Abstract
Simple Summary
We used genetically modified mice overexpressing the cytokine transforming growth factor beta 1 (TGF mice) that capture several aspects of the cerebrovascular pathology present in Alzheimer’s disease and vascular cognitive impairment and dementia. To identify the proteins that demonstrated different levels in TGF mice compared to genetically unmodified mice, we performed mass spectrometry on surgically removed cerebral arteries to identify and compare proteins between the two groups. Out of the 3602 identified proteins in brain blood vessels, 20 had significantly different levels in TGF mice. We used multiple public databases to (a) characterize the identified proteins, (b) validate the presence of their RNA transcripts in cerebrovascular cells of mice and humans, and (c) validate their presence in extracellular vesicles (i.e., little pouches of cellular content that participate in cell-to-cell communication) present in human blood. Finally, using human blood, we demonstrated the presence of several of these proteins in blood and in extracellular vesicles isolated from blood. Our research provides protein-level insights into cerebrovascular pathology in age-related dementias. Identified proteins can potentially serve as markers of vascular cognitive impairment and dementia in humans.
Abstract
Cerebrovascular pathology that involves altered protein levels (or signaling) of the transforming growth factor beta (TGFβ) family has been associated with various forms of age-related dementias, including Alzheimer disease (AD) and vascular cognitive impairment and dementia (VCID). Transgenic mice overexpressing TGFβ1 in the brain (TGF mice) recapitulate VCID-associated cerebrovascular pathology and develop cognitive deficits in old age or when submitted to comorbid cardiovascular risk factors for dementia. We characterized the cerebrovascular proteome of TGF mice using mass spectrometry (MS)-based quantitative proteomics. Cerebral arteries were surgically removed from 6-month-old-TGF and wild-type mice, and proteins were extracted and analyzed by gel-free nanoLC-MS/MS. We identified 3602 proteins in brain vessels, with 20 demonstrating significantly altered levels in TGF mice. For total and/or differentially expressed proteins (p ≤ 0.01, ≥ 2-fold change), using multiple databases, we (a) performed protein characterization, (b) demonstrated the presence of their RNA transcripts in both mouse and human cerebrovascular cells, and (c) demonstrated that several of these proteins were present in human extracellular vesicles (EVs) circulating in blood. Finally, using human plasma, we demonstrated the presence of several of these proteins in plasma and plasma EVs. Dysregulated proteins point to perturbed brain vessel vasomotricity, remodeling, and inflammation. Given that blood-isolated EVs are novel, attractive, and a minimally invasive biomarker discovery platform for age-related dementias, several proteins identified in this study can potentially serve as VCID markers in humans.
Keywords: cerebrovascular pathology, age-related dementia, mouse model, cerebrovascular proteomics, mass spectrometry, human plasma, protein biomarkers, extracellular vesicles
1. Introduction
With advancing age, blood vessels in the brain become increasingly vulnerable to pathologies. Damage to the brain’s vasculature disrupts the neurovascular unit, a multicellular system in which neurons, vascular cells (smooth muscle, pericytes, and endothelial cells), astrocytes, and microglia collaborate to ensure proper brain function [1,2]. Cerebrovascular damage can cause and/or aggravate age-related cognitive decline and dementia [3,4,5]. Affecting an estimated 55 million people worldwide, age-related dementias are a major cause of disability and dependency among the elderly (World Health Organization). A cerebrovascular pathology partly involving altered signaling or increased levels of the cytokine transforming growth factor beta 1 (TGFβ1) has been associated with various types of dementias, including the two most frequent forms, namely Alzheimer’s disease (AD) and vascular cognitive impairment and dementia (VCID) [6,7,8,9,10]. Additionally, hereditary small vessel diseases with cognitive deficits, namely cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) and cerebral autosomal recessive arteriopathy with subcortical infarcts and leukoencephalopathy (CARASIL), show loss of function of the HTRA1 or high-temperature requirement A serine peptidase 1 gene, which results in upregulation of TGFβ signaling [11,12]. In particular, immunohistochemical analysis of the cerebral small arteries in CARASIL patients shows increased TGFβ1 protein expression in the tunica media [11]. Moreover, alterations in TGFβ family signaling forms the basis for several vascular disorders in humans, including hereditary hemorrhagic telangiectasia [13,14,15,16] and primary pulmonary hypertension [17]. Importantly, accumulating lines of evidence point to a link between cerebrovascular health and TGFβ family signaling [6,7]. Increased risk of sporadic vascular dementia has been associated with the Pro10Leu single-nucleotide polymorphism (SNP) in the TGFβ1 gene [8], which is known to impact the TGFβ1 protein level [9].
TGFβ family members, including TGFβ1, are multifunctional cytokines that bind to type I, II, and III receptors [18]. Mouse models lacking TGFβ signaling components such as type I or II receptors (e.g., ACVRL1, TGFβRI, TGFβRII) die mid-gestation due to impaired vascular development [19]. Transgenic mice overexpressing a constitutively active form of TGFβ1 in the brain (TGF mice), originally developed to recapitulate the cerebrovascular pathology seen in AD [20], were later found to lack the cerebral amyloid angiopathy typical of AD [21,22] and, as such, were found to better recap the cerebrovascular pathology seen in VCID. Cerebrovascular structural abnormalities observed in TGF mice include thickened vascular wall; microvascular injury and degeneration, such as smaller capillary endothelial cells and pericytes, and abnormal chromatin condensation in endothelial cell nuclei; and string vessel pathology [20,21,23,24]. Functional abnormalities such as impaired vascular reactivity primarily related to endothelial-mediated dilatation, chronic cerebral hypoperfusion, and compromised neurovascular coupling are also hallmarks of TGF mice [23,24]. While TGF mice either do not develop cognitive deficits or do only in advanced age [25,26], they readily develop them when submitted to a comorbid cardiovascular risk factor for dementia, hence being a good model of VCID [27,28,29].
In recent years, -omics approaches, such as single-cell/nucleus transcriptomics and proteomics, have been used to profile the mammalian cerebrovasculature [30,31,32,33]. These approaches have provided insight into transcriptome- and proteome-level changes in brain vessels from AD patients and mouse models [34,35]. However, to date, VCID-related pathology of brain vessels lacks similar profiling. Addressing this gap in knowledge, we set out to (a) characterize the cerebrovascular proteome of TGF mice using mass spectrometry (MS)-based quantitative proteomics, as well as (b) identify proteins with biomarker potential in humans using an in silico bioinformatics approach. Given that proteins are regarded as effectors of biological functions, proteomics findings are generally considered directly suited for biomarker and drug development work.
2. Materials and Methods
2.1. Mice
Six-month-old transgenic TGF mice and their C57BL/6J wild-type (WT) littermates were used in this study. TGF mice overexpress a constitutively active form of TGFβ1 under the control of the glial fibrillary acidic protein (GFAP) promoter on a C57BL/6J background (line T64) [36]. To eliminate sex-related differences in brain structures [37] and potentially in the vasculature [38], only males were used. A total of 18 mice, in particular 9 TGF mice and 9 WT littermates, were employed based on expected variances and differences between groups by our previous and others’ studies [12,23,35]. Mice were housed under a 12 h light–dark cycle, in a room with controlled temperature (23 °C) and humidity (50%). Mice had access to tap water and food (Teklad Rodent chow, Research Diets Inc., New Brunswick, NJ, USA) ad libitum. All experiments were performed in compliance with the Animal Ethics Committee of the Montreal Neurological Institute and the Canadian Council on Animal Care guidelines, and complied with the ARRIVE 2.0 guidelines [39].
2.2. Surgical Extraction of Cerebral Arteries
The circle of Willis and major cerebral arteries along with their main branches were surgically removed from mice and individually stripped from the attached pia matter to obtain a clean preparation of vascular tissue, as previously described [33]. Arteries extracted from three mice were combined to constitute one biological replicate and stored at −80 °C. Three biological replicates (B1, B2, B3) were prepared for each of the two groups.
2.3. Cerebrovascular Proteomics Workflow
Protein extraction from mouse cerebral arteries was performed using a published and validated protocol [33]. Thereafter, the processing of samples for MS analysis, as well as the MS runs, preprocessing, and bioinformatics were performed without the knowledge of group allocation (i.e., WT or TGF). A brief description of the procedure is provided in Supplemental information.
2.4. Generation of Statistically Significant Protein Lists
Statistics were performed with the knowledge of group allocations using GraphPad Prism version 9.4.1. Specifically, proteins with altered levels between WT and TGF cerebral arteries were identified through parametric Student t and non-parametric Mann–Whitney U tests. The p-values were corrected for multiple testing using the Holm–Šídák method. Varying stringency was used to generate a database of two lists of proteins with altered levels between WT and TGF cerebral arteries. List 1 proteins were as follows: only proteins with p < 0.01, peptide score ≥ 35 (< 1% false discovery rate), and fold change ≥ 2 (up or down) were included, whereas peptides showing high variability (> 55%) among replicates were excluded. List 2, more stringent, consisted of List 1 proteins identified with > 2 peptides.
2.5. Characterization and Classification of Proteins
The gene associated with each identified protein was queried using the UniProt database [40] employing the UniProtKB accession number of each protein. Cellular Component Analysis and the PANTHER Overrepresentation Test were conducted using the PANTHER Classification System (PANTHER version 17.0 Released 22 February 2022, accessed 24 and 26 April 2022, respectively) [41,42] on the UniProtKB accession number of identified proteins, and with Mus musculus selected for the organism. For Cellular Component Analysis, the PANTHER GO-slim ontology annotation set was used, which contains 3361 terms—namely 2267 biological process, 550 molecular function and 544 cellular component terms (http://www.pantherdb.org/panther/goSlim.jsp, accessed on 26 April 2022). Fisher’s Exact test followed by False Discovery Rate (FDR) correction was used for PANTHER pathways overrepresented in genes associated with identified proteins in mouse brain vessels compared to the entire Mus musculus genome. The PANTHER pathway database consists of 177, mainly regulatory, signaling pathways. Protein interactors of TGFβ1 were identified by querying the BioGrid database, the IntAct Molecular Interaction database (http://www.ebi.ac.uk/intact/, accessed on 26 April 2022) [43], and an in-house database [35] that is a compendium of several databases, including BIND, BioGRID, HPRD, HIMAP, and EcoCyc databases. Protein interactions were restricted to those observed in Mus musculus and/or Homo sapiens.
2.6. Comparison against Public Transcriptomics Datasets
Published single-cell transcriptomics datasets were examined to demonstrate that RNA transcripts of proteins identified were also present in mouse and/or human brain vascular cells. Analyses were performed on List 2 proteins only. For relative gene expression levels of proteins in mouse brain vascular cell types (e.g., endothelial, smooth muscle cells), two mouse cerebrovascular single-cell transcriptomics datasets [31,44] were downloaded from the NCBI GEO repository [45], and each gene was ranked by its relative abundance. For correlation between mouse and human relative gene expression in brain vascular endothelial cells, we used the dataset compiled by Yang and colleagues [34]. List 2 proteins were also compared for (a) common pathways across three publicly available databases, notably KEGG (https://www.genome.jp/kegg/, accessed on 16 November 2023), Reactome (https://reactome.org/, accessed on 16 November 2023), and PANTHER, and (b) molecular functions and biological processes, between humans and mice using the Uniprot database [40].
2.7. Comparison against the Public Human Extracellular Vesicles (EV) Database
Vesiclepedia [46], an extracellular vesicle (EV) database version 5.1, was used to identify List 1 and 2 proteins detected in the TGF cerebrovasculature and also detected in human EVs. These proteins constitute a rich source of brain vasculature-specific biomarkers, as well as receptors known for delivering molecules across the blood–brain barrier.
