Abstract
Objective:
In this review, we aim to provide an overview of literature on lymph node (LN) histomorphological features and their relationship with the prognosis in colorectal cancer (CRC).
Background:
Lymph nodes play a crucial role in the treatment and prognosis of CRC. The presence of LN metastases considerably worsens the prognosis in CRC patients. Literature has shown that the total number of LNs and the number negative LNs (LNnegs) has prognostic value in CRC patients. In esophageal carcinoma, LN size seems to be surrogate of the host antitumor response and a potentially clinically useful new prognostic biomarker for (y)pN0 esophageal carcinoma.
Methods:
A comprehensive search was performed in Pubmed, Embase, Medline, CINAHL, and the Cochrane library in March 2021. The PRISMA guidelines were followed. Only studies focusing on histomorphological features and LN size and their relation to overall survival were selected.
Results:
A total of 9 unique articles met all inclusion criteria and were therefore included in this systematic review. Six of these studies investigated HMF (eg, paracortical hyperplasia, germinal center predominance, and sinus histiocytosis) and 4 studies LNneg size and their relationship with overall survival. The presence of paracortical hyperplasia and an increased number of large LNnegs is related to a more favorable prognosis in CRC.
Conclusion:
The results of this systematic review seem to support the hypothesis that there is a relationship between the host antitumor response reflected in different histomorphological reaction patterns visible in LNnegs and LNneg size related to survival in CRC patients.
Keywords: colorectal cancer, lymph nodes, immune system, survival
Mini abstract: Lymph node (LN) staging plays an essential role in the treatment and prognosis of colorectal cancer. It has been hypothesized that nonmetastatic LN contains information indicative of a host antitumor response. This review supports this hypothesis and its relation with improved survival in colorectal cancer.
Definitions/abbreviations used
-
-
TNM stage I: The primary tumor has grown into the submucosa (T1) or has invaded the muscular layer of the colon or rectum (T2). There are no regional lymph node metastases and no distant metastases (T1 or T2, N0, M0).
-
-
TNM stage II: The primary tumor has grown through the muscular layer of the colon or the rectum into the subserosal fat (T3) or through the peritoneal surface (T4). (T3 or T4, N0, M0).
-
-
TNM stage III: Irrespective of the extent of invasion of the primary tumor, the cancer has spread to regional lymph nodes, there are no distant metastases (T1-4, N1 or N2, M0).
-
-
TNM stage IV: Irrespective of the extent of invasion of the primary tumor and the number of lymph node metastases, the cancer has spread to other parts of the body (presence of distant metastases) (any T, any N, M1).
-
-
Sinus histiocytosis (SH): The presence of large monocytic cells with vesicular nuclei and well-defined, somewhat granular, eosinophilic cytoplasm within the sinusoidal structures of the lymph nodes.
-
-
Germinal center predominance (GCP): Lymph nodes with the presence of an increased number of germinal centers inside the secondary lymphoid follicles.
-
-
Paracortical hyperplasia (PH): Lymph nodes with an expansion of the paracortical region due to an increased number of lymphocytes in these regions.
-
-
Lymphocyte depletion (LD): Lymph nodes showing a paucity of lymphocytes and an absence of germinal centers as well as fibrosis or hyalinization of the cortex region.
-
-
Unstimulated lymph nodes (ULN): Lymph nodes with a thin cortex showing lymphocytic follicles and ill-defined deep cortical regions.
-
-
Lymph node size (LNS): The largest diameter of lymph nodes in millimeters measured in the pathological specimen. Figure 1 shows a schematic view of lymph node structure and the location of immune cells.
