outcomes. Suicidal self-poisoning death was considered the primary outcome of the study while the need for ICU admission and the length of the hospital stay were the secondary outcomes. Based on TUPCC protocols and guidelines, the decision of the need for ICU admission is taken for patients suffering from one or more of the following: presentation with intractable seizures not responding to the usual antiepileptics, significant respiratory embarrassment and need for high flow O2, and mechanical ventilation, need for vasopressors for hemodynamic instability, and renal replacement therapy.25
Compliance with ethical standards
The current study was started after being approved by the Research Ethical Committee of Tanta Faculty of Medicine (Approval code 35856/9/22). Data were retrieved from the admission records without a declaration of participant identity. All data were handled namelessly to maintain the confidentiality of the data. The requirement for informed consent have been waived.
Power of the study
The power of the current study was 99.7% for suicidal deaths among suicidal self-poisoned patients during the study period by using post hoc power calculation by G-power program version 3.1.9.4. Based on the difference between two independent proportions (suicidal self-poisoning death rate in the year before and the year following the COVID-19 pandemic declaration in Egypt, 5.1% and 10.6% respectively) at a sample size of (1,051 and 979 respectively) and a type one error threshold (α) < 0.05.
Statistical analysis
Statistical analysis was conducted by the Statistical Package for Social Sciences (IBM SPSS Statistics) version, version 26 for Windows (IBM Corp., Armonk, N.Y., USA). Categorical variables were introduced using counts and percentages. Continuous numerical variables not following the normal distribution were presented as the median and interquartile range (IQR; expressed as the 25th—75th percentiles). Regarding numerical variables having normal distribution, they were introduced using mean and standard deviation (SD). Pearson’s Chi-square test and Fisher’s exact test were used to test the associations between categorical variables. Testing the association between a categorical and an ordinal variable was done using the Chi-square test for trend (linear-by-linear association). Comparisons of numerical variables between the groups were done using either the Mann-Whitney test (abnormally distributed variables) or the independent samples T-test (normally distributed variables). The significance level was adopted at a P-value <0.05 to interpret the results of tests.26
Results
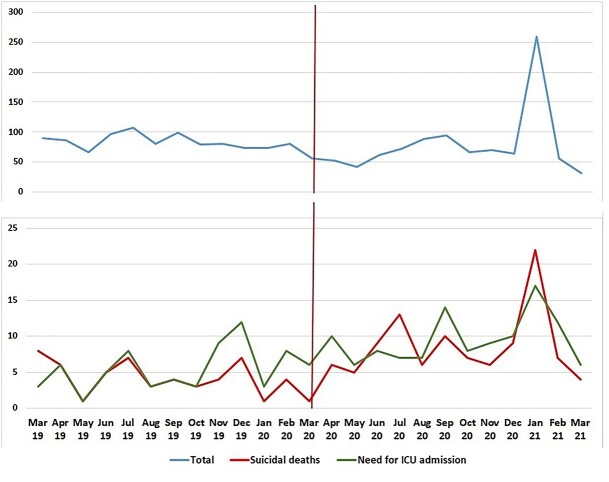
The monthly numbers of admitted suicidal self-poisoned patients showed that there was a significant decrease in the numbers of admitted patients during the initial five months after the pandemic declaration (the lockdown period) but the number of admitted patients significantly increased during January 2021 (peak of the second wave of the pandemic in Egypt) (increased from 7% to 26.5%, P < 0.001) (Table 1).
Table 1.
Monthly numbers of admitted suicidal self-poisoned patients one year before and one year following the COVID-19 pandemic declaration in March 2020.
| Admission month | 2019–2020 (n = 1,051) | 2020–2021 (n = 979) | Test statistic | P-value |
|---|---|---|---|---|
| March | 126 (12%) | 52 (5.3%) | X2ChS = 28.248 | <0.001* |
| April | 86 (8.2%) | 52 (5.3%) | X2ChS = 6.595 | 0.010* |
| May | 66 (6.3%) | 42 (4.3%) | X2ChS = 3.983 | 0.046* |
| June | 97 (9.2%) | 62 (6.3%) | X2ChS = 5.890 | 0.015* |
| July | 107 (10.2%) | 72 (7.4%) | X2ChS = 5.036 | 0.025* |
| August | 81 (7.7%) | 89 (9.1%) | X2ChS = 1.265 | 0.261 |
| September | 99 (9.4%) | 94 (9.6%) | X2ChS = 0.020 | 0.889 |
| October | 79 (7.5%) | 67 (6.8%) | X2ChS = 0.344 | 0.558 |
| November | 81 (7.7%) | 70 (7.2%) | X2ChS = 0.228 | 0.633 |
| December | 74 (7%) | 64 (6.5%) | X2ChS = 0.203 | 0.652 |
| January | 74 (7%) | 259 (26.5%) | X2ChS = 139.320 | <0.001* |
| February | 81 (7.7%) | 56 (5.7%) | X2ChS = 3.179 | 0.075 |
n: Number; X2ChS: Pearson’s Chi-square test for independence of observations.
*significant at P < 0.05.
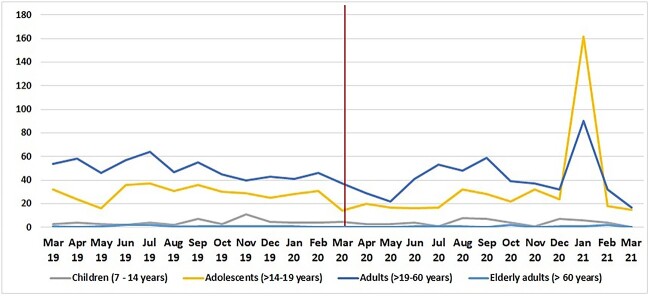
As illustrated in Table 2 and Figs 2–4, the medians of age of suicidal self-poisoned patients in the year before and following the declaration of the pandemic were 21 and 20 years respectively, with significant difference between both years (P = 0.034). In addition, there was significant lower rates of suicidal self-poisoning among adults and significant higher rates among adolescents during the pandemic year (P = 0.010). Regarding gender and residence, there were no statistical differences between both years of the study. Using a single drug or poison for suicidal self-poisoning was the most prevalent before and during the pandemic, with no significant difference. The delay time was significantly longer during the pandemic year than before the pandemic (3 versus 2 h, respectively). The need for ICU admission and suicidal self-poisoning deaths were significantly increased while, the length of hospital stay was significantly shorter during the same period.
Table 2.