2.8. Proteomics of Plasma and Plasma EVs
Human plasma from 13 healthy consenting individuals (7 male and 6 female) was purchased from BioIVT (Westbury, NY, USA; bioivt.com) and used for proteomics analysis. Five hundred (500) µL of each type of human plasma was precleared by centrifugations at 1500× g for 10 min and at 10,000× g for 10 min. Precleared plasma (supernatant) was used for abundant protein depletion or total EV isolation. For depletion of abundant proteins, 10 µL of precleared plasma was loaded onto High-Select™ Top14 Abundant Protein Depletion spin columns (ThermoFisher, Waltham, MA, USA; catalog # A36369) and flowthrough collected as per manufacturer’s instructions. For isolation of total EVs, 150 μL of precleared plasma was loaded onto qEVsingle 35 nm sized exclusion chromatography columns (IZON, Westbury, MA, USA; product code # ICS-35), and total EVs were isolated as per manufacturer’s instructions. The precleared (or undepleted) plasma, depleted plasma, and total EV fractions (200 µL of fractions 6–8) were analyzed by proteomics as recently described [47]. EV isolation was confirmed by detection of proteins from the “Top 100 EV Proteins” list in the Vesiclepedia database. Additional MISEV guidelines were also followed.
2.9. Formatting Guideline Used for Genes and Proteins
For ease of reading, we used the gene symbol for proteins. In accordance with the organism-specific formatting guidelines, mouse proteins (indicated by their gene symbols as mentioned above) have the first letter in upper-case (e.g., Acta2), while human proteins were fully capitalized (e.g., ACTA2). When specifically indicating a gene, the symbols were italicized (e.g., Acta2, ACTA2).
3. Results
3.1. Characterization of Proteins Detected in Mouse Brain Vessels
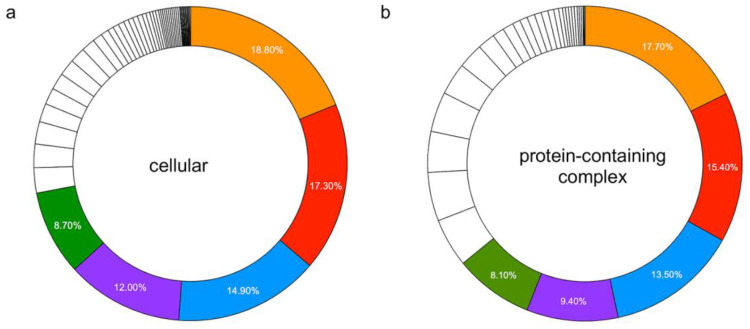
We identified 3602 proteins from high-quality peptides (peptide score ≥ 35) in brain vessels of WT and TGF mice. Identified proteins included canonical vascular proteins, such Claudin-5 (Cldn5), Solute carrier family 2 (Slc2a1), and von Willebrand factor (Vwf). Using the UniProt database, it was determined that the majority of proteins identified (n = 3575; 99.3%) were products of known genes. Cellular Component Analysis, conducted using the PANTHER Classification System, found 2785 component hits in two main categories: cellular (n = 2167 genes) and/or protein-containing complex (n = 618 genes). The top five cellular components were intracellular anatomical structures (n = 1624 genes), membrane (n = 1495 genes), organelle (n = 1290 genes), cytoplasm (n = 1037 genes), and cell periphery (n = 754 genes), the latter defined as part of a cell encompassing the (a) cell cortex cell region just beneath the plasma membrane and often containing a network of actin filaments and associated proteins, (b) the plasma membrane, and (c) any external encapsulating structures (Figure 1a). The top five protein-containing complex components were catalytic (n = 181 genes), nuclear (n = 157 genes), membrane (n = 138 genes), ribonucleoprotein (n = 96 genes), and intracellular (n = 83 genes) (Figure 1b).
Figure 1.
Percent distribution of the top 5 cellular and protein-containing complex components. Percentages represent the percent of gene hit against the total number of component hits in (a) cellular (n = 69 components): ▋ intracellular anatomical structures; ▋ membrane; ▋ organelle; ▋ cytoplasm; ▋ cell periphery; (b) Protein-containing complex (n = 32 components): ▋ catalytic; ▋ nuclear; ▋ membrane; ▋ ribonucleoprotein; ▋ intracellular.
Using the PANTHER Overrepresentation Test, we identified seven pathways to be significantly (p < 0.05, FDR corrected) overrepresented at a > 2-fold enrichment (FEn) in mouse brain vessels, relative to the entire Mus musculus genome. These comprised pathways involved in (a) vasomotor regulation, namely endothelin signaling (FEn = 2.37) and 5-hydroxytryptamine/serotonin degradation (FEn = 3.21) pathways, the integrin signaling pathway (FEn = 2.79), and cytoskeletal regulation by Rho GTPase (FEn = 2.77), and (b) cellular metabolism/energetics, namely the tricarboxylic acid cycle (FEn = 4.10), glycolysis (FEn = 3.59), and the insulin/IGF pathway–protein kinase B signaling cascade (FEn = 2.53).
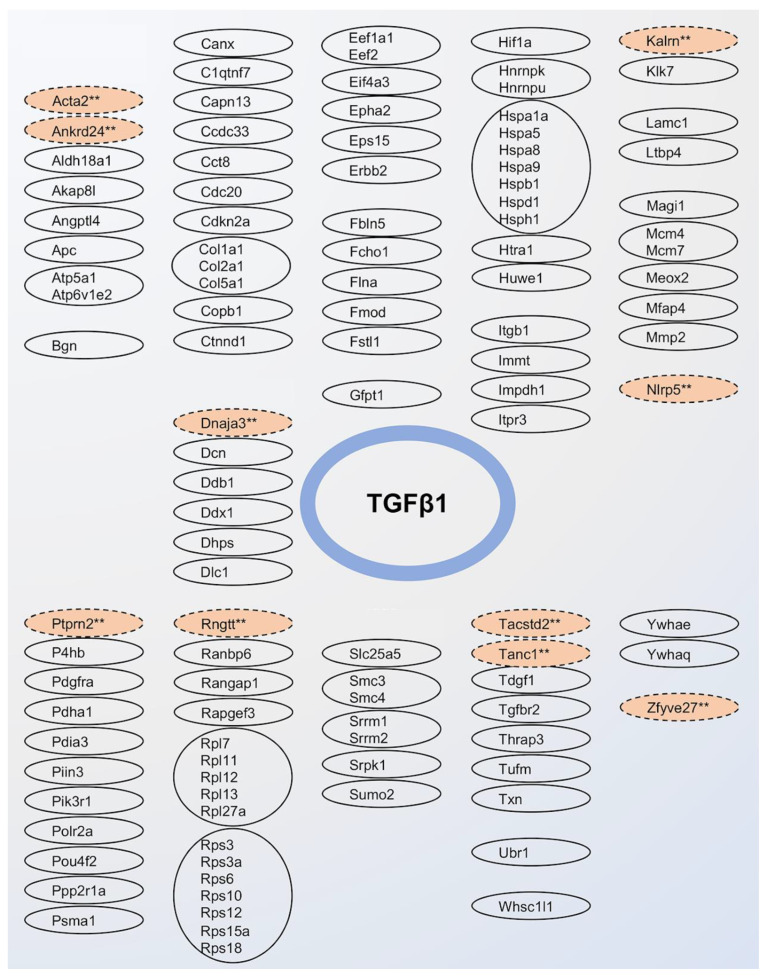
In our list of 3602 proteins, we identified 102 (2.8%) direct interactors of TGFβ1, with ≥ 3 interactors detected from the following protein families: collagen (Col), heat shock proteins (Hsp), and large (Rpl) and small (Rps) ribosomal proteins (Figure 2). We also identified 1942 (53.9%) indirect interactors of TGFβ1.
Figure 2.
Protein interactors of TGFβ1. Solid circles indicate direct interactors, and dashed circles indicate indirect interactors. Protein interactors belonging to the same family of proteins are grouped together. Salmon colors depict TGFβ1 interactors with significant (p ≤ 0.01, denoted as ** in the figure) 2-fold level change in the cerebrovasculature of TGF mice.
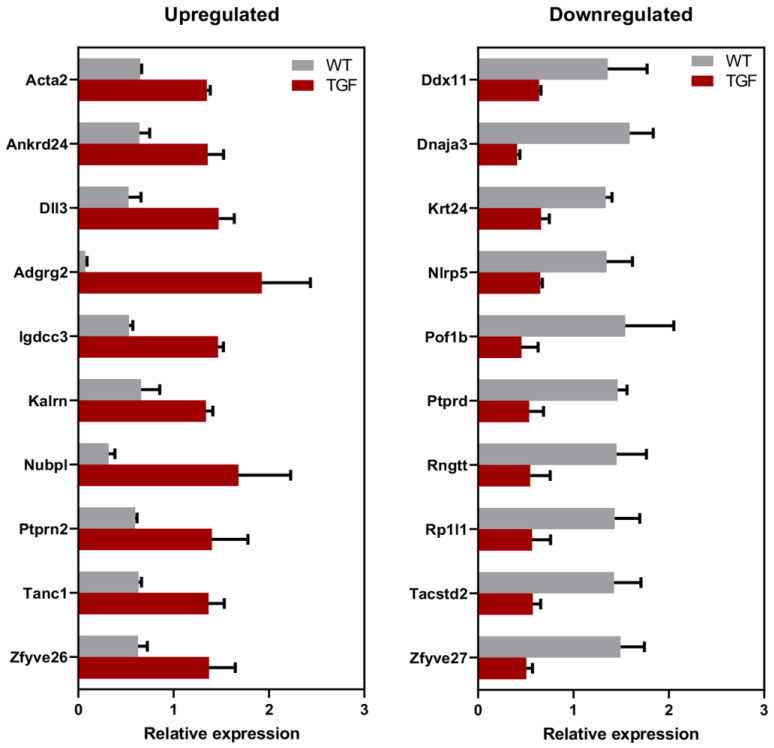
3.2. Proteins with Altered Levels in the Brain Vessels of TGF and WT Mice
Compared to WT mice, 60 proteins (1.7%) showed significantly altered levels (p ≤ 0.01 and twofold change) in the arteries of TGF mice. These 60 proteins constituted List 1 proteins (Supplemental Table S1). Of these, 20 proteins were significantly (p < 0.01) detected with ≥ 2 peptides, with 10 showing level increases (Acta2, Ankrd24, Dll3, Adgrg2, Igdcc3, Kalrn, Nubpl, Ptprn2, Tanc1, Zfyve26), and 10 showing decreases (Ddx11, Dnaja3, Krt24, Nlrp5, Pof1b, Ptprd, Rngtt, Rp1l1, Tacstd2, Zfyve27) (Figure 3, Supplemental Table S1). These 20 proteins constituted List 2 proteins (see full names of proteins in Table 1). Half (n = 10) of List 2 proteins were indirect interactors of TGFβ1 (Figure 2).
Figure 3.
Relative expression of List 2 proteins in TGF brain vessels. Proteins with significantly altered levels in brain vessels of TGF mice relative to WT detected using the highest stringency in our database (p ≤ 0.01, 2-fold change, and ≥ 2 peptides) constitute List 2 proteins (n = 20).
Table 1.
