Abstract
Objective:
Our objective was to identify factors associated with COVID-19 vaccination in trauma patients and to provide an opportunity for patients to engage in conversations about vaccination.
Background:
The trauma surgery service offers a unique opportunity to promote preventative health interventions in hard-to-reach populations.
Methods:
Trauma inpatients in Chicago, IL were recruited for this mixed-methods study from February 2022 to April 2022. Participants completed a survey on demographics, COVID-19 vaccination status, and Experiences of Discrimination Scale adapted for medical settings. Differences between vaccinated and unvaccinated patients were analyzed using the Wilcoxon-rank sum test. A semistructured, qualitative interview was completed. Qualitative data was transcribed and analyzed using Grounded Theory Methodology.
Results:
Fifty-eight trauma patients were surveyed, representing 88% of patients approached. Only 23 (40%) patients reported full vaccination to COVID-19. Previous vaccination (at least 1 dose) was associated with greater concern for COVID-19 (OR 3.47, 95% CI 1.987–6.964, P < 0.001) and higher income (OR 1.21, 95% CI 1.02–1.44, P = 0.03). Higher Experiences of Discrimination Scale scores were associated with decreased likelihood of prior vaccination (OR 0.97, 95% CI 0.95–0.99, P = 0.04). On qualitative analysis, recurrent themes included vaccination motivated by either community-based or personal health-related values, and disinterest in vaccination based on perceived low need or skepticism of experimentation. Fifteen patients (26%) eligible for a vaccine dose consented to onsite vaccination after the survey.
Conclusions:
Trauma patients who have experienced more discrimination in medical settings have lower rates of COVID-19 vaccination. Vaccination rates in our population were over 2 times lower than citywide rates, but admission to the trauma service can increase comprehensive care.
Keywords: COVID-19 vaccine, discrimination, health disparities, structural racism, trauma, vaccine hesitancy
Mini-Abstract: The trauma surgery service offers a unique opportunity to promote public health interventions in hard-to-reach populations with low vaccination rates. We surveyed trauma surgery patients and offered the opportunity to engage in conversations about vaccination. Trauma patients who have experienced more discrimination in medical settings have lower rates of COVID-19 vaccination.
Public health crises such as pandemics necessitate interventions that effectively reach every sector of the population. However, populations affected by structural racism and discrimination have historically been underserved and overlooked by public health efforts.1 As a result of factors related to structural racism and structural violence, COVID-19 death rates are 65% higher in Black Americans, while data reported by the Kaiser Family Foundation showed that the vaccination rates (by at least 1 dose) in White Americans are 6% higher than in Black Americans (56% vs 50%, latest data from November 2022).2 Vaccination is one of the most effective tools against COVID-19, and lower vaccination rates among communities of color and low-income communities contribute to the unequal disease burden in these groups.3 Justifiable vaccine hesitancy exists in Black populations, given the history of medical experimentation and distrust in the government and the medical profession.4 Vaccination hesitancy has long term, widespread implications for the future well-being of these communities and the trajectory of racial health disparities broadly.
Admission to the hospital, particularly through trauma care, offers a unique opportunity to interface with patients who might not otherwise present to the healthcare system. Medical mistrust is often tied to personal or community experiences of discrimination, resulting in the decision to reduce interaction with the medical field by this population.5 The nature of trauma requires these patients who may be hesitant to seek care for nonacute conditions to interface with the healthcare system in the setting of an acute injury. Additionally, the complexity of traumatic injuries and polytrauma often result in extended hospital stays, allowing for prolonged contact with healthcare professionals and the system broadly.6 Overall, this provides an opportunity for intervention and relationship building in a population that may not otherwise be reached by the current practices of our healthcare system.
Factors associated with low vaccine uptake need to be further explored to improve the effectiveness of public health interventions. We aimed to explore how experiences with health care and discrimination shape perspectives toward the public health interventions, using the COVID-19 vaccine as a case study. We hypothesized that greater experiences of discrimination in healthcare settings is associated with lower COVID-19 vaccination. Understanding these factors associated with the uptake of public health guidelines will inform not only future COVID-19 outreach but can also broadly inform the public health response to future crises.
