Abstract
Objective:
To assess the 5-year recurrence rate of incisional hernia repair in Ventral Hernia Working Group (VHWG) 3 hernia with a slowly resorbable mesh.
Summary Background Data:
Incisional hernia recurs frequently after initial repair. In potentially contaminated hernia, recurrences rise to 40%. Recently, the biosynthetic Phasix mesh has been developed that is resorbed in 12–18 months. Resorbable meshes might be a solution for incisional hernia repair to decrease short- and long-term (mesh) complications. However, long-term outcomes after resorption are scarce.
Methods:
Patients with VHWG grade 3 incisional midline hernia, who participated in the Phasix trial (Clinilcaltrials.gov: NCT02720042) were included by means of physical examination and computed tomography (CT). Primary outcome was hernia recurrence; secondary outcomes comprised of long-term mesh complications, reoperations, and abdominal wall pain [visual analogue score (VAS): 0–10].
Results:
In total, 61/84 (72.6%) patients were seen. Median follow-up time was 60.0 [interquartile range (IQR): 55–64] months. CT scan was made in 39 patients (68.4%). A recurrence rate of 15.9% (95% confidence interval: 6.9–24.8) was calculated after 5 years. Four new recurrences (6.6%) were found between 2 and 5 years. Two were asymptomatic. In total, 13/84 recurrences were found. No long-term mesh complications and/or interventions occurred. VAS scores were 0 (IQR: 0–2).
Conclusions:
Hernia repair with Phasix mesh in high-risk patients (VHWG 3, body mass index >28) demonstrated a recurrence rate of 15.9%, low pain scores, no mesh-related complications or reoperations for chronic pain between the 2- and 5-year follow-up. Four new recurrences occurred, 2 were asymptomatic. The poly-4-hydroxybutyrate mesh is a safe mesh for hernia repair in VHWG 3 patients, which avoids long-term mesh complications like pain and mesh infection.
Keywords: biosynthetic mesh, CT scan, incisional hernia, long-term, recurrence
Mini abstract
Potentially contaminated VHWG 3 incisional hernia recurs frequently, and slowly resorbable Phasix meshes might be a solution. Since long-term outcomes are scarce, a 5-year follow-up was conducted. Results show a low recurrence rate of 15.9%, 4 recurrences between 2 and 5 years, and no long-term mesh complications, making the Phasix mesh a promising device.
INTRODUCTION
An incisional hernia frequently develops after midline laparotomy, varying between 15% in the normal population and up to 50% in high-risk groups.1 Incisional hernia may lead to pain, incarceration, and quality of life deterioration.2 For patients with a symptomatic incisional hernia, abdominal wall restoration by surgical reconstruction is indicated, which is generally performed by placement of a permanent synthetic mesh, as incisional hernia repair with suture only is known to result in high recurrence rates.3
Incisional hernia repair with permanent synthetic meshes is effective but may lead to long-term complications, such as seroma, chronic sinus tract formation, mesh infection, enterocutaneous fistulas, pain, and nerve entrapment after tacking of the mesh.4,5 Resorbable biologic meshes have been introduced to avoid these risks.6 Yet, a pitfall of these biological meshes is that their so-called remodeling characteristics do not always give the abdominal wall sufficient support for adequate restoration in the long term. Consequently, high recurrence rates are seen after the use of biologic meshes, especially when defects are bridged.7,8 Biosynthetic resorbable meshes have recently been developed to counter the disadvantages of biological and synthetic meshes.9 One of these is the biosynthetic poly-4-hydroxybutyrate (P4HB) Phasix mesh, which is resorbed after 12–18 months, which hypothetically provides the right timing for the abdominal wall to reconstruct, while infection susceptibility and long-term mesh complications are supposedly decreased compared to permanent synthetic meshes.10 Long-term mesh complications requiring reinterventions in incisional hernia repair using synthetic meshes are reported to be as high as 4.5% in 5 years.11 Reinterventions for chronic pain following synthetic mesh repair are reported to be 0.1–0.8.11,12 A multicenter international prospective cohort study was performed for incisional hernia repair with the P4HB Phasix mesh in potentially contaminated hernia. The 2-year follow-up results have been published previously.13
However, studies investigating long-term resorbable mesh behavior (>2 years) are scarce. Long-term studies are needed since surgeons fear incisional hernia recurrence after complete resorption of the mesh. Nonetheless, resorbable meshes may have an advantage in comparison to permanent synthetic mesh with regard to complications and reinterventions long-term. The main purpose of the present study was to evaluate long-term incisional hernia recurrence by physical examination and abdominal computed tomography (CT) scan. Secondary outcomes include long-term mesh complications and reoperations, abdominal wall pain at the scar and location and defect size of the recurrent hernias.