Biomarker potential List 2 proteins detected in human extracellular vesicles. We note that the gene symbols of proteins are capitalized in accordance with the organism-specific formatting guidelines—in this case, indicating human proteins. The “X” denotes that a protein is present and/or has been identified. Abbreviations: EV, extracellular vesicle; HBEC, human brain endothelial cells; p, protein; r, mRNA.
| ID (Human) |
Common Name | Vesiclepedia Identified Molecule | Reported Detected in Vascular Cell and/or Blood, to Date | Type | |||||
|---|---|---|---|---|---|---|---|---|---|
| Vascular [Ref. ID] | Blood [Ref. ID] | Primary HBEC | HBEC EV | Plasma (Depleted) | Plasma EV | ||||
| p | r | ||||||||
| ACTA2 | Actin Alpha 2 | X | X | Endothelial [48,49] | Plasma [50,51] | X | X | X | X |
| ANKRD24 | Ankyrin Repeat Domain 24 | X | - | - | |||||
| DLL3 | Delta-Like Canonical Notch Ligand 3 | X | X | - | - | X | |||
| ADGRG2 (GPR64) | Adhesion G Protein-Coupled Receptor G2 (also known as G Protein-Coupled Receptor 64) | X | X | - | - | ||||
| IGDCC3 | Immunoglobulin Superfamily, DCC Subclass, Member 3 | X | - | - | X | ||||
| KALRN | Kalirin RhoGEF Kinase | X | X | - | Plasma [52] | X | |||
| NUBPL | Nucleotide Binding Protein-Like | X | X | - | - | ||||
| PTPRN2 | Protein Tyrosine Phosphatase, Receptor Type N2 | X | - | - | |||||
| TANC1 | Tetratricopeptide Repeat, Ankyrin Repeat, and Coiled-Coil Containing 1 | X | X | - | - | X | X | X | |
| ZFYVE26 | Zinc Finger FYVE-Type Containing 26 | X | X | - | - | X | |||
| DDX11 | DEAD/H-Box Helicase 11 | X | X | - | - | X | |||
| DNAJA3 | DnaJ Heat Shock Protein Family (Hsp40) Member A3 | X | X | - | - | ||||
| KRT24 | Keratin 24 | X | X | - | Plasma [50] | X | X | ||
| NLRP5 | NOD-like Receptor Family Pyrin Domain Containing 5 | - | - | X | |||||
| POF1B | POF1B Actin Binding Protein | X | - | - | |||||
| PTPRD | Protein Tyrosine Phosphatase Receptor Type D | X | - | - | X | X | |||
| RNGTT | RNA Guanylyltransferase And 5′-Phosphatase | X | X | - | - | ||||
| RP1L1 | Retinitis Pigmentosa 1-like 1 | - | - | X | |||||
| TACSTD2 | Tumor Associated Calcium Signal Transducer 2 | X | Endothelial [53] | - | |||||
| ZFYVE27 | Zinc Finger FYVE-Type Containing 27 | X | X | - | - | ||||
3.3. Comparison against Published Transcriptomics in Mouse Brain Vascular Cells
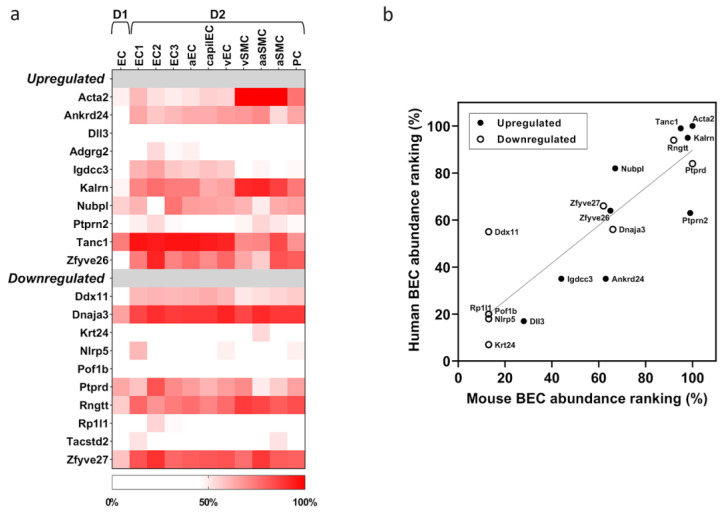
Examination of published single-cell transcriptomics data demonstrated that RNA transcripts of the above-mentioned 20 List 2 proteins are present in one or more cell types of the mouse brain vasculature. Abundance ranking of their gene expression in two separate single-cell transcriptomics databases, ranging from low (< 30%) to very high (> 90%), are shown in Figure 4a and Supplemental Figure S1. Comparison of transcripts in the arterial endothelial cell (aEC) and arterial smooth muscle cell (aSMC) categories identified 11/20 of these transcripts to be present in both cell types (Acta2, Ankrd24, Kalrn, Nubpl, Tanc1, Zfyve26, Ddx11, Dnaja3, Ptprd, Rngtt, Zfyve27) with an abundance ranking of ≥ 50% (indicating moderate to high abundance). In contrast, 1/20 transcript (Igdcc3) and 2/20 transcripts (Ptprn2, Tacstd2) demonstrated an abundance ranking of ≥ 50% in aEC and aSMC, respectively.
Figure 4.
Relative gene expression of List 2 proteins in public vascular datasets. (a) Relative gene expression of the 20 List 2 proteins in mouse cerebrovascular single cell transcriptome databases D1 [44] and D2 [31]. Abbreviations: EC, endothelial cell; aEC, arterial EC; capilEC, capillary EC; vEC, venular EC; vSMC, venular smooth muscle cell; aaSMC, arteriole SMC; aSMC, arterial SMC; PC, pericyte; (b) Correlation between mouse and human relative gene expression of the 20 List 2 proteins in brain vascular endothelial cells. Upregulated and downregulated proteins are shown as closed and open symbols, respectively. Solid line represents the linear regression (Pearson r2 = 0.64, p < 0.001) and dotted lines are 99% confidence bands.
3.4. Translatability of Findings to Human
To demonstrate the translatability of our findings (i.e., differentially expressed mouse proteins are also expressed in human brain vasculature), the relative gene expressions of our List 2 proteins were compared in public RNAseq databases between human and mouse brain vascular endothelial cells. Most (n = 18) of the proteins showed similar gene expression in the two species as demonstrated by a strong correlation (Pearson r2 = 0.64, p < 0.001) in the expression ranking between humans and mice (Figure 4b). It was determined using three databases (KEGG, Reactome, PANTHER) that 11/18 proteins have common pathways (Table 2). In addition, we also compared molecular functions and biological processes between humans and mice using the Uniprot database and found that the majority of these functions and processes overlap between the two species (Supplemental Figure S4; Supplemental Table S3). Additionally, List 2 proteins were examined in proteomics datasets from human brain endothelial cells [54,55,56], which is part of the BBB Carta project [54]. Out of the 20 List 2 proteins, 6 were detectable in human brain endothelial cells, including ACTA2, DLL3, TANC1, NLRP5, PTPRD, and RP1L1.
Table 2.
Summary of common pathways for the 20 List 2 significant proteins in mice and humans. The databases used for pathway comparison were KEGG (blue), Reactome (green), and PANTHER (orange). The colors of the arrows in the “Common” column identify a specific pathway. Italic writing indicates that the pathway is specific to humans (i.e., cellular responses to stimuli for DDX11) and underlined writing indicates that the pathway is specific to mice (i.e., disease for RNGTT) for the protein in question. Abbreviations: KEGG, Kyoto Encyclopedia of Genes and Genomes; Reactome, Reactome Pathway Database; PANTHER, Protein Analysis Through Evolutionary Relationships.
| Protein | KEGG | Reactome | PANTHER | Common |
|---|---|---|---|---|
| ACTA2 | Vascular smooth muscle contraction | Muscle contraction | Alzheimer disease—presinilin | ✓ ✓ ✓ |
| Motor proteins | Signal transduction | Signaling | ||
| Apelin signaling pathway | - | Inflammation | ||
| Relaxin signaling pathway | - | Cytoskeletal regulation by Rho GPTase | ||
| ANKRD24 | - | - | - | |
| DLL3 | Endocrine resistance | Developmental biology | Angiogenesis | ✓ ✓ ✓ |
| Notch signaling pathway | - | Notch signaling pathway | ||
| Th1 Th2 cell differenciation | - | - | ||
| Pathways in cancer | - | - | ||
| ADGRG2 | - | - | - | |
| IGDCC3 | - | - | - | |
| KALRN | - | Developmental biology | - | ✓ |
| - | Signal transduction | - | ||
| NUBPL | - | Metabolism | - | ✓ |
| PTPRN2 | Type 1 diabetes mellitus | Immune system | - | ✓ ✓ |
| TANC1 | - | - | - | |
| ZFYVE26 | - | - | - | |
| DDX11 | Cell cycle | Cellular responses to stimuli | - | ✓ |
| DNAJA3 | Viral carcinogenesis | - | - | ✓ |
| KRT24 | Estrogen signaling pathway | Developmental biology | - | ✓ ✓ |
| Staphylococcus aureus infection | - | - | ||
| NLRP5 | - | - | - | |
| POF1B | - | - | - | |
| PTPRD | Cell adhesion molecules | Neuronal system | - | ✓ ✓ |
| RNGTT | mRNA surveillance pathway | Gene expression | - | ✓ ✓ |
| - | Metabolism of RNA | - | ||
| - | Disease | - | ||
| RP1L1 | - | - | - | |
| TACSTD2 | - | - | - | |
| ZFYVE27 | Endocytosis | - | - | ✓ |
3.5. Blood Biomarker Potential in Human
Using a publicly available database, Vesiclepedia, we demonstrated that 80% (n = 16) of the 20 List 2 differentially expressed proteins in the TGF cerebrovasculature were detected in human EVs (Table 1), with several detected in easily accessible biofluids (e.g., plasma [50,51,52]). In addition, Acta2 and Tacstd2 were detected in EVs secreted by vascular endothelial cells [48,49,53]. Acta2 was also detected in EVs secreted by human blood–brain barrier cells [55]. Overall, 70% (n = 42) of the 60 TGF List 1 differentially expressed proteins (which includes List 2 proteins) were detected in human EVs in Vesiclepedia (Supplemental Table S1).
In addition, the 20 proteins in List 2 were also validated in the proteome of healthy human plasma to demonstrate their biomarker potential in humans. Depletion of abundant proteins from plasma was necessary to detect the presence of some of these proteins by proteomics. At least four of the List 2 proteins (ACTA2, KRT24, TANC1, and IGDCC3) were detectable in depleted human plasma (Table 1). An example of an extracted ion chromatogram and an MS/MS spectrum for a TANC1 peptide in non-depleted and depleted plasma is shown in Supplemental Figure S2a,b.
Total EVs were also isolated from these plasma samples using size-exclusion chromatography and analyzed by proteomics. EV isolation was confirmed by detection of more than 60 EV proteins, which were mostly absent in the undepleted plasma samples (Supplemental Table S2). At least seven of the List 2 proteins (ACTA2, KALRN, TANC1, ZFYVE26, DDX11, KRT24, and PTPRD) were detectable in the total plasma EVs. Examples of extracted ion chromatograms and MS/MS spectra for the peptides of ACTA2 and KALRN in plasma and total EVs are shown in Supplemental Figure S3a–d.
4. Discussion
TGF mice overexpress a constitutively active form of TGFβ1 in brain astrocytes and recapitulate aspects of the cerebrovascular pathology seen in VCID and AD (but not the amyloid pathology). Particularly, they display thickened vascular walls due to accumulation of extracellular matrix proteins, string vessel pathology, impaired dilatory function, cerebral hypoperfusion, neurovascular uncoupling, and cerebral microhemorrhages [20,21,23,57,58]. Here, we demonstrate that the cerebrovascular proteome is significantly altered in TGF mice. Specifically, 60 proteins (1.7% of total identified proteins in WT mice) showed significant altered levels (p ≤ 0.01 and twofold change) in the cerebral arteries of TGF mice compared to those of WT littermates. We focus our discussion on how level perturbations in List 2 proteins (n = 20), identified using stringent criteria from the 60 List 1 proteins, relate to the cerebrovascular abnormalities seen in TGF mice, in particular perturbation in vasomotricity, remodeling, and inflammation.
4.1. Perturbation in Vascular Tone and Vasomotricity
We identified three proteins with altered levels in the TGF cerebral vasculature, namely Acta2, Tacstd2, and Tanc1, that are known to influence vascular tone.