Demographic and toxicological data of suicidal self-poisoned patients admitted one year before and one year following the COVID-19 pandemic declaration in March 2020.
| Variables | 2019–2020 (n = 1,051) | 2020–2021 (n = 979) | Test statistic | P-value | |
|---|---|---|---|---|---|
| Age (years) | Median [IQR] | 21 [17–29] | 20 [18–27] | Z = 2.117 | 0.034* |
| Min - Max | 7–76 | 7–75 | |||
| Age groups | Children (7–14 years) | 55 (5.2%) | 50 (5.1%) | XL = 6.671 | 0.010* |
| Adolescents (>14–19 years) | 364 (34.6%) | 408 (41.7%) | |||
| Adults (>19–60 years) | 620 (59%) | 512 (52.3%) | |||
| Elderly (>60 years) | 12 (1.1%) | 9 (0.9%) | |||
| Gender | Male | 342 (32.5%) | 319 (32.6%) | X2ChS = 0.000 | 0.983 |
| Female | 709 (67.5%) | 660 (67.4%) | |||
| Residence | Urban | 467 (44.4%) | 408 (41.7%) | X2ChS = 1.573 | 0.210 |
| Rural | 584 (55.6%) | 571 (58.3%) | |||
| Number of poisons | Single ingestion | 995 (94.7%) | 923 (94.3%) | X2ChS = 0.149 | 0.699 |
| Multiple ingestion | 56 (5.3%) | 56 (5.7%) | |||
| Delay time (hours) | Median [IQR] | 2 [1–4] | 3 [1.5–6] | Z = 6.783 | <0.001* |
| Min – Max | 0.25–72 | 0.11–168 | |||
| Need for ICU admission | No | 984 (93.6%) | 861 (87.9%) | X2ChS = 19.731 | <0.001* |
| Yes | 67 (6.4%) | 118 (12.1%) | |||
| Suicidal deaths | Survivors | 997 (94.9%) | 875 (89.4%) | X2ChS = 21.247 | <0.001* |
| Non-survivors | 54 (5.1%) | 104 (10.6%) | |||
| Length of hospital stay | <24 h | 893 (85%) | 860 (87.8%) | XL = 4.931 | 0.026* |
| 24–48 h | 104 (9.9%) | 87 (8.9%) | |||
| >48 h | 54 (5.1%) | 32 (3.3%) | |||
n: Number; IQR: interquartile range; Min: minimum; Max: maximum; h: hours; X2ChS: Pearson’s Chi-square test for independence of observations; Z: Mann–Whitney test; XL: Chi-square test for linear-by-linear association (Cochran-Armitage test for trend).
*significant at P < 0.05.
Fig. 2.
Number of suicidal self-poisoned patients admitted to TUPCC from the beginning of March 2019 to the end of February 2021 differentiated by age groups.
Fig. 4.
Number of total suicidal self-poisoned patients, suicidal self-poisoned deaths and patients need for ICU admission admitted to TUPCC from the beginning of March 2019 to the end of February 2021.
Table 3 shows that aluminum and zinc phosphides were the most prevalent poisons used for suicidal self-poisoning in both years, with a significant increase during the pandemic (from 36.1% to 46.7%, P < 0.001). Using alcohol, organophosphorus compounds, carbamates and anticonvulsants for suicidal self-poisoning was significantly lower during the year following the COVID-19 pandemic declaration.
Table 3.
Types of single ingestion poisons used by suicidal self-poisoned patients admitted one year before and one year following the COVID-19 pandemic declaration in March 2020.
| Type of poison | 2019–2020 (n = 995) | 2020–2021 (n = 923) | Test statistic | P-value |
|---|---|---|---|---|
| Household and pesticide poisons: | ||||
| • Aluminum and zinc phosphides | 359 (36.1%) | 431 (46.7%) | X2ChS = 22.274 | <0.001* |
| • Organophosphorus compounds | 79 (7.9%) | 45 (4.8%) | X2ChS = 7.445 | 0.006* |
| • Carbamates | 64 (6.4%) | 35 (3.8%) | X2ChS = 6.827 | 0.009* |
| • Pyrethroids | 7 (0.7%) | 5 (0.5%) | X2ChS = 0.202 | 0.653 |
| • Hydrocarbons | 1 (0.1%) | 1 (0.1%) | FE | 1.000 |
| • Corrosives | 11 (1.1%) | 13 (1.4%) | X2ChS = 0.354 | 0.552 |
| CNS depressant drugs: | ||||
| • Opiates | 12 (1.2%) | 9 (1.0%) | X2ChS = 0.237 | 0.627 |
| • Benzodiazepines | 31 (3.1%) | 22 (2.4%) | X2ChS = 0.958 | 0.328 |
| • Antipsychotics | 81 (8.1%) | 85 (9.2%) | X2ChS = 0.687 | 0.407 |
| • Antidepressants | 55 (5.5%) | 46 (5%) | X2ChS = 0.286 | 0.593 |
| • Anticonvulsants | 47 (4.7%) | 25 (2.7%) | X2ChS = 5.388 | 0.020* |
| Alcohols | 13 (1.3%) | 3 (0.3%) | X2ChS = 5.569 | 0.018* |
| Cardiovascular drugs | 52 (5.2%) | 48 (5.2%) | X2ChS = 0.001 | 0.978 |
| Xanthine derivatives | 49 (4.9%) | 39 (4.2%) | X2ChS = 0.537 | 0.463 |
| Anti-diabetic drugs | 34 (3.4%) | 26 (2.8%) | X2ChS = 0.571 | 0.450 |
| Paracetamol | 31 (3.1%) | 35 (3.8%) | X2ChS = 0.657 | 0.418 |
n: Number; FE: Fisher’s exact test; X2ChS: Pearson’s Chi-square test for independence of observations.
*significant at P < 0.05.
Table 4 clarifies that the year after the declaration of the pandemic showed significantly high rates of exposure to aluminum and zinc phosphides, reaching 50.1% from 39.1% and 44.2% from 34.5% in adolescents and adults age groups, respectively (P < 0.05). On the other hand, during this year, exposure to organophosphorus compounds was significantly decreased in adolescents, reaching 3.9% from 7.5%, and exposure to carbamates was significantly decreased in adults reaching 4.3% from 7.4% (P < 0.05).
Table 4.
Types of single ingestion poisons used by suicidal self-poisoned patients admitted one year before and one year following the COVID-19 pandemic declaration in March 2020 according to the age groups.
