Abstract
American Indians and Alaska Natives suffer from disproportionately high rates of chronic mental and physical health conditions. These health inequities are linked to colonization and its downstream consequences. Most of the American Indian and Alaska Native health inequities research uses a deficit framework, failing to acknowledge the resilience of American Indian and Alaska Native people despite challenging historical and current contexts. This scoping review is based on a conceptual model which acknowledges the context of colonization and its consequences (psychological and health risk factors). However, rather than focusing on health risk, we focus on protective factors across three identified domains (social, psychological, and cultural/spiritual), and summarize documented relationships between these resilience factors and health outcomes. Based on the scoping review of the literature, we note gaps in extant knowledge and recommend future directions. The findings summarized here can be used to inform and shape future interventions which aim to optimize health and well-being in American Indian and Alaska Native peoples.
Despite decades of research focused on American Indian and Alaska Native health inequities, these groups continue to have a reduced life expectancy compared to other racial and ethnic groups and are disproportionately affected by chronic diseases (Espey et al., 2014; Gone & Trimble, 2012). These health inequities are a product of colonization by European countries starting in the 16th century and the collective traumas and atrocities that were inflicted on these groups (Gone et al., 2019). American Indians and Alaska Natives have endured a history of ethnic and cultural genocide (Heart, 2011) including massacres of communities, forced relocation, genocidal policies, forcibly removing children from their families and placing them into boarding schools, and loss of culture and language due to government enforced prohibition (Thornton, 1997). Beyond the immediate loss of life and land, colonization contributed to many downstream outcomes with important implications for health. Specifically, colonization is linked to historical trauma, or “the cumulative emotional and psychological wounding over the lifespan and across generations, emanating from massive group trauma” (Brave Heart, 2003).
For American Indians and Alaska Natives, historical trauma manifests in high incidence of future trauma exposure (Beals et al., 2002; Manson et al., 2005; Robin et al., 1997), intergenerational trauma (Cromer et al., 2018) and is further compounded by experiences of ongoing racism and discrimination (Akinade et al., 2023; Herron & Venner, 2022; Solomon et al., 2022). Historical trauma is also related to a constellation of psychological, biological, physiological, and behavioral outcomes, named as the Historical Trauma Response (HTR) (Brave Heart, 1998), which contributes to inequities in mental and physical health (Gone et al., 2019, John-Henderson & Ginty, 2020; John-Henderson et al., 2020; John-Henderson et al., 2022a; John-Henderson et al., 2022b). Based on these relationships, health interventions rooted in culture have been suggested and utilized to address the health consequences of historical trauma (Gone, 2013; Gone & Calf Looking, 2011; Pomerville & Gone, 2019).
Despite an environment and context with potentially elevated levels of stress and adversity, American Indians and Alaska Natives demonstrate tremendous resilience (Hartmann et al., 2019; Oré et al., 2016; Reinschmidt et al., 2016; Teufel-Shone et al., 2018). Resilience has been previously defined as “the capacity of a system to adapt successfully to disturbances that threaten the viability, function or development of the system.” (Masten, 2014). This definition is applicable to a wide range of dynamic systems, including biological systems within the human body (e.g., cardiovascular system), individuals, communities, and societies. (Masten, Lucke, Nelson, Stallworthy, 2021). Resilience has been central to the survival of American Indian and Alaska Native people, and this resilience has been demonstrated across the lifespan (Oré et al., 2016), including youth (Gilgun, 2002; Henson et al., 2017; Lafromboise et al., 2006; Stumblingbear-Riddle & Romans, 2012), young adults (Nikolaus et al., 2021) and older adults (Kahn et al., 2016; Reinschmidt et al., 2016). Although the resilience observed in these groups is a response to challenges rooted in long and ongoing history of cultural loss and degradation, and continued discrimination, what remains less clear are the multi-level factors underpinning resilience, and how these factors relate to positive physical and mental health outcomes. Over the past 3 decades, there has been a growing movement towards strength-based approaches to understanding health and resilience across racial and ethnic groups (Tse et al., 2016). While resilience was once conceived as something remarkable and only observed in some individuals, it is now seen as something that is accessible and inherent to basic human adaptational systems (Masten, 2001). As such, identification of resilience factors linked to positive health is an important step in addressing persistent health inequities.
However, to date, by and large, the narrative of the American Indian and Alaska Native health inequities literature has centered on risk factors, and more specifically on biological and behavioral risk factors. This deficit approach to research can reinforce feelings of hopelessness and self-blame (Wood et al., 2018). Furthermore, there is limited incorporation of Indigenous perspectives and voices in this work, which can lead to a paternalistic narrative focusing exclusively on weaknesses (O’Neill et al., 1998). Emphasizing risk factors rather than resilience factors fails to acknowledge the tremendous resilience of American Indian and Alaska Native people which was acknowledged here previously. As stated by James Clairmont, a Lakota spiritual elder, the concept of resilience is inherent to tribal culture, “The closest translation of ‘resilience’ is a sacred word that means ‘resistance’…. resisting bad thoughts, bad behaviors. We accept what life gives us, good and bad, as gifts from the Creator. We try to get through hard times, stressful times, with a good heart. The gift [of adversity] is the lesson we learn from overcoming it.” (Graham, 2001, p. 1).
Since American Indian and Alaska Native health inequities are a product of current environments and circumstances, along with the stress and trauma associated with historical and current atrocities and hardships, research which aims to understand and address these health inequities without integration of these factors and experiences is problematic and incomplete (de Leeuw et al., 2012). The importance of historical and current context in this work is the primary reason for focusing exclusively on American Indians and Alaska Natives in the current work. While there are certainly shared experiences and cultural values between these groups and other Indigenous groups, we chose to focus this effort exclusively on these two groups to maximize shared context and histories. Furthermore, in prior research it is commonplace for American Indians and Alaska Natives to be grouped together in analyses (Godfrey et al, 2022; Henson et al., 2017; Kruse et al., 2022).
There are existing reviews which summarize the work on resilience in Indigenous youth (I.e., American Indians and Alaska Natives) (Heid et al., 2022; Wexler, 2014), in Canadian Indigenous youth (Toombs, Kowatch, & Mushquash, 2016), and in Arctic indigenous youth (Ulturgasheva et al., 2014). However, the focus of these reviews is on the factors that promote general resilience in these groups (I.e., strength, purpose fortitude), with less emphasis on how resilience factors are linked to downstream health outcomes, and with focus on one specific age group. A previous review focused on identifying themes of American Indian and Alaska Native resilience highlighted the needs for more efforts to link resilience factors with health outcomes to maximize the efficacy of health promotion efforts for these populations (Teufel-Shone et al., 2018).
The primary purpose of the current review is to synthesize research documenting links between American Indian and Alaska Native resilience factors and health outcomes so that these findings can be useful towards future health promotion efforts. As a construct, resilience has been defined in many ways, however, for the purpose of this review, resilience is conceptualized according to the following definition, “the process of harnessing biological, psychosocial, structural and cultural resources to sustain well-being,” (Panter-Brick & Leckman, 2013). While well-being can also be defined in many ways, in the current scoping review, we focus on mental and physical health outcomes as indices of well-being. The conceptual model for this review is based on prior theoretical work and is depicted in Figure 1. To begin with, the model recognizes the context of colonization and downstream consequences of colonization including historical trauma, childhood trauma, psychological stress, and cultural degradation and discrimination. While our model acknowledges the significant body of work indicating a relationship between the consequences of colonization and poor health, here we place emphasis on the resilience factors which are linked to positive health outcomes. We also include arrows in our model stemming from the consequences of colonization to the resilience factors, because although this is not the focus of the current review, we posit that these adverse and challenging experiences may contribute to or promote these resilience factors.
Figure 1.
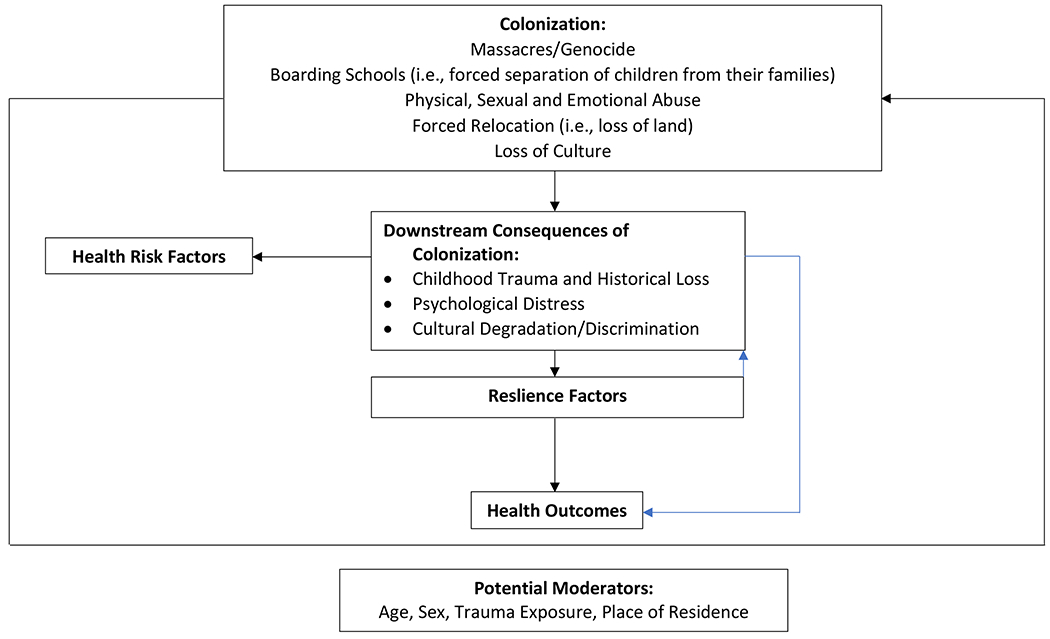
Conceptual model including context of colonization and downstream consequences and related health risk factors.