METHODS
The study protocol for the long-term update was approved by the medical ethics committee of the Imelda Hospital in Bonheiden, Belgium, whereafter every participating center (Bispebjerg Hospital, Copenhagen, Denmark; Elkerliek Hospital, Helmond, the Netherlands; University Hospital Lille, Lille, France; Vivantes Klinikum Spandau, Berlin, Germany; University Hospital Leuven, Leuven, Belgium; University College London Hospital, London, United Kingdom; University Hospital Gent, Gent, Belgium; Hôpital Cochin, Paris, France; Isala Hospital, Zwolle, the Netherlands; Università di Roma Sapienza, Rome, Italy; IJsselland hospital, Capelle aan den IJssel, the Netherlands; Chirurgische Praxis Ärztehaus, Cottbus, Germany; Isala Hospital, Zwolle, the Netherlands) had been sent the protocol for board review. Informed consent was obtained from every participating patient. This trial was registered at ClinicalTrials.gov (NCT:02720042).
Study Design
The methods of the original trial and results of the 2-year follow-up of the Phasix study were previously published.13,14
In brief: between 2016 and 2017, patients with a Ventral Hernia Working Group (VHWG) grade 3 midline incisional hernia were included in the single-arm interventional study. VHWG grade 3 incisional hernias are considered potentially contaminated hernias, with subsequent risk for complications.15 Patients from fifteen different European medical institutions scheduled for elective VHWG grade 3 incisional hernia repair were included. Patients underwent open incisional hernia repair with the placement of a P4HB mesh (Phasix Mesh, BARD B.D., Warwick, RI). The mesh was placed in the retro-rectus position (sublay), overlapping all edges of the defect by 5 cm.
Patients received standard care in their treating center postoperatively and were seen after 1, 3, 6, 12, 18, and 24 months for follow-up and screened for surgical site occurrence (SSO), reoperation rate, pain at the site of surgery, and hernia recurrence.
For the current investigation, all patients who were previously included in the study were invited at the beginning of April 2021 to July 2022 to the outpatient clinic for a physical examination by their operating surgeon and an abdominal nonenhanced CT scan. Baseline characteristics of patients included in the long-term study were collected from the 2-year follow-up.
Primary and Secondary Outcomes
Primary outcome was the incidence of incisional hernia recurrence by Kaplan–Meier analysis after 5 years of follow-up. Incisional hernia recurrence was defined according to the definition of the European Hernia Society: “any abdominal wall gap with or without bulge in the area of a postoperative scar perceptible or palpable by clinical examination or imaging”.16
The abdominal CT scan was assessed and reported by a radiologist from the local medical institution where the index incisional hernia repair with Phasix mesh was performed. If any discrepancies between the physical examination and CT were observed, the CT findings were decisive. If CT scanning was not deemed possible, only a physical examination was performed. Additional secondary outcomes were visual analogue score (VAS: 0–10) of abdominal wall pain at the scar site, long-term mesh complications, reoperations, and CT findings such as the location of the defect, size of the defect, fluid collections around the scar, and curvilinear distortions of soft-tissue thickening due to mesh fibrosis as described by Gavlin et al.17 The curvilinear distortion could imply fibrotic mesh remnants in the abdominal wall.
Statistics
Continuous variables were presented as mean with standard deviation (SD) or median with interquartile range (IQR). Discrete variables were presented as absolute numbers and percentages.
Overall cumulative recurrence rates were estimated using Kaplan–Meier analysis and a curve was plotted for overall recurrence incidence up to 5 years in an intention-to-treat analysis. Recurrence rate was mentioned with a standard error and its 95% confidence interval (95% CI). Risk factors for hernia recurrence like body mass index (BMI), reasons for VHWG 3, and incisional hernia width at inclusion for hernia recurrence were analyzed using Cox regression analysis with risk factors as independent variables and recurrence as dependent value expressed as hazard ratio (HR) in a per-protocol analysis.