| Type of poison | Children (7–14 years) | Adolescents (>14–19 years) | Adults (>19–60 years) | Elderly adults (>60 years) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2019–2020 (n = 52) |
2020–2021 (n = 49) |
P-value | 2019–2020 (n = 348) |
2020–2021 (n = 381) |
P-value | 2019–2020 (n = 583) |
2020–2021 (n = 484) |
P-value | 2019–2020 (n = 12) |
2020–2021 (n = 9) |
P-value | |
| Household and pesticide poisons: | ||||||||||||
| • AlP and ZnP | 17 (32.7%) | 22 (44.9%) | 0.208 X2 | 136 (39.1%) | 191 (50.1%) | 0.003*X2 | 201 (34.5%) | 214 (44.2%) | 0.001* X2 | 5 (41.7%) | 4 (44.4%) | 1.000 FE |
| • OPCs | 3 (5.8%) | 3 (6.1%) | 1.000 FE | 26 (7.5%) | 15 (3.9%) | 0.039*X2 | 48 (8.2%) | 27 (5.6%) | 0.091 X2 | 2 (16.7%) | 0 (0%) | 0.486 FE |
| • Carbamates | 5 (9.6%) | 1 (2%) | 0.206 FE | 15 (4.3%) | 12 (3.1%) | 0.407 X2 | 43 (7.4%) | 21 (4.3%) | 0.038* X2 | 1 (8.3%) | 1 (11.1%) | 1.000 FE |
| • Pyrethroids | 1 (1.9%) | 0 (0%) | 1.000 FE | 3 (0.9%) | 3 (0.8%) | 1.000 FE | 3 (0.5%) | 2 (0.4%) | 1.000 FE | 0 (0%) | 0 (0%) | NA |
| • Hydrocarbons | 1 (1.9%) | 1 (2%) | 1.000 FE | 0 (0%) | 0 (0%) | NA | 0 (0%) | 0 (0%) | NA | 0 (0%) | 0 (0%) | NA |
| • Corrosives | 0 (0%) | 2 (4.1%) | 0.233 FE | 4 (1.1%) | 6 (1.6%) | 0.755 FE | 5 (0.9%) | 5 (1%) | 0.762 FE | 2 (16.7%) | 0 (0%) | 0.486 FE |
| CNS depressant drugs: | ||||||||||||
| • Opiates | 1 (1.9%) | 0 (0%) | 1.000 FE | 1 (0.3%) | 0 (0%) | 0.477 FE | 10 (1.7%) | 9 (1.9%) | 0.859 X2 | 0 (0%) | 0 (0%) | NA |
| • Benzodiazepines | 0 (0%) | 0 (0%) | NA | 11 (3.2%) | 6 (1.6%) | 0.156 X2 | 20 (3.4%) | 15 (3.1%) | 0.762 X2 | 0 (0%) | 1 (11.1%) | 0.429 FE |
| • Antipsychotics | 2 (3.8%) | 5 (10.2%) | 0.260 FE | 22 (6.3%) | 29 (7.6%) | 0.495 X2 | 57 (9.8%) | 50 (10.3%) | 0.764 X2 | 0 (0%) | 1 (11.1%) | 0.429 FE |
| • Antidepressants | 4 (7.7%) | 1 (2%) | 0.363 FE | 21 (6%) | 13 (3.4%) | 0.094 X2 | 30 (5.1%) | 32 (6.6%) | 0.308 X2 | 0 (0%) | 0 (0%) | NA |
| • Anticonvulsants | 4 (7.7%) | 3 (6.1%) | 1.000 FE | 14 (4%) | 9 (2.4%) | 0.200 X2 | 29 (5%) | 13 (2.7%) | 0.056 X2 | 0 (0%) | 0 (0%) | NA |
| Alcohols | 0 (0%) | 0 (0%) | NA | 3 (0.9%) | 0 (0%) | 0.108 FE | 10 (1.7%) | 3 (0.6%) | 0.105 X2 | 0 (0%) | 0 (0%) | NA |
| Cardiovascular drugs | 2 (3.8%) | 2 (4.1%) | 1.000 FE | 19 (5.5%) | 30 (7.9%) | 0.193 X2 | 30 (5.1%) | 16 (3.3%) | 0.141 X2 | 1 (8.3%) | 0 (0%) | 1.000 FE |
| Xanthine derivatives | 1 (1.9%) | 1 (2%) | 1.000 FE | 28 (8%) | 20 (5.2%) | 0.128 X2 | 20 (3.4%) | 18 (3.7%) | 0.800 X2 | 0 (0%) | 0 (0%) | NA |
| Anti-diabetic drugs | 1 (1.9%) | 2 (4.1%) | 0.610 FE | 13 (3.7%) | 8 (2.1%) | 0.187 X2 | 20 (3.4%) | 15 (3.1%) | 0.762 X2 | 0 (0%) | 1 (11.1%) | 0.429 FE |
| Paracetamol | 2 (3.8%) | 3 (6.1%) | 0.672 FE | 12 (3.4%) | 13 (3.4%) | 0.979 X2 | 17 (2.9%) | 19 (3.9%) | 0.363 X2 | 0 (0%) | 0 (0%) | NA |
AlP and ZnP: Aluminum and zinc phosphides; OPCs: Organophosphorus compounds; FE: Fisher’s exact test; NA: non-applicable; X2: Pearson’s Chi-square test for independence of observations.
*significant difference (P < 0.05) for Chi-square/FE test comparing the poison frequency in the two periods within the age group.
Table 5 demonstrates that the year after the declaration of the pandemic showed significantly high exposure rates to aluminum and zinc phosphides, reaching 53.3% from 40.1% and 43.5% from 34.1% in male and female patients, respectively (P < 0.001). On the other hand, exposure to carbamates, anticonvulsants and alcohols was significantly low in this year (reaching 4.3% from 10.7%, 3% from 6.4% and 1% from 3.7%, respectively, P < 0.05) in male patients. While in female patients, the exposure to organophosphorus compounds significantly decreased from 6.4% reaching 3.2% in the pandemic year (P < 0.05).
Table 5.
Types of single ingestion poisons used by suicidal self-poisoned patients admitted one year before and one year following the COVID-19 pandemic declaration in March 2020 according to the gender.
| Type of poison | Male | Female | ||||
|---|---|---|---|---|---|---|
| 2019–2020 (n = 327) | 2020–2021 (n = 304) | P-value | 2019–2020 (n = 668) |
2020–2021 (n = 619) | P-value | |
| Household and pesticide poisons: | ||||||
| • Aluminum and zinc phosphides | 131 (40.1%) | 162 (53.3%) | <0.001* X2 | 228 (34.1%) | 269 (43.5%) | <0.001* X2 |
| • Organophosphorus compounds | 36 (11%) | 25 (8.2%) | 0.237 X2 | 43 (6.4%) | 20 (3.2%) | 0.008* X2 |
| • Carbamates | 35 (10.7%) | 13 (4.3%) | 0.002* X2 | 29 (4.3%) | 22 (3.6%) | 0.470 X2 |
| • Pyrethroids | 3 (0.9%) | 1 (0.3%) | 0.625 FE | 4 (0.6%) | 4 (0.6%) | 1.000 FE |
| • Hydrocarbons | 0 (0%) | 0 (0%) | NA | 1 (0.1%) | 1 (0.2%) | 1.000 FE |
| • Corrosives | 3 (0.9%) | 3 (1%) | 1.000 FE | 8 (1.2%) | 10 (1.6%) | 0.524 X2 |
| CNS depressant drugs: | ||||||
| • Opiates | 10 (3.1%) | 9 (3%) | 0.943 X2 | 2 (0.3%) | 0 (0%) | 0.500 FE |
| • Benzodiazepines | 3 (0.9%) | 7 (2.3%) | 0.209 FE | 28 (4.2%) | 15 (2.4%) | 0.078 X2 |
| • Antipsychotics | 31 (9.5%) | 33 (10.9%) | 0.568 X2 | 50 (7.5%) | 52 (8.4%) | 0.543 X2 |
| • Antidepressants | 5 (1.5%) | 8 (2.6%) | 0.330 X2 | 50 (7.5%) | 38 (6.1%) | 0.339 X2 |
| • Anticonvulsants | 21 (6.4%) | 9 (3%) | 0.041* X2 | 26 (3.9%) | 16 (2.6%) | 0.187 X2 |
| Alcohols | 12 (3.7%) | 3 (1%) | 0.027* X2 | 1 (0.1%) | 0 (0%) | 1.000 FE |
| Cardiovascular drugs | 7 (2.1%) | 4 (1.3%) | 0.429 X2 | 45 (6.7%) | 44 (7.1%) | 0.793 X2 |
| Xanthine derivatives | 6 (1.8%) | 3 (1%) | 0.507 FE | 43 (6.4%) | 36 (5.8%) | 0.643 X2 |
| Anti-diabetic drugs | 1 (0.3%) | 2 (0.7%) | 0.611 FE | 33 (4.9%) | 24 (3.9%) | 0.354 X2 |
| Paracetamol | 4 (1.2%) | 1 (0.3%) | 0.375 FE | 27 (4%) | 34 (5.5%) | 0.221 X2 |
FE: Fisher’s exact test; NA: non-applicable; X2: Pearson’s Chi-square test for independence of observations.