In contrast to dominant notions of health, Indigenous models of health are holistic and emphasize the interconnectedness of multiple domains of one’s life and experiences (Ahenakew, 2011). In line with this approach to health, in the current scoping review, we will include resilience factors across multiple domains which are linked to health outcomes. These domains will be identified based on the empirical evidence that emerges in the scoping review. As depicted in our model, these resilience domains could have direct effects on health, or may affect health indirectly, by moderating the degree to which the consequences of colonization negatively impact health resilience.
Once the domains of resilience are identified based on the review of the existing literature, we will summarize the existing literature for each domain. Within each domain, we will report findings across developmental periods if applicable. In our figure, we also note that age, biological sex, trauma exposure, and place of residence (i.e., tribal reservation vs. urban residence) could act as moderators of the proposed model. Some of these moderators are considered in the research included in this review, while others should be explored in future research. Finally, based on the synthesized literature, we propose future directions for promoting health and wellness and improved understanding the mechanisms through which resilience factors may contribute to American Indian and Alaska Native health.
Method
We conducted a scoping review following the methods and approach outlined by Arksey & O’Malley (2005) in their methodological paper on scoping studies. Scoping reviews are utilized to examine the range of research on a given topic, to synthesize and share findings, and to identify current gaps in the literature (Arksey & O’Malley, 2005). In the current scoping review, the goal was to answer the following research question: “What are the identified resilience factors linked to positive health outcomes in American Indians and Alaska Natives?” Next, we identified relevant studies using a variety of approaches. In April of 2023, we used electronic databases PUBMED-MEdline and Psycinfo. Different combinations of search terms were utilized including protective factors, resilience, health, health outcomes, American Indians, health resilience, health disparities, health inequities, inequity, disparity, mental health, physical health, social, cultural, socio-cultural, psychological, biopsychosocial, and spiritual. We searched for articles with these terms in the subject heading, title, abstract, or keyword section. We also reviewed reference lists from existing reviews of American Indian and Alaska Native health to identify additional articles. From these searches, a total of 71 articles emerged ranging from the year 1997-2023. The authors reviewed the collection of articles collaboratively and excluded any articles that were theoretical (i.e., lacking empirical data), articles that used a deficit approach, and articles that did not focus exclusively on American Indian or Alaska Native samples or communities. After this process, 34 articles remained, and three health protective domains emerged: Social Protective Factors, Psychological Factors, and Cultural/Spiritual Factors. The findings from work within each of these domains are presented below.
Results
Social Protective Factors (N=13)
The link between social factors, experiences, environments and health has been well-documented in many racial and ethnic groups. In general, while social connectedness is linked to positive health outcomes (Barger, 2013; Berkman et al., 2000; Fothergill et al., 2011), social isolation relates to compromised health and mortality (Holt-Lunstad et al., 2015). Qualitative research in American Indian and Alaska Native communities indicates that families and the individuals who make up their social network are important sources of strength and direction (McMahon, Kenyon & Carter, 2013; In line with these relationships, there is a growing body of work specific to American Indians, indicating that social connectedness is linked to positive mental and physical health which we summarize here.
Social Protective Factors and Mental Health Outcomes
Depression and anxiety are two mental health outcomes that are closely tied to the psychological traumas and stressors which contribute to American Indian health inequities (Brockie et al., 2015; Kenney & Singh, 2016; Warne et al., 2017). Furthermore, depression and anxiety are linked to suicide in the general population (American Association of Suicidology, 2010), which is a leading cause of early mortality in American Indians and Alaska Natives (Indian Health Services, 2023). Similarly, American Indians diagnosed with anxiety and depressive disorders are twice as likely to experience a substance use disorder (Riekmann et al., 2012), and are at greater risk for hypertension (Ho et al., 2015). These links between depression and anxiety and the primary causes of early mortality for American Indians and Alaska Natives provide a strong impetus to understand the resilience factors which offset risk for depression and anxiety, as well as poor mental health more broadly.
In one qualitative study, American Indian youth were asked to speak about both the challenges and positive qualities they associated with living on a tribal reservation. Many of the American Indian youth who participated in the study indicated that living on a reservation made it easier for them to access social support and allowed them to develop and nurture intergenerational relationships (Wood et al., 2018). In turn, social support and positive relationships across generations allow for a sense of safety and well-being. In a separate study, social connectedness was negatively related to symptoms of depression and anxiety in Blackfeet American Indian adults (John-Henderson et al., 2020b). Finally, one study reported that American Indian and Alaska Native youth who reported higher levels of family cohesion reported lower levels of symptoms of depression and anxiety (Palimaru et al., 2022).
Social Protective Factors and Suicide Behavior
In other racial/ethnic groups, social relationships inform suicide risk (Chang et al., 2017; Van Meter et al., 2019). In a sample of American Indian/Alaska Native adolescents, the relationship between social relationships and suicide risk was gender specific. Specifically, for girls, positive relationships with adults at home, at school and in the community were independently associated with lower-suicide-attempt prevalence. In contrast, among boys, only positive relationships with adults at home showed an association with lower-suicide attempt prevalence (FitzGerald et al., 2017).
A separate but related study investigated whether positive relationships with adults at home, in school, and in the community are protective for suicide among American Indian/Alaska Native, Hispanic, and non-Hispanic White adolescents. While positive relationships with adults in the home and in the community were protective for Hispanic and non-Hispanic White adolescents, only positive relationships with adults in the home were protective for American Indian adolescents (Fullerton et al., 2019). A related study found that there were gender differences in the types of support were the most protective with regards to suicide risk for American Indian and Alaska Native youth. Specifically, for females, community support was the most protective for having seriously thought about committing suicide, while family support was associated with having made a suicide plan and having attempted suicide. For males, school support was the most protective for having thought about suicide, having made a suicide plan and for having attempted suicide (Parshall, Qedan, Espinoza & English, 2023). Finally, another study reported that general social support availability appears to affect risk for suicide in American Indian high school students, with those students who reported high levels of social support being less likely to report attempting suicide (Agyemang et al., 2022). Overall, these findings indicate that there are several social protective factors which are important in reducing the risk for suicidal behavior in American Indian and Alaska Native youth.
Social Protective Factors and General Health Resilience
With regards to health resilience more generally, one study utilized a community-engaged approach to identify strategies used by American Indians to promote and maintain wellness and good health. The study included 39 American Indian adults who self-identified as resilient. The qualitative data indicated that social relationships were linked to wellness and survival. Participants spoke about the important role of supportive family members and people in their extended social networks in successfully making healthy changes. They also spoke about how the desire to serve as a role model for healthy behavior acted as an impetus for improving their own health. Finally, participants spoke about how being around others who were engaging in healthy behaviors made them more likely to do the same (Hulen et al., 2019).
Social Protective Factors and Substance Use
Recreational alcohol and other drug use was not prevalent in American Indians prior to colonization. The historical traumas which forced relocations and placement in boarding schools, as well as laws leading to cultural degradation and limited use of spiritual practices disrupted the well-being of American Indian communities and contributed to many of the currently observed health inequities, including substance use (Brave Heart 2005; Duran & Duran, 1995). There are known biological, psychological, and social risk and protective factors for addiction (Skewes & Gonzales, 2013). Understanding protective factors is critical to reducing risk for substance use disorders (SUDs).
Previous literature focusing on substance use in American Indian youth indicates that the family environment and family relationships are important in reducing risk for SUD. Social support, supportive family relationships, and positive social interactions have also been found to be protective factors for SUD in American Indian youth, in part by helping them make healthier decisions regarding substance use (Baldwin et al., 2011).
As noted above, social support appears to be a health resilience factor for American Indian youth in the context of SUD. Social support can be expressed in many ways, and one expression of support which appears to promote health resilience related to SUD for American Indian adults is the expression of love. A mixed-methods study collected qualitative and quantitative study collected data from two indigenous tribes measured the amount of love, verbal and physical affection available in one’s childhood environment and in their current family environment. The study found that higher levels of love and verbal and physical affection in both one’s childhood environment and current family environment was negatively linked to alcohol abuse symptoms (McKinley & Scarnato, 2021)
Social Protective Factors and Health in American Indian adults who experienced Childhood Trauma
As with other racial and ethnic groups, a positive relationship between number of adverse childhood experiences (ACEs) and depressive symptoms has been found in American Indian adults (McKinley et al., 2021; Roh et al., 2015). However, perceived social support was found to alleviate depressive symptoms for those adults reporting ACEs (Roh et al., 2015). Furthermore, in contrast to ACEs which was positively related to depressive and anxiety symptoms in American Indian adults, social support drawn from both the family and larger community was negatively related to levels of anxiety (McKinley et al., 2021).