4.1.1. Increased Vascular Tone
The contraction of blood vessels in response to the stretch resulting from pulsatile blood flow is dependent on the interaction between thin and thick myofilaments, composed of Acta2 (or α-2 actin) and β-myosin, respectively [59,60]. Increased Acta2 level in the TGF cerebrovasculature likely increases vascular tone, hence contributing to the impaired vasomotricity observed in brain arteries of TGF mice [23]. Our finding of increased Acta2 levels in the TGF cerebral arteries parallels observations in peripheral arteries, where the overactivation of TGFβ1 signaling stimulates the expression of smooth muscle contractile genes, including ACTA2 [61,62]. Additional evidence linking Acta2 to the regulation of vascular tone includes (a) the observation that Acta2-null-mice demonstrate compromised vascular tone, contractility, and blood flow [63], and (b) the dilative phenotype found in ACTA2 missense mutations seen in cerebral arteriopathy in humans [64].
4.1.2. Attempt to Compensate by Promoting Vasodilation
In contrast to the vasocontractile phenotype promoted by upregulated Acta2, decreased Tacstd2 protein levels in the TGF cerebrovasculature point to an attempt at promoting vasodilation via modulation of Ca2+ levels. Tacstd2 is known to increase Ca2+ levels in the cytosol by inducing its release from internal stores [65,66], which increases vascular smooth muscle contractility [33]. Therefore, a decrease in Tacstd2 level promotes vasodilation. Tanc1, demonstrating increased levels in TGF brain vessels, is an indirect interactor of TGFβ1 [67], and a scaffold protein associated with regulation of excitatory (e.g., glutamatergic) synapse strength in both brain and non-brain tissue [68,69]. It is, therefore, possible that increased levels of Tanc1 is an attempt to promote blood vessel dilation via modulation of neurogenic signaling [70]. Indeed, Tanc1 has been shown to interact with NMDA (N-methyl-D-aspartate) and AMPA (α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid) glutamate receptor subunits encoded by GRIN2B and GRIA1 [71], and present in cerebral blood vessels [33,72].
In addition to the three proteins known to influence vascular tone, we also detected decreased levels of the ATP-dependent DNA helicase Ddx11, an alteration likely related to the contractile phenotype associated with chronic cerebral hypoperfusion in TGF mice [29,57,58]. Supporting this is the observation that in the vascular endothelium in humans, the DDX11 gene is repressed under hypoxic conditions [73].
4.2. Cerebrovascular Remodeling
Remodeling of the cerebrovasculature is a key phenotypic feature of TGF mice [20,21,23,24]. In general, vascular remodeling is the process of altering blood vessel structure and arrangement via cell growth, proliferation, migration, death, and/or the production or degradation of the extracellular matrix [74]. Similar to the remodeling observed in TGF brain vessels, increase in the TGFβ1 level is known to promote aspects of vascular modeling, such as a proliferative phenotype, in peripheral arteries, as demonstrated (a) in cultured vascular smooth muscle cells from human pulmonary artery [75] and (b) in murine carotid artery vascular media due to localized overexpression of TGFβ1 in the endothelium [76]. We found that 11 of the 20 proteins with altered levels in the TFG cerebral vasculature were known influencers of vascular remodeling, namely Dll3, Adgrg2, Krt24, Ptprd, Ptprn2, Igdcc3, Rngtt, Rp1l1, Tacstd2, Zfyve26, and Zfyve27. Below, we highlight their specific links with processes contributing to vascular remodeling.
4.2.1. Vascular Remodeling via Promotion of Cell Proliferation
Recent literature suggests that TGFβ1 overexpression can upregulate the expression of several Notch signaling pathway proteins [77]. Indeed, an increase in Dll3 level, a core member of the canonical Notch signaling pathway, was observed in TGF vessels. Dll3 binds to the Notch family of receptors (Notch1 to 4) [78], of which Notch1 and Notch4 were detected in cerebral arteries of TGF and WT mice. In humans, an elevated DLL3 level has been linked with pathological angiogenesis via the DLL3/NOTCH4 signaling pathway [79]. Adgrg2, a G-protein coupled receptor, was increased in brain vessels of TGF mice. The literature indicates that G-protein coupled receptor signaling may play a role in arterial smooth muscle cell transformation [80]. In line with this, upregulation in ADGRG2 transcripts has been reported during the transformation of quiescent human coronary artery smooth muscle cells to a proliferative and migratory phenotype observed in atherosclerosis [80]. Cytokeratin Krt24, a known anti-proliferative factor in the epidermis [81,82], was decreased in the TGF cerebrovasculature. Given that differential expression of cytokeratins has been observed in vascular smooth muscle cells, often in the setting of a proliferative state [83], a decreased Ktr24 level likely contributes to cell proliferation and remodeling. Decreased Ptprd and increased Ptprn2 levels were also found in the TGF cerebrovasculature. These two proteins belong to the protein tyrosine phosphatase family of signaling molecules that regulate cellular processes, including differentiation and proliferation [84]. A decreased Ptprd protein level in a peripheral artery (i.e., pulmonary, rodent) was found to alter vascular smooth muscle cell morphology and migration, primarily via focal adhesion and cell cytoskeleton modulation [85]. Protein Ptprn2 is a direct interactor of SMADs [86], the main downstream signal transducers for the TGFβ superfamily receptors. Variations in the PTPRN2 gene have been associated with calcified atherosclerotic plaque, a subclinical marker of atherosclerosis, in human peripheral arteries [87,88], and familial stroke [89]. Increase in Ptprn2 (or human PTPRN2) protein level is also known to perturb the lipid-dependent sequestration of an actin-remodeling factor [90], a process capable of facilitating vascular remodeling. While the exact role of Igdcc3 (or human IGDCC3) protein in brain vessels is unknown, its gene expression pattern strongly overlaps with regions of high Wnt activity during embryonic development [91], suggesting that its increase in the TGF cerebrovasculature may be associated with a proliferative phenotype [92].
4.2.2. Attempt to Attenuate Vascular Remodeling
Levels of proteins Rngtt, Rp1l1, Tacstd2, Zfyve26, and Zfyve27, which are known to promote a proliferative phenotype in various cancers, were decreased in the brain vasculature of TGF mice, likely as an attempt to attenuate vascular proliferation and remodeling. Reduction in the Rngtt level, a protein that caps nascent mRNA [93], has been shown to compromise the activity of Wnt3a/β-catenin [94] and Hedgehog [95] pathways, both involved in a proliferative phenotype in the vessel wall [92,96]. Commonly associated with retinal degeneration, the RPL11 gene has also been associated with brain arteriovenous malformations [97] and cancer [98,99] in humans. Similarly, expression of the TGFβ1 response gene, TACSTD2 (or TROP2) [100], in cancer tissue (e.g., human glioma) has been shown to correlate with microvessel density—a commonly used marker for estimation of angiogenesis [101,102]. In addition, by conducting experiments in both humans and mice, Guo et al. demonstrated that Tacstd2 (or human TACSTD2) promotes the expression of MMP13 and PECAM1, two well-known angiogenesis factors, via activation of ERK-1 and -2 signaling pathways [103]. With regard to Zfyve26, decreased levels in mice are known to disrupt endolysosomal membrane trafficking [104], which in turn can exacerbate vascular calcification [105]. Therefore, its increase in the TGF cerebrovasculature may be a compensatory attempt at attenuating remodeling. Zfyve27 (or human ZFYVE27) was recently found to promote endothelial cell migration and angiogenesis in humans, with its knockdown affecting these processes [106].
4.3. Chronic Inflammation
While TGFβ1 has been known to function both as an anti- and a pro-inflammatory cytokine [107], a pro-inflammatory phenotype has been observed in TGF mice [24,108], including inflammation of brain vessels characterized by activated perivascular astrocytes and microglial cells [21]. TGFβ1 is known to stimulate the production of reactive oxygen species (ROS) in vascular cell types, including endothelial and smooth muscle cells [109,110]. ROS are free radicals derived from molecular oxygen, and their overproduction in the cerebrovasculature contributes to the inflammatory response [111] and promotes dysfunction by shifting cell bioenergetics [112]. Six of the twenty proteins with altered levels in the TFG cerebral vasculature, namely Nlrp5, Pof1b, Kalrn, Nubpl, Dnaja3, and Ankrd24, had links to inflammation, as described below.
4.3.1. Proteins Indicative of an Inflammatory Process
Decreases in Nlrp5 and Pof1b levels were observed in TGF brain vessels. Nlrp5 (or human NLRP5) belongs to a class of cytoplasmic pattern recognition receptors [113] and is known to be expressed in both mouse and human cerebrovasculature, largely in endothelial cells [31,114] and pericytes [31,115]. Given that treatment with hydrogen peroxide (an endogenous ROS) decreases the expression of NLRP5 in human cerebral endothelial cells, its decrease in the TGF cerebrovasculature may indicate ROS overproduction and an inflammatory environment [114]. With regard to Pof1b (or human POF1B), its gene expression in blood has been associated with ischemic stroke in humans [116]. POF1B is also known to be highly expressed in epithelial cells with tight junctions, where it localizes at tight junctions and regulates cytoskeleton dynamics [117]. In the vasculature, Pof1B/POF1B expression has been observed in endothelial cells and pericytes [31,34,44], and may contribute to the regulation of the blood–brain barrier permeability, similar to its function in the epithelium. Its decrease in the TGF cerebrovasculature may indicate a compromised blood–brain barrier and an inflammatory environment.
4.3.2. Attempt at Reducing Inflammation
Altered levels of proteins Kalrn, Dnaja3, Nubpl, Spen, and Ankrd24 may suggest compensatory attempts at reducing inflammation in the TGF cerebrovasculature. An increased Kalrn level was found in TGF brain vessels. In humans, KALRN, a guanine nucleotide exchange factor, is known to associate with and down-regulate inducible nitric oxide synthase (iNOS) activity, and thereby the production of nitric oxide, a free radical [118,119]. Interestingly, polymorphisms in the KALRN gene have been associated with an increased risk of both cerebrovascular and cardiovascular diseases, including ischemic stroke [120] and coronary artery disease [119,121,122]. Perturbed levels of mitochondrial proteins Dnaja3 and Nubpl may also be an attempt at attenuating inflammation in the TGF cerebrovasculature via (a) decreased Dnaja3-associated dampening of innate immunity [123] and (b) increased Nubpl-associated dampening of ROS production [124]. While little is known about Ankrd24, it can interact with nuclear factor kappa B (NF-κB) [43], a transcriptional activator of inflammatory mediators. Direct interaction of Ankrd24 with NF-κB may serve a similar function as the interaction of the stress response protein Ankrd2 with NF-κB repressor subunit p50, which results in potent repression of inflammatory responses [125]. Interestingly, vasomotor impairment in TGF cerebral arteries was restored by the nonsteroidal anti-inflammatory drug (NSAID) indomethacin and pioglitazone [108], the latter likely via activation of PPARγ receptors in brain vessels and reduction in NF-κB and IL-6 levels [126].
4.3.3. Blood Biomarker and Translatability to Humans
In our study, we confirmed the presence of four List 2 proteins (ACTA2, KRT24, TANC1, and IGDCC3) in depleted human plasma and seven List 2 proteins (ACTA2, KALRN, TANC1, ZFYVE26, DDX11, KRT24, and PTPRD) in total plasma EVs. These findings hold significant promise for blood biomarker research, diagnostics, and treatment, particularly in the investigation of vascular brain injury in age-related dementias. Notably, a recent review [127] underscores the emerging role of EVs in blood plasma as biomarkers in age-related dementias, further emphasizing the importance of our results.