Colorectal cancer (CRC) is the third most common cancer and the second most common cause of cancer-related death worldwide.1 Treatment is based on clinical disease stage [tumor, node, and metastasis (TNM) classification]. The presence of metastatic disease in the regional lymph nodes (LN) is one of the most important prognostic indicators determining (neo)adjuvant treatment.2–4
A higher number of LN metastases [positive LN (LNpos)] has been associated with a poorer prognosis in CRC patients.3,5 A review by Kim et al explored alternative factors that can influence survival beyond the number of LNpos such as LN ratio, LN distribution or location of metastatic LN, tumor deposits, and extracapsular invasion.6 A high LN ratio (LNpos/total number of LN) has been associated with poor prognosis.7–11 However, there is no consensus on what the universal cutoff value for LN ratio for clinical practice should be, which hinders clinical implementation of this factor.6 Although there is evidence supporting the use of lymph node distribution (LND) as a classification for metastatic LN,12,13 LND classification is currently not used in clinical practice for treatment decisions. One of the main reason for this might be that it is a time consuming process for surgeons and pathologists to process and report findings in LNs by location.14 Furthermore, there are studies suggesting that pathologic N status (eg, number of positive LN) was more significantly associated with survival than LND.14 Both tumor deposits and extracapsular invasion are emerging prognostic factors, but although the reporting of tumor deposits is recommended in international guidelines, treatment decisions are currently not using this information.6
Most literature about LNs in CRC focuses on the presence of metastasis in the LN. However, it has been suggested that regional, tumor-draining LN play a pivotal role in the initiation of a robust host antitumor response and that an increased LN size might be related with a better prognosis.15 A recent study by Kloft et al investigating esophageal cancers showed that irrespective of treatment modality, (y)pN0 patients with large LNneg had the best overall survival suggesting that LNneg size might be a surrogate marker of the host antitumor response and a potentially clinically useful new prognostic biomarker.16
In this review, we aim to provide an overview of the current literature on LN histomorphological features, their relationship with survival in CRC and the potential clinical value of these features in the diagnosis and treatment of CRC patients.
METHODS
This systematic review was reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.17,18 The review protocol was registered in the PROSPERO database (CRD42021244847).
Search Strategy
A search was performed in Pubmed, Embase, CINAHL, and the Cochrane database for the period from inception to March 2021. A second search was performed on the December 20, 2022, to assure no new publications were missed. The full search strategy is available in Appendix 1. Two reviewers independently performed the article selection and reviewed all included articles. Discrepancies were either resolved by discussion or by a third reviewer. The primary outcome of this systematic review is overall survival related to negative LN histomorphology. The following inclusion criteria were used: (1) studies that investigated the negative LN histomorphological reaction pattern (eg, sinus histiocytosis (SH), paracortical activity, LN hyperplasia, and LN size) in relation to survival in colorectal cancer patients, (2) study included 10 or more patients, (3) studies reported in English, German, or Dutch. Case reports, animal studies, letters to the editor, meeting abstracts, and expert opinions were excluded.
Data Extraction and Risk of Bias Assessment
Two reviewers (A.P. and B.V.) performed data extraction and risk of bias analysis independently, any differences were resolved by consensus. Data extracted included study characteristics (eg, year of publication, country of origin, design, and tumor type of interest), baseline patient characteristics, what negative LN histomorphology was assessed and survival data (Supplemental Table 1, http://links.lww.com/AOSO/A252). Quality assessment was performed by using the Quality In Prognosis Studies (QUIPS) checklist.19 Study domains (ie, study participation, study attrition, prognostic factor measurement, outcome measurement, study confounding, and statistical analysis and reporting) were assessed separately as being low, moderate, or high risk of bias.
Data Analysis
Basic descriptive statistics were used to summarize patient characteristics and survival data. The interquartile range (IQR) or the standard deviation was provided, when informative, for the interpretation of medians and means, respectively.
RESULTS
Literature Search
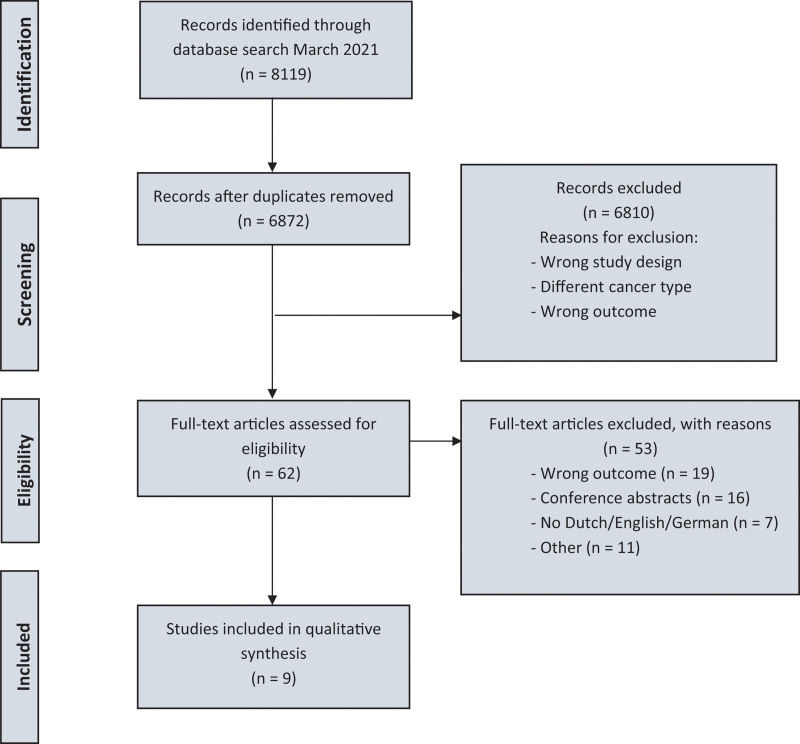
The search was performed in March 2021, and 6870 unique articles were identified of which 70 were included in the full-text analysis. Nine articles met all inclusion criteria and were included in qualitative synthesis. The PRISMA flow-chart is shown in Figure 2.