Statistical analysis was performed with SPSS software version 26 (IBM SPSS Statistics for Mac version 26; IBM Corporation, Armonk, NY).
RESULTS
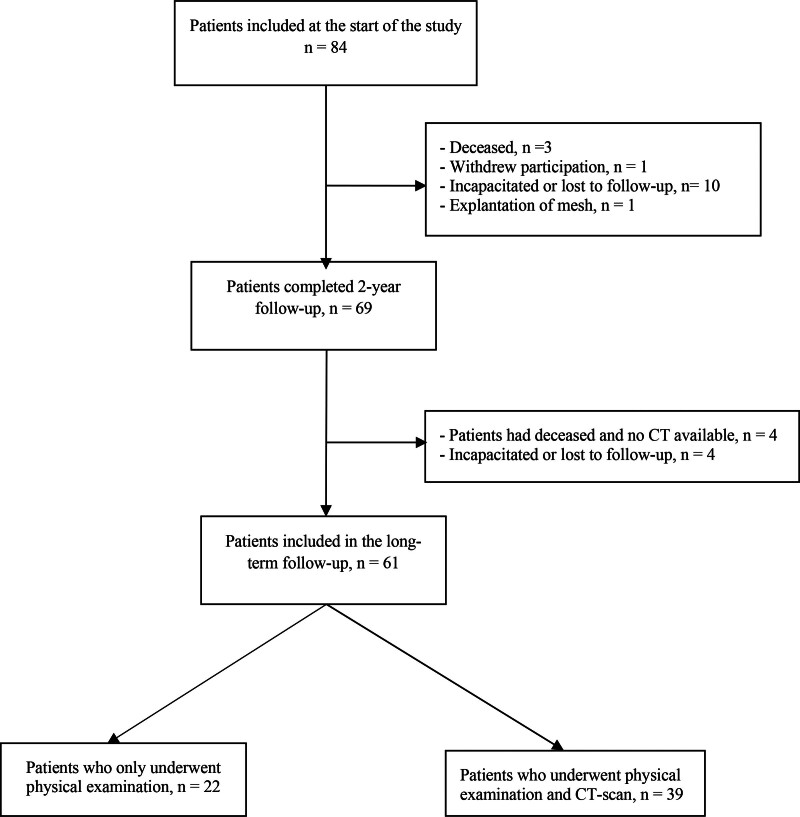
Of the 84 patients included in the (original) study, 15 patients (17.9%) did not complete the 2-year follow-up due to incapacitation or loss to follow-up (n = 7), mesh explantation (n = 4, 3 due to recurrence and 1 due to mesh infection), withdrawal from participation (n = 1), or death (n = 3). Of the remaining 69 eligible patients, 4 patients (5.8%) had deceased without prior CT scanning, and 4 (5.8%) were incapacitated or lost to follow-up. This resulted in a total of 61 patients that were included in the long-term study with a median of 60.0 months (IQR: 55–64) follow-up (Fig. 1).
FIGURE 1.
Study flow diagram.
Baseline Characteristics
Baseline characteristics of the 61 patients included for long-term assessment can be found in Table 1.16 Sixty percent of patients were male, mean age was 62.7 years, and previous wound infection or stoma presence were the main reasons for the incisional hernia to be graded VHWG 3. Other risk factors for incisional hernia formation were a mean BMI of 28.1 (SD: 3.9) and a history of cancer in 42.7% of patients. For most patients, the index incisional hernia repair with Phasix mesh was the primary incisional hernia surgery, with most of the patients having multiple midline defects (42.6%).
TABLE 1.
Baseline Characteristics of Patients With Long-Term Follow-Up
| Patients With Long-Term Follow-Up | N = 61 (%) |
|---|---|
| Sex | |
| Male | 37 (60.7%) |
| Female | 24 (39.3%) |
| Age, mean (SD) (years) | 62.7 (12.3) |
| Body mass index, mean (SD) (kg/m2) | 28.1 (4.0) |
| Smoking | 27 (44.3%) |
| COPD | 13 (21.3%) |
| Diabetes | 7 (11.5%) |
| Immunosuppression | 2 (3.3%) |
| History of cancer | 26 (42.7%) |
| VHWG 3 subdivision* | |
| Previous wound infection | 39 (63.9%) |
| Stoma present | 15 (24.6%) |
| Violation of the GI tract | 4 (6.6%) |
| Other | 3 (4.9%) |
| Index incisional hernia | |
| Primary | 51 (83.6%) |
| First recurrence | 5 (8.2%) |
| >1 recurrence | 5 (8.2%) |
| EHS incisional hernia classification† | |
| M1 | 1 (1.6%) |
| M2 | 13 (21.3%) |
| M3 | 12 (19.7%) |
| M4 | 7 (11.5%) |
| M5 | 2 (3.3%) |
| Multiple M defects | 26 (42.6%) |
| Median hernia width (cm) | 7 (5–10) |
| Median hernia length (cm) | 10 (6–15) |
| Follow-up time, median (IQR) (months) | 60.0 (55–64) |
Patients could present themselves with multiple reasons for VHWG 3 classification.