METHODS
Design
This investigation was a pragmatic, mixed-methods study of trauma patients admitted to the trauma center between February and April 2022. The study included a survey and semistructured, qualitative interview for patients, with time to answer any patient questions about COVID-19 vaccination and the opportunity to request vaccination as an inpatient.
Patients
Participants included all patients who were admitted to the hospital because of traumatic injury. All patients were over the age of 16 and were able to communicate in English. Patients were approached by study staff in their inpatient rooms for interviews near their discharge date or when medically stable. The overall demographics of participants are outlined in Table 1.
TABLE 1.
Participant Demographics
| Demographics | N (%) |
|---|---|
| Gender | |
| Male Female Nonbinary |
35 (60.3%) 22 (37.9%) 1 (1.7%) |
| Race | |
| Black or African American Caucasian Asian |
41 (70.7%) 16 (27.6%) 1 (1.7%) |
| Ethnicity | |
| Hispanic or Latinx Non-Hispanic or Latinx |
6 (10.3%) 52 (89.7%) |
| Age | |
| 16–25 26–40 41–60 61+ |
18 (31%) 19 (32.8%) 14 (24.1%) 7 (12.1%) |
Baseline patient demographics including gender identity, self-identified race, self-identified ethnicity, and age are shown.
N = number of patients. Percent of total patients included in the study indicated in parentheses.
Procedures
Patients provided verbal consent to participate in this study. The survey included questions on demographic factors, COVID-19 vaccination status, and the Everyday Discrimination Scale (EDS) adapted for medical settings. The EDS is a validated, 7-question survey, with higher scores indicating greater experiences of discrimination in healthcare. Greater agreement with each statement on a scale of 1–5 indicated a greater degree of experienced discrimination in the medical setting. Factors influencing vaccine uptake, including institutional trust and the role of discrimination in healthcare, were identified and explored through semistructured interviews. Interviewers were 4 first-year medical students (authors GK, RA, SO, and IB; 3 females and 1 male) with previous training in qualitative research methods, and interviewers identified themselves as when approaching patient rooms for participation in the study. The patients did not have a previous relationship with the interviewers, and the interviewers reported to the patients that they were conducting the study out of interest in patient perspectives on the COVID-19 vaccine. The interviewer encouraged participants to expand on responses when applicable. Interviews ranged from 5 to 20 minutes in length. General information about the COVID-19 vaccine, including the opportunity to ask questions and to request to be vaccinated while inpatient, was provided to the patient through this conversation with the interviewer if the patient 2 expressed interest. Qualitative interviews were audio-recorded and transcribed to maintain the accuracy of representation and quotation and stored in a secured university drive. Following the survey and qualitative interview, patients were asked if they would like to discuss questions about the COVID-19 vaccine with the medical student interviewer and given the opportunity to request vaccination in the hospital, and this decision was recorded and quantified as the number of patients seeking vaccination after the encounter. The COREQ checklist has been included as a supplemental file http://links.lww.com/AOSO/A268. Approval for this study was obtained from the University of Chicago’s Institutional Review Board, #21-2041.
Analysis
Descriptive statistics were analyzed and reported, including previous vaccination status. EDS score was summed for each participant and compared between patients who had at least 1 COVID-19 vaccine dose and those without the vaccine. Further demographic differences between patients who had at least 1 COVID-19 vaccine dose and unvaccinated patients were assessed using Wilcoxon-rank Sum or Fisher’s Exact tests. Reported concern for COVID-19 infection in oneself or a loved one on a survey scale of 1–4 was also collected and analyzed between groups. For variables that were statistically significant between groups, univariate linear regression was used to determine the degree of correlation with vaccination. Qualitative interview transcriptions were inductively coded using Grounded Theory Methodology to generate themes.7 Each of the 58 interviews were read and coded by 2 separate coders; a total of 4 coders analyzed the interviews as a whole. Additionally, the pairing of coders was rotated for each interview to increase variation in coder overlap. Codes were harmonized, and themes were generated from all interviews by the team of 5 coders.