FIGURE 2.
Flow diagram of the article selection process.
FIGURE 1.
Schematic representation of lymph node structure.
Baseline Study Characteristics
Two prospective cohort studies20,21 and 7 retrospective cohort studies22–28 were included. The baseline characteristics of the included studies and patients are summarized in Supplemental Table 1, http://links.lww.com/AOSO/A252. The primary cancer was located in the colon in 5 studies, in the rectum in 1 study and colorectal in 3 studies. The reported mean or median age of patients ranged from 50 to 71 years. All studies reported sufficient follow-up for our research question.
Seven of 9 studies reported tumor stage using the Dukes classification, which was converted to AJCC/UICC eighth edition for the purpose of the current study.29 Five studies included TNM stage I CRC patients, 9 included TNM stage II CRC, 5 studies included TNM stage III CRC, and 1 included TNM stage IV CRC. The reported primary outcome was mostly 5-year overall survival, although some studies did not specify outcome range or used cancer-specific survival. Due to heterogeneity, pooling of data was not possible.
Sinus Histiocytosis
Three studies22–24 examined the association between the presence of SH in negative LNs and survival. The studies of Murray et al and Patt et al showed a favorable survival for patients where SH was present in the locoregional LN when all patients were analyzed together irrespective of tumor stage (76.7% vs 58.6%, P < 0.05 and 75% vs 50%, P < 0.05). However, the study by Pihl et al of stage II CRC patients did not show any association between the presence of SH and survival (Table 1).
TABLE 1.
Sinus Histiocytosis and Survival
| Study | Stage | Location | Absent SH, n | Survival | Present SH, n (%) | Survival | P * | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Colon | Rectum | Alive | Dead | % | Alive | Dead | % | |||
| Murray et al22 | II III II & III |
63 67 130 |
– – – |
31 20 51 |
14 22 36 |
68.9 47.6 58.6 |
17 16 33 |
1 9 10 |
94.4 64.0 76.7 |
<0.1 >0.2 <0.05 |
| Patt et al23 | I II III I–III |
1 15 20 36 |
– – – – |
0 4 5 9 |
0 6 3 9 |
0 40.0 62.5 50.0 |
1 4 9 14 |
0 5 3 4 |
100 80.0 75.0 75.0 |
N.A. N.A. N.A. <0.05 |
| Pihl et al24 | II | 71 | 63 | 68 | 23 | 74.7 | 32 | 5 | 86.5 | 0.38 |
A P < 0.05 was considered significant.
N.A. indicates not available; SH, sinus histiocytosis.
Germinal Center Predominance
Five studies20,23–25,28 examined the relationship between germinal center predominance (GCP) and survival. One study showed that increased GCP was associated with significant longer survival in stage II patients (77% vs 83%, P = 0.003)20 (Table 2). None of the other studies showed a relationship between GCP and survival.
TABLE 2.
Germinal Center Predominance and Survival
| Study | Stage (n) | Location | Absent GCP*, n | Survival | Present GCP*, n (%) | Survival | P * | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Colon | Rectum | Alive | Dead | % | Alive | Dead | % | |||
| Tsakraklides et al28 | I (16) II (19) III (24) I–III (59) |
– – – – |
– – – – |
– – – – |
– – – – |
– – – – |
14 16 13 42 |
2 3 11 17 |
87.5 84.2 54.2 71.2 |
N.A.*** N.A. N.A. N.A. |
| Patt et al23 | I–III (36) | 36 | – | – | – | – | – | – | – | n.s. |
| Pihl et al24 | II (134) | 71 | 63 | 21 | 2 | 91.3 | 79 | 26 | 75.2 | 0.21 |
| Pihl et al20 | I (71) II (213) III (163) IV (72) |
– – – – |
– – – – |
32 81 52 6 |
1 24 21 24 |
97 77 71 20 |
31 87 45 9 |
2 12 19 21 |
94 83 70 30 |
0.3 0.003 0.4 0.09 |
| Nacopulou et al (1981) | I II III I–III |
– – – 112 |
– – – 42 |
– – – – |
– – – – |
– – – – |
12 28 2 42 |
2 15 20 37 |
85 65 9 53 |
N.A. N.A. N.A. N.A. |
A P < 0.05 was considered significant.