Existing data also highlights community ties and connection as factors capable of promoting positive health outcomes specifically for American Indians who have experienced childhood trauma. One study found that the relationship between childhood trauma and elevated levels of immune system inflammation (i.e., a marker of increased risk for inflammatory diseases) which is observed in other racial and ethnic groups, was not evident in Blackfeet American Indian adults who reported high levels of connectedness to their community as adults (John-Henderson et al., 2020). These findings indicate that community connectedness may promote physiological resilience in adulthood particularly for those adults who experienced trauma during childhood. Likewise, the presence or availability of social support related to improved mental and physical health for American Indian adults with Type 2 Diabetes who reported adverse childhood experiences (Brockie et al., 2018). It is posited that social support and social connectedness may allow individuals who experienced childhood trauma to acquire positive coping strategies through learning from others and that this knowledge may offer protection from the negative effects of ACEs.
Psychological Protective Factors (N=5)
Psychological resilience or the ability to adapt in the face of adversity (Ong et al., 2006) has been negatively correlated with a range of poor mental and physical health conditions including increased depressive symptomatology, post-traumatic stress disorder and physical disability (Burns & Anstey, 2010; Connor et al., 2003; Hardy et al., 2004; Mehta et al., 2008). Based on these findings, the relationship between psychological resilience and mental and physical health was investigated in a sample of older American Indian adults (Schure et al., 2013). In this study, independent of demographics and other health measures, psychological resilience was related to health resilience, with those American Indian adults who reported higher levels of psychological resilience reporting lower levels of depressive symptomatology and chronic pain, and higher levels of both mental and physical health (Schure et al., 2013).
Another psychological factor which relates to stress resilience is personal-mastery-or personal sense of control over goal achievement (Pearlin et al., 1981). American Indian and Alaska Native culture is founded on collectivist principles and emphasizes reliance on one’s social group (Barnhardt & Kalagwey, 2005; Lafromboise, 1992). Based on the collectivist nature of American Indian culture (Lafromboise, 1992), investigators tested whether communal-mastery, or a sense of shared efficacy, was more related to emotional outcomes including depressive mood relative to personal mastery in a sample of American Indian women. In this study, when faced with high stress circumstances, women who were high in communal-mastery experienced a less pronounced increase in depressive mood, compared to women who were low in communal mastery (Hobfoll et al., 2002).
While it has long been widely accepted that emotions are implicated in both mental and physical health (Mayne, 2001), and while emotions are integrated into indigenous models of health (Ahenakew, 2011), empirical data to support the role of emotions in American Indian health disparities has only recently begun to accumulate. Emotion regulation refers to efforts to influence which emotions we have, when we have them, and how we experience and express these emotions (Gross, 1998). In other racial and ethnic groups, a relationship between emotion regulation strategy use and mental and physical health has been well-documented (Berking & Wupperman, 2012; Kraiss et al., 2020; Low et al., 2021). Until recently, the role of emotion regulation in informing physical and mental health outcomes in American Indians had not been investigated. However, a new and growing body of work highlights links between emotion regulation and health outcomes in American Indians, indicating that emotion regulation may be a source of resilience. In one prospective study, emotion regulation strategies were found to predict Post-Traumatic Stress Symptoms (PTSS) in American Indian adults. Specifically, higher use of emotion reappraisal, or changing the meaning of emotional events to alter emotional experience, predicted lower PTSS (Tyra et al., 2021). The findings here indicate that use of emotion reappraisal may be a source of resilience in the context of a life event and may promote positive mental health outcomes when facing a stressor.
A separate study also documented a relationship between emotion regulation and mental health relevant outcomes in the context of the COVID-19 pandemic. This study reported that American Indian adults who experienced childhood trauma who used expressive suppression infrequently, had less of an increase in psychological stress and symptoms of depression compared to those American Indian adults who had similar levels of trauma but used expressive suppression more frequently (McCullen et al., 2022). Finally, one study found a relationship between reported use of emotion regulation strategies and markers linked to risk for cardiovascular disease in a sample of American Indian adults living on a tribal reservation. This study reported that lower use of expressive suppression was associated with lower ambulatory pulse rate, and lower ambulatory systolic and diastolic blood pressure as monitored over a 7-day period (Tyra et al., 2023).
Cultural and Spiritual Protective Factors (N=16)
A recurring factor in resilience research in American Indian and Alaska Native peoples is engagement in traditional cultural and spiritual practices (Allen et al., 2022; Gone & Calf Looking, 2011; Gonzalez et al., 2022; Stumblingbear-Riddle & Romans, 2012; Wexler, 2014). The indigenous stress coping model features traditional cultural and spiritual practices as a key moderator of the relationship between trauma (I.e., childhood trauma, historical, and intergenerational) and negative health outcomes (I.e., physical and mental) and substance misuse (Walters & Simoni, 2002). Furthermore, recent work has supported the conceptualization of traditional culture as a social determinant of mental health and well-being (Masotti et al., 2020). There are many facets of traditional cultural practice which may benefit health (i.e., protective factors, resilience factors). These include family and community support, spirituality, traditional healing identity and ceremonial practices (Fleming & Ledogar, 2008; Kirmayer et al., 2011; LaFromboise et al., 2006).
Cultural Factors and Health
Recent work has demonstrated that despite ongoing harms of colonization on American Indian and Alaska Native peoples, youth still hold perspective of hope and see reservations as places of wellness and health emphasizing the role of culture in youth resilience (Wood et al., 2018). In one study, in a sample of American Indian youth living on or near reservations, engagement and in traditional cultural practices was linked to higher levels of self-esteem (Stumblingbear-Riddle & Romans, 2012), and self-esteem has been found to prospectively predict depression in other racial and ethnic groups (Sowislo & Orth, 2013). In a separate sample of American Indian youth living in an American Indian community, those youth who felt curious about their traditional culture, ate nutritious foods more frequently. Similarly, those American Indian youth who had integrated American Indian practices into their lives, also ate nutritious foods more frequently (Lee, 2011).
A separate study developed a culturally grounded after school program which focused on local cultural values and organized activities guided by local cultural practitioners. After 10 sessions of the program, urban American Indian youth reported higher levels of self-esteem and increased ability to build general resilience, two outcomes with likely implications for mental and physical health resilience (Hunter et al., 2022).
The “Remember the Removal” Program provides an example of how culture, history and language can provide comprehensive health benefits to American Indian young adults. This program retraces the Trail of tears with the goal of increasing Cherokee knowledge, culture, and language. Thirty Cherokee participants (mainly young adults) completed the program and completed measures of physical, mental, spiritual and cultural health and well-being at the start of the program, at the end of the program, and again 6-months after completion of the program. At the end of the program, participants had improved diet and exercise, improved mental health, and improved social and cultural connection. At the 6-month follow-up, participants still exhibited lower levels of depression, anger, and stronger Cherokee Identity (Lewis et al., 2022).
Among American Indian adults, traditional cultural engagement has been associated with positive mental health (Kading et al., 2015) reduced mental health problems and trauma (i.e., historical and personal) related difficulties (Bear et al., 2018; Shea et al., 2019; Wexler, 2014; Wolsko et al., 2007). In addition to engaging with culture, cultural connectedness has also been investigated as a resilience factor. In one study, American Indian adults were administered the Cultural Connectedness scale, which measures connectedness across three subscales: i) identity, ii) traditions, and iii) spirituality (Snowshoe et al., 2015) and a measure of mental health and well-being. The findings indicated a positive link between cultural connectedness and mental health and well-being, with American Indian adults who reported feeling more connected to Native culture also reporting better mental-health and well-being (Masotti et al., 2020).
Related to culture, there is growing interest in whether residing on a tribal reservation confers health benefits. While residing on a tribal reservation is associated with increased risks for some health-compromising behaviors (Sarche & Spicer, 2008), it is suggested that tribal reservations can make it easier for American Indians to regularly engage in traditional ways of life, protect their cultural values, and use their tribal languages. As a result, these reservations may help to preserve American Indian identity (Thornton, 1997). One study utilized data from two American Indian tribes to investigate whether the length of time one spends living on a tribal reservation relates to levels of psychological distress. They found that it in both tribes, American Indian adults who had spent most of their lives living on a reservation had lower levels of psychological distress compared to those American Indian adults who spent portions of their live off the reservation (Huyser et al., 2018), suggesting that residing on a tribal reservation may confer benefits for health.
Similar relationships between culture and health are observed in American Indian elders and older adults. Specifically, American Indian elders have demonstrated resilience to mental health difficulties after accounting for demographics and other health measures (Schure, 2013). This resilience has been inextricably linked to traditional cultural connection (Grandbois & Sanders, 2009). Engagement in traditional culture among aging American Indians has also been inversely associated with memory problems (Adamsen et al., 2021).