RESULTS
Fifty-eight trauma patients were surveyed, representing 88% of patients approached. The demographics of study participants are demonstrated in Table 1. Of note, 70.7% of patients participating in the study identified as Black or African American, and 60.3% identified as male. There were no significant differences in previous vaccination status by race, ethnicity, age, or gender identity. Only 23 (40%) patients reported full vaccination to COVID-19, defined as at least 2 doses of a 2-dose series at the time of the study. These findings reveal that COVID-19 vaccination rates are up to 31% lower in the trauma population at baseline compared to the city as a whole (40% and 71.2%, respectively).8
Median total EDS score was 13 in the unvaccinated group (those who reported zero doses of the COVID-19 vaccine), and 8 in the vaccinated group (those with at least 1 dose of the COVID-19 vaccine) (P = 0.02, Table 2). Unvaccinated patients were more likely to report lower socioeconomic status (P = 0.05, Table 2). With each increase in income class on the survey, the likelihood of being vaccinated increased by an odds ratio of 1.21 (95% CI 1.02–1.44, P = 0.03). Greater concern for COVID-19 on survey scale of 1–4 was also strongly correlated with previous vaccination (OR 3.47 for each 1-point increase, 95% CI 1.99–6.96, P < 0.0001, Table 2).
TABLE 2.
Participant Demographics by Previous Vaccination Status
| Vaccinated (Patients With Any # of Doses) n=33 |
Not Vaccinated (No Doses) n=25 |
P | |
|---|---|---|---|
| Gender identity | 0.87 | ||
| Male Female Nonbinary |
19 13 1 |
16 9 0 |
|
| Race | 0.87 | ||
| Black or African American White or Caucasian Asian |
22 10 1 |
19 6 0 |
|
| Ethnicity | 1 | ||
| Non-Hispanic or Latino Hispanic or Latino |
30 3 |
22 3 |
|
| Age | 0.16 | ||
| 16–25 26–40 41–60 61+ |
8 9 10 6 |
10 10 4 1 |
|
| Income | 0.05 | ||
| $0–$30,000 $30,000–$60,000 $60,000–$100,000 >$100,000 |
17 11 5 0 |
20 2 0 1 |
|
| Education status | 0.31 | ||
| Some high school/diploma Some college Bachelors degree Masters degree or higher |
19 7 5 2 |
18 5 1 0 |
|
| Average concern about COVID on a scale of 1–4 (4—very concerned, 1—not concerned) | 3.41 | 1.87 | <0.0001 |
| Total EDS score (median) | 8.0 | 13.0 | 0.02 |
Self-reported demographic characteristics, responses to survey questions about concern for self or a family member contracting COVID-19, and median combined score on the Everyday Discrimination Scale adapted for medical settings are displayed in number of patients or average/median score in each group based on previous vaccination status. Previous vaccination status was distinguished by having zero vaccine doses before the survey or having one or more doses prior to the survey. Higher EDS scores indicate greater experiences of discrimination faced by the patient in the medical setting. P values from a 2-sample t-test given in the right column.
Thematic saturation was achieved with 58 qualitative interviews. Responses to the semistructured interviews illustrated patient reasons for vaccinating or not vaccinating, as well as general attitudes toward vaccines and the healthcare system. Major themes extracted from patient responses are summarized in Table 3. Patients who were vaccinated revealed varied motivations for choosing to get vaccinated for COVID-19 based on extrinsic and intrinsic interests at an almost equal rate (N = 15 and N = 17, respectively). Patients described extrinsic motivation as a desire to protect others and a sense of social responsibility. For those who reported intrinsic motivation, their personal health status, including comorbidities and fear of death, were most commonly reported. Awareness of racial disparities in COVID-19 mortality was also represented in this category as an intrinsic motivator for patients who did not want to be “another statistic.”