According to the article of Muysoms et al.16
IQR indicates interquartile range; SD, standard deviation.
Perioperative Characteristics of Patients Included in the 5-Year Follow-Up
Median operative time for the index incisional hernia repair with Phasix mesh was 155 minutes (IQR: 113.5–223.5), and more than half of patients (57.4%) underwent component separation technique (CST) (Table 2). Most of the CST procedures (31.1%) entailed an anterior component separation otherwise known as the (modified) Ramirez procedure.18 Median admission time was 8 days (IQR: 6–14); and 23 patients (37.7%) suffered from SSOs during the short-term follow-up, with seroma and surgical site infection being the most prevalent (11.5%).
TABLE 2.
Perioperative Characteristics of Patients With Long-Term Follow-Up
| N = 61 (%) | |
|---|---|
| Operating time, median (IQR) (minutes) | 155 (113.5–223.5) |
| Component separation technique | 35 (57.4%) |
| Anterior component separation, open | 19 (31.1%) |
| Posterior component separation | 10 (16.4%) |
| Anterior component separation, endoscopic | 6 (9.8%) |
| Hospital admission time, median (IQR) (days) | 8 (6–14) |
| Postoperative surgical site occurrences* | 23 (37.7%) |
| Seroma | 7 (11.5%) |
| Surgical site infection | 7 (11.5%) |
| Wound dehiscence | 5 (8.2%) |
| Hematoma | 4 (6.6%) |
Any SSO that occurred during the 2-year follow-up, excluding hernia recurrence.
IQR indicates interquartile range; SD, standard deviation.
Primary and Secondary Outcomes
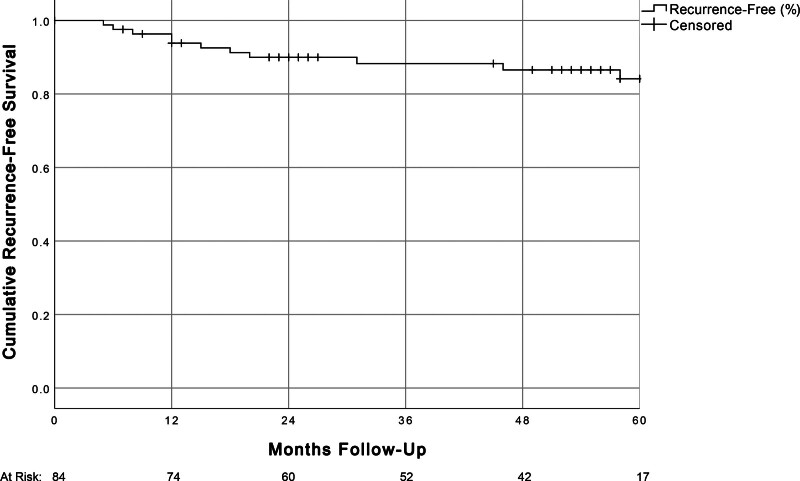
The cumulative recurrence calculated by Kaplan–Meier intention-to-treat analysis is shown in Figure 2. After 5 years, a recurrence rate of 15.9% (95% CI: 6.9–24.8) was found. Four patients (6.6%) developed a new incisional hernia recurrence between 2 and 5 years. Two of the patients were asymptomatic. Three recurrences were found by CT scanning, and one by physical examination (Table 3). None of these patients suffered from a surgical site infection postoperatively. Hernia location was umbilical in 2 patients, and supra-umbilical in 1 patient. Mean recurrence size was 11.8 cm2 (SD 15.8 cm2). Recurrences occurred in 6/12 patients with CST, and the other 6/12 without CST.