As noted previously, American Indians endure a disproportionately large burden of SUD (Beals, 2005; Walls et al., 2021) highlighting the necessity of leveraging the strengths and uplifting communities to address this burden through culturally grounded intervention and prevention efforts (Soto et al., 2022). In addition to the previously noted links between Native culture and positive health outcomes, extant work indicates traditional cultural engagement and spirituality play a critical role in alcohol cessation (Gone & Calf Looking, 2011; Stone et al., 2006). Recent work has further supported traditional cultural engagement as protective against substance misuse (Brown et al., 2022; Hirchak et al., 2021) and current efforts are seeking to establish the efficacy of traditional cultural engagement as substance use prevention among American Indian youth (D’Amico et al., 2021).
Overall, the existing work on cultural and spiritual protective factors highlights their central role in promoting positive outcomes for American Indians and Alaska Natives across the lifespan and represent a promising avenue for future health equity research and intervention development.
Discussion
The purpose of the current work was to provide a scoping review of the existing literature on resilience factors and health outcomes in American Indians and Alaska Native peoples. This project was motivated by a recognition for the need to continue to shift focus of American Indian and Alaska Native health research from risk towards resilience. As acknowledged previously, American Indians and Alaska Natives continue to be disproportionately affected by chronic mental and physical health conditions (Espey et al., 2014; Gone & Trimble, 2012). While highlighting these inequities is needed to push forward efforts to improve health for American Indians and Alaska Natives, these inequities must be contextualized in the history of colonization and oppression and should be used to motivate researchers and scholars to elucidate factors which allow American Indians and Alaska Natives to thrive and exhibit good health despite a potential underlying context of adversity and trauma. Only through improved understanding and awareness of these resilience factors can effective interventions be designed to promote optimal health and well-being.
To prioritize community well-being and benefit to American Indian and Alaska Native peoples, health research in Indigenous communities must center community member voices at each stage of the research process. A leading model in ensuring appropriate and beneficial research is Community Based Participatory Research (Christopher et al., 2011; LaVeaux & Christopher, 2010). This approach emphasizes the importance of equitable partnerships between community members, stakeholders and researchers and the equal input and involvement of all partners in all phases of the research process. This level of collaboration may strain under resourced and overburdened American Indian community systems. As such, recent calls to action have coined the term regenerative research a term referring to the intentional design of research efforts to promote sustainability and growth of community resources through the research process, rather than only focusing on the downstream benefits of providing information from research findings (Coser et al., 2021). Examples of such community engaged work are widespread and growing in indigenous communities (e.g., Blue Bird Jernigan et al., 2012; Hulen et al., 2019; Teufel-Shone, Schwartz, et al., 2018), and should be used to guide future research efforts.
In addition to elucidating resilience factors across three identified domains (I.e., social, psychological, cultural/spiritual) and their relation to health outcomes, this review draws attention to areas in the literature which are lacking and warrant increased attention in future work. The resilience domain with the smallest number of studies was the psychological domain. This is of interest as the body of work on psychological resilience factors and health outcomes is quite robust across other racial and ethnic groups (Aspinwall & Tedeschi, 2010; Park, Peterson & Szvarca, 2014). To build knowledge in this area for American Indian and Alaska Native peoples, it will be critical to increase community engaged research so that culturally relevant psychological factors which may be sources of resilience are measured appropriately. Furthermore, across all identified domains, there is a general lack of longitudinal research. While documenting cross-sectional relationships between resilience factors and health outcomes is an important step, it is imperative that future research utilizes longitudinal designs to understand dynamic correspondence between changes in these resilience factors and changes in health-relevant outcomes.
We acknowledge that the three individual domains of resilience factors likely interact and inform one another in complex ways. We believe that an important direction of future work should aim to understand the pathways which connect these resilience domains and to better understand interactions between factors across domains. For example, it is possible that a social protective factor such as positive social relationships impacts levels of engagement in cultural activities, and in doing so improves symptoms of depression and anxiety. It is also possible that a factor in one domain may moderate the impact of a factor in a separate domain on health resilience. For example, high levels of family support (I.e., social domain) could promote a positive health outcome (e.g., low levels of anxiety) particularly for American Indians or Alaska Natives who also frequently use emotion reappraisal (I.e., psychological domain). A more nuanced understanding of these pathways and relationships will allow for the design and employment of culturally specific and comprehensive health interventions with a greater chance of contributing to positive and enduring changes in health for American Indian and Alaska Native peoples.
Behavioral factors (e.g., physical activity, dietary intake, sleep) could act as independent resilience factors for American Indian and Alaska Native peoples which promote positive health. It is also possible that the resilience factors identified in the current scoping review may promote positive health outcomes by changing health behaviors. These potential indirect pathways should be explored in future research. Furthermore, future efforts on studying resilience and health in American Indians and Alaska Natives should aim to elucidate barriers to these resilience factors. In other words, it will be important to identify the factors which make it challenging to access or utilize these resilience factors. This information would be valuable in tailoring interventions to address these barriers or challenges to increase observed resilience and positive health outcomes. Finally, while some of the extant literature does consider resilience factors at different points in the lifespan, future studies with samples with a large age range could consider age as a potential moderator of the implications of these resilience factors for health outcomes.
Conclusion
The primary motivation for this work was to provide a synthesis of resilience factors linked to health in American Indian and Alaska Native peoples. The process of collecting work to include in this review provided further evidence of the tendency to focus on deficits rather than strengths in the American Indian and Alaska Native health inequities literature. More specifically, most of the published work in this area continues to use a risk framework to present their findings, but these findings could be presented using a resilience framework. By changing the framing or presentation of findings to highlight resilience rather than risk, researchers may be less likely to foster hopelessness and more likely to promote health behavior changes or other lifestyle changes. The current scoping review synthesizes extant work on resilience factors in American Indians and Alaska Natives and their relationships with health outcomes and calls for more health equity research which utilizes a resilience framework. Furthermore, the review highlights the need for work which considers the interactions between different domains of resilience to better inform the development of effective interventions which aim to increase resilience and consequently improve health for American Indian and Alaska Native peoples.
Table 1.
List of studies included in the social resilience domain.
| Authors | Sample | Sample size | Mean age, % Sex, Racial background |
|---|---|---|---|
| Agyemang et al., 2022 | American Indian/Alaska Native students | 19,067 | Suicide attempts |
| Baldwin et al., 2011 | American Indian youth | 269 | Alcohol and drug use |
| Brockie, Elms and Walls, 2018 | American Indian adults | 192 | Self-rated physical and mental health |
| FitzGerald et al., 2017 | American Indian youth | 2,794 | Suicide attempts |
| Fullerton et al., 2019 | American Indian/Alaska Native youth | 2,218 | Suicide attempts |
| Hulen et al., 2019 | American Indian adults | 39 | Health care provider assessed wellness, healthy behaviors |
| John-Henderson et al., 202 | American Indian adults | 90 | Markers of Immune system inflammation |
| McKinley et al., 2021 | American Indian adults | 117 | Symptoms of depression and anxiety |
| McKinley & Scarnato, 2021 | American Indian adults | 436 | Alcohol use |
| Palimaru et al., 2022 | American Indian/Alaska Native youth | 142 | Symptoms of depression and anxiety |
| Parshall et al., 2023 | American Indian/Alaska Native students | 3,018 | Suicide outcomes |
| Roh et al., 2015 | American Indian older adults | 233 | Depressive symptoms |
| Wood et al., 2018 | American Indian youth | 40 | Self-reported well-being and safety |
Table 2.
List of studies included in the psychological resilience domain.
| Authors | Sample | Sample size | Mean age, % Sex, Racial background |
|---|---|---|---|
| Hobfoll et al., 2002 | American Indian women | 103 | Depressive mood and anger |
| McCullen, Counts & John-Henderson | American Indian adults | 210 | Depressive symptoms and psychological stress |
| Schure, Odden & Goins, 2013 | American Indian adults | 185 | Depressive symptoms, chronic pain, mental and physical health |
| Tyra, Ginty, & John-Henderson, 2021 | American Indian adults | 210 | Post-traumatic stress symptoms |
| Tyra et al., 2023 | American Indian adults | 100 | Ambulatory blood pressure |
Table 3.