*significant difference (P < 0.05) for Chi-square/FE test comparing the poison frequency in the two periods within the sex group.
The monthly numbers of deaths due to suicidal self-poisoning showed that there was a significant decrease in the numbers of deaths during March 2020 (the first month of the pandemic) (reaching 3.8% from 16.7%, P = 0.011) while there were no significant differences in the following months of lockdown. On the other hand, there was a dramatic significant increase in the incidence of deaths due to suicidal self-poisoning during January 2021 (the peak of the second wave of the pandemic in Egypt) (increased from 1.9% to 21.2%, P = 0.001) (Table 6).
Table 6.
Monthly numbers of suicidal self-poisoned deaths one year before and one year following the COVID-19 pandemic declaration in March 2020.
| Admission month | 2019–2020 (n = 54) | 2020–2021 (n = 104) | Test statistic | P-value |
|---|---|---|---|---|
| March | 9 (16.7%) | 4 (3.8%) | FE | 0.011* |
| April | 6 (11.1%) | 6 (5.8%) | FE | 0.342 |
| May | 1 (1.9%) | 5 (4.8%) | FE | 0.665 |
| June | 5 (9.3%) | 9 (8.7%) | FE | 1.000 |
| July | 7 (13%) | 13 (12.5%) | X2ChS = 0.007 | 0.934 |
| August | 3 (5.6%) | 6 (5.8%) | FE | 1.000 |
| September | 4 (7.4%) | 10 (9.6%) | FE | 0.773 |
| October | 3 (5.6%) | 7 (6.7%) | FE | 1.000 |
| November | 4 (7.4%) | 6 (5.8%) | FE | 0.736 |
| December | 7 (13%) | 9 (8.7%) | X2ChS = 0.725 | 0.394 |
| January | 1 (1.9%) | 22 (21.2%) | X2ChS = 10.647 | 0.001* |
| February | 4 (7.4%) | 7 (6.7%) | FE | 1.000 |
n: Number; FE: Fishers exact test; X2ChS: Pearson’s Chi-square test for independence of observations.
*significant at P < 0.05.
Analysis of the demographic and toxicological data of deaths due to suicidal self-poisoning in the year before and after the declaration of the pandemic revealed no statistical differences regarding the age, gender and number of poisons used to induce suicide. In comparison, there was a significant increase in suicidal self-poisoned deaths from rural areas (P = 0.025), and the median delay time was significantly shorter during the pandemic year than before the pandemic declaration (2 versus 3 h, respectively). Regarding the rate of the need for ICU admission among patients before suicidal self-poisoning death occurred, there was no significant difference in the year before and after the declaration of the pandemic (Table 7).
Table 7.
Demographic and toxicological data of suicidal self-poisoned deaths one year before and one year following the COVID-19 pandemic declaration in March 2020.
| Variables | 2019–2020 (n = 54) | 2020–2021 (n = 104) | Test statistic | P-value | |
|---|---|---|---|---|---|
| Age (years) | Median [IQR] | 19 [16–27] | 22 [17–33.5] | Z = 1.805 | 0.071 |
| Min - Max | 7–52 | 13–73 | |||
| Age groups | Children (7–14 years) | 3 (5.6%) | 3 (2.9%) | XL = 2.217 | 0.137 |
| Adolescents (>14–19 years) | 25 (46.3%) | 41 (39.4%) | |||
| Adults (>19–60 years) | 26 (48.1%) | 57 (54.8%) | |||
| Elderly (>60 years) | 0 (0%) | 3 (2.9%) | |||
| Gender | Male | 20 (37%) | 37 (35.6%) | X2ChS = 0.033 | 0.856 |
| Female | 34 (63%) | 67 (64.4%) | |||
| Residence | Urban | 27 (50%) | 33 (31.7%) | X2ChS = 5.037 | 0.025* |
| Rural | 27 (50%) | 71 (68.3%) | |||
| Number of poisons | Single ingestion | 53 (98.1%) | 102 (98.1%) | FE | 1.000 |
| Multiple ingestion | 1 (1.9%) | 2 (1.9%) | |||
| Delay time (hours) | Median [IQR] | 3 [2–5] | 2 [1–3] | Z = 3.123 | 0.002* |
| Min – Max | 0.5–20 | 0.5–11 | |||
| Need for ICU admission | No | 8 (14.8%) | 28 (26.9%) | X2ChS = 2.962 | 0.085 |
| Yes | 46 (85.2%) | 76 (73.1%) | |||
n: Number; IQR: interquartile range; Min: minimum; Max: maximum; X2ChS: Pearson’s Chi-square test for independence of observations; XL: Chi-square test for trend (linear by linear association); FE: Fisher’s exact test; Z: Mann–Whitney test.
*significant at P < 0.05.
Table 8 reveals that a large scale of poisons was involved in deaths due to suicidal self-poisoning in the year before the pandemic declaration. In contrast, only five poisons were involved in suicidal self-poisoning deaths in the year after the pandemic declaration, with a significant increase in deaths from aluminum and zinc phosphides, reaching 96.1% (P < 0.001).
Table 8.
Types of single ingestion poisons that led to suicidal self-poisoned deaths one year before and one year following the COVID-19 pandemic declaration in March 2020.
| Type of poison | 2019–2020 (n = 53) | 2020–2021 (n = 102) | Test statistic | P-value |
|---|---|---|---|---|
| Household and pesticide poisons: | ||||
| • Aluminum and zinc phosphides | 34 (64.2%) | 98 (96.1%) | X2ChS = 28.134 | <0.001* |
| • Organophosphorus compounds | 1 (1.9%) | 0 (0%) | FE | 0.342 |
| • Pyrethroids | 1 (1.9%) | 0 (0%) | FE | 0.342 |
| • Hydrocarbons | 1 (1.9%) | 0 (0%) | FE | 0.342 |
| CNS depressant drugs: | ||||
| • Opiates | 0 (0%) | 1 (1%) | FE | 1.000 |
| • Benzodiazepines | 1 (1.9%) | 0 (0%) | FE | 0.342 |
| • Antipsychotics | 3 (5.7%) | 1 (1%) | FE | 0.116 |
| • Antidepressants | 1 (1.9%) | 0 (0%) | FE | 0.342 |
| • Anticonvulsants | 2 (3.8%) | 0 (0%) | FE | 0.115 |
| Alcohols | 0 (0%) | 1 (1%) | FE | 1.000 |
| Cardiovascular drugs | 2 (3.8%) | 0 (0%) | FE | 0.115 |
| Xanthine derivatives | 0 (0%) | 1 (1%) | FE | 1.000 |
| Anti-diabetic drugs | 1 (1.9%) | 0 (0%) | FE | 0.342 |
| Paracetamol | 3 (5.7%) | 0 (0%) | FE | 0.038* |
n: Number; FE: Fisher’s exact test; X2ChS: Pearson’s Chi-square test for independence of observations.
