Abstract
Simple Summary
Modifications of gene expression (epigenetic alterations) have been implicated in the pathogenesis of complex diseases, such as Alzheimer’s disease (AD). Apolipoprotein E (ApoE), a major lipid carrier in the central nervous system, possesses three variants, E2, E3, and E4, with APOE4 increasing the risk of developing AD. The APOE gene undergoes epigenetic modifications. Diet, lifestyle, and pollutants might interact with the human genome. It is possible that environment and lifestyle can modify AD risk through epigenetic mechanisms involving the APOE gene and its promoter (a sequence of DNA to which proteins bind to initiate transcription) conditioning the imbalance between ApoE isoforms. One of the epigenetic mechanisms is DNA methylation at three sites of APOE CpG islands. A comprehensive interpretation of APOE-mediated effects within AD pathophysiology includes epigenetic mechanisms by which the equilibrium of its isoforms is regulated.
Abstract
Sporadic Alzheimer’s disease (AD) derives from an interplay among environmental factors and genetic variants, while epigenetic modifications have been expected to affect the onset and progression of its complex etiopathology. Carriers of one copy of the apolipoprotein E gene (APOE) ε4 allele have a 4-fold increased AD risk, while APOE ε4/ε4-carriers have a 12-fold increased risk of developing AD in comparison with the APOE ε3-carriers. The main longevity factor is the homozygous APOE ε3/ε3 genotype. In the present narrative review article, we summarized and described the role of APOE epigenetics in aging and AD pathophysiology. It is not fully understood how APOE variants may increase or decrease AD risk, but this gene may affect tau- and amyloid-mediated neurodegeneration directly or indirectly, also by affecting lipid metabolism and inflammation. For sporadic AD, epigenetic regulatory mechanisms may control and influence APOE expression in response to external insults. Diet, a major environmental factor, has been significantly associated with physical exercise, cognitive function, and the methylation level of several cytosine-phosphate-guanine (CpG) dinucleotide sites of APOE.
Keywords: apolipoprotein E, Alzheimer’s disease, methylation, dementia, epigenetics, tau protein, amyloid-β, longevity
1. Introduction
The study of complex diseases is based on the association among epigenetics, gene variants, and environmental factors [1,2]. A mixture of many pathogenic pathways and gene expression networks determines the pathophysiology of Alzheimer’s disease (AD). The current model of AD is based on the amyloid-β (Aβ) hypothesis, in which a series of deterministic events may lead from tau protein and Aβ deposition to neurodegeneration and progressive decline of cognitive function. This conceptualization matches autosomal-dominant AD, defined as dominantly inherited AD with pathological confirmation, although it is less appropriate for sporadic AD. A probabilistic AD model connoted by three variants of the disease has been proposed: autosomal-dominant AD, apolipoprotein E (apolipoprotein E gene, APOE) ε4 allele-related sporadic AD, and APOE ε4 allele-unrelated sporadic AD [3]. These three variants suggested a reduced weight of the Aβ hypothesis, giving more importance to environmental factors and lower-risk genes [3].
Epigenetic modifications have been found in AD [4]. From a genetic point of view, the known risk loci (such as ABCA7, APOE, CLU, CR1, BIN1, CD2AP, EPHA1, MS4A6A–MS4A4E, and PICALM genes) [5], showed a low penetrance in causing AD, except for Aβ production-related genes, and none of them have been related to different AD pathogenic pathways. On the contrary, epigenetic alterations may modify transcriptional activity globally throughout different genes and multiple biological pathways. Epigenetic mechanisms may also explain the influence of environmental stimuli such as dietary patterns, harmful exposures, and lifestyle factors on phenotypic outcomes in individuals with the same genetic variants, also in AD [6]. Generally, the genetic sequence and epigenetic code are linked in a clear way according to the methylation mechanism. In fact, some single nucleotide polymorphisms (SNPs) are considered a common epigenetic mark because of the rearranging of cytosine-phosphate-guanine (CpG) dinucleotides with C nucleotide methylation. These CpG-altering SNPs may modulate DNA methylation levels in a cis or trans manner or they may modify gene transcription at regions enhanced of CpG known as CpG islands [7,8,9].
The APOE variants, respectively ε2 ε3, ε4, and ε3r, are determined by four haplotypes at the APOE locus (19q13.32), derived from the allele association of two common SNPs, rs429358 (C3937 → T) and rs7412 (C4075 → T), coding for the different protein isoforms [10]. These four APOE alleles are probably the most investigated variants in the human Caucasian genome [11]. Remarkably, the APOE exon 4 region, encompassing the ε2/ε3/ε4 allele variants, is a well-defined CpG islands-rich area. Moreover, the two common SNPs rs429358 and rs7412 are CpG-altering and modify the CpG content of this area. This APOE CpG island-rich area is a transcriptional enhancer with a specificity linked to the ε4 allele and cell-type [12].