List of studies included in the cultural/spiritual resilience domain.
| Authors | Sample | Sample size | Mean age, % Sex, Racial background |
|---|---|---|---|
| Adamsen, Manson, & Jiang, 2021 | American Indian/Alaska Native adults | 14,827 | Memory problems |
| Bear et al., 2018 | Study specific demographic questionnaire | 1,636 | Mental health status |
| Brown et al., 2022 | American Indian/Alaska Native emerging adults | 91 | Substance use |
| Gone & Calf-Looking, 2015 | American Indian male adults | 4 | Substance Use Disorder |
| Hirchak et al., 2021 | American Indian /Alaska Native youth | 7,307 | Non-prescription opioid use |
| Hunter et al., 2022 | Urban American Indian youth | 18 | Self-esteem |
| Huyser et al., 2018 | American Indian adults | 2,409 | Psychological distress |
| Kading et al, 2015 | American Indian adults | 218 | Positive mental health |
| Lee, 2011 | American Indian youth | 360 | Dietary intake |
| Lewis et al., 2022 | American Indian youth | 30 | Dietary intake and mental health |
| Masotti et al., 2020 | American Indian adults | 344 | Mental health and well-being |
| Shea et al., 2019 | American Indian college students | 32 | Reduced trauma-related difficulties and living well |
| Stone et al., 2006 | American Indian adults | 980 | Alcohol cessation |
| Stumblingbear-Riddle & Romans, 2012 | American Indian adolescents | 196 | Subjective Well-Being |
| Wexler, 2014 | Alaskan Native | 23 | Strength and Purpose |
| Wolsko et al., 2007 | Alaskan Native | 488 | Drug and Alcohol use |
References
- *Adamsen C, Manson SM, & Jiang L (2021). The Association of Cultural Participation and Social Engagement with Self-Reported Diagnosis of Memory Problems Among American Indian and Alaska Native Elders. Journal of Aging and Health, 33(7-8 Suppl), 60S–67S. 10.1177/08982643211014971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Agyemang DO, Madden EF, English K, Venner KL, Handy R, Singh TP, & Qeadan F (2022). The mediation and moderation effect of social support on the relationship between opioid misuse and suicide attempts among native American youth in New Mexico: 2009-2019 Youth Risk Resiliency Survey (NM-YRRS). BMC psychiatry, 22(1), 243. 10.1186/s12888-022-03900-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahenakew C (2011). The birth of the “Windigo”: The construction of Aboriginal health in biomedical and traditional indigenous models of medicine. [Google Scholar]
- Akinade T, Kheyfets A, Piverger N, Layne TM, Howell EA, & Janevic T (2023). The influence of racial-ethnic discrimination on women’s health care outcomes: A mixed methods systematic review. Social Science & Medicine, 316, 114983. 10.1016/j.socscimed.2022.114983 [DOI] [PubMed] [Google Scholar]
- Allen J, Wexler L, & Rasmus S (2022). Protective Factors as a Unifying Framework for Strength-Based Intervention and Culturally Responsive American Indian and Alaska Native Suicide Prevention. Prevention Science, 23(1), 59–72. 10.1007/s11121-021-01265-0 [DOI] [PubMed] [Google Scholar]
- American Association of Suicidology. (2010). Some facts about suicide and depression. Retrieved from http://www.suicidology.org/
- Arksey H, & O’Malley L (2005). Scoping Studies: Towards a Methodological Framework. International Journal of Social Research Methodology: Theory & Practice, 8(1), 19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- Aspinwall LG, & Tedeschi RG (2010). The value of positive psychology for health psychology: progress and pitfalls in examining the relation of positive phenomena to health. Annals of behavioral medicine : a publication of the Society of Behavioral Medicine, 39(1), 4–15. 10.1007/s12160-009-9153-0 [DOI] [PubMed] [Google Scholar]
- *Baldwin JA; Brown BG; Wayment HA; Nez RA; Brelsford KM Culture and Context: Buffering the Relationship between Stressful Life Events and Risky Behaviors in American Indian Youth. Subst. Use Misuse 2011,46, 1380–1394. [DOI] [PubMed] [Google Scholar]
- Barger SD (2013). Social integration, social support and mortality in the US National Health Interview Survey. Psychosomatic medicine, 75(5), 510–517. 10.1097/PSY.0b013e318292ad99 [DOI] [PubMed] [Google Scholar]
- Barnhardt R, & Kawagley AO (2005). Indigenous Knowledge Systems and Alaska Native Ways of Knowing. Anthropology & Education Quarterly, 36(1), 8–23. 10.1525/aeq.2005.36.1.008 [DOI] [Google Scholar]
- Beals J, Manson SM, Shore JH, Friedman M, Ashcraft M, Fairbank JA, & Schlenger WE (2002). The prevalence of posttraumatic stress disorder among American Indian Vietnam veterans: Disparities and context. Journal of Traumatic Stress, 15(2), 89–97. 10.1023/A:1014894506325 [DOI] [PubMed] [Google Scholar]
- *Bear UR, Garroutte EM, Beals J, Kaufman CE, & Manson SM (2018). Spirituality and mental health status among Northern Plain tribes. Mental Health, Religion & Culture, 21(3), 274–287. 10.1080/13674676.2018.1469121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berking M, & Wupperman P (2012). Emotion regulation and mental health: recent findings, current challenges, and future directions. Current opinion in psychiatry, 25(2), 128–134. 10.1097/YCO.0b013e3283503669 [DOI] [PubMed] [Google Scholar]
- Berkman LF, Glass T, Brissette I, & Seeman TE (2000). From social integration to health: Durkheim in the new millennium. Social science & medicine (1982), 51(6), 843–857. 10.1016/s0277-9536(00)00065-4 [DOI] [PubMed] [Google Scholar]
- Blue Bird Jernigan V, Salvatore AL, Styne DM, & Winkleby M (2012). Addressing food insecurity in a Native American reservation using community-based participatory research. Health Education Research, 27(4), 645–655. 10.1093/her/cyr089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brave Heart, M. Y. H. (1998). The return to the sacred path: Healing the historical trauma and historical unresolved grief response among the lakota through a psychoeducational group intervention. Smith College Studies in Social Work, 68(3), 287–305. 10.1080/00377319809517532 [DOI] [Google Scholar]
- Brave Heart MYH. (2005). Substance abuse, co-occurring mental health disorders, and the historical trauma response among American Indians/Alaska Natives (Research Monograph). Washington, DC: Bureau of Indian Affairs, DASAP. [Google Scholar]
- *Brockie TN, Elm JHL, & Walls ML (2018). Examining protective and buffering associations between sociocultural factors and adverse childhood experiences among American Indian adults with type 2 diabetes: a quantitative, community-based participatory research approach. BMJ open, 8(9), e022265. 10.1136/bmiopen-2018-022265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brockie TN, Dana-Sacco G, Wallen GR, Wilcox HC, & Campbell JC (2015). The relationship of adverse childhood experiences to PTSD, depression, poly-drug use and suicide attempt in reservation-based Native American adolescents and young adults. American Journal of Community Psychology, 55(3-4), 411–421. 10.1007/s10464-015-9721-3 [DOI] [PubMed] [Google Scholar]
- *Brown RA, Palimaru AI, Dickerson DL, Etz K, Kennedy DP, Hale B, Johnson CL, & D’Amico EJ (2022). Cultural Dynamics, Substance Use, and Resilience Among American Indian/Alaska Native Emerging Adults in Urban Areas. Adversity and Resilience Science. 10.1007/s42844-022-00058-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns RA, & Anstey KJ (2010). The Connor–Davidson Resilience Scale (CD-RISC): Testing the invariance of a uni-dimensional resilience measure that is independent of positive and negative affect. Personality and Individual Differences, 48(5), 527–531. 10.1016/j.paid.2009.11.026 [DOI] [Google Scholar]
- Chapman DP, Croft JB, Liu Y, Perry GS, Presley-Cantrell LR, & Ford ES (2013). Excess frequent insufficient sleep in American Indians/Alaska natives. Journal of environmental and public health, 2013, 259645. 10.1155/2013/259645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang Q, Chan CH, & Yip PSF (2017). A meta-analytic review on social relationships and suicidal ideation among older adults. Social science & medicine (1982), 191, 65–76. 10.1016/j.socscimed.2017.09.003 [DOI] [PubMed] [Google Scholar]
- Christopher S, Saha R, Lachapelle P, Jennings D, Colclough Y, Cooper C, Cummins C, Eggers MJ, FourStar K, Harris K, Kuntz SW, LaFromboise V, LaVeaux D, McDonald T, Bird JR, Rink E, & Webster L (2011). Applying Indigenous Community-Based Participatory Research Principles to Partnership Development in Health Disparities Research: Family & Community Health, 34(3), 246–255. 10.1097/FCH.0b013e318219606f [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor KM, Davidson JR, & Lee LC (2003). Spirituality, resilience, and anger in survivors of violent trauma: a community survey. Journal of traumatic stress, 16(5), 487–494. 10.1023/A:1025762512279 [DOI] [PubMed] [Google Scholar]
- Coser A, Kominsky TK, & White EJ (2021). For the Good of the Community: Considering the Impact of Evidence-Based Treatment Adaptation on Tribal Communities. The Behavior Therapist, 44(4), 161–170. [PMC free article] [PubMed] [Google Scholar]
- Cromer LD, Gray ME, Vasquez L, & Freyd JJ (2018). The Relationship of Acculturation to Historical Loss Awareness, Institutional Betrayal, and the Intergenerational Transmission of Trauma in the American Indian Experience. Journal of Cross-Cultural Psychology, 49(1), 99–114. 10.1177/0022022117738749 [DOI] [Google Scholar]
