Abstract
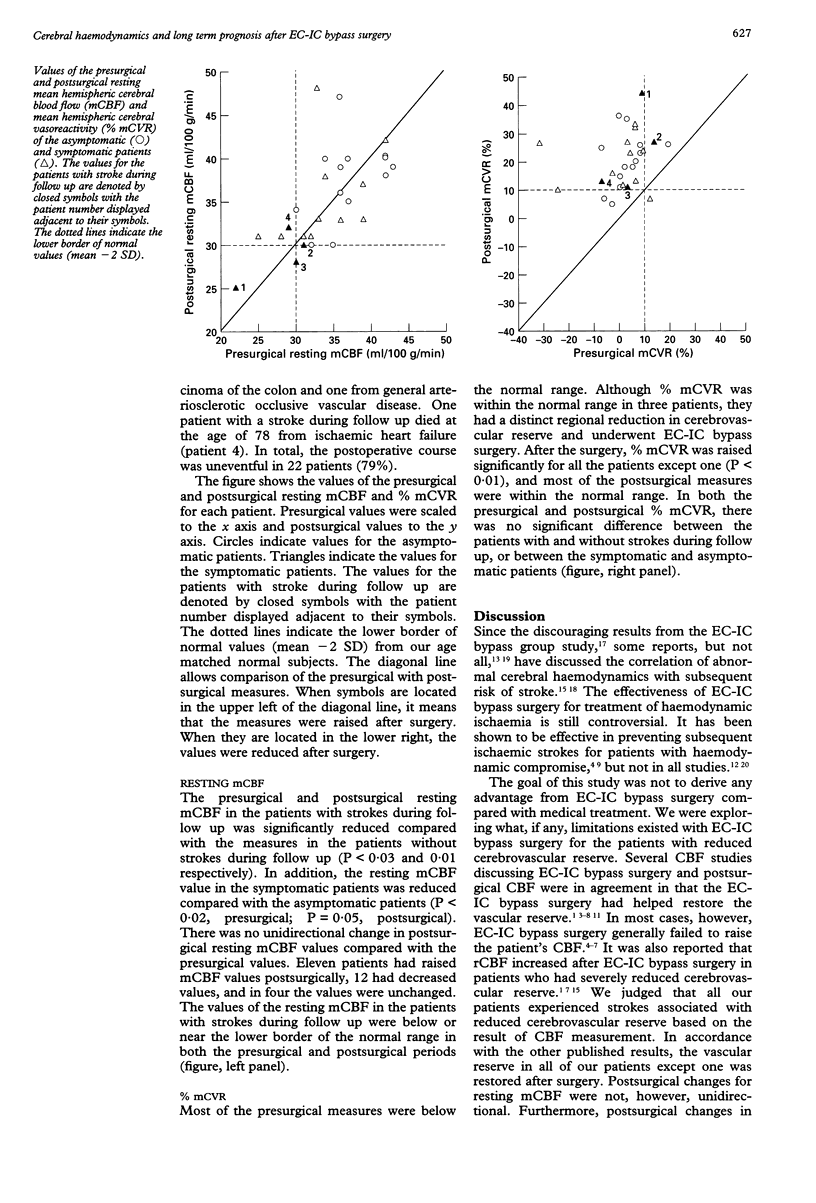
The effectiveness of extracranial-intracranial arterial (EC-IC) bypass surgery for haemodynamic stroke remains controversial. In this study correlation of presurgical and postsurgical cerebral haemodynamics with long term prognosis was evaluated. Twenty eight patients (25 men, three women: mean age 61.4 (SD 8.2) years) with reduced cerebrovascular reserve due to steno-occlusive cerebral vascular disease formed the study group. Measurement of mean hemispheric cerebral blood flow (mCBF) and the cerebral vasodilatory capacity (% mCVR) with an intravenous acetazolamide injection were performed by a xenon-133 inhalation method and SPECT. Patients were treated with EC-IC bypass surgery and measurements of mCBF and % mCVR were made again about one month after surgery. The patients were then observed for a long period (range 27-115 months). During the observation period, four patients experienced subsequent ischaemic strokes. The presurgical and the postsurgical resting mCBF for the affected hemisphere were significantly reduced in the patients with strokes during follow up compared with the values in patients without strokes during follow up (P < 0.03 and 0.01 respectively). The % mCVR of the affected hemisphere was significantly raised after surgery in all patients except one (P < 0.01). The postsurgical change in resting mCBF was not unidirectional. In conclusion, resting mCBF was unchanged and % mCVR was improved after EC-IC bypass surgery in patients with reduced cerebrovascular reserve. The group of patients with a reduced presurgical and postsurgical resting mCBF continue to be a high risk group for subsequent ischaemic stroke seen after EC-IC bypass surgery.