Since the early 1990s, many reports have shown that APOE may play a fundamental role in AD neurodegeneration. For sporadic AD, APOE allele ε4 is a key genetic risk factor [13,14,15], with a semidominant inheritance [16], and associated to the ApoE4 isoform. The APOE ε4 allele is a major AD risk factor in both men and women between 40 and 90 years, and for all ethnic groups. Conversely, in sporadic AD, the APOE allele ε2, associated to the ApoE2 isoform, could have a protective effect [17,18]. The risk for sporadic AD in APOE ε4-carriers is increased, but the presence of the APOE ε4 allele alone is not a causal factor for AD pathology [19]. In this context, epigenetics may represent a candidate for a point of overlapping among several genetic risk factors for AD, such as the APOE ε4 allele, and the AD pathophysiological processes. Human ApoE is a glycoprotein of 299-amino acids, traditionally binding phospholipids, and cholesterol. ApoE is produced in three common isoforms (ApoE2, ApoE3, and ApoE4) differing in two amino acid residues at positions 112 and 158, and one very uncommon isoform (ApoE3r) [12]. In AD pathophysiology, a global interpretation of APOE-mediated effects includes epigenetic mechanisms by which the homeostasis of its isoforms is regulated [20]. In the present review article, we briefly summarized and highlighted the complex epigenetic regulation of the APOE gene in aging and sporadic AD.
2. The Role of Apolipoprotein E in Alzheimer’s Disease Pathogenesis
For sporadic AD, the APOE 4 allele is the most important genetic risk factor, as well as for the earlier stages of cognitive decline represented by mild cognitive impairment (MCI) [21], but its expression is poorly understood. Astrocytes and activated microglia produced the major amount of ApoE in the brain. Having one APOE ε4 allele conducts to a 4-fold increased risk of developing AD, while having two APOE ε4 alleles conducts to a 12-fold increased risk, in comparison with the APOE ε3-carriers. Conversely, the uncommon heterozygous carriers of the APOE ε2 allele have an AD risk 40% lower and the homozygous carriers have a further reduced risk [22]. In brain, APOE ε4-carriers with normal cognition displayed higher Aβ and tau burden than APOE ε3-carriers; conversely, APOE ε2-carriers had reduced global Aβ burden, without differences in regional tau burden or accumulation over time [23]. The contribution in AD pathogenesis from APOE involves not only Aβ aggregation and its clearance, but also tau-mediated neurodegeneration [24], microglia impairment [25,26], astrocyte reactivity [27], and blood–brain barrier disruption [28,29].
The three ApoE isoforms bind and transport Aβ peptides with differential affinity during AD pathogenesis [30,31], being highest for ApoE4, intermediate for ApoE3, and lowest for ApoE2 [32,33]. Therefore, their effects are also different concerning Aβ aggregation and clearance, but not Aβ production [34,35]. ApoE also can affect tau-mediated neurodegeneration and tauopathy by modulating microglial responses to Aβ plaque pathology [36,37,38]. Thus, different ApoE isoforms may be associated with an increased or reduced AD risk [31,32], based on different combined effects of ApoE isoforms on both deposits of Aβ and neurofibrillary tangles [39]. APOE and its ε2/ε3/ε4 alleles have been connected by several genetic studies to different disorders and physiological conditions. Epigenetic alterations could explain the association between APOE and its associated diseases, considering that disease-associated genetic signals may also reflect a site sequence architecture for epigenetic codes [12].
3. Apolipoprotein E, Human Longevity, and Alzheimer’s Disease
A genetic association of APOE with both human longevity and AD was found, but the mechanistic contribution of APOE in aging and long life is largely under investigation. APOE pleiotropic roles may be explained by its exceptional epigenetic properties. In the AD brain, these epigenetic changes could contribute to neural cell dysfunction. Additionally, DNA methylation modifications have been found on specific genes associated with AD pathology such as APOE. In the AD brain, it was shown that APOE CpG islands were differentially methylated in an APOE-genotype and tissue-specific way [40]. In the APOE CpG islands, AD typically showed a lower level of DNA methylation occurring in brain regions affected by AD pathophysiology (highest levels in the cerebellum, with moderate levels in the hippocampus and the lowest levels in the frontal lobe). However, in the APOE CpG islands, there was a complex interplay among the presence of the APOE ε4 allele, AD status, and DNA methylation levels. AD-specific methylation differences were mainly attributed to the APOE ε3/ε4 heterozygous subjects [40]. Allele variations in the major APOE CpG islands of targeted replacement (TR) mice expressing human APOE may affect its methylation in the brain [41]. Epigenetic changes may link modified gene expression with environmental stimuli such as dietary patterns and physical exercise. In animal models, APOE alleles may have alterations in epigenetic regulation responding to external stimuli reported in studies on APOE TR mice [42].