TABLE 3.
Insight on Decision to Vaccinate or Not from Qualitative Questions
| Theme | Representative Quote |
|---|---|
| Patients choose to become vaccinated because of a sense of social responsibility (N = 15) | “I want us [my family] to be protected and more protected against COVID…and I have older family members that I always visit” |
| Patients consider vaccination a decision for personal health rather than community health (N = 17) | “Being over 60, and having COPD,” “I’m really susceptible more than COVID than others will be” |
| Patients did not vaccinate because they view it as ineffective for their personal health or experimental (N = 13) | “If you get it, it ain’t doing nothing for you because a lot of people are getting it and still dying behind it. So it’s really no point in getting it in my eyes.”“Some of them are dying. So I personally don’t feel that I want a vaccine, something that has not been fully tested. Something that’s being experimented. I don’t want to be a part of that.” |
| Patients distrust the vaccine due to experienced discrimination or history of exploitation (N = 14) | “It would scare the crap out of anybody because they even said how they were in the Tuskegee experiment and syphilis experiment and all that crap. So, yeah, he’s experimented on us a lot as black people, so that in itself is discouraging. So the very people that supposed to be here to protect you are the very people that was here to ruin you”“I mean, it’s really in who you know, your connects, because people of color, we don’t get no special treatment unless we got somebody with us connect with some special treatment” |
Four major themes which emerged from coding of qualitative interviews by 2 independent coders are listed in the left column. Representative quotes from each theme were selected from interviews and are listed in the right column.
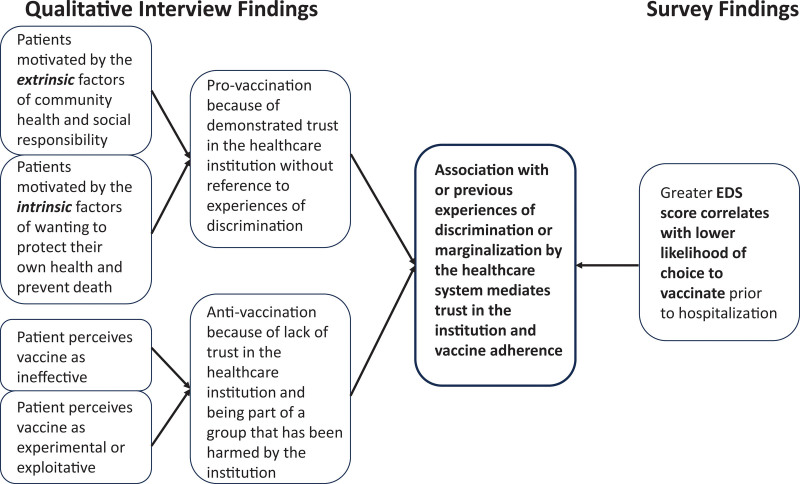
For those patients who discussed their decision not to receive the COVID-19 vaccine, 2 major themes emerged. The first was a belief that the vaccine was not necessary or was ineffective in protecting people from COVID-19 (N = 13). Some patients reported feeling that the vaccine was an experiment imposed by the government in which they did not want to participate, suggesting mistrust in the lack of transparency from public officials (N = 14). Some patients (N = 3) directly cited historical instances of experimentation and exploitation of Black patients that caused extreme harm, such as the Tuskegee Experiment, as justification for their mistrust of the COVID-19 vaccine.9 The vast majority of patients reported no barriers to accessing vaccination for themselves or anyone they knew. A summary of the combined insights from the survey and qualitative analysis is demonstrated in Figure 1.
FIGURE 1.
Summary of combined mixed-methods findings.
Following the survey and brief conversation with the medical student interviewer, 15 patients (26%) consented to have the inpatient pharmacy dispatched to administer a dose of the vaccine. Average concern about COVID-19 on a scale of 1–4 was highly correlated with the decision to be vaccinated after the study (P = 0.0001).