5. Conclusions
By performing MS-based vascular proteome profiling in a mouse model of cerebrovascular pathology related to VCID, we identified multiple proteins demonstrating significantly altered levels. Level dysregulation in these proteins points to perturbations in brain vessel vasomotricity, remodeling, and inflammation. We further demonstrated that several of the differentially expressed mouse proteins are (a) expressed in human brain vasculature and (b) found as cargo proteins in EVs from human plasma. Given the growing popularity of EVs in blood as a novel and minimally invasive biomarker discovery platform for age-related dementias, several of the proteins identified in our study using MS can serve as VCID protein biomarkers in humans.
Acknowledgments
We thank L. Tessier, S. Williamson, and K. Chan (HHT-National Research Council Canada) for their technical assistance with mass spectrometry.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/biology12121500/s1, Figure S1: Relative gene expression of List 2 proteins in public vascular datasets; Figure S2: Examples of extracted ion chromatograms and MS/MS spectra in precleared plasma and depleted plasma; Figure S3: Examples of extracted ion chromatograms and MS/MS spectra in precleared plasma and total plasma EVs; Figure S4: The figure shows the reproducibility between two biological runs of control animals (top panel) and between control and TGFbeta runs (bottom panel). The median relative standard deviation among replicates of control and TGFbeta is 10.1% and 15.7%, respectively and between control and TGFbeta samples is 26%; Table S1: List 1 and List 2 proteins; Table S2: EV markers detected; Table S3: Molecular Functions and Biological Processes of List 2 Proteins in Mice and Human. References [128,129,130] are cited in the supplementary materials.
Author Contributions
Conceptualization, A.B.; methodology, A.S.H., A.T.S., C.E.D. and A.B.; software, A.S.H., Z.M., A.T.S. and A.B.; validation, A.S.H., Z.M., A.T.S. and A.B.; formal analysis, A.S.H., Z.M., A.T.S., F.E.D. and A.B.; writing—review and editing, A.S.H., Z.M., A.T.S., F.E.D., C.E.D., D.B.S., E.H. and A.B.; visualization, A.S.H., Z.M., F.E.D. and A.B.; supervision, A.B.; funding acquisition, A.S.H., E.H. and A.B. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
All experiments were approved by the Animal Ethics Committee of the Montreal Neurological Institute (approval codes: 2007-5385; 2007-5471), and complied with the Canadian Council on Animal Care and the Animal Research: Reporting In Vivo Experiments (ARRIVE) guidelines.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data available upon request to the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by Canadian Institutes of Health Research (CIHR-MOP-126001) to E.H.; NRC Ideation New Beginnings grant to A.S.H. and A.B. (2019–2020); the Fonds de Recherche Québec—Santé (FRQS: Chercheur boursiers Junior 1, 2020–2024), and the Fonds de soutien à la recherche pour les neurosciences du vieillissement from the Fondation Courtois to A.B.; Vascular Training Platform (VAST, 2023–2024) to Z.M.; Bourse de Mérite de la faculté de Médecine de l’Université de Montréal (2021–2022) and the Fonds de Recherche Québec—Santé (FRQS; Bourse de formation de maîtrise, 2022–2023) to F.E.D.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Iadecola C. The Neurovascular Unit Coming of Age: A Journey through Neurovascular Coupling in Health and Disease. Neuron. 2017;96:17–42. doi: 10.1016/j.neuron.2017.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cauli B., Hamel E. Revisiting the role of neurons in neurovascular coupling. Front. Neuroenergetics. 2010;2:9. doi: 10.3389/fnene.2010.00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iadecola C. The Pathobiology of Vascular Dementia. Neuron. 2013;80:844–866. doi: 10.1016/j.neuron.2013.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jellinger K.A. Pathology and pathogenesis of vascular cognitive impairment-a critical update. Front. Aging Neurosci. 2013;5:17. doi: 10.3389/fnagi.2013.00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gorelick P.B., Scuteri A., Black S.E., Decarli C., Greenberg S.M., Iadecola C., Launer L.J., Laurent S., Lopez O.L., Nyenhuis D., et al. Vascular contributions to cognitive impairment and dementia: A statement for healthcare professionals from the american heart association/american stroke association. Stroke. 2011;42:2672–2713. doi: 10.1161/STR.0b013e3182299496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.ten Dijke P., Arthur H.M. Extracellular control of TGFbeta signalling in vascular development and disease. Nat. Rev. Mol. Cell Biol. 2007;8:857–869. doi: 10.1038/nrm2262. [DOI] [PubMed] [Google Scholar]
- 7.Kandasamy M., Anusuyadevi M., Aigner K.M., Unger M.S., Kniewallner K.M., de Sousa D.M.B., Altendorfer B., Mrowetz H., Bogdahn U., Aigner L. TGF-β Signaling: A Therapeutic Target to Reinstate Regenerative Plasticity in Vascular Dementia? Aging Dis. 2020;11:828–850. doi: 10.14336/AD.2020.0222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim Y., Lee C. The gene encoding transforming growth factor beta 1 confers risk of ischemic stroke and vascular dementia. Stroke. 2006;37:2843–2845. doi: 10.1161/01.STR.0000244782.76917.87. [DOI] [PubMed] [Google Scholar]
- 9.Martelossi Cebinelli G.C., Paiva Trugilo K., Badaró Garcia S., Brajão de Oliveira K. TGF-β1 functional polymorphisms: A review. Eur. Cytokine Netw. 2016;27:81–89. doi: 10.1684/ecn.2016.0382. [DOI] [PubMed] [Google Scholar]
- 10.Khedr E.M., Gomaa A.M.S., Ahmed O.G., Sayed H.M.M., Gamea A. Cognitive Impairment, P300, and Transforming Growth Factor β1 in Different Forms of Dementia. J. Alzheimers Dis. 2020;78:837–845. doi: 10.3233/JAD-200885. [DOI] [PubMed] [Google Scholar]
- 11.Li H., Zhao Y., Liu T., Hu X., Teng Z. The Role of Neuroimaging in Cerebral Small Vessel Disease. Frontiers Media SA; Lausanne, Switzerland: 2023. [(accessed on 26 September 2023)]. Available online: https://play.google.com/store/books/details?id=FoW2EAAAQBAJ. [Google Scholar]
- 12.Zellner A., Scharrer E., Arzberger T., Oka C., Domenga-Denier V., Joutel A., Lichtenthaler S.F., Müller S.A., Dichgans M., Haffner C. CADASIL brain vessels show a HTRA1 loss-of-function profile. Acta Neuropathol. 2018;136:111–125. doi: 10.1007/s00401-018-1853-8. [DOI] [PubMed] [Google Scholar]
- 13.Gallione C.J., Repetto G.M., Legius E., Rustgi A.K., Schelley S.L., Tejpar S., Mitchell G., Drouin É., Westermann C.J., Marchuk D.A. A combined syndrome of juvenile polyposis and hereditary haemorrhagic telangiectasia associated with mutations in MADH4 (SMAD4) Lancet. 2004;363:852–859. doi: 10.1016/S0140-6736(04)15732-2. [DOI] [PubMed] [Google Scholar]
- 14.Wong S.H., Hamel L., Chevalier S., Philip A. Endoglin expression on human microvascular endothelial cells association with betaglycan and formation of higher order complexes with TGF-beta signalling receptors. Eur. J. Biochem. 2000;267:5550–5560. doi: 10.1046/j.1432-1327.2000.01621.x. [DOI] [PubMed] [Google Scholar]
- 15.Johnson D.W., Berg J.N., Baldwin M.A., Gallione C.J., Marondel I., Yoon S.J., Stenzel T.T., Speer M., Pericak-Vance M.A., Diamond A., et al. Mutations in the activin receptor-like kinase 1 gene in hereditary haemorrhagic telangiectasia type 2. Nat. Genet. 1996;13:189–195. doi: 10.1038/ng0696-189. [DOI] [PubMed] [Google Scholar]
- 16.McAllister K.A., Grogg K.M., Johnson D.W., Gallione C.J., Baldwin M.A., Jackson C.E., Helmbold E.A., Markel D.S., McKinnon W.C., Murrell J., et al. Endoglin, a TGF-beta binding protein of endothelial cells, is the gene for hereditary haemorrhagic telangiectasia type 1. Nat. Genet. 1994;8:345–351. doi: 10.1038/ng1294-345. [DOI] [PubMed] [Google Scholar]
- 17.Rol N., Kurakula K.B., Happé C., Bogaard H.J., Goumans M.-J. TGF-β and BMPR2 Signaling in PAH: Two Black Sheep in One Family. Int. J. Mol. Sci. 2018;19:2585. doi: 10.3390/ijms19092585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Derynck R., Zhang Y.E. Smad-dependent and Smad-independent pathways in TGF-beta family signalling. Nature. 2003;425:577–584. doi: 10.1038/nature02006. [DOI] [PubMed] [Google Scholar]
- 19.Goumans M.-J., Liu Z., ten Dijke P. TGF-beta signaling in vascular biology and dysfunction. Cell Res. 2009;19:116–127. doi: 10.1038/cr.2008.326. [DOI] [PubMed] [Google Scholar]
- 20.Wyss-Coray T., Lin C., Sanan D.A., Mucke L., Masliah E. Chronic overproduction of transforming growth factor-beta1 by astrocytes promotes Alzheimer’s disease-like microvascular degeneration in transgenic mice. Am. J. Pathol. 2000;156:139–150. doi: 10.1016/S0002-9440(10)64713-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tong X.-K., Hamel E. Simvastatin restored vascular reactivity, endothelial function and reduced string vessel pathology in a mouse model of cerebrovascular disease. J. Cereb. Blood Flow. Metab. 2015;35:512–520. doi: 10.1038/jcbfm.2014.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lacombe P., Mathews P.M., Schmidt S.D., Breidert T., Heneka M.T., Landreth G.E., Feinstein D.L., Galea E. Effect of anti-inflammatory agents on transforming growth factor beta over-expressing mouse brains: A model revised. J. Neuroinflammation. 2004;1:11. doi: 10.1186/1742-2094-1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tong X.-K., Nicolakakis N., Kocharyan A., Hamel E. Vascular remodeling versus amyloid beta-induced oxidative stress in the cerebrovascular dysfunctions associated with Alzheimer’s disease. J. Neurosci. 2005;25:11165–11174. doi: 10.1523/JNEUROSCI.4031-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nicolakakis N., Aboulkassim T., Aliaga A., Tong X.-K., Rosa-Neto P., Hamel E. Intact memory in TGF-β1 transgenic mice featuring chronic cerebrovascular deficit: Recovery with pioglitazone. J. Cereb. Blood Flow. Metab. 2011;31:200–211. doi: 10.1038/jcbfm.2010.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Martinez-Canabal A., Wheeler A.L., Sarkis D., Lerch J.P., Lu W.-Y., Buckwalter M.S., Wyss-Coray T., Josselyn S.A., Frankland P.W. Chronic over-expression of TGFβ1 alters hippocampal structure and causes learning deficits. Hippocampus. 2013;23:1198–1211. doi: 10.1002/hipo.22159. [DOI] [PubMed] [Google Scholar]