FIGURE 2.
Cumulative recurrence-free survival of patients with Phasix mesh in the intention-to-treat analysis (n = 84).
TABLE 3.
Recurrence Outcomes in Patients With Long-Term Follow-Up
| CT and PE* N (%) | Exclusively PE* N (%) | |
|---|---|---|
| CT scan | 39 (63.9) | |
| New recurrent incisional hernia | 3 (7.7%) | |
| Size of recurrence, mean (SD) (cm2) | 11.8 (15.8) | |
| Fluid collections seen around scar | 2 (5.1%) | |
| Postinterventional architectonical distortion | 19 (48.7%) | |
| Location of new recurrences | ||
| Supra-umbilical | 1 (2.6%) | |
| Umbilical | 2 (5.2%) | |
| Physical examination | 22 (36.1%) | |
| New recurrent incisional hernia | 1 (4.5%) | |
| Prior hernia recurrence present* | 5 (8.2%) | |
| Total recurrences after 5 years | 9 (14.8%) |
Hernia recurrence found during the 2-year follow-up study.
SD indicates standard deviation.
Cox regression for prediction of hernia recurrence showed no statistical significance with respect to baseline BMI (HR: 1.086 per kg/m2; 95% CI: 0.908–1.298) or incisional hernia width (HR: 0.991 per cm; 95% CI: 0.977–1.005).
In 19/39 patients (48.7%) who underwent CT, curvilinear distortion due to scar tissue was seen. Median abdominal wall pain VAS score of the scar area was 0 (range 0–2). No long-term mesh-related complications or incarcerations occurred after the 2 initial years of follow-up. Reintervention due to mesh complications or mesh explantation for chronic pain did not occur.
DISCUSSION
The present study demonstrated a cumulative incisional hernia recurrence rate in high-risk patients (VHWG grade 3 and average BMI >28) of 15.9% after 5 years by Kaplan–Meier analysis. After resorption of the mesh, 4 patients (6.6%) included in the long-term follow-up suffered from a new incisional hernia recurrence between 2 and 5 years, with 2 of these hernias being asymptomatic. Low pain scores were observed and no long-term mesh complications or reoperations for mesh complications or chronic pain occurred between 2 and 5 years after the index hernia repair.
The current study is one of the first 5-year follow-up studies investigating the recurrence rate of incisional hernia after repair with a slowly absorbable synthetic mesh with radiological follow-up. A recently published 5-year follow-up study of a cohort undergoing incisional hernia repair with Phasix mesh by Roth et al19 reported a recurrence rate of 22.0%. However, no radiological confirmation of patients without a clinical recurrence was performed. Moreover, a heterogenous pool of ventral hernia (primary and incisional) was included, and different types of mesh placement (onlay and retro-rectus) were applied. In a systematic review and pooled analysis by Mellia et al9 on outcomes of the Phasix mesh following ventral hernia repair, a recurrence rate of 28/270 (10.4%) was observed after 26.8 months, with significantly more frequent recurrences in the onlay position versus the sublay position (14.2% vs 4.4%). However, no radiological follow-up regimen was mentioned. Other cohorts examining the Phasix mesh in incisional hernia repair reported recurrence rates of 12.7%–17.9% following 3- to 5-year follow-up,20,21 yet also without radiological evaluation of recurrences. The study by Layer et al22 investigating follow-up outcomes by retrospective medical chart review mentioned a 22.2 % recurrence rate after a median of 41 months. However, this study also included different mesh placement locations (ie, intraperitoneal, onlay, and retro-rectus) and observed different recurrence rates between placement locations. The recurrence rate with retro-rectus placement amounted to 12.5%.
Incisional hernia in this study encompassed VHWG 3 hernia. Recurrence rates in literature mention 30.6% after long-term follow-up with permanent synthetic meshes in a study investigating 22 cases with complex VHWG 3 hernia.23 Another study by Brahmbhatt et al24 showed a recurrence rate of 19% after 20 months with synthetic mesh in VHWG 3 hernia. The present study showed a recurrence rate of 15.9%. However, the VHWG 3 hernia in the current study concerned a previous wound infection in 63.9% of patients and in 31.2% a presence of a stoma and violation of the gastrointestinal tract, which may have led to better outcomes compared to other VHWG 3 hernia studies. For noncomplex incisional hernias, rates of long-term recurrence with synthetic meshes have been reported in 19% in open intraperitoneal repair and 20%–32% in laparoscopic repair after 5 years.25,26 The long-term study by Burger et al27 found a recurrence rate of around 30% after 5 years. These 3 long-term studies did not use radiological follow-up to detect recurrences. Hence, these outcomes of grade 1–2 cases are lesser compared to the current 5-year recurrence rate with grade 3 patients, but notion should be made that the surgeons participating in the current study were all dedicated hernia surgeons.