Full text
PDF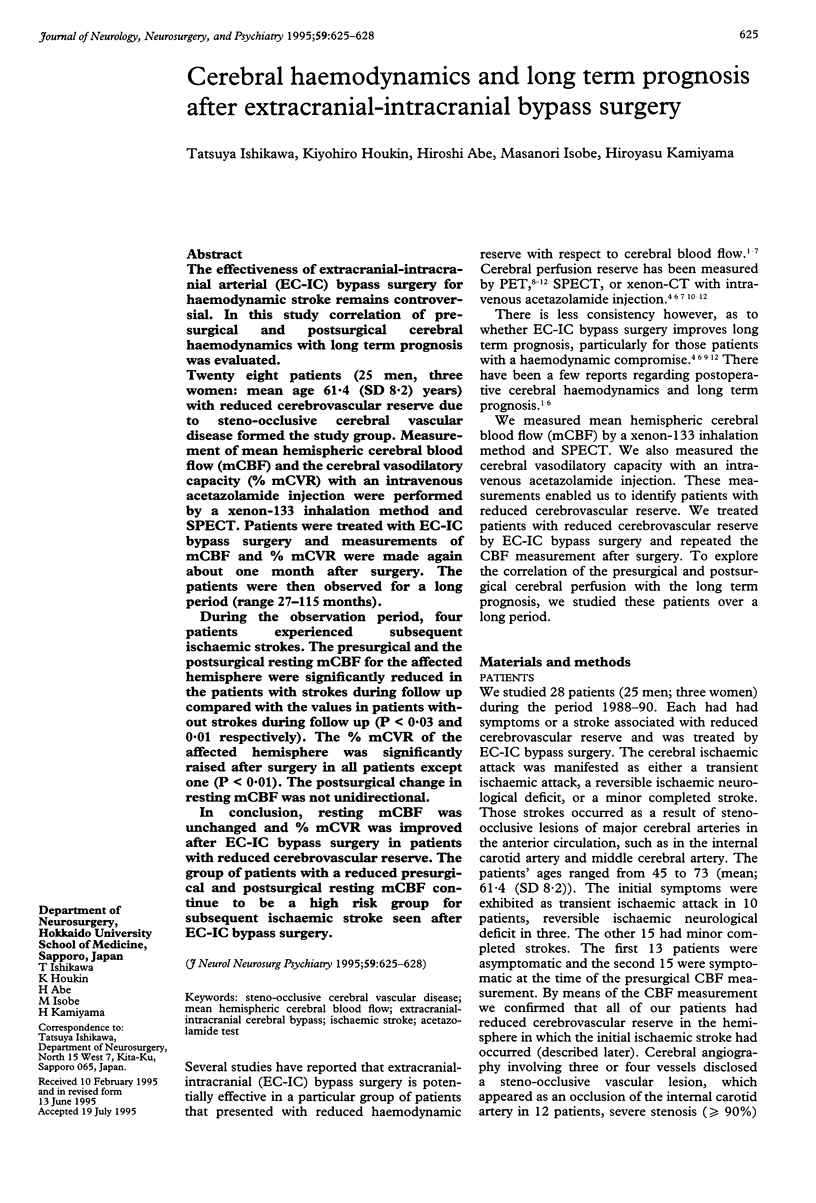

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anderson D. E., McLane M. P., Reichman O. H., Origitano T. C. Improved cerebral blood flow and CO2 reactivity after microvascular anastomosis in patients at high risk for recurrent stroke. Neurosurgery. 1992 Jul;31(1):26–34. doi: 10.1227/00006123-199207000-00005. [DOI] [PubMed] [Google Scholar]
- Baron J. C., Bousser M. G., Rey A., Guillard A., Comar D., Castaigne P. Reversal of focal "misery-perfusion syndrome" by extra-intracranial arterial bypass in hemodynamic cerebral ischemia. A case study with 15O positron emission tomography. Stroke. 1981 Jul-Aug;12(4):454–459. doi: 10.1161/01.str.12.4.454. [DOI] [PubMed] [Google Scholar]
- Gibbs J. M., Wise R. J., Thomas D. J., Mansfield A. O., Russell R. W. Cerebral haemodynamic changes after extracranial-intracranial bypass surgery. J Neurol Neurosurg Psychiatry. 1987 Feb;50(2):140–150. doi: 10.1136/jnnp.50.2.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishikawa T., Yasui N., Suzuki A., Hadeishi H., Shishido F., Uemura K. STA-MCA bypass surgery for internal carotid artery occlusion--comparative follow-up study. Neurol Med Chir (Tokyo) 1992 Jan;32(1):5–9. doi: 10.2176/nmc.32.5. [DOI] [PubMed] [Google Scholar]
- Kanno I., Uemura K., Higano S., Murakami M., Iida H., Miura S., Shishido F., Inugami A., Sayama I. Oxygen extraction fraction at maximally vasodilated tissue in the ischemic brain estimated from the regional CO2 responsiveness measured by positron emission tomography. J Cereb Blood Flow Metab. 1988 Apr;8(2):227–235. doi: 10.1038/jcbfm.1988.53. [DOI] [PubMed] [Google Scholar]
- Kleiser B., Widder B. Course of carotid artery occlusions with impaired cerebrovascular reactivity. Stroke. 1992 Feb;23(2):171–174. doi: 10.1161/01.str.23.2.171. [DOI] [PubMed] [Google Scholar]
- Kuroda S., Kamiyama H., Abe H., Houkin K., Isobe M., Mitsumori K. Acetazolamide test in detecting reduced cerebral perfusion reserve and predicting long-term prognosis in patients with internal carotid artery occlusion. Neurosurgery. 1993 Jun;32(6):912–919. doi: 10.1227/00006123-199306000-00005. [DOI] [PubMed] [Google Scholar]