GCP indicates germinal center predominance; N.A., not available.
Paracortical Hyperplasia
Fives studies examined the association between paracortical hyperplasia (PH) in negative LNs and survival. Patt et al reported a significant improved survival in stage I to III sigmoid cancer with increased PH (35% vs 74%, P = <0.05)23 (Table 3). Similar findings were reported by Pihl et al for PH in negative LNs and survival in stage II and stage III CRC patients.20,24 Pihl et al also investigated PH in tumor-involved LN and demonstrated a favorable survival in patients with PH compared with patients without (50% vs 73%, P = 0.009).
TABLE 3.
Paracortical Hyperplasia and Survival
| Study | Stage (n) | Location | Absent PH, n | Survival | Present PH*, n (%) | Survival | P * | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Colon | Rectum | Alive | Dead | % | Alive | Dead | % | |||
| Tsakraklides et al28 | I (9) II (11) III (8) I–III (28) |
– – – 33 |
– – – 110 |
– – – – |
– – – – |
– – – – |
5 5 2 15 |
3 5 5 13 |
67 55 44 54 |
N.A.*** N.A. N.A. N.A. |
| Patt et al23 | I (1) II (15) III (20) I–III (36) |
1 15 20 36 |
– – – – |
0 2 4 6 |
0 4 7 11 |
0 33 36 35 |
1 7 6 14 |
0 2 3 5 |
100 78 67 74 |
N.A. N.A. N.A. <0.05 |
| Pihl et al24 | II (134) | 71 | 63 | 37 | 15 | 71.2 | 63 | 13 | 83 | 0.04 |
| Pihl et al20 | I (71) II (213) III (163) IV (72) |
– – – – |
– – – – |
31 83 47 5 |
2 19 24 28 |
94 81 68 15 |
32 85 50 10 |
1 17 16 17 |
97 83 74 37 |
0.3 0.025 0.047 0.09 |
| Nacopoulou et al25 | I II III I–III |
– – – 112 |
– – – 42 |
– – – – |
– – – – |
– – – – |
9 13 4 – |
2 9 1 – |
81 59 80 – |
N.A. N.A. N.A. N.A. |
A P < 0.05 was considered significant.
N.A. indicates not available; PH, paracortical hyperplasia.
Lymph Node Size
Four studies investigated the relationship between LN size and survival in CRC patients.21,24,26,27 LN size was determined by macroscopically measuring the largest diameter of each LN. Two studies divided the patients in 2 groups, those with small LN versus those with large LN based on a self-defined cutoff value. Pihl et al stated that the presence of enlarged negative LN (>4.5 mm) tended to be associated with longer survival in stage II CRC, but this did not reach statistical significance (79% vs 86%, P = 0.057).24 Murphy et al defined LN ≥4 mm as large and showed a significant difference in survival in stage II CRC in favor of patients with large LNneg (73.3% vs 88.0%, P = 0.0015).26
The 2 remaining studies by Märkl and colleagues,21,27 investigating colon cancer without LN metastasis used a cutoff value of >5 mm for large LN. In the first study by Märkl et al, patients were classified based on the number of large LNs present. Patients with >7 LNs larger than 5 mm were classified as high (LN5High), and patients with <7 large LNs were classified as low (LN5Low). LN5High patients showed a better survival in comparison with LN5Low patients (P = 0.024). This was especially true for patients with higher T category (T1/2 vs T3/4, P = 0.033). They also showed a trend toward lower chance of progressive disease in the LN5High group [1 out of 28 (LN5high) vs 17 out of 69 (LN5low); P = 0.072).
In the 2016 study, patients were classified as LN5-very low (LN5vl, 0–1 LNs >5 mm), LN5-Low (LN5l, 2–5 LNs >5 mm), or LN5-High (LN5h, >5 LNs >5 mm). Survival analysis of the 3 groups showed a nonsignificant trend toward shorter median overall survival in de LN5vl group compared with both other groups (71 months vs 76 months, P = 0.230). The restriction to locally advanced patients (pT3/4) reveals significant survival differences with poor overall survival of the LN5vl group. Median overall survival for LN5vl, LN5l, and LN5h was 40, 57, 71 months, respectively (P = 0.022).