In the strategy for replacing mouse ApoE in the APOE TR models, we should consider differences between human and mouse APOE gene clusters, the complexity of transcriptional control of human APOE, and the structure of the targeting construct [43]. Moreover, lifestyle factors like education, smoking, alcohol consumption, and physical activity may weaken genetic risk in the process of age-related cognitive decline and dementia. At this regard, twelve potentially modifiable risk factors have been investigated to prevent or delay up to 40% the risk for different types of dementias including AD, i.e., lower educational level, hypertension, hearing loss, smoking, obesity, depressive syndromes, physical inactivity, diabetes, low social contact, immoderate alcohol consumption, air pollution, and traumatic brain injury [44]. The complex interactions among lifestyle, genetics, and age-related cognitive decline may encourage behaviors maintaining cognitive health in older age, including dietary habits [45]. At this regard, ApoE may be important for the pathophysiology of lipid metabolism [46] and central nervous system (CNS), although the role in healthy aging and longevity has seen its value grow [47,48,49].
In the lipid metabolism pathophysiology, ApoE may be related with normal/pathological aging, while its function in CNS pathophysiology needs further clarification [50]. In fact, in the CNS, there was about a quarter of total body cholesterol that may exert a significant impact on synaptic plasticity [51]. With advancing age, cholesterol metabolism may modify, and its related brain changes may be associated with the pathophysiology of AD [51]. So, in longevity and healthy aging, lipid and cholesterol maintenance are a critical factor also from an interventional point of view. Dietary interventions may manage the detrimental effects of the APOE ε4 allele [52], with a Mediterranean dietary pattern potentially including higher n-3 polyunsaturated fatty acid (PUFA) intakes [53,54].
Studies on longevity and healthy aging are related because subjects who live longer tend to be healthier for a greater part of their lives [55]. Healthy aging can be described as achieving older age maintaining intact cognition and/or mobility and without disabilities or multimorbidity. This last can be defined as the coexistence of two or more chronic diseases in the same subjects [56]. The detrimental effects of the APOE ε4 allele on longevity could influence the probability of a long human lifespan [55]. The APOE ε2 allele has a greater frequency in long-lived individuals than the ε4 allele [57]. Thus, the main longevity factor is the APOE ε3/ε3 genotype. The greater frequency of the ε3 allele in older individuals and their offspring than in controls derives from the higher amount of the homozygous APOE ε3/ε3 genotype in comparison with the ε2/ε3 or ε3/ε4 genotypes [58].
4. Specific Epigenetic Modifications of Apolipoprotein E in Alzheimer’s Disease
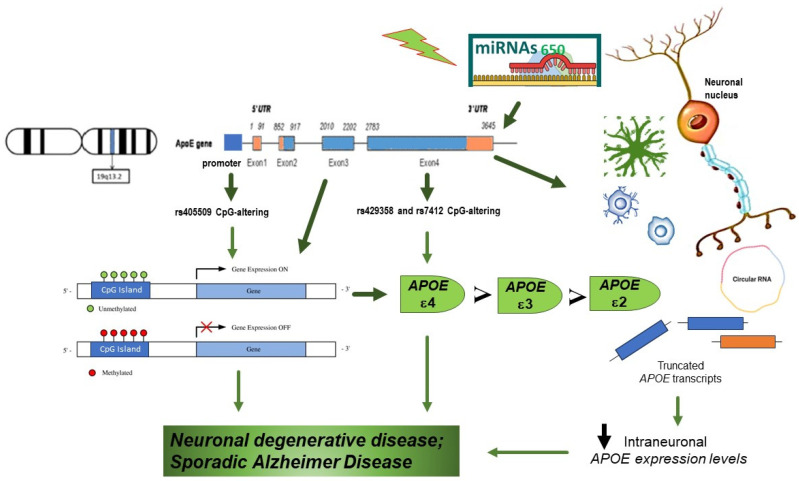
In response to environmental stimuli, epigenetic marks and signals may enable temporal combination of regulatory events through mechanisms including DNA methylation, histone modification/chromatin conformation, and noncoding microRNAs (miRNAs). In the APOE gene, several studies investigating DNA methylation suggested an age-dependent flow and APOE DNA methylation specific for brain area. The impact of aging on APOE methylation is based on the general link between DNA methylation and longevity, although current studies on the association among aging and APOE methylation patterns are limited and with little sample size as later described. The APOE genomic sequence is approximately 4 kb in size (chromosome19:45408714-45412650, hg19) including its promoter. This region encompasses 172 CpG dinucleotides [59]. At the APOE locus, three functional SNPs may modify DNA methylation, and of these, rs405509 is in the promoter region, while the other two SNPs (rs429358 and rs7412), which define the APOE e2/e3/e4 isoforms, are within exon 4 (Figure 1). Genetic variability in the APOE neural expression may contribute to the risk of AD considering that relative APOE ε4 mRNA expression is higher in AD patient than in healthy controls [60]. Moreover, together with the qualitative effect on the AD risk of the APOE e2/e3/e4 polymorphisms, functional APOE promoter mutations may determine quantitative variation of expression of these alleles that is a fundamental determinant of AD occurrence. In the late 1990s and early 2000s, polymorphic sites in the first intron and the proximal promoter the of APOE gene cluster (−1019 to +407) affecting APOE expression were identified, showing the deleterious effect of the Th1/E47cs T allele and the protective effect of the −491 T allele [61,62,63,64,65] (Table 1). Notably, these polymorphisms have been related with a differential AD risk [66,67,68].