- 26.Lifshitz V., Weiss R., Benromano T., Kfir E., Blumenfeld-Katzir T., Tempel-Brami C., Assaf Y., Xia W., Wyss-Coray T., Weiner H.L., et al. Immunotherapy of cerebrovascular amyloidosis in a transgenic mouse model. Neurobiol. Aging. 2012;33:432.e1–432.e13. doi: 10.1016/j.neurobiolaging.2011.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tong X.-K., Trigiani L.J., Hamel E. High cholesterol triggers white matter alterations and cognitive deficits in a mouse model of cerebrovascular disease: Benefits of simvastatin. Cell Death Dis. 2019;10:89. doi: 10.1038/s41419-018-1199-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Trigiani L.J., Royea J., Tong X.-K., Hamel E. Comparative benefits of simvastatin and exercise in a mouse model of vascular cognitive impairment and dementia. FASEB J. 2019;33:13280–13293. doi: 10.1096/fj.201901002R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Trigiani L.J., Lacalle-Aurioles M., Bourourou M., Li L., Greenhalgh A.D., Zarruk J.G., David S., Fehlings M.G., Hamel E. Benefits of physical exercise on cognition and glial white matter pathology in a mouse model of vascular cognitive impairment and dementia. Glia. 2020;68:1925–1940. doi: 10.1002/glia.23815. [DOI] [PubMed] [Google Scholar]
- 30.Garcia F.J., Sun N., Lee H., Godlewski B., Mathys H., Galani K., Zhou B., Jiang X., Ng A.P., Mantero J., et al. Single-cell dissection of the human brain vasculature. Nature. 2022;603:893–899. doi: 10.1038/s41586-022-04521-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vanlandewijck M., He L., Mäe M.A., Andrae J., Ando K., Del Gaudio F., Nahar K., Lebouvier T., Laviña B., Gouveia L., et al. A molecular atlas of cell types and zonation in the brain vasculature. Nature. 2018;554:475–480. doi: 10.1038/nature25739. [DOI] [PubMed] [Google Scholar]
- 32.He L., Vanlandewijck M., Mäe M.A., Andrae J., Ando K., Del Gaudio F., Nahar K., Lebouvier T., Laviña B., Gouveia L., et al. Single-cell RNA sequencing of mouse brain and lung vascular and vessel-associated cell types. Sci. Data. 2018;5:180160. doi: 10.1038/sdata.2018.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Badhwar A., Stanimirovic D.B., Hamel E., Haqqani A.S. The proteome of mouse cerebral arteries. J. Cereb. Blood Flow. Metab. 2014;34:1033–1046. doi: 10.1038/jcbfm.2014.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang A.C., Vest R.T., Kern F., Lee D.P., Agam M., Maat C.A., Losada P.M., Chen M.B., Schaum N., Khoury N., et al. A human brain vascular atlas reveals diverse mediators of Alzheimer’s risk. Nature. 2022;603:885–892. doi: 10.1038/s41586-021-04369-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Badhwar A., Brown R., Stanimirovic D.B., Haqqani A.S., Hamel E. Proteomic differences in brain vessels of Alzheimer’s disease mice: Normalization by PPARγ agonist pioglitazone. J. Cereb. Blood Flow. Metab. 2016;37:1120–1136. doi: 10.1177/0271678X16655172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wyss-Coray T., Feng L., Masliah E., Ruppe M.D., Lee H.S., Toggas S.M., Rockenstein E.M., Mucke L. Increased central nervous system production of extracellular matrix components and development of hydrocephalus in transgenic mice overexpressing transforming growth factor-beta 1. [(accessed on 28 March 2023)];Am. J. Pathol. 1995 147:53–67. Available online: https://www.ncbi.nlm.nih.gov/pubmed/7604885. [PMC free article] [PubMed] [Google Scholar]
- 37.Spring S., Lerch J.P., Henkelman R.M. Sexual dimorphism revealed in the structure of the mouse brain using three-dimensional magnetic resonance imaging. Neuroimage. 2007;35:1424–1433. doi: 10.1016/j.neuroimage.2007.02.023. [DOI] [PubMed] [Google Scholar]
- 38.Krabbe-Hartkamp M.J., van der Grond J., de Leeuw F.E., de Groot J.C., Algra A., Hillen B., Breteler M.M., Mali W.P. Circle of Willis: Morphologic variation on three-dimensional time-of-flight MR angiograms. Radiology. 1998;207:103–111. doi: 10.1148/radiology.207.1.9530305. [DOI] [PubMed] [Google Scholar]
- 39.Percie du Sert N., Hurst V., Ahluwalia A., Alam S., Avey M.T., Baker M., Browne W.J., Clark A., Cuthill I.C., Dirnagl U., et al. The ARRIVE guidelines 2.0: Updated guidelines for reporting animal research. BMJ Open Sci. 2020;4:e100115. doi: 10.1136/bmjos-2020-100115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.UniProt Consortium UniProt: The universal protein knowledgebase in 2021. Nucleic Acids Res. 2021;49:D480–D489. doi: 10.1093/nar/gkaa1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mi H., Ebert D., Muruganujan A., Mills C., Albou L.-P., Mushayamaha T., Thomas P.D. PANTHER version 16: A revised family classification, tree-based classification tool, enhancer regions and extensive API. Nucleic Acids Res. 2021;49:D394–D403. doi: 10.1093/nar/gkaa1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mi H., Muruganujan A., Huang X., Ebert D., Mills C., Guo X., Thomas P.D. Protocol Update for large-scale genome and gene function analysis with the PANTHER classification system (v.14.0) Nat. Protoc. 2019;14:703–721. doi: 10.1038/s41596-019-0128-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Del Toro N., Shrivastava A., Ragueneau E., Meldal B., Combe C., Barrera E., Perfetto L., How K., Ratan P., Shirodkar G., et al. The IntAct database: Efficient access to fine-grained molecular interaction data. Nucleic Acids Res. 2022;50:D648–D653. doi: 10.1093/nar/gkab1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang Y., Chen K., Sloan S.A., Bennett M.L., Scholze A.R., O’Keeffe S., Phatnani H.P., Guarnieri P., Caneda C., Ruderisch N., et al. An RNA-sequencing transcriptome and splicing database of glia, neurons, and vascular cells of the cerebral cortex. J. Neurosci. 2014;34:11929–11947. doi: 10.1523/JNEUROSCI.1860-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Edgar R., Domrachev M., Lash A.E. Gene Expression Omnibus: NCBI gene expression and hybridization array data repository. Nucleic Acids Res. 2002;30:207–210. doi: 10.1093/nar/30.1.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kalra H., Simpson R.J., Ji H., Aikawa E., Altevogt P., Askenase P., Bond V.C., Borràs F.E., Breakefield X., Budnik V., et al. Vesiclepedia: A compendium for extracellular vesicles with continuous community annotation. PLoS Biol. 2012;10:e1001450. doi: 10.1371/journal.pbio.1001450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Caron N.S., Haqqani A.S., Sandhu A., Aly A.E., Findlay Black H., Bone J.N., McBride J.L., Abulrob A., Stanimirovic D., Leavitt B.R., et al. Cerebrospinal fluid biomarkers for assessing Huntington disease onset and severity. Brain Commun. 2022;4:fcac309. doi: 10.1093/braincomms/fcac309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Peterson D.B., Sander T., Kaul S., Wakim B.T., Halligan B., Twigger S., Pritchard K.A., Oldham K.T., Ou J.-S. Comparative proteomic analysis of PAI-1 and TNF-alpha-derived endothelial microparticles. Proteomics. 2008;8:2430–2446. doi: 10.1002/pmic.200701029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pallet N., Sirois I., Bell C., Hanafi L.-A., Hamelin K., Dieudé M., Rondeau C., Thibault P., Desjardins M., Hebert M.-J. A comprehensive characterization of membrane vesicles released by autophagic human endothelial cells. Proteomics. 2013;13:1108–1120. doi: 10.1002/pmic.201200531. [DOI] [PubMed] [Google Scholar]
- 50.Kalra H., Adda C.G., Liem M., Ang C.-S., Mechler A., Simpson R.J., Hulett M.D., Mathivanan S. Comparative proteomics evaluation of plasma exosome isolation techniques and assessment of the stability of exosomes in normal human blood plasma. Proteomics. 2013;13:3354–3364. doi: 10.1002/pmic.201300282. [DOI] [PubMed] [Google Scholar]
- 51.Little K.M., Smalley D.M., Harthun N.L., Ley K. The plasma microparticle proteome. Semin. Thromb. Hemost. 2010;36:845–856. doi: 10.1055/s-0030-1267038. [DOI] [PubMed] [Google Scholar]
- 52.Al Kaabi A., Traupe T., Stutz M., Buchs N., Heller M. Cause or effect of arteriogenesis: Compositional alterations of microparticles from CAD patients undergoing external counterpulsation therapy. PLoS ONE. 2012;7:e46822. doi: 10.1371/journal.pone.0046822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.de Jong O.G., Verhaar M.C., Chen Y., Vader P., Gremmels H., Posthuma G., Schiffelers R.M., Gucek M., Van Balkom B.W.M. Cellular stress conditions are reflected in the protein and RNA content of endothelial cell-derived exosomes. J. Extracell. Vesicles. 2012;1:18396. doi: 10.3402/jev.v1i0.18396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Haqqani A.S., Stanimirovic D.B. Prioritization of Therapeutic Targets of Inflammation Using Proteomics, Bioinformatics, and In Silico Cell-Cell Interactomics. Methods Mol. Biol. 2019;2024:309–325. doi: 10.1007/978-1-4939-9597-4_20. [DOI] [PubMed] [Google Scholar]
- 55.Haqqani A.S., Delaney C.E., Tremblay T.-L., Sodja C., Sandhu J.K., Stanimirovic D.B. Method for isolation and molecular characterization of extracellular microvesicles released from brain endothelial cells. Fluids Barriers CNS. 2013;10:4. doi: 10.1186/2045-8118-10-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cayrol R., Haqqani A.S., Ifergan I., Dodelet-Devillers A., Prat A. Isolation of human brain endothelial cells and characterization of lipid raft-associated proteins by mass spectroscopy. Methods Mol. Biol. 2011;686:275–295. doi: 10.1007/978-1-60761-938-3_13. [DOI] [PubMed] [Google Scholar]
- 57.Buckwalter M., Pepper J.-P., Gaertner R.F., Von Euw D., Lacombe P., Wyss-Coray T. Molecular and functional dissection of TGF-beta1-induced cerebrovascular abnormalities in transgenic mice. Ann. N. Y. Acad. Sci. 2002;977:87–95. doi: 10.1111/j.1749-6632.2002.tb04801.x. [DOI] [PubMed] [Google Scholar]
- 58.Gaertner R.F., Wyss-Coray T., Von Euw D., Lesné S., Vivien D., Lacombe P. Reduced brain tissue perfusion in TGF-beta 1 transgenic mice showing Alzheimer’s disease-like cerebrovascular abnormalities. Neurobiol. Dis. 2005;19:38–46. doi: 10.1016/j.nbd.2004.11.008. [DOI] [PubMed] [Google Scholar]
- 59.Bacakova L., Travnickova M., Filova E., Matějka R., Stepanovska J., Musilkova J., Zarubova J., Molitor M. Muscle Cell and Tissue: Current Status of Research Field. IntechOpen; Rijeka, Croatia: 2018. [(accessed on 2 January 2020)]. The Role of Vascular Smooth Muscle Cells in the Physiology and Pathophysiology of Blood Vessels; p. 229. Available online: https://books.google.com/books?hl=en&lr=&id=J7-QDwAAQBAJ&oi=fnd&pg=PA229&dq=The+Role+of+Vascular+Smooth+Muscle+Cells+in+the+Physiology+and+Pathophysiology+of+Blood+Vessels&ots=SIWW2CgxHX&sig=8wuktfI_DW5YlkRZzBWazIY_t-Y. [Google Scholar]