- Leblanc R., Tyler J. L., Mohr G., Meyer E., Diksic M., Yamamoto L., Taylor L., Gauthier S., Hakim A. Hemodynamic and metabolic effects of cerebral revascularization. J Neurosurg. 1987 Apr;66(4):529–535. doi: 10.3171/jns.1987.66.4.0529. [DOI] [PubMed] [Google Scholar]
- Powers W. J., Martin W. R., Herscovitch P., Raichle M. E., Grubb R. L., Jr Extracranial-intracranial bypass surgery: hemodynamic and metabolic effects. Neurology. 1984 Sep;34(9):1168–1174. doi: 10.1212/wnl.34.9.1168. [DOI] [PubMed] [Google Scholar]
- Powers W. J., Tempel L. W., Grubb R. L., Jr Influence of cerebral hemodynamics on stroke risk: one-year follow-up of 30 medically treated patients. Ann Neurol. 1989 Apr;25(4):325–330. doi: 10.1002/ana.410250403. [DOI] [PubMed] [Google Scholar]
- Schmiedek P., Piepgras A., Leinsinger G., Kirsch C. M., Einhüpl K. Improvement of cerebrovascular reserve capacity by EC-IC arterial bypass surgery in patients with ICA occlusion and hemodynamic cerebral ischemia. J Neurosurg. 1994 Aug;81(2):236–244. doi: 10.3171/jns.1994.81.2.0236. [DOI] [PubMed] [Google Scholar]
- Vorstrup S., Brun B., Lassen N. A. Evaluation of the cerebral vasodilatory capacity by the acetazolamide test before EC-IC bypass surgery in patients with occlusion of the internal carotid artery. Stroke. 1986 Nov-Dec;17(6):1291–1298. doi: 10.1161/01.str.17.6.1291. [DOI] [PubMed] [Google Scholar]
- Vorstrup S., Henriksen L., Paulson O. B. Effect of acetazolamide on cerebral blood flow and cerebral metabolic rate for oxygen. J Clin Invest. 1984 Nov;74(5):1634–1639. doi: 10.1172/JCI111579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yonas H., Smith H. A., Durham S. R., Pentheny S. L., Johnson D. W. Increased stroke risk predicted by compromised cerebral blood flow reactivity. J Neurosurg. 1993 Oct;79(4):483–489. doi: 10.3171/jns.1993.79.4.0483. [DOI] [PubMed] [Google Scholar]