- D’Amico EJ, Dickerson DL, Rodriguez A, Brown RA, Kennedy DP, Palimaru AI, Johnson C, Smart R, Klein DJ, Parker J, McDonald K, Woodward MJ, & Gudgell N (2021). Integrating traditional practices and social network visualization to prevent substance use: Study protocol for a randomized controlled trial among urban Native American emerging adults. Addiction Science & Clinical Practice, 16(1), 56. 10.1186/s13722-021-00265-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Leeuw SD, Maurice S, Holyk T, Greenwood M, Adam W (2012). With reserves: colonial geographies and First Nations Health. Annals of the American Association of Geographers, 102, 904–911. [Google Scholar]
- Duran E, Duran B. (1995). Native American post-colonial psychology. New York, NY: Suny Press; 1995. 1 [Google Scholar]
- Espey DK, Jim MA, Cobb N, Bartholomew M, Becker T, Haverkamp D, & Plescia M (2014). Leading causes of death and all-cause mortality in American Indians and Alaska Natives. American journal of public health, 104 Suppl 3(Suppl 3), S303–S311. 10.2105/AJPH.2013.301798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *FitzGerald CA, Fullerton L, Green D, Hall M, & Peñaloza LJ (2017). The Association Between Positive Relationships with Adults and Suicide-Attempt Resilience in American Indian Youth in New Mexico. American Indian and Alaska native mental health research (Online), 24(2), 40–53. 10.5820/aian.2402.2017.40 [DOI] [PubMed] [Google Scholar]
- Fleming J, & Ledogar RJ (2008). Resilience and Indigenous Spirituality: A Literature Review. Pimatisiwin, 6(2), 47–64. [PMC free article] [PubMed] [Google Scholar]
- Fothergill KE, Ensminger ME, Robertson J, Green KM, Thorpe RJ, & Juon HS (2011). Effects of social integration on health: A prospective study of community engagement among African American women. Social science & medicine (1982), 72(2), 291–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Fullerton L, FitzGerald CA, Hall ME, Green D, DeBruyn LM, & Peñaloza LJ (2019). Suicide Attempt Resiliency in American Indian, Hispanic, and Anglo Youth in New Mexico: The Influence of Positive Adult Relationships. Family & community health, 42(3), 171–179. 10.1097/FCH.0000000000000223 [DOI] [PubMed] [Google Scholar]
- Gilgun JF (2002). Completing the Circle: American Indian Medicine Wheels and the Promotion of Resilience of Children and Youth in Care. Journal of Human Behavior in the Social Environment, 6(2), 65–84. 10.1300/J137v06n02_05 [DOI] [Google Scholar]
- Godfrey TM, Cordova-Marks FM, Jones D, Melton F, & Breathett K (2022). Metabolic Syndrome Among American Indian and Alaska Native Populations: Implications for Cardiovascular Health. Current hypertension reports, 24(5), 107–114. 10.1007/s11906-022-01178-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gone JP (2013). Redressing First Nations historical trauma: Theorizing mechanisms for indigenous culture as mental health treatment. Transcultural Psychiatry, 50(5), 683–706. [DOI] [PubMed] [Google Scholar]
- Gone JP, & Calf Looking PE (2011). American Indian Culture as Substance Abuse Treatment: Pursuing Evidence for a Local Intervention. Journal of Psychoactive Drugs, 43(4), 291–296. 10.1080/02791072.2011.628915 [DOI] [PubMed] [Google Scholar]
- *Gone JP, & Calf Looking PE (2015). The Blackfeet Indian culture camp: Auditioning an alternative indigenous treatment for substance use disorders. Psychological Services, 12(2), 83–91. [DOI] [PubMed] [Google Scholar]
- Gone JP, Hartmann WE, Pomerville A, Wendt DC, Klem SH, & Burrage RL (2019). The impact of historical trauma on health outcomes for indigenous populations in the USA and Canada: A systematic review. American Psychologist, 74(1), 20–35. 10.1037/amp0000338 [DOI] [PubMed] [Google Scholar]
- Gone JP, & Trimble JE (2012). American Indian and Alaska Native mental health: diverse perspectives on enduring disparities. Annual review of clinical psychology, 8, 131–160. 10.1146/annurev-clinpsy-032511-143127 [DOI] [PubMed] [Google Scholar]
- Gonzalez MB, Sittner KJ, & Walls ML (2022). Cultural efficacy as a novel component of understanding linkages between culture and mental health in Indigenous communities. American Journal of Community Psychology, ajcp.12594. 10.1002/ajcp.12594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham BL (2001). Resilience among American Indian youth: First Nations’ youth resilience study. (Doctoral dissertation, University of Minnesota, 2001). Dissertation Abstracts International: Section B: The Sciences and Engineering, 62, 3–B. [Google Scholar]
- Grandbois DM, & Sanders GF (2009). The Resilience of Native American Elders. Issues in Mental Health Nursing, 30(9), 569–580. 10.1080/01612840902916151 [DOI] [PubMed] [Google Scholar]
- Gross JJ (1998). The emerging field of emotion regulation: An integrative review. Review of General Psychology, 2(3), 271–299. 10.1037/1089-2680.2.3.271 [DOI] [Google Scholar]
- Hardy SE, Concato J, & Gill TM (2004). Resilience of community-dwelling older persons. Journal of the American Geriatrics Society, 52(2), 257–262. 10.1111/j.1532-5415.2004.52065.x [DOI] [PubMed] [Google Scholar]
- Hartmann WE, Wendt DC, Burrage RL, Pomerville A, & Gone JP (2019). American Indian historical trauma: Anticolonial prescriptions for healing, resilience, and survivance. The American Psychologist, 74(1), 6–19. 10.1037/amp0000326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heart MY, Chase J, Elkins J, & Altschul DB (2011). Historical trauma among Indigenous Peoples of the Americas: concepts, research, and clinical considerations. Journal of psychoactive drugs, 43(4), 282–290. 10.1080/02791072.2011.628913 [DOI] [PubMed] [Google Scholar]
- Heid O, Khalid M, Smith H, Kim K, Smith S, Wekerle C, Six Nations Youth Mental Wellness Committee, Bomberry T, Hill LD, General DA, Green TTJ, Harris C, Jacobs B, Jacobs N, Kim K, Horse ML, Martin-Hill D, McQueen KCD, Miller TF, Noronha N, … Wekerle C. (2022). Indigenous Youth and Resilience in Canada and the USA: a Scoping Review. Adversity and resilience science, 3(2), 113–147. 10.1007/s42844-022-00060-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herron JL, & Venner KL (2022). A Systematic Review of Trauma and Substance Use in American Indian and Alaska Native Individuals: Incorporating Cultural Considerations. Journal of racial and ethnic health disparities, 10.1007/s40615-022-01250-5. Advance online publication. 10.1007/s40615-022-01250-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henson M, Sabo S, Trujillo A, & Teufel-Shone N (2017). Identifying Protective Factors to Promote Health in American Indian and Alaska Native Adolescents: A Literature Review. The Journal of Primary Prevention, 38(1–2), 5–26. 10.1007/s10935-016-0455-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Hirchak K, Amiri S, Espinoza J, Herron J, Hernandez-Vallant A, Cloud V, & Venner K (2021). Trends in Non-Medical Prescription Opioid Use among Urban and Rural American Indian and Alaska Native Youth Residing in New Mexico: 2013-2017. American Indian and Alaska native mental health research (Online), 28(1), 1–16. 10.5820/aian.2801.2021.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Hobfoll SE, Jackson A, Hobfoll I, Pierce CA, & Young S (2002). The impact of communal-mastery versus self-mastery on emotional outcomes during stressful conditions: a prospective study of Native American women. American journal of community psychology, 30(6), 853–871. 10.1023/A:1020209220214 [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Baker M, Harris T, & Stephenson D (2015). Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspectives on psychological science: a journal of the Association for Psychological Science, 10(2), 227–237. 10.1177/1745691614568352 [DOI] [PubMed] [Google Scholar]
- *Hulen E, Hardy LJ, Teufel-Shone N, Sanderson PR, Schwartz AL, & Begay RC (2019). Community Based Participatory Research (CBPR): A Dynamic Process of Health care, Provider Perceptions and American Indian Patients’ Resilience. Journal of health care for the poor and underserved, 30(1), 221–237. 10.1353/hpu.2019.0017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Hunter A, Carlos M, Muniz FB, Leybas Nuño V, Tippeconnic Fox MJ, Carvajal S, Lameman B, & Yuan N (2022). Participation in a Culturally Grounded Program Strengthens Cultural Identity, Self-esteem, and Resilience in Urban Indigenous Adolescents. American Indian and Alaska native mental health research (Online), 29(1), 1–21. 10.5820/aian.2901.2022.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Huyser KR, Angel RJ, Beals J, Cox JH, Hummer RA, Sakamoto A, Manson SM, & AI-SUPERPFP Team (2018). Reservation Lands as a Protective Social Factor: An Analysis of Psychological Distress among Two American Indian Tribes. Socius : sociological research for a dynamic world, 4, 10.1177/2378023118807022. 10.1177/2378023118807022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Indian Health Services. (2023, February 9). Trends in Inidan Health 2014 Edition. https://www.ihs.gov/sites/dps/themes/newihstheme/display_objects/documents/Trends2014Book508.pdf