CONCLUSIONS
In this study, we examined rates of COVID-19 vaccination among patients admitted to the trauma surgery service and investigated relationships between institutional trust, experiences of discrimination, and participation in public health initiatives in a patient group with significantly low levels of access to necessary health care, coupled with a high burden of chronic diseases.8 This trauma patient population also includes a large number of minority and marginalized populations. These associations alone indicate a failure of our public health infrastructure to serve these patients and to mitigate the impact of structural racism, themes that were further explored in this study. Although vaccine adherence was low in the initial study population, over a quarter of these trauma patients eligible for another vaccine dose consented to onsite vaccination after a brief conversation with a medical student willing and able to listen to and answer questions. We feel this exemplifies the opportunity that trauma care presents the opportunity to easily provide concurrent general health and public care measures to patients.
The association of personal experiences of discrimination in medical settings with lower rates of vaccination was underscored by the comments from patients who expressed fears of experimentation and distrust related to historic instances of exploitation. This suggests these remain—and understandably so—strong influences on a patient’s decision to participate in public health interventions today. The connection between experiences of discrimination and health-seeking behavior among marginalized groups has been described in previous studies. In an investigation of patients living with a disability, rates of health-seeking behaviors were reported as significantly lower among those who perceived discrimination compared with those who did not.10 Medical and social mistreatment in the healthcare setting is also correlated with reduced interactions with medical care among people who use drugs.11 The connection between experiences of discrimination and health-seeking behaviors may also be modified by the factor of generational mistrust, a theme that was referred to by many patients in this study. Other studies have found that mistrust is negatively associated with adherence to public health-protective behaviors, and Black Americans have particularly high rates of mistrust.12,13 Our study included a majority Black population, many of whom were affected by interpersonal violence. These patients represent another example of a marginalized group, whose health-seeking behavior is affected by past experiences of discrimination and identification with groups that have historically been exploited by the medical system. In this case, vaccination for COVID-19 represents a health-seeking behavior.
The relationship between structural discrimination and negative experiences in the healthcare setting has been recently explored as they relate to perspectives on COVID-19. One study looked at the impact of experiencing discrimination on behaviors related to the COVID-19 pandemic, using the general EDS scale, questions about structural and healthcare discrimination, and the medical mistrust index.14 The researchers found that everyday discrimination and healthcare discrimination were associated with significantly greater general medical mistrust. They also found that discrimination in health care and structural discrimination were associated with higher endorsement of health-specific COVID-19 conspiracy beliefs. Our study expands upon these findings by applying the EDS adapted for the medical setting to understand the relationship between past experiences of discrimination, specifically when accessing healthcare and COVID-19-related behavior. Our findings directly investigated the decision to vaccinate for COVID-19, as it correlates with EDS scores in healthcare settings within a population affected by traumatic injury.
Our study has several limitations. Our survey was not designed as a pre/postintervention measure to evaluate the impact of discussion with the interviewer upon willingness to be vaccinated during their inpatient admission. Additionally, the majority of patients who agreed to receive a COVID-19 vaccine dose as inpatients had received at least 1 dose already. Thus, while we find it interesting that 26% of patients did ask to have pharmacy dispatched after their interviews, we cannot conclude whether this was related to our study or to the discussions patients had with medical student interviewers. Additionally, the study was performed as a convenience sample in a trauma center with a patient population that is not representative of the broader public, so extrapolating these conclusions may be limited without further studies.
In summary, our mixed-methods study has uncovered extrinsic and intrinsic motivations for adherence to vaccination, a proxy for participation in other healthcare recommendations. Trauma patient populations similar to this study population represent a group of patients who are limited by experiences of discrimination in healthcare settings, which may contribute to hesitancy to vaccines and other health measures. This study demonstrates the influence that discriminatory experiences in the healthcare setting have on vaccination rates, which may translate to other areas of personal and public health.