Lymph Node Histologic Patterns and Tumor Positive Nodes
Two studies compared LN histomorphological patterns between LNneg and LNpos CRC and their association with 5-year survival.25,28 Both studies compared the relationship between survival and lymphocyte predominance in de paracortex, GCP, Lymphocyte depletion (LD) in the paracortex, and unstimulated LN. Tsakraklides et al found a more favorable survival in patients with GCP compared with lymphocyte predominance/PH or unstimulated LN (71% vs 54%), but these results were not statistically significant. Nacopoulou et al found that patients with LNs showing lymphocyte predominance/PCP pattern had the best 5-year survival followed by patients with GCP pattern in their LN (68% vs 53%). Patients showing LD or unstimulated LNs had the poorest survival (10% vs 17%, respectively). The difference between histomorphological patterns was statistically significant, P < 0.05. When restricting to patients without LN metastasis, the trends for surival became less clear. GCP showed the best overall survival (70%) compared with paracortical predominance (66%), LD (16%), and unstimulated LNs (36%), but this difference was not significant.
Risk of Bias Assessment
A summary of the risk of bias assessment for each included study is shown in Figure 3. Overall, most studies were rated as having low or moderate risk of bias for most items. Possible study confounding appeared to be the most common problem.
FIGURE 3.
Risk of bias assessment using the QUIPS tool. Green, low risk of bias; yellow, moderate risk of bias; red, high risk of bias. QUIPS indicates quality in prognosis.
DISCUSSION
The findings of our review support the hypothesis that changes in LN morphology, for example, paracortical predominance or enlargement of regional LNnegs, might be indicative of an improved survival in stage II colorectal cancer patient. Changes seen in the histomorphology seem to suggest a potential relationship with the host antitumor response.
During the last two decades, no articles were published investigating immunological changes inside LNnegs. However, we were able to identify several old studies suggesting that changes in LN histomorphology may provide a “readout” of the host antitumor response and might provide clinically relevant information. This review shows that an increase in lymphocytes in the paracortex (so called paracortical predominance) seems to be a prognostic feature associated with a better survival.20,23,24 Matsuno et al reported that tumor antigens can cause immune activation through germinal center hyperplasia, PH, and SH in pancreatic cancer.30 Based on these results, it can be hypothesized that an increase in lymphocytes in the paracortex could be considered as surrogate for an active immune response of the host against the cancer.31
There are various reasons for LNs to grow in size, most common are the presence of LN metastases, immune activation, or the presence of intranodal fat. Immune activation causes enlargement due to hyperplasia of different cellular components in LNs (eg, follicular hyperplasia, PH, and SH).32 A recent study by Ruisch et al33 suggested that the size of LNnegs is related to the presence of follicular hyperplasia as well as the presence of intranodal fat in those LNs. In this study, the number of lymphoid follicles seemed to be higher in larger LNnegs. The authors hypothesized that LNneg surface area could be a potential clinical marker for the immunogenicity of the primary tumor and/or successful activation of a host’s response to tumor antigens. A study by Okada et al34 found that the presence high number of natural killer cells in the LNs was associated with a larger diameter of LNnegs and a significantly better survival. Combined, these results seem to support findings reported by Kloft et al in esophageal carcinoma.16
The immunogenicity of CRC tumors and the role of tumor-infiltrating lymphocytes (TILs) has seen a rise in interest over the last decades. pMMR tumors responding to ICI showed significant higher levels of T cells with CD8 and programmed death-1 (PD-1) coexpression before treatment, possibly indicating an active host antitumor response. Other studies indicate that certain TILs (CD3+, CD8+, and CD45RO+) play an important role in CRC tumor progression and prognosis.35–39 In 2005, a study by Pagès et al40 showed that patients with a high presence of tumor infiltrating and effector T cells (CD45RO+) were less likely to disseminate to regional lymph nodes and to lymphovascular and perineural structures. The Immunoscore (IS) further explores the prognostic value of TILs in CRC. Many studies using the IS showed that CRC patients with a high level of CD3+ and CD8+ had prolonged overall survival, disease-free survival and time to recurrence regardless of microsatellite status.35,39,41,42 A biopsy-adapted IS could possibly even aid with predicting therapy response in rectal cancer patients.43,44 Together with our observation, that hyperplasia of the LN paracortex (also known as a T-cell zone) relates to prolonged survival, this underlines that the host antitumor response probably is more than a local response and LNs play an important in the immunological reaction to the tumor.