Figure 1.
Apolipoprotein E (APOE) gene pleiotropic roles may be explained by its exceptional epigenetic properties. The APOE ε2/ε3/ε4 alleles are produced by two cytosine-phosphate-guanine (CpG)-altering SNPs (rs429358 and rs7412) in the core region of the APOE CpG islands. APOE ε4 carriers have the greatest number of CpG dinucleotide sites, while APOE ε2 carriers have the smallest number, so methylation levels for most CpG sites are in the order of APOE ε4 carriers > APOE ε3/ε3 > APOE ε2 carriers. In the promoter region, there is another SNP, rs405509. Furthermore, other epigenetics mechanisms are linked to the processing of primary miR-650 to mature miR-650 is mis regulated. miR-650 can significantly reduce the expression of APOE.
In AD, the association between these polymorphic sites and the variability of sequence in the proximal promoter with ApoE protein levels are not clearly understood. In fact, among different studies, findings on the levels of expression of APOE RNA and the relationship with the ApoE levels varied. In human AD postmortem brain, there was elevated methylation in frontal lobe of a 5′-C-phosphate-G-3′ (CpG) island overlapping with exon four and downstream [69]. APOE has a well-defined CpG island external to the promoter region and overlapping with the APOE 3′-exon. In the human genome, these 3′-CpG islands are very rare, representing < 1% of the total CpG islands, and are also conserved in other mammals [70,71]. However, the APOE CpG island methylation level relates to the level of expression of four known APOE transcripts. The majority of the total APOE mRNA, with higher expression in the AD frontal lobe than in the frontal lobe of control subjects, is constituted by circular RNAs, mRNAs, and truncated APOE transcripts. The findings of several studies suggested several changes in the epigenome and the regulatory role of epigenomic elements related to the risk or clinical presentation of several neurological diseases, although the exact clinical significance of these signatures in the quantities of RNA and methylation level of CGI in the APOE 3′-exon was still unclear [69] (Table 1).
At the level of the individual CpG site, epigenetic regulation was shown by up/down patterns in the methylation profiles between samples and tissues. Significant differences in the global methylation levels among several regions of the brain were discovered across postmortem brain tissues. In brain regions primary affected by AD such as frontal lobe, temporal lobe, and hippocampus, methylation levels were lower. Conversely, we observed in the cerebellum, a region apparently without profound pathological alterations in AD but with recent important findings, the highest methylation levels, suggesting a correlation between the methylation levels of the APOE CpG islands and the vulnerability of brain regions in AD patients [40]. In fact, age- and AD-related alterations in several cerebellar subregions may also impact numerous functional domains, especially those affecting cognitive processing [72].
Genetic variants, which consist of CpG-altering SNP, can modify DNA methylation levels. These genetic variations may act like regulatory elements connecting genetic changes not only with the protein isoforms, but also with epigenetic variability [73] (Table 1). As previously described, the APOE ε2/ε3/ε4 alleles are produced by two CpG-altering SNPs (rs429358 and rs7412) residing in the core region of the APOE CpG islands. The APOE ε4 allele, if compared with ε2 or ε3 alleles, adds one more CpG, further saturating a small 12 bp region with 4 CpG sites. On the contrary, the APOE ε2 allele eliminates 1 CpG and opens a 33-bp CpG-free region. Consequently, these two SNPs may alter the regional CpG burden and probably influence global DNA methylation of the CpG islands (Figure 1). These CpG load changes might change the binding profiles of methyl-CpG binding domain proteins, associated to methylated DNA through their exclusive amino acid patterns [74].