- 60.Guo D.-C., Papke C.L., Tran-Fadulu V., Regalado E.S., Avidan N., Johnson R.J., Kim D.H., Pannu H., Willing M.C., Sparks E., et al. Mutations in Smooth Muscle Alpha-Actin (ACTA2) Cause Coronary Artery Disease, Stroke, and Moyamoya Disease, Along with Thoracic Aortic Disease. Am. J. Hum. Genet. 2009;84:617–627. doi: 10.1016/j.ajhg.2009.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Calvier L., Chouvarine P., Legchenko E., Hoffmann N., Geldner J., Borchert P., Jonigk D., Mozes M.M., Hansmann G. PPARγ Links BMP2 and TGFβ1 Pathways in Vascular Smooth Muscle Cells, Regulating Cell Proliferation and Glucose Metabolism. Cell Metab. 2017;25:1118–1134.e7. doi: 10.1016/j.cmet.2017.03.011. [DOI] [PubMed] [Google Scholar]
- 62.Long X., Miano J.M. Transforming Growth Factor-β1 (TGF-β1) Utilizes Distinct Pathways for the Transcriptional Activation of MicroRNA 143/145 in Human Coronary Artery Smooth Muscle Cells. J. Biol. Chem. 2011;286:30119–30129. doi: 10.1074/jbc.M111.258814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Schildmeyer L.A., Braun R., Taffet G., Debiasi M., Burns A.E., Bradley A., Schwartz R.J. Impaired vascular contractility and blood pressure homeostasis in the smooth muscle alpha-actin null mouse. FASEB J. 2000;14:2213–2220. doi: 10.1096/fj.99-0927com. [DOI] [PubMed] [Google Scholar]
- 64.Cuoco J.A., Busch C.M., Klein B.J., Benko M.J., Stein R., Nicholson A.D., Marvin E.A. ACTA2 Cerebral Arteriopathy: Not Just a Puff of Smoke. Cerebrovasc. Dis. 2018;46:161–171. doi: 10.1159/000493863. [DOI] [PubMed] [Google Scholar]
- 65.Lenárt S., Lenárt P., Šmarda J., Remšík J., Souček K., Beneš P. Trop2: Jack of All Trades, Master of None. Cancers. 2020;12:3328. doi: 10.3390/cancers12113328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ripani E., Sacchetti A., Corda D., Alberti S. Human Trop-2 is a tumor-associated calcium signal transducer. Int. J. Cancer. 1998;76:671–676. doi: 10.1002/(SICI)1097-0215(19980529)76:5<671::AID-IJC10>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- 67.Szklarczyk D., Kirsch R., Koutrouli M., Nastou K., Mehryary F., Hachilif R., Gable A.L., Fang T., Doncheva N.T., Pyysalo S., et al. The STRING database in 2023: Protein-protein association networks and functional enrichment analyses for any sequenced genome of interest. Nucleic Acids Res. 2023;51:D638–D646. doi: 10.1093/nar/gkac1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Smith J.G., Newton-Cheh C. Genome-wide association studies of late-onset cardiovascular disease. J. Mol. Cell Cardiol. 2015;83:131–141. doi: 10.1016/j.yjmcc.2015.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Arking D.E., Junttila M.J., Goyette P., Huertas-Vazquez A., Eijgelsheim M., Blom M.T., Newton-Cheh C., Reinier K., Teodorescu C., Uy-Evanado A., et al. Identification of a sudden cardiac death susceptibility locus at 2q24.2 through genome-wide association in European ancestry individuals. PLoS Genet. 2011;7:e1002158. doi: 10.1371/journal.pgen.1002158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Urrecha M., Romero I., DeFelipe J., Merchán-Pérez A. Influence of cerebral blood vessel movements on the position of perivascular synapses. PLoS ONE. 2017;12:e0172368. doi: 10.1371/journal.pone.0172368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gasparini A., Tosatto S.C.E., Murgia A., Leonardi E. Dynamic scaffolds for neuronal signaling: In silico analysis of the TANC protein family. Sci. Rep. 2017;7:6829. doi: 10.1038/s41598-017-05748-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.LeMaistre J.L., Sanders S.A., Stobart M.J., Lu L., Knox J.D., Anderson H.D., Anderson C.M. Coactivation of NMDA receptors by glutamate and D-serine induces dilation of isolated middle cerebral arteries. J. Cereb. Blood Flow. Metab. 2012;32:537–547. doi: 10.1038/jcbfm.2011.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Manalo D.J., Rowan A., Lavoie T., Natarajan L., Kelly B.D., Ye S.Q., Garcia J.G.N., Semenza G.L. Transcriptional regulation of vascular endothelial cell responses to hypoxia by HIF-1. Blood. 2005;105:659–669. doi: 10.1182/blood-2004-07-2958. [DOI] [PubMed] [Google Scholar]
- 74.Renna N.F., de Las Heras N., Miatello R.M. Pathophysiology of vascular remodeling in hypertension. Int. J. Hypertens. 2013;2013:808353. doi: 10.1155/2013/808353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sturrock A., Cahill B., Norman K., Huecksteadt T.P., Hill K., Sanders K., Karwande S.V., Stringham J.C., Bull D.A., Gleich M., et al. Transforming growth factor-beta1 induces Nox4 NAD(P)H oxidase and reactive oxygen species-dependent proliferation in human pulmonary artery smooth muscle cells. Am. J. Physiol. Lung Cell Mol. Physiol. 2006;290:L661–L673. doi: 10.1152/ajplung.00269.2005. [DOI] [PubMed] [Google Scholar]
- 76.Schulick A.H., Taylor A.J., Zuo W., Qiu C.-B., Dong G., Woodward R.N., Agah R., Roberts A.B., Virmani R., Dichek D.A. Overexpression of transforming growth factor β1 in arterial endothelium causes hyperplasia, apoptosis, and cartilaginous metaplasia. Proc. Natl. Acad. Sci. USA. 1998;95:6983–6988. doi: 10.1073/pnas.95.12.6983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Fan J., Shen W., Lee S.-R., Mathai A.E., Zhang R., Xu G., Gillies M.C. Targeting the Notch and TGF-β signaling pathways to prevent retinal fibrosis in vitro and in vivo. Theranostics. 2020;10:7956–7973. doi: 10.7150/thno.45192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Gridley T. Notch signaling in vascular development and physiology. Development. 2007;134:2709–2718. doi: 10.1242/dev.004184. [DOI] [PubMed] [Google Scholar]
- 79.Zhang P., He D., Chen Z., Pan Q., Du F., Zang X., Wang Y., Tang C., Li H., Lu H., et al. Chemotherapy enhances tumor vascularization via Notch signaling-mediated formation of tumor-derived endothelium in breast cancer. Biochem. Pharmacol. 2016;118:18–30. doi: 10.1016/j.bcp.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 80.Karagiannis G.S., Weile J., Bader G.D., Minta J. Integrative pathway dissection of molecular mechanisms of moxLDL-induced vascular smooth muscle phenotype transformation. BMC Cardiovasc. Disord. 2013;13:4. doi: 10.1186/1471-2261-13-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gül D., Habtemichael N., Dietrich D., Dietrich J., Gößwein D., Khamis A., Deuss E., Künzel J., Schneider G., Strieth S., et al. Identification of cytokeratin24 as a tumor suppressor for the management of head and neck cancer. Biol. Chem. 2022;403:869–890. doi: 10.1515/hsz-2021-0287. [DOI] [PubMed] [Google Scholar]
- 82.Min M., Chen X.-B., Wang P., Landeck L., Chen J.-Q., Li W., Cai S.-Q., Zheng M., Man X.-Y. Role of keratin 24 in human epidermal keratinocytes. PLoS ONE. 2017;12:e0174626. doi: 10.1371/journal.pone.0174626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Stintzing S., Ocker M., Hartner A., Amann K., Barbera L., Neureiter D. Differentiation patterning of vascular smooth muscle cells (VSMC) in atherosclerosis. Virchows Arch. 2009;455:171–185. doi: 10.1007/s00428-009-0800-4. [DOI] [PubMed] [Google Scholar]
- 84.Alonso A., Sasin J., Bottini N., Friedberg I., Friedberg I., Osterman A., Godzik A., Hunter T., Dixon J., Mustelin T. Protein tyrosine phosphatases in the human genome. Cell. 2004;117:699–711. doi: 10.1016/j.cell.2004.05.018. [DOI] [PubMed] [Google Scholar]
- 85.Xu J., Zhong Y., Yin H., Linneman J., Luo Y., Xia S., Xia Q., Yang L., Huang X., Kang K., et al. Methylation-mediated silencing of PTPRD induces pulmonary hypertension by promoting pulmonary arterial smooth muscle cell migration via the PDGFRB/PLCγ1 axis. J. Hypertens. 2022;40:1795–1807. doi: 10.1097/HJH.0000000000003220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Celarain N., Tomas-Roig J. Changes in Deoxyribonucleic Acid Methylation Contribute to the Pathophysiology of Multiple Sclerosis. Front. Genet. 2019;10:1138. doi: 10.3389/fgene.2019.01138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Agha G., Mendelson M.M., Ward-Caviness C.K., Joehanes R., Huan T., Gondalia R., Salfati E., Brody J.A., Fiorito G., Bressler J., et al. Blood Leukocyte DNA Methylation Predicts Risk of Future Myocardial Infarction and Coronary Heart Disease. Circulation. 2019;140:645–657. doi: 10.1161/CIRCULATIONAHA.118.039357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Divers J., Palmer N.D., Langefeld C.D., Brown W.M., Lu L., Hicks P.J., Smith S.C., Xu J., Terry J.G., Register T.C., et al. Genome-wide association study of coronary artery calcified atherosclerotic plaque in African Americans with type 2 diabetes. BMC Genet. 2017;18:105. doi: 10.1186/s12863-017-0572-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ilinca A., Martinez-Majander N., Samuelsson S., Piccinelli P., Truvé K., Cole J., Kittner S., Soller M., Kristoffersson U., Tatlisumak T., et al. Whole-Exome Sequencing in 22 Young Ischemic Stroke Patients with Familial Clustering of Stroke. Stroke. 2020;51:1056–1063. doi: 10.1161/STROKEAHA.119.027474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sengelaub C.A., Navrazhina K., Ross J.B., Halberg N., Tavazoie S.F. PTPRN2 and PLCβ1 promote metastatic breast cancer cell migration through PI(4,5)P2-dependent actin remodeling. EMBO J. 2016;35:62–76. doi: 10.15252/embj.201591973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Chong A., Teo J.X., Ban K.H.K. Distinct epigenetic signatures elucidate enhancer-gene relationships that delineate CIMP and non-CIMP colorectal cancers. Oncotarget. 2016;7:28027–28039. doi: 10.18632/oncotarget.8473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Weerackoon N., Gunawardhana K.L., Mani A. Wnt Signaling Cascades and Their Role in Coronary Artery Health and Disease. J. Cell Signal. 2021;2:52–62. doi: 10.33696/Signaling.2.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Dunn S., Cowling V.H. Myc and mRNA capping. Biochim. Biophys. Acta. 2015;1849:501–505. doi: 10.1016/j.bbagrm.2014.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Posternak V., Ung M.H., Cheng C., Cole M.D. MYC Mediates mRNA Cap Methylation of Canonical Wnt/β-Catenin Signaling Transcripts by Recruiting CDK7 and RNA Methyltransferase. Mol. Cancer Res. 2017;15:213–224. doi: 10.1158/1541-7786.MCR-16-0247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Chen P., Zhou Z., Yao X., Pang S., Liu M., Jiang W., Jiang J., Zhang Q. Capping Enzyme mRNA-cap/RNGTT Regulates Hedgehog Pathway Activity by Antagonizing Protein Kinase A. Sci. Rep. 2017;7:2891. doi: 10.1038/s41598-017-03165-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Majesky M.W., Dong X.R., Hoglund V., Daum G., Mahoney W.M., Jr. The adventitia: A progenitor cell niche for the vessel wall. Cells Tissues Organs. 2012;195:73–81. doi: 10.1159/000331413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zhang M., Ding X., Zhang Q., Liu J., Zhang Y., Zhang Y., Tian Z., Li W., Zhu W., Kang H., et al. Exome sequencing of 112 trios identifies recessive genetic variants in brain arteriovenous malformations. J. Neurointerv. Surg. 2020;13:568–573. doi: 10.1136/neurintsurg-2020-016469. [DOI] [PubMed] [Google Scholar]