- John-Henderson NA, & Ginty AT (2020). Historical trauma and social support as predictors of psychological stress responses in American Indian adults during the COVID-19 pandemic. Journal of Psychosomatic Research, 139, Article 110263. 10.1016/j.jpsychores.2020.110263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *John-Henderson NA, Henderson-Matthews B, Ollinger SR, Racine J, Gordon MR, Higgins AA, Horn WC, Reevis SA, Running Wolf JA, Grant D, & Rynda-Apple A (2020). Adverse Childhood Experiences and Immune System Inflammation in Adults Residing on the Blackfeet Reservation: The Moderating Role of Sense of Belonging to the Community. Annals of behavioral medicine : a publication of the Society of Behavioral Medicine, 54(2), 87–93. 10.1093/abm/kaz029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- John-Henderson NA, Grant VM, Johnson LR 3rd, Lafromboise ME, Malatare M, Salois EM, & Oosterhoff B (2022a). Historical loss: Implications for physical activity levels in American Indian adults. The Journal of rural health : official journal of the American Rural Health Association and the National Rural Health Care Association, 10.1111/jrh.12673. Advance online publication. 10.1111/jrh.12673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- John-Henderson NA, Oosterhoff B, Kampf TD, Hall B, Johnson LR, Laframboise ME, Malatare M, Salois E, Carter JR, & Adams AK (2022b). Historical Loss: Implications for Health of American Indians in the Blackfeet Community. Annals of behavioral medicine : a publication of the Society of Behavioral Medicine, 56(2), 193–204. 10.1093/abm/kaab032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Kading ML, Hautala DS, Palombi LC, Aronson BD, Smith RC, & Walls ML (2015). Flourishing: American Indian Positive Mental Health. Society and Mental Health, 5(3), 203–217. 10.1177/2156869315570480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahn CB, Reinschmidt K, Teufel-Shone NI, Oré CE, Henson M, & Attakai A (2016). American Indian Elders’ resilience: Sources of strength for building a healthy future for youth. American Indian and Alaska Native Mental Health Research (Online), 23(3), 117–133. 10.5820/aian.2303.2016.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenney MK, & Singh GK (2016). Adverse childhood experiences among American Indian/Alaska Native children: The 2011–2012 National Survey of Children’s Health. Scientifica, 2016, 7424239 10.1155/2016/7424239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirmayer LJ, Dandeneau S, Marshall E, Phillips MK, & Williamson KJ (2011). Rethinking Resilience from Indigenous Perspectives. The Canadian Journal of Psychiatry, 56(2), 84–91. 10.1177/070674371105600203 [DOI] [PubMed] [Google Scholar]
- Kraiss JT, Ten Klooster PM, Moskowitz JT, & Bohlmeijer ET (2020). The relationship between emotion regulation and well-being in patients with mental disorders: A meta-analysis. Comprehensive psychiatry, 102, 152189. 10.1016/j.comppsych.2020.152189 [DOI] [PubMed] [Google Scholar]
- Kruse G, Lopez-Carmen VA, Jensen A, Hardie L, & Sequist TD (2022). The Indian Health Service and American Indian/Alaska Native Health Outcomes. Annual review of public health, 43, 559–576. 10.1146/annurev-publhealth-052620-103633 [DOI] [PubMed] [Google Scholar]
- LaFromboise TD (1992). An interpersonal analysis of affinity, clarification, and helpful responses with American Indians. Professional Psychology: Research and Practice, 23(4), 281–286. 10.1037/0735-7028.23.4.281 [DOI] [Google Scholar]
- LaFromboise TD, Hoyt DR, Oliver L, & Whitbeck LB (2006). Family, community, and school influences on resilience among American Indian adolescents in the upper midwest. Journal of Community Psychology, 34(2), 193–209. 10.1002/jcop.20090 [DOI] [Google Scholar]
- LaVeaux D, & Christopher S (2010). Contextualizing CBPR: Key Principles of CBPR meet the Indigenous research context. 16. [PMC free article] [PubMed]
- *Lee. (2011). Relationships among body mass index, nutrition, internalizing symptoms, and ethnic identity of Cherokee youth attending a private Native American secondary school. ProQuest Dissertations Publishing. [Google Scholar]
- *Lewis ME, Smith J, Wildcat S, Anderson A, & Walls ML (2022). The Health Effects of a Cherokee Grounded Culture and Leadership Program. International journal of environmental research and public health, 19(13), 8018. 10.3390/ijerph1913801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Low RST, Overall NC, Chang VT, Henderson AME, & Sibley CG (2021). Emotion regulation and psychological and physical health during a nationwide COVID-19 lockdown. Emotion (Washington, D.C.), 21(8), 1671–1690. 10.1037/emo0001046 [DOI] [PubMed] [Google Scholar]
- Manson SM, Beals J, Klein SA, Croy CD, & the AI-SUPERPFP Team. (2005). Social Epidemiology of Trauma Among 2 American Indian Reservation Populations. American Journal of Public Health, 95(5), 851–859. 10.2105/AJPH.2004.054171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Masotti P, Dennem J, Hadani S, Banuelos K, King J, Linton J, Lockhart B, & Patel C (2020). The Culture is Prevention Project: Measuring Culture as a Social Determinant of Mental Health for Native/Indigenous Peoples. American Indian and Alaska native mental health research (Online), 27(1), 86–111. 10.5820/aian.2701.2020.86 [DOI] [PubMed] [Google Scholar]
- Masten AS (2001). Ordinary magic: Resilience processes in development. American Psychologist, 56(3), 227–238. 10.1037/0003-066X.56.3.227 [DOI] [PubMed] [Google Scholar]
- Masten AS (2014). Global perspectives on resilience in children and youth. Child development, 85(1), 6–20. 10.1111/cdev12205 [DOI] [PubMed] [Google Scholar]
- Masten AS, Lucke CM, Nelson KM, & Stallworthy IC (2021). Resilience in development and psychopathology: Multisystem perspectives. Annual Review of Clinical Psychology, 17, 521–549. 10.1146/annurev-clinpsy-081219-120307 [DOI] [PubMed] [Google Scholar]
- Mayne TJ (2001). Emotions and health. In Mayne TJ & Bonanno GA (Eds.), Emotions: Current issues and future directions (pp. 361–397). Guilford Press. [Google Scholar]
- *McCullen JR, Counts CJ, & John-Henderson NA (2022). Childhood adversity and emotion regulation strategies as predictors of psychological stress and mental health in American Indian adults during the COVID-19 pandemic. Emotion. Advance online publication. 10.1037/emo0001106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *McKinley CE, Boel-Studt S, Renner LM, & Figley CR (2021). Risk and protective factors for symptoms of depression and anxiety among American Indians: Understanding the roles of resilience and trauma. Psychological trauma : theory, research, practice and policy, 13(1), 16–25. 10.1037/tra0000950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *McKinley CE, & Scarnato JM (2021). What’s love got to do with it? “Love” and Alcohol Use among U.S. Indigenous Peoples: Aligning Research with Real-world Experiences. Journal of ethnic & cultural diversity in social work, 30(1-2), 26–46. 10.1080/15313204.2020.1770650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMahon, Kenyon DB, & Carter JS. (2013). “My Culture, My Family, My School, Me”: Identifying Strengths and Challenges in the Lives and Communities of American Indian Youth. Journal of Child and Family Studies, 22(5), 694–706. 10.1007/s10826-012-9623-z [DOI] [Google Scholar]
- Mehta M, Whyte E, Lenze E, Hardy S, Roumani Y, Subashan P, Huang W, & Studenski S (2008). Depressive symptoms in late life: associations with apathy, resilience and disability vary between young-old and old-old. International journal of geriatric psychiatry, 23(3), 238–243. 10.1002/gps.1868 [DOI] [PubMed] [Google Scholar]
- Nikolaus CJ, Sinclair K, Buchwald D, & Suchy-Dicey AM (2021). Association of stress and resilience with cardiometabolic health among American Indian and Alaska Native adults. Preventive Medicine Reports, 24, 101517. 10.1016/j.pmedr.2021.101517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Neill J, Reading J, Leader A (1998). Changing the relations of surveillance: the development of a discourse of resistance in Aboriginal epidemiology. Human Organization, 57, 230–237. [Google Scholar]
- Ong AD, Bergeman CS, Bisconti TL, & Wallace KA (2006). Psychological resilience, positive emotions, and successful adaptation to stress in later life. Journal of personality and social psychology, 91(4), 730–749. 10.1037/0022-3514.91A730 [DOI] [PubMed] [Google Scholar]
- Oré CE, Teufel-Shone NI, & Chico-Jarillo TM (2016). AMERICAN INDIAN AND ALASKA NATIVE RESILIENCE ALONG THE LIFE COURSE AND ACROSS GENERATIONS: A LITERATURE REVIEW. American Indian and Alaska Native Mental Health Research (Online), 23(3), 134–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Palimaru AI, Dong L, Brown RA, D’Amico EJ, Dickerson DL, Johnson CL, & Troxel WM (2022). Mental health, family functioning, and sleep in cultural context among American Indian/Alaska Native urban youth: A mixed methods analysis. Social science & medicine (1982), 292, 114582. 10.1016/j.socscimed.2021.114582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panter-Brick C, & Leckman JF (2013). Editorial Commentary: Resilience in child development--interconnected pathways to wellbeing. Journal of child psychology and psychiatry, and allied disciplines, 54(4), 333–336. 10.1111/jcpp.12057 [DOI] [PubMed] [Google Scholar]