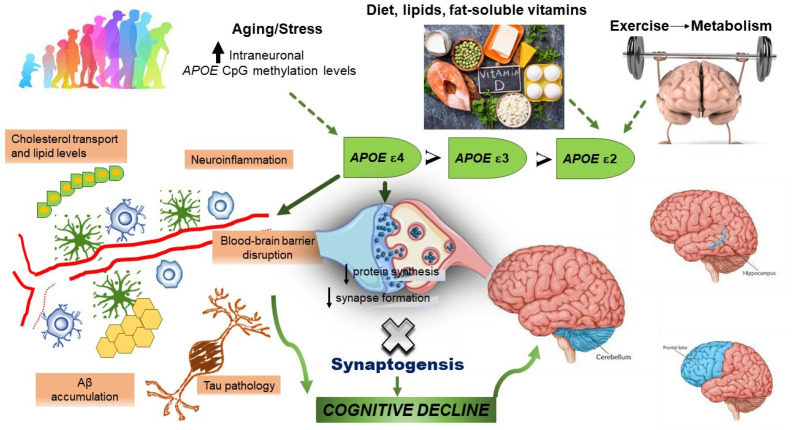
Furthermore, within the APOE CpG islands, there is evidence of indirect indicators of protein binding which consist of histone marks and a DNase I hypersensitivity cluster. These findings suggested that the APOE CpG islands and exon 4 may be a site for chromatin remodeling and protein binding. Considering that environmental stimuli could influence DNA methylation gradually with aging, the differences in APOE CpG island methylation between healthy subjects and patients with AD increased with age [75]. Taken together, different methylation scenarios may be represented by the inheritance of different ε2/ε3/ε4 alleles in the APOE CpG islands, which could accumulate or change continuously with age, also modified by environmental factors. Recent results showed that methylation levels for most CpG sites may be in the order of APOE ε4-carriers (greatest number of CpG sites) > APOE ε3/ε3-carriers > APOE ε2-carriers (smallest number of CpG sites) [76] (Table 1). These changes could potentially alter protein binding, with some consequences on biological systems, even affecting the pathophysiological processes of multiple diseases and plasma lipids levels. APOE methylation could partially mediate the effects of age on plasma lipid (Figure 2).
Figure 2.
Despite the high lifetime risk linked to the presence of the APOE ε3/ε4 and APOE ε4/ε4 genotypes (the greatest risk factor for developing Alzheimer’s disease, AD), stochastic factors (such as environment, diet, physical exercise, and aging), may play a significant role as epigenetic modifiers, influencing the imbalance among the different ApoE isoforms. The role of APOE ε4 allele in AD pathogenesis involves not only amyloid-β aggregation and clearance, but also tau-mediated neurodegeneration, microglia dysfunction, astrocyte reactivity, and blood–brain barrier disruption. These changes may only occur in brain regions profoundly affected by AD pathophysiology (highest levels in the cerebellum, with moderate levels in the hippocampus and the lowest levels in the frontal lobe).
Table 1.
Overview of studies illustrating epigenetic signatures of apolipoprotein E gene (APOE) in aging and Alzheimer’s disease (AD).
| APOE Exons, Promoter, and CGI | ||||
|---|---|---|---|---|
| Study | Study Design | Sample Size |
Age or Mean Age at Death (Years) | Principal Findings |
| Foraker et al., 2015 [40] | Cross-sectional | AD: 15 Controls: 10 |
AD: 82.7 ± 9.3 Controls: 84.9 ± 8.9 |
In the cerebellum there was the highest levels of methylation (marginal mean = 93%), with lower levels in the hippocampus (marginal mean = 85%), and the lowest levels in the frontal lobe (marginal mean = 77%) of AD brain compared to controls. There was a complex interaction among the presence of the APOE ε4 allele, AD status, and DNA methylation levels in the APOE CpG islands. AD-specific methylation differences were mainly attributed to the ε3/ε4 heterozygous subjects |
| Lambert et al., 1997 [60] | Cross-sectional | Frontal lobe ε3ε4, ε2ε4, ε2ε3 AD cases: 14 Controls: 12 |
AD: 74.1 ± 11.8 (five male and nine female) controls: 83.0 ± 10.6 | In heterozygotes AD, APOE ε4 mRNA expression is increased in patients with AD compared with healthy controls: genetic variability in the neural expression at the APOE locus contributes to AD risk. APOE ε3ε4 heterozygote subjects (high ε4 expressors and/or low ε3 expressors) were more likely to develop AD than subjects with high ε3 expressors and/or low ε4 expressors |
| Lee et al., 2020 [69] | Cross-sectional | Frontal lobe AD: 44 Controls: 21 Cerebellum AD: 51 Controls: 25 |
Frontal lobe AD: 86.8 ± 6.9 Controls: 87.9 ± 8.6 Cerebellum AD: 74.6 ± 9.3 Controls: 73.5 ± 10.9 |
APOE has a single CpG island overlapping with its 3′-exon. APOE circular RNA and full-length mRNA each constitute one third of the total APOE RNA, with truncated mRNAs likely constituting some of the missing fraction. All APOE RNA species had significantly higher expression in AD frontal lobe than in controls, suggesting a possible modified mechanism of gene action for APOE in AD involving also an epigenetically regulated transcriptional program driven by DNA methylation in the APOE CpG island |
| Yu et al., 2013 [73] | Cross-sectional | Frontal lobe AD: 9 Controls: 6 |
AD: 86.8 ± 6.9 Controls: 87.9 ± 8.6 |
APOE 3′-exon CpG island exhibited transcriptional enhancer/silencer activity, modulating expression of genes at the APOE locus in a cell type-, DNA methylation- and ε2/ε3/ε4 allele-specific manner. These results suggested a novel functional role for a 3′-exon CpG island involving the protein isoforms and also an epigenetically regulated transcriptional program |
| Ma et al., 2015 [76] | Cross-sectional | 475 men and 518 women | 18–87 | The 13 APOE CpG sites were categorized into three groups: Group 1 exhibited hypermethylation (>50%, in the promoter region), Group 2 showed hypomethylation (<50%, in the first two exons and introns), and Group 3 exhibited hypermethylation (>50%, in the exon 4). APOE methylation was significantly associated to age and plasma total cholesterol. APOE methylation patterns differed across APOE ε variants and the promoter variant rs405509, which further had a significant interaction with age |
| Wang et al., 2008 [77] | Cross-sectional | Prefrontal cortex AD: 24 Matched controls: 10 Blood samples AD: 6 Matched controls: 6 |
AD: 80.9 ± 9.3 matched controls: 80.0 ± 9.8 Blood samples AD: 81 ± 4.5 matched controls: 80.0 ± 5.2 |
In the AD brain samples, a notably age-specific epigenetic drift was identified, suggesting a role of epigenetic effects in the AD development. APOE gene is of bimodal structure, with a hypomethylated CpG-poor promoter and a fully methylated 39-CpG-island, containing the sequences for the ε4-haplotype |
CpG: 5′-C-phosphate-G-3′; CpG: cytosine-phosphate-guanine.