*significant at P < 0.05.
Discussion
Concerns about increased suicidal attempts as a consequence of the COVID-19 pandemic have been raised worldwide.8 Previously, increased suicidal deaths have been reported during the Spanish Flu epidemic in 1918–1919. Researchers have related this to fears caused by the epidemic and the lack of social interaction.27 Having the same fears and social isolation during the COVID-19 pandemic has raised concerns about suicide rates in the current pandemic.28
In Egypt, the COVID-19 pandemic’s first wave started in March 2020 and peaked in June 2020, while the second wave began in mid-October and reached its peak in December 2020 and January 20213. Therefore, the current study aimed to evaluate the rate and pattern of suicide attempts and deaths by self-poisoning among patients admitted to TUPCC, Tanta University Hospitals, Egypt, one year before and one year following the COVID-19 pandemic declaration in Egypt.
The current study revealed that most admitted poisoned patients during the year after the declaration of the pandemic were due to suicidal issues (63.8%). However, there was a slight decrease in the total number of suicidal self-poisoned cases admitted during this year compared to the year before the declaration of the pandemic. At the same time, the rate of the need for ICU admission and suicidal self-poisoning deaths was significantly higher during the year after the declaration of the pandemic. In addition, the detailed monthly analysis of the numbers of admitted suicidal self-poisoned patients showed a significant decline during the months of the lockdown during the 1st wave of the pandemic, with subsequent significant elevation later on by the end of the second wave (January 2021) when compared with the incidence of suicidal self-poisoned cases during the same months of the year before the pandemic. Moreover, the monthly number of deaths due to suicidal self-poisoning showed a significant decrease during the first month of the pandemic (March 2020). On the other hand, it was alarming that there was a significant increase in deaths due to suicidal self-poisoning during the peak of the second wave of the pandemic in Egypt (January 2021).
This was in accordance with previous studies done in Egypt by Fayed and Sharif24 and Italy by Milella et al.29 which reported a decrease in the incidence of suicidal poisoning during the lockdown period compared to previous years. The authors in the Egyptian study attributed this decline to the decreased number of all admitted poisoning cases throughout the lockdown period that may be due to quarantine measures that restrict all transportation during the lockdown. But even so, they demonstrated that suicidal admissions constituted the highest incidence of admitted poisoned cases (58.2%), with a significant increase in mortality rates during the lockdown period among poisoned patients admitted to TUPCC. In the same line, Motawei et al.30 reported that Mansoura Emergency Hospital Poison Unit, Egypt cared for 26.2% fewer patients in 2020 than the two years before the pandemic.
Similarly, a fall in hospital presentations of self-poisoning has been reported during the first five months of the pandemic in Sri Lanka.31 Moreover, the initial lowering in self-poisoning rates in Poland have managed to decrease the overall number of self-poisoning cases during the year 2020.32 In Norway, the initial lowering in all suicidal deaths (including self-poisoning) was attributed to keeping mental health services open, in addition to the governmental role in financial support to people affected by the lockdown.9 The governmental support has managed to reduce suicidal self-poisoning rates initially in Japan as well. However, elevated rates later in the pandemic have also been reported.10
In the United Kingdom, suicidal rates from both self-poisoning and self-injury were reduced with strict lockdown measures, followed by elevation after easing the lockdown measures in May 20204. Lower rates of suicidal self-poisoning in France were attributed to the social support seen in national crises.11 Similar results were also found in the United States,33 and Germany.34 In the same line, Reger et al.35 reported that large-scale crises might lead to increased social support in the short term, so people who usually are alone receive more attention and become more socially supported than usual. In addition, life difficulties during such crises become less urgent with more appreciation for life.
On the other hand, Hadeiy et al.36 found no significant difference in the total number of intentional self-poisoning cases when comparing the frequencies of self-poisoning events and the proportions of hospital mortality one year before and one year after the pandemic in Tehran. They explained this result by saying that the period of lockdown helped more in family gatherings rather than loneliness, with better support to those suffering from anxiety, thus explaining the lower rates of self-poisoning early in the pandemic.
Conversely, higher rates of self-poisoning were reported in Taiwan in the 1st half of 2020. This was related to the financial hardship and unemployment that caused huge economic stress leading to higher rates of mental stress, substance use and suicide.37 In Nepal, similar increases were also reported in the early months of the pandemic.38 These results were in line with previous clinical and non-clinical studies that had expected higher rates of suicidal ideations and suicidal attempts during the COVID-19 pandemic. However, the main limitation of these studies was the lack of long-period assessment, making it hard to generalize their results.39 In addition, Neumann et al.40 predicted that the suicidal rates might increase with lockdowns and pandemic progression due to the resultant depression despite the decreased number of poisoned cases during the initial lockdown.
The effect of the pandemic on different groups of the population was not similar. The response was variable from one country to another and from one group to another.10 The susceptibility of varying age groups to self-poisoning and suicide was also variable from one place to another during the pandemic. In the current study, there were higher rates of suicidal self-poisoning among adolescents and lower rates among adults during the pandemic. In the same line, higher rates of suicide in young adults and adolescents during the pandemic were reported in Nepal,38 Tehran,36 and the United States.21,41 Suggesting that, the mental health of adolescents was affected by the pandemic and raising concerns about long-term consequences.42 Moreover, school closure as well could have worked as a double-edged weapon. Reducing outdoor activities might have affected some students’ mental well-being.10
On the other hand, lower rates of self-poisoning in adults were also reported in Japan. This decline was attributed to reduced working hours and working from home, which helped to reduce the burden on working adults with more productivity and better life satisfaction.10 In Tehran, household support during the lockdown was addressed as a good reason for suicide reduction.36 However, the lockdown could have resulted in reverse effects with increased housework and risk of domestic violence, thus affecting the housewives’ psychological health.43
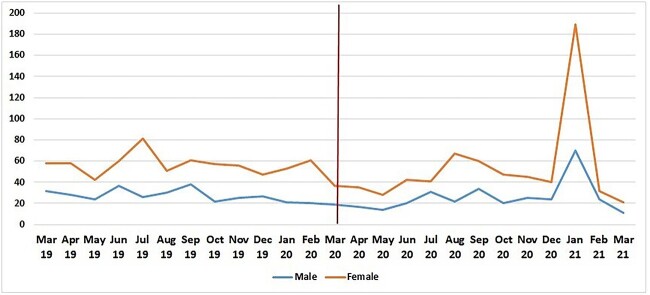
Variable effects of the COVID-19 pandemic on gender have been reported around the world. In the current study, gender was not significantly affected during the start of the pandemic; however higher rate of female self-poisoning was reported late in the pandemic as shown in Fig. 3. Similar results were reported in Japan,10 Nepal,38 and the United States,21 while lower rates of female self-harm were reported in France,11 and the United Kingdom.44 Conversely, increased self-poisoning among men was reported in Poland,32 and Tehran.36 This was explained by the higher economic burden on men during the pandemic.10
Fig. 3.