Future studies should explore the association between experiences of discrimination and vaccination in other settings with other patient populations, given the previously described relationship between marginalization and health-seeking behavior. Other health-seeking behaviors should be further investigated as they relate to public health initiatives in order to improve healthcare uptake in these populations and prevent public health crises like COVID-19 in the future. Finally, there is great need for future interventional research, which aims to discover effective measures for establishing trust in populations with high EDS scores in the medical setting.
ACKNOWLEDGMENTS
We would like to thank all of the trauma patients who donated their time to participating in the study and sharing their experiences and perspectives.
Supplementary Material
Footnotes
The authors declare that they have nothing to disclose.
This study was approved by the University of Chicago’s Institutional Review Board: #21-2041.
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.annalsofsurgery.com).
REFERENCES
- 1.Churchwell K, Elkind MSV, Benjamin RM, et al. ; American Heart Association. Call to action: structural racism as a fundamental driver of health disparities: a presidential advisory from the american heart association. Circulation. 2020;142:e454–e468. [DOI] [PubMed] [Google Scholar]
- 2.Latest Data on COVID-19 Vaccinations by Race/Ethnicity. KFF. Available at: https://www.kff.org/coronavirus-covid-19/issue-brief/latest-data-on-covid-19-vaccinations-by-race-ethnicity/. Accessed December 23, 2022 [Google Scholar]
- 3.Tai DBG, Sia IG, Doubeni CA, et al. Disproportionate Impact of COVID-19 on racial and ethnic minority groups in the United States: a 2021 update. J Racial Ethn Health Disparities. 2022;9:2334–2339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Laurencin CT. Addressing justified vaccine hesitancy in the black community. J Racial Ethn Health Disparities. 2021;8:543–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Understanding and Ameliorating Medical Mistrust Among Black Americans. The Commonwealth Fund. [Google Scholar]
- 6.Mathew PJ, Jehan F, Kulvatunyou N, et al. The burden of excess length of stay in trauma patients. Am J Surg. 2018;216:881–885. [DOI] [PubMed] [Google Scholar]
- 7.Strauss A, Corbin J. Grounded theory methodology: an overview. In: Handbook of Qualitative Research. Sage Publications, Inc; 1994:273–285. [Google Scholar]
- 8.Chicago Health Atlas. Chicago Health Atlas. Available at: https://chicagohealthatlas.org/chicagohealthatlas.org/. Accessed December 23, 2022. [Google Scholar]
- 9.Tuskegee Study - Timeline - CDC - OS. Published December 20, 2022. Available at: https://www.cdc.gov/tuskegee/timeline.htm. Accessed December 23, 2022. [Google Scholar]
- 10.Moscoso-Porras MG, Alvarado GF. Association between perceived discrimination and healthcare-seeking behavior in people with a disability. Disabil Health J. 2018;11:93–98. [DOI] [PubMed] [Google Scholar]
- 11.Meyerson BE, Russell DM, Kichler M, et al. I don’t even want to go to the doctor when I get sick now: healthcare experiences and discrimination reported by people who use drugs, Arizona 2019. Int J Drug Policy. 2021;93:103112. [DOI] [PubMed] [Google Scholar]
- 12.Bogart LM, Ojikutu BO, Tyagi K, et al. COVID-19 related medical mistrust, health impacts, and potential vaccine hesitancy among black americans living with HIV. J Acquir Immune Defic Syndr. 2021;86:200–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arnett MJ, Thorpe RJ, Gaskin DJ, et al. Race, medical mistrust, and segregation in primary care as usual source of care: findings from the exploring health disparities in integrated communities study. J Urban Health. 2016;93:456–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.An Investigation of Associations Between Race, Ethnicity, and Past Experiences of Discrimination with Medical Mistrust and COVID-19 Protective Strategies. SpringerLink. Available at: https://link.springer.com/article/10.1007/s40615-021-01080-x. Accessed December 23, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]