In the epigenetic scenario, miRNAs are known to be small non-coding RNAs with a length of ~22 nucleotides. They are also implicated in AD, as shown by the altered expression of miRNA 650 (miR-650) in AD brains [78]. Bioinformatic analysis showed that miR-650 may target the expression of three AD-related components: APOE, presenilin 1 (PSEN1), and cyclin-dependent kinase 5 (CDK5), with recent findings confirming that miR-650 may reduce in vitro the expression of APOE, PSEN1, and CDK5 [78].
5. Epigenetics of Apolipoprotein E and Cognitive Function: Contrasting Evidence in Alzheimer’s Disease
Several lifestyle and environmental stimuli could explain the effects of APOE genotype on AD and cognitive functioning, such as exercise [79], education [80], and vitamin D status [81] (Figure 2). Vitamin D is often referred to as a neurosteroid with neuroprotective and anti-inflammatory properties. Although the interplay between APOE genotype and vitamin D metabolism or transport in the nervous system is yet to be established, it is known that APOE contributes to the transport of lipid-soluble vitamins in the circulation and influences several immunological, inflammatory, and neurodegenerative processes [82]. Furthermore, APOE polymorphism and dietary responsiveness to fat-soluble vitamins, flavonoids, and n-3 PUFA were described, indicating APOE ε3 as a more flexible and responsive genotype than APOE ε4 [82]. Among implications for the development and progression of AD, vitamin D supplementation may be another potential strategy to consider for the APOE ε4 allele-carriers. Some reports showed that higher vitamin D concentrations in APOE ε4 homozygous carriers allow them to perform better at memory scores [83]. Then, compared to the APOE ε3/ε3-carriers, the APOE ε4-carriers showed earlier onset of cognitive impairment in AD. However, after the disease onset, the effect of the APOE genotype on the progression of cognitive impairment remained debated [84].
For this reason, epigenetic modifications of APOE, such as DNA methylation, may have a key role in maintaining intact cognitive function in older age. Growing DNA methylation levels at the APOE promoter region were found on postmortem prefrontal cortex samples of sporadic AD individuals using MALDI-TOF mass spectrometry and lymphocytes [77]. A notably age-specific epigenetic drift was identified, supporting a potential role of epigenetic effects in AD development. These results may partly explain the differences between APOE ε4 carriers and noncarriers in the benefits triggered by long-term exercise that might depend, at least partially, on mechanisms of metabolic response of prefrontal cortex to physical activity [79].
Numerous studies have indagated the relationship between APOE DNA methylation and AD or MCI [85,86,87]. Instead, the association between APOE DNA methylation and cognitive function in healthy subjects without cognitive impairment was evaluated by two studies, with controversial findings [88,89]. Liu and colleagues found an inverse association between DNA methylation in the APOE gene region and delayed recall capacity among 289 older African American people with a mean age of 67 years during normal cognitive aging [88]. Conversely, the other study, conducted in a large European cohort, observed no association between general cognitive functioning and APOE DNA methylation [89].
Many reports have suggested that neuroinflammation may have a key role in AD pathogenesis [90]. Dietary habits are known to influence systemic inflammation, neuroinflammation, and inflammaging [91]. A recent study conducted in a cohort of racially diverse middle-aged people (n = 411), pursued to identify DNA methylation sites associated with cognitive function in the genomic region of APOE. Regarding the inflammatory potential of the diet, among the dietary inflammatory index, cognitive performance, and the methylation level of several CpG sites have been detected significant relationships [92].