- 98.Dong J., Maj C., Tsavachidis S., Ostrom Q.T., Gharahkhani P., Anderson L.A., Wu A.H., Ye W., Bernstein L., Borisov O., et al. Sex-Specific Genetic Associations for Barrett’s Esophagus and Esophageal Adenocarcinoma. Gastroenterology. 2020;159:2065–2076.e1. doi: 10.1053/j.gastro.2020.08.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Zhang J., Huang J.Y., Chen Y.N., Yuan F., Zhang H., Yan F.H., Wang M.J., Wang G., Su M., Lu G., et al. Whole genome and transcriptome sequencing of matched primary and peritoneal metastatic gastric carcinoma. Sci. Rep. 2015;5:13750. doi: 10.1038/srep13750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Eisenwort G., Jurkin J., Yasmin N., Bauer T., Gesslbauer B., Strobl H. Identification of TROP2 (TACSTD2), an EpCAM-like molecule, as a specific marker for TGF-β1-dependent human epidermal Langerhans cells. J. Investig. Dermatol. 2011;131:2049–2057. doi: 10.1038/jid.2011.164. [DOI] [PubMed] [Google Scholar]
- 101.Ning S., Guo S., Xie J., Xu Y., Lu X., Chen Y. TROP2 correlates with microvessel density and poor prognosis in hilar cholangiocarcinoma. J. Gastrointest. Surg. 2013;17:360–368. doi: 10.1007/s11605-012-2105-1. [DOI] [PubMed] [Google Scholar]
- 102.Ning S., Liang N., Liu B., Chen X., Pang Q., Xin T. TROP2 expression and its correlation with tumor proliferation and angiogenesis in human gliomas. Neurol. Sci. 2013;34:1745–1750. doi: 10.1007/s10072-013-1326-8. [DOI] [PubMed] [Google Scholar]
- 103.Guo X., Zhu X., Zhao L., Li X., Cheng D., Feng K. Tumor-associated calcium signal transducer 2 regulates neovascularization of non-small-cell lung cancer via activating ERK1/2 signaling pathway. Tumour Biol. 2017;39:1010428317694324. doi: 10.1177/1010428317694324. [DOI] [PubMed] [Google Scholar]
- 104.Khundadze M., Kollmann K., Koch N., Biskup C., Nietzsche S., Zimmer G., Hennings J.C., Huebner A.K., Symmank J., Jahic A., et al. A hereditary spastic paraplegia mouse model supports a role of ZFYVE26/SPASTIZIN for the endolysosomal system. PLoS Genet. 2013;9:e1003988. doi: 10.1371/journal.pgen.1003988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Cai Y., Wang X.-L., Flores A.M., Lin T., Guzman R.J. Inhibition of endo-lysosomal function exacerbates vascular calcification. Sci. Rep. 2018;8:3377. doi: 10.1038/s41598-017-17540-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Arora A., Kivelä A.M., Wang L., Minkeviciene R., Taskinen J.H., Zhang B., Koponen A., Sun J., Shirane M., Zhou Y., et al. Protrudin regulates FAK activation, endothelial cell migration and angiogenesis. Cell Mol. Life Sci. 2022;79:220. doi: 10.1007/s00018-022-04251-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wyss-Coray T., Mucke L. Inflammation in neurodegenerative disease--a double-edged sword. Neuron. 2002;35:419–432. doi: 10.1016/S0896-6273(02)00794-8. [DOI] [PubMed] [Google Scholar]
- 108.Nicolakakis N., Aboulkassim T., Ongali B., Lecrux C., Fernandes P., Rosa-Neto P., Tong X.-K., Hamel E. Complete rescue of cerebrovascular function in aged Alzheimer’s disease transgenic mice by antioxidants and pioglitazone, a peroxisome proliferator-activated receptor gamma agonist. J. Neurosci. 2008;28:9287–9296. doi: 10.1523/JNEUROSCI.3348-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Liu X.-H., Zhang Q.-Y., Pan L.-L., Liu S.-Y., Xu P., Luo X.-L., Zou S.-L., Xin H., Qu L.-F., Zhu Y.-Z. NADPH oxidase 4 contributes to connective tissue growth factor expression through Smad3-dependent signaling pathway. Free Radic. Biol. Med. 2016;94:174–184. doi: 10.1016/j.freeradbiomed.2016.02.031. [DOI] [PubMed] [Google Scholar]
- 110.Hu T., Ramachandrarao S.P., Siva S., Valancius C., Zhu Y., Mahadev K., Toh I., Goldstein B.J., Woolkalis M., Sharma K., et al. Reactive oxygen species production via NADPH oxidase mediates TGF-beta-induced cytoskeletal alterations in endothelial cells. Am. J. Physiol. Ren. Physiol. 2005;289:F816–F825. doi: 10.1152/ajprenal.00024.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Kvietys P.R., Granger D.N. Role of reactive oxygen and nitrogen species in the vascular responses to inflammation. Free Radic. Biol. Med. 2012;52:556–592. doi: 10.1016/j.freeradbiomed.2011.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Durgin B.G., Straub A.C. Redox control of vascular smooth muscle cell function and plasticity. Lab. Investig. 2018;98:1254–1262. doi: 10.1038/s41374-018-0032-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Lupfer C., Kanneganti T.-D. Unsolved Mysteries in NLR Biology. Front. Immunol. 2013;4:285. doi: 10.3389/fimmu.2013.00285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Nagyőszi P., Nyúl-Tóth Á., Fazakas C., Wilhelm I., Kozma M., Molnár J., Haskó J., Krizbai I.A. Regulation of NOD-like receptors and inflammasome activation in cerebral endothelial cells. J. Neurochem. 2015;135:551–564. doi: 10.1111/jnc.13197. [DOI] [PubMed] [Google Scholar]
- 115.Nyúl-Tóth Á., Kozma M., Nagyőszi P., Nagy K., Fazakas C., Haskó J., Molnár K., Farkas A.E., Végh A.G., Váró G., et al. Expression of pattern recognition receptors and activation of the non-canonical inflammasome pathway in brain pericytes. Brain Behav. Immun. 2017;64:220–231. doi: 10.1016/j.bbi.2017.04.010. [DOI] [PubMed] [Google Scholar]
- 116.Amini H., Shroff N., Stamova B., Ferino E., Carmona-Mora P., Zhan X., Sitorus P.P., Hull H., Jickling G.C., Sharp F.R., et al. Genetic variation contributes to gene expression response in ischemic stroke: An eQTL study. Ann. Clin. Transl. Neurol. 2020;7:1648–1660. doi: 10.1002/acn3.51154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Padovano V., Lucibello I., Alari V., Della Mina P., Crespi A., Ferrari I., Recagni M., Lattuada D., Righi M., Toniolo D., et al. The POF1B candidate gene for premature ovarian failure regulates epithelial polarity. J. Cell Sci. 2011;124:3356–3368. doi: 10.1242/jcs.088237. [DOI] [PubMed] [Google Scholar]
- 118.Youn H., Ji I., Ji H.P., Markesbery W.R., Ji T.H. Under-expression of Kalirin-7 Increases iNOS activity in cultured cells and correlates to elevated iNOS activity in Alzheimer’s disease hippocampus. [(accessed on 18 June 2019)];J. Alzheimers Dis. 2007 12:271–281. doi: 10.3233/JAD-2007-12309. Available online: https://www.ncbi.nlm.nih.gov/pubmed/18057561. [DOI] [PubMed] [Google Scholar]
- 119.Wang L., Hauser E.R., Shah S.H., Pericak-Vance M.A., Haynes C., Crosslin D., Harris M., Nelson S., Hale A.B., Granger C.B., et al. Peakwide mapping on chromosome 3q13 identifies the kalirin gene as a novel candidate gene for coronary artery disease. Am. J. Hum. Genet. 2007;80:650–663. doi: 10.1086/512981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Krug T., Manso H., Gouveia L., Sobral J., Xavier J.M., Albergaria I., Gaspar G., Correia M., Viana-Baptista M., Simões R.M., et al. Kalirin: A novel genetic risk factor for ischemic stroke. Hum. Genet. 2010;127:513–523. doi: 10.1007/s00439-010-0790-y. [DOI] [PubMed] [Google Scholar]
- 121.Shafiei A., Pilehvar-Soltanahmadi Y., Ziaee S., Mofarrah M., Zarghami N. Association between Serum Kalirin Levels and the KALRN gene rs9289231 Polymorphism in Early-Onset Coronary Artery Disease. [(accessed on 17 April 2019)];J. Tehran Heart Cent. 2018 13:58–64. Available online: https://www.ncbi.nlm.nih.gov/pubmed/30483314. [PMC free article] [PubMed] [Google Scholar]
- 122.Zhang W., Kuncewicz T., Yu Z.-Y., Zou L., Xu X., Kone B.C. Protein-protein interactions involving inducible nitric oxide synthase. Acta Physiol. Scand. 2003;179:137–142. doi: 10.1046/j.1365-201X.2003.01119.x. [DOI] [PubMed] [Google Scholar]
- 123.Maletzko A., Key J., Wittig I., Gispert S., Koepf G., Canet-Pons J., Torres-Odio S., West A.P., Auburger G. Increased presence of nuclear DNAJA3 and upregulation of cytosolic STAT1 and of nucleic acid sensors trigger innate immunity in the ClpP-null mouse. Neurogenetics. 2021;22:297–312. doi: 10.1007/s10048-021-00657-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Paradies G., Petrosillo G., Pistolese M., Di Venosa N., Federici A., Ruggiero F.M. Decrease in mitochondrial complex I activity in ischemic/reperfused rat heart: Involvement of reactive oxygen species and cardiolipin. Circ. Res. 2004;94:53–59. doi: 10.1161/01.RES.0000109416.56608.64. [DOI] [PubMed] [Google Scholar]
- 125.Bean C., Verma N.K., Yamamoto D.L., Chemello F., Cenni V., Filomena M.C., Chen J., Bang M.L., Lanfranchi G. Ankrd2 is a modulator of NF-κB-mediated inflammatory responses during muscle differentiation. Cell Death Dis. 2014;5:e1002. doi: 10.1038/cddis.2013.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Deng Y., Jiang X., Deng X., Chen H., Xu J., Zhang Z., Liu G., Yong Z., Yuan C., Sun X., et al. Pioglitazone ameliorates neuronal damage after traumatic brain injury via the PPARγ/NF-κB/IL-6 signaling pathway. Genes. Dis. 2020;7:253–265. doi: 10.1016/j.gendis.2019.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Badhwar A., Haqqani A.S. Biomarker potential of brain-secreted extracellular vesicles in blood in Alzheimer’s disease. Alzheimers Dement. 2020;12:e12001. doi: 10.1002/dad2.12001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Haqqani A.S., Kelly J.F., Stanimirovic D.B. Quantitative Protein Profiling by Mass Spectrometry Using Label-Free Proteomics. Methods Mol. Biol. 2008;439:241–256. doi: 10.1007/978-1-59745-188-8_17. [DOI] [PubMed] [Google Scholar]
- 129.Hirosawa M., Hoshida M., Ishikawa M., Toya T. MASCOT: Multiple Alignment System for Protein Sequences Based on Three-Way Dynamic Programming. Comput. Appl. Biosci. 1993;9:161–167. doi: 10.1093/bioinformatics/9.2.161. [DOI] [PubMed] [Google Scholar]
- 130.Théry C., Witwer K.W., Aikawa E., Alcaraz M.J., Anderson J.D., Andriantsitohaina R., Antoniou A., Arab T., Archer F., Atkin-Smith G.K., et al. Minimal Information for Studies of Extracellular Vesicles 2018 (MISEV2018): A Position Statement of the International Society for Extracellular Vesicles and Update of the MISEV2014 Guidelines. J. Extracell. Vesicles. 2018;7:1535750. doi: 10.1080/20013078.2018.1535750. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data available upon request to the corresponding author.