In addition to the VHWG grade 3 characteristic increasing the risk for the development of incisional hernia, patients included in this cohort had a mean BMI of 28.1 kg/m2. High BMI is a risk factor for incisional hernia recurrence, and patients with a BMI higher than 27 kg/m2 appear to have a higher risk of developing incisional hernia.28
A possible hypothesis for the observed rate of recurrence after mesh degradation in this study could be that abdominal walls are subjected to the “use it or lose it” principle. As with bone tissue, gradual loading of the abdominal wall by slowly prolonged mesh degradation could potentially stimulate growth factors for aponeurotic healing and scar remodeling to a functioning abdominal wall during the period of resorption of the mesh. Another possible influential factor to the recurrence rate could be the retro-rectus dissection prior to placement of the mesh. The retro-rectus dissection could provide an additional 30%–40% of medialization during closure of the midline.29
Chronic pain after mesh implantation is an important outcome parameter. While significantly reducing the risk of hernia recurrence, permanent synthetic mesh implantation is associated with the onset of chronic pain.30 After 5 years of follow-up, mesh explantation due to chronic pain has been reported in 1% of patients treated with permanent synthetic mesh using multiple types of mesh placement (ie, onlay, sublay, and intraperitoneal) for incisional hernia repair.11 In addition, mesh size significantly influences pain outcome.31,32 The median VAS score at the site of surgery was 0 in this long-term study. This is possibly due to the resorption of the mesh.
Another important issue in incisional hernia repair is the occurrence of long-term mesh-related complications. Bowel obstruction, adhesions, chronic pain, and enterocutaneous fistula due to mesh implantation may occur up to 5 years after intraperitoneal open and laparoscopic incisional hernia mesh repair.11 Subsequently, about 4.5% of patients will require surgical treatment for a long-term mesh-related complication.11 In the study by Patel et al,33 bowel obstruction and mesh infection accounted for 14.4% and 26.4% respectively, of the 125 reoperations after 2.2 years of follow-up. While there is ample evidence for using mesh repair in incisional hernia surgery, mesh-related complications are a problem in the long term. In this regard, a resorbable mesh seems a viable alternative. In both this study and the American long-term Phasix study, no long-term mesh-related complications were found.19 The soluble Phasix mesh is an option for patients who fear the presence and possible complications of the presence of a permanent mesh.
In the present study, no distinction was made between symptomatic and asymptomatic incisional hernia. While most patients had a CT scan made, 2 of the found recurrences were asymptomatic and undetectable during physical examination. The clinical significance and surgical relevance of these asymptomatic incisional hernias are debatable.34 The patients with asymptomatic recurrences in this study were not reoperated.
The main limitation of the current study is that not all 69 patients were assessable leading to the risk of survivor bias. Furthermore, not every patient received a CT scan; therefore, the asymptomatic hernia recurrence rate might be an underestimation. Lastly, included index incisional hernias were only midsized with an average hernia defect size of 60 cm2.
In conclusion, a recurrence rate of 15.9% was observed in high-risk patients (VHWG 3 and mean BMI >28 kg/m2) after 5 years. Between 2 and 5 years, no long-term mesh complications, reinterventions due to mesh complications, or mesh explantations occurred. Four new incisional hernia recurrences were found (6.6%), of which 2 were asymptomatic. The PH4B resorbable mesh is a safe and promising device in incisional hernia repair suggesting tissue reconstruction takes place for the abdominal wall, which can avoid long-term mesh complications like pain and mesh infection. Comparative studies with large pore permanent synthetic mesh in different settings of contamination are warranted.
Footnotes
Published online 28 November 2023
This study was supported by research grants from BARD BD. The grants were used to compensate for costs made by the outpatient visit en computed tomography scans. All meshes used in the study were provided by BARD BD. BARD BD was not involved in the design, conduct, follow-up, or analysis of the 5-year follow-up study. This investigator-initiated study was funded by BD Bard for the utilization of CT scans. The funder had no part in the writing, statistics of interpretation of the data in this manuscript.