The NICHE trial is one of the first studies administering neoadjuvant immune checkpoint inhibition (ICI) in nonmetastatic colon cancer and showing impressive responses in 100% (20/20) of dMMR and 27% (4/15) of pMMR patients. Although showing low response numbers in pMMR, an underlying immune activation was visible in the tumor microenvironment suggestive for tumor recognition. A longer duration of treatment can possibly further increase response rates in these pMMR tumors.45 Another recent study by Cercek et al investigated the use of ICI in the form of PD-1 blockade in dMMR rectal cancer. All 12 patients showed a clinical complete response after 6 months and omitted chemoradiotherapy and surgery.46 Both these studies show great potential of ICI in especially dMMR CRC. Being able to differentiate between large LNneg and large LN with metastases could aid in the identification of immunoactive pMMR tumors susceptible for pMMR. Future work is required to establish the viability of this concept.
There are several limitations to the current study. First, literature was scarce and several publications were from the 1980s, thus the methodology of these articles can be questionable. Still, valuable information was obtained from these studies. Second, the majority of the included studies were retrospective, single center studies with potential patient selection bias. Third, due to heterogeneous and scarce data and varying cutoff values for LN size, performing a meta-analysis was not possible. Despite these limitations, this systematic review provides the first available assessment of literature on the prognostic value of LNnegs histomorphology in CRC patients.
In summary, literature on the relationship between histomorphological patterns in regional negative lymph nodes and survival of CRC patients is very limited. Nevertheless, the results of this systematic review seem to support the hypothesis that there might be a relation between the host antitumor response reflected in different histomorphological reaction pattern visible in LNnegs, LNneg size, and survival in CRC patients. These findings suggest that it might be clinically useful to differentiate between large LNneg and large LNs with metastases through radiological imaging at diagnosis as large LNneg might indicate a highly immunogenic CRC microenvironment which might be treated differently in the near future. Based on the findings of this literature review, further work appears to be warranted to prospectively relate radiological LN findings to detailed histopathological assessment of LN microarchitecture, which might be achieved through a combination of radiomics and deep learning–based analysis of histological images. This type of study may pave the way to translate the measurable host antitumor reaction into patient-specific treatment decisions ultimately improving personalized care.
ACKNOWLEDGMENTS
HIG is supported in part by the National Institute for Health and Care Research (NIHR) Leeds Biomedical Research Centre. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Supplementary Material
Footnotes
Published online 6 November 2023
H.I.G. and J.M. are joint senior authors and joint corresponding authors.
Disclosure: The authors declare that they have nothing to disclose.
All authors were involved in the conceptualization and design of this review. A.J.P., M.K., and L.F.S.K. designed the search strategy with input from J.M.P.K. A.J.P. and B.A.v.d.V. collected and analyzed the data. A.J.P., B.A.v.d.V., H.I.G., and J.M. were responsible for data interpretation. A.J.P. drafted the first version of the article under supervision of H.I.G. and J.M. All authors were involved in the critical revision and final approval of the version to be published.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.annalsofsurgery.com).
H.I.G. and J.M. are joint senior authors and joint corresponding authors.
REFERENCES
- 1.Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–249. [DOI] [PubMed] [Google Scholar]
- 2.Brierley JD, Gospodarowicz MK, Wittekind C. TNM classification of malignant tumours. John Wiley & Sons; 2017. [Google Scholar]
- 3.Kim J, Huynh R, Abraham I, et al. Number of lymph nodes examined and its impact on colorectal cancer staging. Am Surg. 2006;72:902–905. [PubMed] [Google Scholar]