Number of suicidal self-poisoned patients admitted to TUPCC from the beginning of March 2019 to the end of February 2021 differentiated by gender.
The residency of involved suicidal self-poisoned patients showed no significant difference between both years, but there was a significant increase in the incidence of suicidal self-poisoned deaths from rural areas during the year following the declaration of the pandemic in this study. This could be explained by Kasemy et al.17 who found an increased risk of attempting suicide among patients living in rural areas and those with low socioeconomic status. This was attributed to the consequent illicit drug use associated with low income and the resulting anxiety.45,46
A significant increase in the pre-hospitalization time was found during the year following the declaration of the pandemic in this study. Avoiding hospital visits and delayed presentation in the emergency department has been reported by many studies during the pandemic, as a result of people’s fear of contracting COVID-19 infection.47–49 This also could explain the significant decrease in the length of the hospital stay during the same year in this study. Moreover, delayed hospital arrival, seeking medical advice and initiating resuscitation procedures may be potential factors for higher morbidities and mortalities in 2020 during the lockdown.50
Using a single substance for suicidal self-poisoning was the most prevalent before and during the pandemic in the current study. The most commonly used poison was phosphides (including aluminum and zinc phosphides), with a significant increase during the pandemic. Moreover, during the pandemic phosphides (including both aluminum and zinc phosphides) accounted for 96.1% of suicidal self-poisoning deaths from a single exposure, with a significant increase from the year before (64.2%). This could explain the significant increase in the rates of the need for ICU admission and suicidal self-poisoning deaths from rural areas during the pandemic. This was comparable with Behera et al.51 who reported that about 51% of deaths due to poison intake in North India during the COVID-19 pandemic were secondary to aluminum phosphide poisoning. They probably attributed this result to the delayed hospital arrival during lockdown with the lack of a specific antidote for aluminum phosphide poisoning.
Phosphide poisoning is emerging as a common self-poisoning agent with too high morbidity and mortality rates in Egypt due to its low price and easy availability in rural areas.52,53 Moreover, it is sold without restrictions, lacking proper container instructions.24 Phosphides are highly toxic and highly lethal poisons. The release of phosphine gas following ingestion results in multi-organ failure with a higher probability of death.54 In a five years period study, conducted in TUPCC, a strong link between higher mortality rates from aluminum phosphide and young ages, rural residency, suicidal self-poisoning, and the longer pre-hospitalization period has been reported.55
In the current study, organophosphates’ and carbamates’ use for suicidal self-poisoning was significantly lower during the pandemic; however, they remained the most common poisons used following phosphides. More or less in the same line, organophosphates were the most common poison used for self-poisoning in Nepal,38 while painkillers were the most prevalent in Poland,32 and paracetamol was the most prevalent in United States.41 Substances used in self-poisoning cases are continuously changing and affected by many factors including: local environment, culture, and different strategies in poison prevention in various countries. Pesticides are the most used poison for self-poisoning in developing agricultural countries. While using medical drugs is most common for self-poisoning in developed countries.56
Although our results revealed a significant increase in suicidal self-poisoned deaths during the COVID-19 pandemic, there was no significant difference in the age and gender of died suicidal self-poisoned patients in both years. Higher mortality rates from self-poisoning during the pandemic were also reported in Sri Lanka by Knipe et al.31 In Iran, mortality in the pandemic was higher among men and was associated significantly with increased age.36 On the other hand, the number of deaths following self-harm was nearly the same as before the pandemic in both France11 and Korea.22
Conclusion
The effect of the COVID-19 pandemic on suicidal self-poisoning was variable as the pandemic went on in Egypt. Suicidal self-poisoning was the manner of poisoning in about two-thirds of total admitted poisoned patients through the year following the declaration of the pandemic in Egypt, however, the total number of suicidal self-poisoned patients during this year was slightly decreased compared to the year before. Furthermore, our study reported a significant lowering in the rate of suicidal self-poisoned patients during months of the lockdown following the declaration of the pandemic in Egypt, with a subsequent significant increase that reached an alarming level during the peak of the second wave of the pandemic in Egypt.
A higher rate of female suicidal self-poisoning was reported late in the pandemic. Adolescents were the most vulnerable in mental health affection, while adults may benefit from releasing work stress during the pandemic. There was a significant increase in the incidence of suicidal self-poisoning deaths in rural areas. Phosphide poisoning was the most commonly used poison during the year following the declaration of the pandemic, and significant delays in getting to the hospital due to the lockdown may be the reason for the high rates of ICU admissions and suicidal self-poisoning deaths during this year.
Strength and limitations
It is worth mentioning that this study was the first to analyze the pattern of suicidal self-poisoning and suicidal self-poisoning deaths over an extended period one year before and one year following the start of the COVID-19 pandemic in Egypt. Although, TUPCC is a large central poison control center in Egypt, it is still a one-center study and the results cannot be generalized. So, future larger-scale studies over a longer period with detailed analysis of suicidal self-poisoning circumstances are essential for generalization.
Recommendations
Studying the effect of the COVID-19 pandemic on suicidal self-poisoning may help the preparation for defensive measures against similar crises and lockdowns in the future, especially in developing countries with low resources as Egypt. Close attention should be paid to the mental and psychological health of females and adolescents to help to reduce the incidence of suicide attempts among these critical population groups especially during any crisis or pandemics. Considering permanent changes in the working system and applying new modalities to relieve adults’ stressors could help lower suicidal rates. In developing countries, it is essential to restrict pesticide handling and establish free psychic consultations to reduce suicidal self-poisoning attempts and suicidal self-poisoning deaths, especially in rural areas.
Acknowledgments
The authors express their appreciation to TUPCC for facilitating data collection and acknowledge their colleagues responsible for electronic documentation of patient data for their assistance in this work.
Contributor Information
Amira Elsayed Elhawary, Forensic Medicine and Clinical Toxicology Department, 6th floor, Faculty of Medicine, Tanta University, Medical Campus, Al‑Geish Street, Tanta, Gharbia 31527, Egypt.
Heba Ibrahim Lashin, Forensic Medicine and Clinical Toxicology Department, 6th floor, Faculty of Medicine, Tanta University, Medical Campus, Al‑Geish Street, Tanta, Gharbia 31527, Egypt.
Noha Fawzy Fnoon, Neuropsychiatry Department, Faculty of Medicine, Tanta University, Medical Campus, Al‑Geish Street, Tanta, Gharbia 31527, Egypt.
Ghada Attia Sagah, Forensic Medicine and Clinical Toxicology Department, 6th floor, Faculty of Medicine, Tanta University, Medical Campus, Al‑Geish Street, Tanta, Gharbia 31527, Egypt.