Disclosure: The authors state that they have no proprietary interest in the products named in this article.
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
REFERENCES
- 1.Dewulf M, Muysoms F, Vierendeels T, et al. Prevention of incisional hernias by prophylactic mesh-augmented reinforcement of midline laparotomies for abdominal aortic aneurysm treatment: five-year follow-up of a randomized controlled trial. Ann Surg. 2022;276:e217–e222. [DOI] [PubMed] [Google Scholar]
- 2.van Veenendaal N, Poelman MM, van den Heuvel B, et al. Patient-reported outcomes after incisional hernia repair. Hernia. 2021;25:1677–1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luijendijk RW, Hop WC, van den Tol MP, et al. A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med. 2000;343:392–398. [DOI] [PubMed] [Google Scholar]
- 4.Rogmark P, Smedberg S, Montgomery A. Long-term follow-up of retromuscular incisional hernia repairs: recurrence and quality of life. World J Surg. 2018;42:974–980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leber GE, Garb JL, Alexander AI, et al. Long-term complications associated with prosthetic repair of incisional hernias. Arch Surg. 1998;133:378–382. [DOI] [PubMed] [Google Scholar]
- 6.Christopher AN, Morris MP, Jia H, et al. Resorbable synthetic ventral hernia repair in contaminated fields: outcomes with poly-4-hydroxybutyrate mesh. Plast Reconstr Surg. 2021;148:1367–1375. [DOI] [PubMed] [Google Scholar]
- 7.Miserez M, Grass G, Weiss C, et al. ; LAPSIS Investigators. Closure of the LAPSIS trial. Br J Surg. 2010;97:1598. [DOI] [PubMed] [Google Scholar]
- 8.Miserez M, Lefering R, Famiglietti F, et al. Synthetic versus biological mesh in laparoscopic and open ventral hernia repair (LAPSIS): results of a multinational, randomized, controlled, and double-blind trial. Ann Surg. 2021;273:57–65. [DOI] [PubMed] [Google Scholar]
- 9.Mellia JA, Othman S, Naga HI, et al. Outcomes of poly-4-hydroxybutyrate mesh in ventral hernia repair: a systematic review and pooled analysis. Plast Reconstr Surg Glob Open. 2020;8:e3158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Rooijen MM, Jairam AP, Tollens T, et al. Outcomes of a new slowly resorbable biosynthetic mesh (Phasix) in potentially contaminated incisional hernias: a prospective, multi-center, single-arm trial. Int J Surg. 2020;83:31–36. [DOI] [PubMed] [Google Scholar]
- 11.Kokotovic D, Bisgaard T, Helgstrand F. Long-term recurrence and complications associated with elective incisional hernia repair. JAMA. 2016;316:1575–1582. [DOI] [PubMed] [Google Scholar]
- 12.Chelala E, Baraké H, Estievenart J, et al. Long-term outcomes of 1326 laparoscopic incisional and ventral hernia repair with the routine suturing concept: a single institution experience. Hernia. 2016;20:101–110. [DOI] [PubMed] [Google Scholar]
- 13.Van Rooijen MMJ, Tollens T, Jorgensen LN, et al. Slowly resorbable biosynthetic mesh: 2-year results in VHWG grade 3 hernia repair. Hernia. 2022;26:131–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Rooijen MMJ, Jairam AP, Tollens T, et al. A post-market, prospective, multi-center, single-arm clinical investigation of Phasix mesh for VHWG grade 3 midline incisional hernia repair: a research protocol. BMC Surg. 2018;18:104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ventral Hernia Working G, Breuing K, Butler CE, et al. Incisional ventral hernias: review of the literature and recommendations regarding the grading and technique of repair. Surgery. 2010;148:544–558. [DOI] [PubMed] [Google Scholar]
- 16.Muysoms FE, Miserez M, Berrevoet F, et al. Classification of primary and incisional abdominal wall hernias. Hernia. 2009;13:407–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gavlin A, Kierans AS, Chen J, et al. Imaging and treatment of complications of abdominal and pelvic mesh repair. Radiographics. 2020;40:432–453. [DOI] [PubMed] [Google Scholar]