- 4.Nelson H, Petrelli N, Carlin A, et al. ; National Cancer Institute Expert Panel. Guidelines 2000 for colon and rectal cancer surgery. J Natl Cancer Inst. 2001;93:583–596. [DOI] [PubMed] [Google Scholar]
- 5.Jin M, Frankel WL. Lymph node metastasis in colorectal cancer. Surg Oncol Clin N Am. 2018;27:401–412. [DOI] [PubMed] [Google Scholar]
- 6.Kim HJ, Choi GS. Clinical implications of lymph node metastasis in colorectal cancer: current status and future perspectives. Ann Coloproctol. 2019;35:109–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peng J, Xu Y, Guan Z, et al. Prognostic significance of the metastatic lymph node ratio in node-positive rectal cancer. Ann Surg Oncol. 2008;15:3118–3123. [DOI] [PubMed] [Google Scholar]
- 8.Attaallah W, Gunal O, Manukyan M, et al. Prognostic impact of the metastatic lymph node ratio on survival in rectal cancer. Ann Coloproctol. 2013;29:100–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gao P, Song Y-x, Wang Z-n, et al. Integrated ratio of metastatic to examined lymph nodes and number of metastatic lymph nodes into the AJCC staging system for colon cancer. PLoS One. 2012;7:e35021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Berger AC, Sigurdson ER, LeVoyer T, et al. Colon cancer survival is associated with decreasing ratio of metastatic to examined lymph nodes. J Clin Oncol. 2005;23:8706–8712. [DOI] [PubMed] [Google Scholar]
- 11.Shimomura M, Ikeda S, Takakura Y, et al. Adequate lymph node examination is essential to ensure the prognostic value of the lymph node ratio in patients with stage III colorectal cancer. Surg Today. 2011;41:1370–1379. [DOI] [PubMed] [Google Scholar]
- 12.Kim CH, Huh JW, Kim HR, et al. Prognostic comparison between number and distribution of lymph node metastases in patients with right-sided colon cancer. Ann Surg Oncol. 2014;21:1361–1368. [DOI] [PubMed] [Google Scholar]
- 13.Hida J-i, Okuno K, Yasutomi M, et al. Number versus distribution in classifying regional lymph node metastases from colon cancer. J Am Coll Surg. 2005;201:217–222. [DOI] [PubMed] [Google Scholar]
- 14.Suzuki O, Sekishita Y, Shiono T, et al. Number of lymph node metastases is better predictor of prognosis than level of lymph node metastasis in patients with node-positive colon cancer. J Am Coll Surg. 2006;202:732–736. [DOI] [PubMed] [Google Scholar]
- 15.Rotman J, Koster BD, Jordanova ES, et al. Unlocking the therapeutic potential of primary tumor-draining lymph nodes. Cancer Immunol Immunother. 2019;68:1681–1688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kloft M, Ruisch JE, Raghuram G, et al. Prognostic significance of negative lymph node long axis in esophageal cancer: results from the randomized controlled UK MRC OE02 Trial. Ann Surg. 2022;277:e320–e331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Panic N, Leoncini E, De Belvis G, et al. Evaluation of the endorsement of the preferred reporting items for systematic reviews and meta-analysis (PRISMA) statement on the quality of published systematic review and meta-analyses. PLoS One. 2013;8:e83138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hayden JA, van der Windt DA, Cartwright JL, et al. Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158:280–286. [DOI] [PubMed] [Google Scholar]
- 20.Pihl E, Nairn RC, Milne BJ, et al. Lymphoid hyperplasia: a major prognostic feature in 519 cases of colorectal carcinoma. Am J Pathol. 1980;100:469. [PMC free article] [PubMed] [Google Scholar]
- 21.Märkl B, Rößle J, Arnholdt HM, et al. The clinical significance of lymph node size in colon cancer. Mod Pathol. 2012;25:1413–1422. [DOI] [PubMed] [Google Scholar]
- 22.Murray D, Hreno A, Dutton J, et al. Prognosis in colon cancer: a pathologic reassessment. Arch Surg. 1975;110:908–913. [DOI] [PubMed] [Google Scholar]
- 23.Patt DJ, Brynes RK, Vardiman JW, et al. Mesocolic lymph node histology is an important prognostic indicator for patients with carcinoma of the sigmoid colon: an immunomorphologic study. Cancer. 1975;35:1388–1396. [DOI] [PubMed] [Google Scholar]
- 24.Pihl E, Malahy MA, Khankhanian N, et al. Immunomorphological features of prognostic significance in Dukes’ class B colorectal carcinoma. Cancer Res. 1977;37:4145–4149. [PubMed] [Google Scholar]
- 25.Nacopoulou L, Azaris P, Papacharalampous N, et al. Prognostic significance of histologic host response in cancer of the large bowel. Cancer. 1981;47:930–936. [DOI] [PubMed] [Google Scholar]