Author contributions
All persons who meet authorship criteria are listed as authors, and all authors certify that they have participated sufficiently in the work. All authors read the manuscript and approve it.
Amira Elhawary conceptualized the study, collected the data, participate in data analysis, interpretation, manuscript writing, and approved the final manuscript.
Heba Lashin conceptualized the study, collected the data, participate in data analysis, interpretation, manuscript writing, and approved the final manuscript.
Noha Fnoon conceptualized the study, collected the data, participate in data analysis, interpretation, manuscript writing, and approved the final manuscript.
Ghada Sagah conceptualized the study, collected the data, participate in data analysis, interpretation, manuscript writing, and approved the final manuscript.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Conflict of interest statement: None declared.
Data availability
The datasets used and/or analyzed during this study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
References
- 1. World Health Organization (WHO) . Mental health and psychosocial considerations during the COVID-19 outbreak. 2020 March 18. © World Health Organization 2020. https://apps.who.int/iris/handle/10665/331490.
- 2. El-Sheekh MM, Hassan IA. Lockdowns and reduction of economic activities during the COVID-19 pandemic improved air quality in Alexandria, Egypt. Environ Monit Assess. 2020:193(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Samir A, Elabd AM, Mohamed W, Baess AI, Sweed RA, Abdelgawad MS. COVID-19 in Egypt after a year: the first and second pandemic waves from the radiological point of view; multi-center comparative study on 2000 patients. Egypt J Radiol Nucl Med. 2021:52(1):168. [Google Scholar]
- 4. Hawton K, Casey D, Bale E, Brand F, Ness J, Waters K, Kelly S, Geulayov G. Self-harm during the early period of the COVID-19 pandemic in England: comparative trend analysis of hospital presentations. J Affect Disord. 2021:282:991–995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Serafini G, Parmigiani B, Amerio A, Aguglia A, Sher L, Amore M. The psychological impact of COVID-19 on the mental health in the general population. QJM. 2020:113(8):531–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ammerman BA, Burke TA, Jacobucci R, McClure K. Preliminary investigation of the association between COVID-19 and suicidal thoughts and behaviors in the U.S. J Psychiatr Res. 2021:134:32–38. [DOI] [PubMed] [Google Scholar]
- 7. Carlin GL, Baumgartner JS, Moftakhar T, König D, Negrin LL. Impact of COVID-19 lockdown on suicide attempts. Wien Klin Wochenschr. 2021:133(17):915–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM. 2020:113(10):707–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Qin P, Mehlum L. National observation of death by suicide in the first 3 months under COVID-19 pandemic. Acta Psychiatr Scand. 2021:143(1):92–93. [DOI] [PubMed] [Google Scholar]
- 10. Tanaka T, Okamoto S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat Hum Behav. 2021:5(2):229–238. [DOI] [PubMed] [Google Scholar]
- 11. Olié E, Nogue E, Picot M, Courtet P. Hospitalizations for suicide attempt during the first COVID-19 lockdown in France. Acta Psychiatr Scand. 2021:143(6):535–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lim M, Lee SU, Park J-I. Difference in suicide methods used between suicide attempters and suicide completers. Int J Ment Health Syst. 2014:8(1):54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Spiller HA, Ackerman JP, Smith GA, Kistamgari S, Funk AR, McDermott MR, Casavant MJ. Suicide attempts by self-poisoning in the United States among 10–25 year olds from 2000 to 2018: substances used, temporal changes and demographics. Clin Toxicol. 2020:58(7):676–687. [DOI] [PubMed] [Google Scholar]
- 14. Kapur N, Turnbull P, Hawton K, Simkin S, Sutton L, Mackway-Jones K, Bennewith O, Gunnell D. Self-poisoning suicides in England: a multicentre study. QJM. 2005:98(8):589–597. [DOI] [PubMed] [Google Scholar]
- 15. Eddleston M. Patterns and problems of deliberate self-poisoning in the developing world. QJM. 2000:93(11):715–731. [DOI] [PubMed] [Google Scholar]
- 16. El-Farouny RH, Helmy MS. Suicidal self poisoning and its relation with personality traits among admitted cases to Menoufia poisoning control center. Egypt J Forensic Sci Appl Toxicol. 2021:21(1):13–30. [Google Scholar]
- 17. Kasemy ZA, Sharif AF, Amin SA, Fayed MM, Desouky DE, Salama AA, Abo Shereda HM, Abdel-Aaty NB. Trend and epidemiology of suicide attempts by self-poisoning among Egyptians. PLoS One. 2022:17(6):e0270026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Abd El Salam HF, Badr El Dine FMM, Abd El Kerim AM, Hieba RR, Kholeif WS. The applicability of Linehan risk assessment scale: a cross-sectional study from Alexandria poison centre, Egypt, during the COVID-19 pandemic. SN Compr Clin Med. 2022:4(1):218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kampf G, Todt D, Pfaender S, Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect. 2020:104(3):246–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Le Roux G, Sinno-Tellier S, Descatha A. COVID-19: home poisoning throughout the containment period. Lancet Public Health. 2020:5(6):e314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yard E, Radhakrishnan L, Ballesteros MF, Sheppard M, Gates A, Stein Z, Hartnett K, Kite-Powell A, Rodgers L, Adjemian J, et al. . Emergency department visits for suspected suicide attempts among persons aged 12-25 years before and during the COVID-19 pandemic - United States, January 2019-May 2021. MMWR Morb Mortal Wkly Rep. 2021:70(24):888–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ryu S, Nam HJ, Jhon M, Lee J-Y, Kim J-M, Kim S-W. Trends in suicide deaths before and after the COVID-19 outbreak in Korea. PLoS One. 2022:17(9):e0273637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. El-Sarnagawy G, Hafez A, Amer R. Characteristics of suicidal poisoned patients admitted to tertiary care center during COVID-19 pandemic. Egypt J Neurol Psychiatr Neurosurg. 2022:58(1):138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fayed MM, Sharif AF. Impact of lockdown due to COVID-19 on the modalities of intoxicated patients presenting to the emergency room. Prehosp Disaster Med. 2021:36(2):145–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Elgazzar FM, Afifi AM, Shama MAE, Askary AE, El-Sarnagawy GN. Development of a risk prediction nomogram for disposition of acute toxic exposure patients to intensive care unit. Basic Clin Pharmacol Toxicol. 2021:129(3):256–267. [DOI] [PubMed] [Google Scholar]
- 26. Hinkle DE, Wiersma W, Jurs SG. Applied statistics for the behavioral sciences. 5th ed. Boston, Mass., London: Houghton Mifflin; 2003. [Google Scholar]
- 27. Wasserman IM. The impact of epidemic, war, prohibition and media on suicide: United States, 1910–1920. Suicide Life Threat Behav. 1992:22(2):240–254. [PubMed] [Google Scholar]