- Park N, Peterson C, Szvarca D, Vander Molen RJ, Kim ES, & Collon K (2014). Positive Psychology and Physical Health: Research and Applications. American journal of lifestyle medicine, 10(3), 200–206. 10.1177/1559827614550277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parshall C, Qeadan F, Espinoza J, & English K (2023). The Association Between Resiliency Factors and Suicide Indicators Among American Indian/Alaska Native Middle School Students in New Mexico: A Strength-Based Analysis. Public health reports (Washington, D.C. : 1974), 333549231156607. Advance online publication. 10.1177/00333549231156607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin LI, Lieberman MA, Menaghan EG, & Mullan JT (1981). The stress process. Journal of Health and Social Behavior, 22, 337–356. [PubMed] [Google Scholar]
- Pomerville A, & Gone JP (2019). Indigenous culture-as-treatment in the era of evidence-based mental health practice. In Fleming C & Manning M (Eds.), Routledge handbook of Indigenous wellbeing (pp. 237–247). New York: Routledge. [Google Scholar]
- Reinschmidt KM, Attakai A, Kahn CB, Whitewater S, & Teufel-Shone N (2016). Shaping a Stories of Resilience Model from urban American Indian elders’ narratives of historical trauma and resilience. American Indian and Alaska Native Mental Health Research (Online), 23(4), 63–85. 10.5820/aian.2304.2016.63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rieckmann T, McCarty D, Kovas A, Spicer P, Bray J, Gilbert S, & Mercer J (2012). American Indians with substance use disorders: treatment needs and comorbid conditions. The American journal of drug and alcohol abuse, 38(5), 498–504. 10.3109/00952990.2012.694530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robin RW, Chester B, Rasmussen JK, Jaranson JM, & Goldman D (1997). Prevalence and Characteristics of Trauma and Posttraumatic Stress Disorder in a Southwestern American Indian Community. American Journal of Psychiatry, 154(11), 1582–1588. 10.1176/ajp.154.11.1582 [DOI] [PubMed] [Google Scholar]
- *Roh S, Burnette CE, Lee KH, Lee YS, Easton SD, & Lawler MJ (2015). Risk and protective factors for depressive symptoms among American Indian older adults: adverse childhood experiences and social support. Aging & mental health, 19(4), 371–380. 10.1080/13607863.2014.938603 [DOI] [PubMed] [Google Scholar]
- Sarche M, & Spicer P (2008). Poverty and health disparities for American Indian and Alaska Native children: current knowledge and future prospects. Annals of the New York Academy of Sciences, 1136, 126–136. 10.1196/annals.1425.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Schure MB, Odden M, & Goins RT (2013). The association of resilience with mental and physical health among older American Indians: the Native Elder Care Study. American Indian and Alaska native mental health research (Online), 20(2), 27–41. 10.5820/aian.2002.2013.27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Shea H, Mosley-Howard GS, Baldwin D, Ironstrack G, Rousmaniere K, & Schroer JE (2019). Cultural revitalization as a restorative process to combat racial and cultural trauma and promote living well. Cultural Diversity and Ethnic Minority Psychology, 25(4), 553–565. 10.1037/cdp0000250 [DOI] [PubMed] [Google Scholar]
- Skewes MC & Gonzalez VM (2013). Biopsychosocial model of addiction. In: Principles of Addiction: Comprehensive Addictive Behaviors and Disorders. Elsevier Inc., San Diego: Academic Press, pp. 61–70. [Google Scholar]
- Snowshoe A, Crooks CV, Tremblay PF, Craig WM, & Hinson RE (2015). Cultural Connectedness Scale (CCS) [Database record]. APA PsycTests. 10.1037/t39610-000 [DOI] [PubMed] [Google Scholar]
- Solomon TGA, Starks RRB, Attakai A, Molina F, Cordova-Marks F, Kahn-John M, Antone CL, Flores M, & Garcia F (2022). The Generational Impact Of Racism On Health: Voices From American Indian Communities: Study examines the generational impact of racism on the health of American Indian communities and people. Health Affairs, 41(2), 281–288. 10.1377/hlthaff.2021.01419 [DOI] [PubMed] [Google Scholar]
- Soto C, West AE, Ramos GG, & Unger JB (2022). Substance and Behavioral Addictions among American Indian and Alaska Native Populations. International Journal of Environmental Research and Public Health, 19(5), 2974. 10.3390/ijerph19052974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sowislo JF, & Orth U (2013). Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies. Psychological bulletin, 139(1), 213–240. 10.1037/a0028931 [DOI] [PubMed] [Google Scholar]
- *Stone RAT, Whitbeck LB, Chen X, Johnson K, & Olson DM (2006). Traditional practices, traditional spirituality, and alcohol cessation among American Indians. Journal of Studies on Alcohol, 67(2), 236–244. 10.15288/jsa.2006.67.236 [DOI] [PubMed] [Google Scholar]
- *Stumblingbear-Riddle G, & Romans JSC (2012). Resilience among urban American Indian adolescents: Exploration into the role of culture, self-esteem, subjective well-being, and social support. American Indian and Alaska Native Mental Health Research (Online), 19(2), 1–19. 10.5820/aian.1902.2012.1 [DOI] [PubMed] [Google Scholar]
- Teufel-Shone NI, Schwartz AL, Hardy LJ, de Heer HD, Williamson HJ, Dunn DJ, Polingyumptewa K, & Chief C (2018). Supporting New Community-Based Participatory Research Partnerships. International Journal of Environmental Research and Public Health, 16(1), 44. 10.3390/ijerph16010044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teufel-Shone NI, Tippens JA, McCrary HC, Ehiri JE, & Sanderson PR (2018). Resilience in American Indian and Alaska Native Public Health: An Underexplored Framework. American Journal of Health Promotion : AJHP, 32(2), 274–281. 10.1177/0890117116664708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornton R (1997). Tribal membership requirements and the demography of ‘old’ and ‘new’ Native Americans. Population Research and Policy Review 16, 33–42. [Google Scholar]
- Toombs E, Kowatch KR, & Mushquash CJ (2016). Resilience in Canadian Indigenous Youth: A scoping review. International Journal of Child and Adolescent Resilience, 4(1), 4–32. Retrieved from https://ijcar-rirea.ca/index.php/ijcar-rirea/article/view/193 [Google Scholar]
- Tse S, Tsoi EW, Hamilton B, O’Hagan M, Shepherd G, Slade M, Whitley R, & Petrakis M (2016). Uses of strength-based interventions for people with serious mental illness: A critical review. The International journal of social psychiatry, 62(3), 281–291. 10.1177/0020764015623970 [DOI] [PubMed] [Google Scholar]
- *Tyra AT, Ginty AT, & John-Henderson NA (2021). Emotion Regulation Strategies Predict PTSS During the COVID-19 Pandemic in an American Indian Population. International journal of behavioral medicine, 28(6), 808–812. 10.1007/s12529-021-09964-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyra AT, Ginty AT, Johnson LR 3rd, Lafromboise ME, Malatare M, Salois E, & John-Henderson NA (2023). Emotion Regulation Strategies Relate to Ambulatory Cardiovascular Activity in an American Indian Community. Psychosomatic medicine, 85(1), 2–7. 10.1097/PSY.0000000000001140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ulturgasheva O, Rasmus S, Wexler L, Nystad K, & Kral M (2014). Arctic indigenous youth resilience and vulnerability: Comparative analysis of adolescent experiences across five cir- cumpolar communities. Transcultural Psychiatry, 51(5), 735–756. 10.1177/1363461514547120 [DOI] [PubMed] [Google Scholar]
- Van Meter AR, Paksarian D, & Merikangas KR (2019). Social Functioning and Suicide Risk in a Community Sample of Adolescents. Journal of clinical child and adolescent psychology : the official journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53, 48(2), 273–287. [DOI] [PubMed] [Google Scholar]
- Walls M, Sittner KJ, Whitbeck LB, Herman K, Gonzalez M, Elm JHL, Hautala D, Dertinger M, & Hoyt DR (2021). Prevalence of Mental Disorders from Adolescence Through Early Adulthood in American Indian and First Nations Communities. International Journal of Mental Health and Addiction, 19(6), 2116–2130. 10.1007/s11469-020-00304-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters KL, & Simoni JM (2002). Reconceptualizing Native Women’s Health: An “Indigenist” Stress-Coping Model. American Journal of Public Health, 92(4), 520–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warne D, Dulacki K, Spurlock M, Meath T, Davis MM, Wright B, & McConnell KJ (2017). Adverse Childhood Experiences (ACE) among American Indians in South Dakota and Associations with Mental Health Conditions, Alcohol Use, and Smoking. Journal of health care for the poor and underserved, 28(4), 1559–1577. 10.1353/hpu.2017.0133 [DOI] [PubMed] [Google Scholar]
- *Wexler L (2014). Looking across three generations of Alaska Natives to explore how culture fosters indigenous resilience. Transcultural Psychiatry, 51(1), 73–92. 10.1177/1363461513497417 [DOI] [PubMed] [Google Scholar]
- *Wolsko C, Lardon C, Mohatt GV, & Orr E (2007). Stress, coping, and well-being among the Yup’ik of the Yukon-Kuskokwim Delta: The role of enculturation and acculturation. International Journal of Circumpolar Health, 66(1), 51–61. 10.3402/ijch.v66i1.18226 [DOI] [PubMed] [Google Scholar]
- *Wood L, Kamper D, & Swanson K (2018). Spaces of hope? Youth perspectives on health and wellness in indigenous communities. Health & place, 50, 137–145. 10.1016/j.healthplace.2018.01.010 [DOI] [PubMed] [Google Scholar]