- 26.Murphy J, Pocard M, Jass JR, et al. Number and size of lymph nodes recovered from dukes B rectal cancers: correlation with prognosis and histologic antitumor immune response. Dis Colon Rectum. 2007;50:1526–1534. [DOI] [PubMed] [Google Scholar]
- 27.Märkl B, Schaller T, Kokot Y, et al. Lymph node size as a simple prognostic factor in node negative colon cancer and an alternative thesis to stage migration. Am J Surg. 2016;212:775–780. [DOI] [PubMed] [Google Scholar]
- 28.Tsakraklides V, Wanebo HJ, Sternberg SS, et al. Prognostic evaluation of regional lymph node morphology in colorectal cancer. Am J Surg. 1975;129:174–180. [DOI] [PubMed] [Google Scholar]
- 29.Weiser MR. AJCC 8th edition: colorectal cancer. Ann Surg Oncol. 2018;25:1454–1455. [DOI] [PubMed] [Google Scholar]
- 30.Matsuno S, Kobari M, Hisano H, et al. Prognosis of the pancreatic cancer in terms of the regional lymph node reaction. Tohoku J Exp Med. 1985;145:291–302. [DOI] [PubMed] [Google Scholar]
- 31.Murphy K, Weaver C. Janeway’s immunobiology. Garland science; 2016. [Google Scholar]
- 32.Weiss LM, O’Malley D. Benign lymphadenopathies. Mod Pathol. 2013;26:S88–S96. [DOI] [PubMed] [Google Scholar]
- 33.Ruisch JE, Kloft M, Fazzi GE, et al. Large negative lymph nodes – a surrogate for immune activation in rectal cancer patients? Pathol Res Pract. 2020;216:153106. [DOI] [PubMed] [Google Scholar]
- 34.Okada K, Sadahiro S, Chan LF, et al. The number of natural killer cells in the largest diameter lymph nodes is associated with the number of retrieved lymph nodes and lymph node size, and is an independent prognostic factor in patients with stage II colon cancer. Oncology (Huntingt). 2018;95:288–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mlecnik B, Bindea G, Kirilovsky A, et al. The tumor microenvironment and immunoscore are critical determinants of dissemination to distant metastasis. Sci Transl Med. 2016;8:327ra326–327ra326. [DOI] [PubMed] [Google Scholar]
- 36.Pagès F, Kirilovsky A, Mlecnik B, et al. In situ cytotoxic and memory T cells predict outcome in patients with early-stage colorectal cancer. J Clin Oncol. 2009;27:5944–5951. [DOI] [PubMed] [Google Scholar]
- 37.Anitei M-G, Zeitoun G, Mlecnik B, et al. Prognostic and predictive values of the immunoscore in patients with rectal cancer. Clin Cancer Res. 2014;20:1891–1899. [DOI] [PubMed] [Google Scholar]
- 38.Wirta EV, Seppälä T, Friman M, et al. Immunoscore in mismatch repair‐proficient and‐deficient colon cancer. J Pathol Clin Res. 2017;3:203–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang X, Yang J, Du L, et al. The prognostic value of Immunoscore in patients with cancer: A pooled analysis of 10,328 patients. Int J Biol Markers. 2020;35:3–13. [DOI] [PubMed] [Google Scholar]
- 40.Pagès F, Berger A, Camus M, et al. Effector memory T cells, early metastasis, and survival in colorectal cancer. N Engl J Med. 2005;353:2654–2666. [DOI] [PubMed] [Google Scholar]
- 41.Pagès F, Mlecnik B, Marliot F, et al. International validation of the consensus Immunoscore for the classification of colon cancer: a prognostic and accuracy study. Lancet. 2018;391:2128–2139. [DOI] [PubMed] [Google Scholar]
- 42.Mlecnik B, Tosolini M, Kirilovsky A, et al. Histopathologic-based prognostic factors of colorectal cancers are associated with the state of the local immune reaction. J Clin Oncol. 2011;29:610–618. [DOI] [PubMed] [Google Scholar]
- 43.El Sissy C, Kirilovsky A, Van den Eynde M, et al. A diagnostic biopsy-adapted immunoscore predicts response to neoadjuvant treatment and selects patients with rectal cancer eligible for a watch-and-wait strategythe biopsy-adapted immunoscore in rectal cancer. Clin Cancer Res. 2020;26:5198–5207. [DOI] [PubMed] [Google Scholar]
- 44.Kirilovsky A, Sissy CE, Zeitoun G, et al. The “Immunoscore” in rectal cancer: could we search quality beyond quantity of life? Oncotarget. 2021;13:18–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chalabi M, Fanchi LF, Dijkstra KK, et al. Neoadjuvant immunotherapy leads to pathological responses in MMR-proficient and MMR-deficient early-stage colon cancers. Nat Med. 2020;26:566–576. [DOI] [PubMed] [Google Scholar]
- 46.Cercek A, Lumish M, Sinopoli J, et al. PD-1 blockade in mismatch repair–deficient, locally advanced rectal cancer. N Engl J Med. 2022;386:2363–2376. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.