However, studies are contrasting in this regard, and whether epigenetic biomarkers could be used for predicting AD is still unclear. In the APOE gene, DNA methylation at two CpG sites (3/13) that are known to show age-dependent changes was related with the total cholesterol and high-density lipoprotein cholesterol ratio, but not with cognitive status, family history of AD, or the risk of cardiovascular disease in a blood-based DNA methylation study of 5828 people from the Generation Scotland cohort [89]. These findings supported that there is no evidence yet for considering APOE methylation as a biomarker for predicting AD or cardiovascular disease, although APOE methylation was associated with the blood levels of cholesterol [89].
Some limitations could affect specific methodologies used in the studies cited for assessing DNA methylation of APOE. Overall, at the transcriptional level, all major cell types have AD pathology, and single cell-level resolution may be critical; moreover, changes in gene expression, including directionality, can be conditional on cell type. The number of significant differentially expressed genes for non-neuronal populations were substantially smaller, likely reflecting reduced power in lower-abundance cell types [93]. Given that astrocytes are the primary producers of brain ApoE, alterations of epigenetically regulated APOE expression in glia may explain a significant part of the genetic AD risk linked to this gene [94]. Furthermore, although several imputation methods exist, a major deficiency lies in the inability to cope with large datasets, such as DNA methylation chips. Therefore, specific methods for imputing missing methylation data are needed [95].
6. Conclusions
In the panorama of current available evidence, the investigation of healthy aging and longevity is currently of remarkable interest. APOE could be considered an epigenetic mediator of senescence considering that different ApoE biochemical pathways in lipid metabolism, neuroinflammation, and neurodegeneration may contribute to longevity and healthy aging. Nonetheless, such areas of investigation are still increasing, since ApoE function in neurodegenerative diseases, particularly AD, cannot be uniquely explained by ApoE effects in lipid metabolism. Furthermore, the imbalance in the ApoE isoforms could explain the pathophysiological process of cognitive impairment linked to sporadic AD [20].
Stochastic factors (such environmental, diet, and pollution) may play a significant role in sporadic AD, despite the elevated lifetime risk linked to APOE ε3/ε4 and APOE ε4/ε4 genotypes. Indeed, according to the notion of stochastic risk or protective factors and although it is known that APOE ε4/ε4-carriers developed dementia about 10 years earlier than APOE ε2 carriers [96], there was still significant discrepancy in the age of onset for APOE ε4/ε4-carriers [22]. During the process of aging, the accumulation of molecular changes driven by genetic and epigenetic events in the organism lead to a loss of phenotypic plasticity over time. Also, epigenetics may be altered during aging processes, and this is particularly important, as age is the greatest risk factor for developing AD [97].
The epigenetic hallmarks of APOE and the impact of APOE epigenetics on aging and sporadic AD are mainly obtained from cross-sectional studies, while additional longitudinal findings are needed to obtain biomarkers of DNA methylation helpful for directionality of gene expression. Future longitudinal studies with methylation profiles are needed to provide a link between the APOE epigenetics and aging-related phenotypes and neurodegenerative disorders, including possible treatment. There is only one agent, the gene therapy LEX 1001, in the pipeline targeting the APOE ε4 allele. In this trial, a viral vector carrying the APOE ε2 allele is being given to antagonize the effects of APOE ε4 [20]. Some categories, i.e., epigenetic agents, have few therapeutic approaches in the pipeline; the present understanding of the biology of these processes may not have matured sufficiently to suggest target mechanisms for disease-modifying therapies [98]. Recent progress in the understanding of AD pathogenesis suggested that dysregulation of mRNA biogenesis may be involved in neurodegeneration. New methodological advances of AD treatment have developed short and synthetic antisense oligonucleotides that recognize target mRNA for posttranscriptional regulation to correct protein expression errors [99]. Dietary interventions may represent the most effective strategies in managing and regulating the onset of age-related diseases in humans, although they have not provided the promotion of longevity [100].
Author Contributions
Conceptualization, M.L.; methodology, M.L and F.P.; validation, R.S., V.D., F.C. and R.Z.; investigation, L.L.; resources, I.B.; data curation, I.B. and L.L.; writing—original draft preparation, M.L.; writing—review and editing, F.P., A.D., V.S. and A.B.; supervision, M.L. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This article does not contain any studies with human participants or animals performed by any of the authors.
Data Availability Statement
The datasets analyzed during the current review are available from the corresponding authors (M.L. and F.P.) upon reasonable request.