- 18.Sneiders D, Yurtkap Y, Kroese LF, et al. Anatomical study comparing medialization after Rives-Stoppa, anterior component separation, and posterior component separation. Surgery. 2019;165:996–1002. [DOI] [PubMed] [Google Scholar]
- 19.Roth JS, Anthone GJ, Selzer DJ, et al. Long-Term, Prospective, multicenter study of poly-4-hydroxybutyrate mesh (Phasix Mesh) for hernia repair in cohort at risk for complication: 60-month follow-up. J Am Coll Surg. 2022;235:894–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Christopher AN, Morris MP, Patel V, et al. An evaluation of clinical and quality of life outcomes after ventral hernia repair with poly-4-hydroxybutyrate mesh. Hernia. 2021;25:717–726. [DOI] [PubMed] [Google Scholar]
- 21.Roth JS, Anthone GJ, Selzer DJ, et al. Prospective, multicenter study of P4HB (Phasix) mesh for hernia repair in cohort at risk for complications: 3-Year follow-up. Ann Med Surg (Lond). 2021;61:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Layer T, Benammi S, Dubuisson V, et al. Incisional hernia repair with a slowly absorbable P4HB mesh: what happens after the mesh disappears? A retrospective longitudinal clinical study. Hernia. 2022;27:387–394. [DOI] [PubMed] [Google Scholar]
- 23.de Vries FEE, Hodgkinson JD, Claessen JJM, et al. Long-term outcomes after contaminated complex abdominal wall reconstruction. Hernia. 2020;24:459–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brahmbhatt R, Carter SA, Hicks SC, et al. Identifying risk factors for surgical site complications after laparoscopic ventral hernia repair: evaluation of the Ventral Hernia Working Group grading system. Surg Infect (Larchmt). 2014;15:187–193. [DOI] [PubMed] [Google Scholar]
- 25.Lavanchy JL, Buff SE, Kohler A, et al. Long-term results of laparoscopic versus open intraperitoneal onlay mesh incisional hernia repair: a propensity score-matched analysis. Surg Endosc. 2019;33:225–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Juvany M, Hoyuela C, Carvajal F, et al. Long-term follow-up (at 5 years) of midline incisional hernia repairs using a primary closure and prosthetic onlay technique: recurrence and quality of life. Hernia. 2018;22:319–324. [DOI] [PubMed] [Google Scholar]
- 27.Burger JW, Luijendijk RW, Hop WC, et al. Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg. 2004;240:578–83; discussion 583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jairam AP, Timmermans L, Eker HH, et al. Prevention of incisional hernia with prophylactic onlay and sublay mesh reinforcement versus primary suture only in midline laparotomies (PRIMA): 2-year follow-up of a multicentre, double-blind, randomised controlled trial. Lancet. 2017;390:567–576. [DOI] [PubMed] [Google Scholar]
- 29.Sneiders D, de Smet GHJ, den Hartog F, et al. Medialization after combined anterior and posterior component separation in giant incisional hernia surgery, an anatomical study. Surgery. 2021;170:1749–1757. [DOI] [PubMed] [Google Scholar]
- 30.Mathes T, Walgenbach M, Siegel R. Suture versus mesh repair in primary and incisional ventral hernias: a systematic review and meta-analysis. World J Surg. 2016;40:826–835. [DOI] [PubMed] [Google Scholar]
- 31.Kockerling F, Simon T, Hukauf M, et al. The importance of registries in the postmarketing surveillance of surgical meshes. Ann Surg. 2018;268:1097–1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hoffmann H, Kockerling F, Adolf D, et al. Analysis of 4,015 recurrent incisional hernia repairs from the herniamed registry: risk factors and outcomes. Hernia. 2021;25:61–75. [DOI] [PubMed] [Google Scholar]
- 33.Patel PP, Love MW, Ewing JA, et al. Risks of subsequent abdominal operations after laparoscopic ventral hernia repair. Surg Endosc. 2017;31:823–828. [DOI] [PubMed] [Google Scholar]
- 34.de Smet GHJ, Sneiders D, Yurtkap Y, et al. ; Hernia-Club Members. Functional outcomes in symptomatic versus asymptomatic patients undergoing incisional hernia repair: replacing one problem with another? A prospective cohort study in 1312 patients. Int J Surg. 2020;82:76–84. [DOI] [PubMed] [Google Scholar]