- 28. Ornell F, Schuch JB, Sordi AO, Kessler FHP. “Pandemic fear” and COVID-19: mental health burden and strategies. Braz J Psychiatry. 2020:42:232–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Milella MS, Boldrini P, Vivino G, Grassi MC. How COVID-19 lockdown in Italy has affected type of calls and Management of Toxic Exposures: a retrospective analysis of a poison control center database from March 2020 to May 2020. J Med Toxicol. 2021:17(3):250–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Motawei SM, Shabka OA, Liu H. Poisoning during the COVID-19 pandemic and lockdown: retrospective analysis of exposures reported to the poison unit of the Mansoura emergency hospital. Toxicol Commun. 2022:6(1):66–70. [Google Scholar]
- 31. Knipe D, Silva T, Aroos A, Senarathna L, Hettiarachchi NM, Galappaththi SR, Spittal MJ, Gunnell D, Metcalfe C, Rajapakse T. Hospital presentations for self-poisoning during COVID-19 in Sri Lanka: an interrupted time-series analysis. Lancet Psychiatry. 2021:8(10):892–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sein Anand Ł, Sein AJ. Self-poisonings before and during the initial year of the COVID-19 pandemic in northern Poland. Int J Occup Med Environ Health. 2022:35(5):527–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Faust JS, Shah SB, Du C, Li S-X, Lin Z, Krumholz HM. Suicide deaths during the COVID-19 stay-at-home advisory in Massachusetts, March to May 2020. JAMA Netw Open. 2021:4(1):e2034273–e2034273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Radeloff D, Papsdorf R, Uhlig K, Vasilache A, Putnam K, Klitzing K. Trends in suicide rates during the COVID-19 pandemic restrictions in a major German city. Epidemiol Psychiatr Sci. 2021:30(e16):e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Reger MA, Stanley IH, Joiner TE. Suicide mortality and coronavirus disease 2019-A perfect storm? JAMA Psychiatry. 2020:77(11):1093–1094. [DOI] [PubMed] [Google Scholar]
- 36. Hadeiy SK, Gholami N, McDonald R, Rezaei O, Kolahi A-A, Zamani N, Shamsi-Lahijani A, Noghrehchi F, Carter G, Hassanian-Moghaddam H. Hospital-treated intentional self-poisoning events and in-hospital mortality in Tehran before and during the COVID-19 pandemic. Curr Psychol. 2022:26:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Tan ST, Chen TH, Yang HW, Su YJ. Changes in poisoning during the COVID-19 pandemic worldwide. Am J Emerg Med. 2022:56:291–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Shrestha R, Siwakoti S, Singh S, Shrestha AP. Impact of the COVID-19 pandemic on suicide and self-harm among patients presenting to the emergency department of a teaching hospital in Nepal. PLoS One. 2021:16(4):e0250706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Dubé JP, Smith MM, Sherry SB, Hewitt PL, Stewart SH. Suicide behaviors during the COVID-19 pandemic: a meta-analysis of 54 studies. Psychiatry Res. 2021:301:113998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Neumann NR, Chai PR, Wood DM, Greller HA, Mycyk MB. Medical toxicology and COVID-19: our role in a pandemic. J Med Toxicol. 2020:16(3):245–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Farah R, Rege SV, Cole RJ, Holstege CP. Suspected suicide attempts by self-poisoning among persons aged 10-19 years during the COVID-19 pandemic - United States, 2020-2022. MMWR Morb Mortal Wkly Rep. 2023:72(16):426–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Harris EC, Barraclough B. Suicide as an outcome for mental disorders: a meta-analysis. Br J Psychiatry. 2018:170(3):205–228. [DOI] [PubMed] [Google Scholar]
- 43. Leslie E, Wilson R. Sheltering in place and domestic violence: evidence from calls for service during COVID-19. J Public Econ. 2020:189:104241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Carr MJ, Steeg S, Webb RT, Kapur N, Chew-Graham CA, Abel KM, Hope H, Pierce M, Ashcroft DM. Effects of the COVID-19 pandemic on primary care-recorded mental illness and self-harm episodes in the UK: a population-based cohort study. Lancet Public Health. 2021:6(2):e124–e135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Liu X, Huang Y, Liu Y. Prevalence, distribution, and associated factors of suicide attempts in young adolescents: school-based data from 40 low-income and middle-income countries. PLoS One. 2018:13(12):e0207823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Sun J, Guo X, Zhang J, Wang M, Jia C, Xu A. Incidence and fatality of serious suicide attempts in a predominantly rural population in Shandong, China: a public health surveillance study. BMJ Open. 2015:5(2):e006762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Czeisler M, Marynak K, Clarke KEN, Salah Z, Shakya I, Thierry JM, Ali N, McMillan H, Wiley JF, Weaver MD, et al. . Delay or avoidance of medical care because of COVID-19-related concerns - United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020:69(36):1250–1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Nab M, Vehmendahl R, Somers I, Schoon Y, Hesselink G. Delayed emergency healthcare seeking behaviour by Dutch emergency department visitors during the first COVID-19 wave: a mixed methods retrospective observational study. BMC Emerg Med. 2021:21(1):56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Pikoulis E, Solomos Z, Riza E, Puthoopparambil SJ, Pikoulis A, Karamagioli E, Puchner KP. Gathering evidence on the decreased emergency room visits during the coronavirus disease 19 pandemic. Public Health. 2020:185:42–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Abdelkader SI, Abdelhamid WG, Wahdan MM, Eweda SA. Assessment of severity and outcome of poisoning before and during the era of COVID-19 pandemic. Toxicol Anal Clin. 2023:35(2):151–159. [Google Scholar]
- 51. Behera A, Singla N, Sharma N, Sharma N. Paradigm shift in pattern and prevalence of poisoning during COVID-19 pandemic. J Family Med Prim Care. 2022:11(1):208–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Deraz RH, Elrafey DS, Mesallam DIA. Acute aluminium phosphide poisoning in East Delta, Egypt: a growing public health problem over the last five years. Egypt Soc Clin Toxicol J. 2022:10(1):49–61. [Google Scholar]
- 53. Sagah GA, Oreby MM, El-Gharbawy RM, Ahmed Fathy AS. Evaluation of potential oxidative stress in Egyptian patients with acute zinc phosphide poisoning and the role of vitamin C. Int J Health Sci (Qassim). 2015:9(4):375–385. [PMC free article] [PubMed] [Google Scholar]
- 54. Shadnia S, Soltaninejad K, Hassanian-Moghadam H, Sadeghi A, Rahimzadeh H, Zamani N, Ghasemi-Toussi A, Abdollahi M. Methemoglobinemia in aluminum phosphide poisoning. Hum Exp Toxicol. 2011:30(3):250–253. [DOI] [PubMed] [Google Scholar]
- 55. El-Sarnagawy G. Predictive factors of mortality in acute aluminum phosphide poisoning: 5 years retrospective study in Tanta poison control unit. Ain Shams J Forensic Med Clin Toxicol. 2017:29(2):70–79. [Google Scholar]
- 56. Albano GD, Malta G, La Spina C, Rifiorito A, Provenzano V, Triolo V, Vaiano F, Bertol E, Zerbo S, Argo A. Toxicological findings of self-poisoning suicidal deaths: a systematic review by countries. Toxics. 2022:10(11):654. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during this study are available from the corresponding author on reasonable request.