Conflicts of Interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Heyn H. A symbiotic liaison between the genetic and epigenetic code. Front. Genet. 2014;5:113. doi: 10.3389/fgene.2014.00113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mill J., Heijmans B.T. From promises to practical strategies in epigenetic epidemiology. Nat. Rev. Genet. 2013;14:585–594. doi: 10.1038/nrg3405. [DOI] [PubMed] [Google Scholar]
- 3.Frisoni G.B., Altomare D., Thal D.R., Ribaldi F., van der Kant R., Ossenkoppele R., Blennow K., Cummings J., van Duijn C., Nilsson P.M., et al. The probabilistic model of Alzheimer disease: The amyloid hypothesis revised. Nat. Rev. Neurosci. 2022;23:53–66. doi: 10.1038/s41583-021-00533-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coppieters N., Dragunow M. Epigenetics in Alzheimer’s disease: A focus on DNA modifications. Curr. Pharm. Des. 2011;17:3398–3412. doi: 10.2174/138161211798072544. [DOI] [PubMed] [Google Scholar]
- 5.Seripa D., Panza F., Paroni G., D’Onofrio G., Bisceglia P., Gravina C., Urbano M., Lozupone M., Solfrizzi V., Bizzarro A., et al. Role of CLU, PICALM, and TNK1 Genotypes in Aging with and without Alzheimer’s Disease. Mol. Neurobiol. 2018;55:4333–4344. doi: 10.1007/s12035-017-0547-x. [DOI] [PubMed] [Google Scholar]
- 6.Cavalli G., Heard E. Advances in epigenetics link genetics to the environment and disease. Nature. 2019;571:489–499. doi: 10.1038/s41586-019-1411-0. [DOI] [PubMed] [Google Scholar]
- 7.Zhang D., Cheng L., Badner J.A., Chen C., Chen Q., Luo W., Craig D.W., Redman M., Gershon E.S., Liu C. Genetic control of individual differences in gene-specific methylation in human brain. Am. J. Hum. Genet. 2010;86:411–419. doi: 10.1016/j.ajhg.2010.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gibbs J.R., van der Brug M.P., Hernandez D.G., Traynor B.J., Nalls M.A., Lai S.L., Arepalli S., Dillman A., Rafferty I.P., Troncoso J., et al. Abundant quantitative trait loci exist for DNA methylation and gene expression in human brain. PLoS Genet. 2010;6:e1000952. doi: 10.1371/journal.pgen.1000952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shoemaker R., Deng J., Wang W., Zhang K. Allele-specific methylation is prevalent and is contributed by CpG-SNPs in the human genome. Genome Res. 2010;20:883–889. doi: 10.1101/gr.104695.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Seripa D., D’Onofrio G., Panza F., Cascavilla L., Masullo C., Pilotto A. The genetics of the human APOE polymorphism. Rejuvenation Res. 2011;14:491–500. doi: 10.1089/rej.2011.1169. [DOI] [PubMed] [Google Scholar]
- 11.Nickerson D.A., Taylor S.L., Fullerton S.M., Weiss K.M., Clark A.G., Stengård J.H., Salomaa V., Boerwinkle E., Sing C.F. Sequence diversity and large-scale typing of SNPs in the human apolipoprotein E gene. Genome Res. 2000;10:1532–1545. doi: 10.1101/gr.146900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yu C.E., Foraker J. Epigenetic considerations of the APOE gene. Biomol. Concepts. 2015;6:77–84. doi: 10.1515/bmc-2014-0039. [DOI] [PubMed] [Google Scholar]
- 13.Corder E.H., Saunders A.M., Strittmatter W.J., Schmechel D.E., Gaskell P.C., Small G.W., Roses A.D., Haines J.L., Pericak-Vance M.A. Gene dose of apolipoprotein e type 4 allele and the risk of Alzheimer’s disease in late onset families. Science. 1993;261:921–923. doi: 10.1126/science.8346443. [DOI] [PubMed] [Google Scholar]
- 14.Chartier-Harlin M.C., Parfitt M., Legrain S., Pérez-Tur J., Brousseau T., Evans A., Berr C., Odile V., Roques P., Gourlet V., et al. Apolipoprotein E, epsilon 4 allele as a major risk factor for sporadic early and late-onset forms of alzheimer’s disease: Analysis of the 19q13,2 chromosomal region. Hum. Mol. Genet. 1994;3:569–574. doi: 10.1093/hmg/3.4.569. [DOI] [PubMed] [Google Scholar]
- 15.Farrer L.A., Cupples L.A., Haines J.L., Hyman B., Kukull W.A., Mayeux R., Myers R.H., Pericak-Vance M.A., Risch N., van Duijn C.M. Effects of age, sex, and ethnicity on the association between apolipoprotein e genotype and alzheimer disease: A meta-analysis. JAMA. 1997;278:1349–1356. doi: 10.1001/jama.1997.03550160069041. [DOI] [PubMed] [Google Scholar]
- 16.Genin E., Hannequin D., Wallon D., Sleegers K., Hiltunen M., Combarros O., Bullido M.J., Engelborghs S., De Deyn P., Berr C., et al. APOE and Alzheimer disease: A major gene with semi-dominant inheritance. Mol. Psychiatry. 2011;16:903–907. doi: 10.1038/mp.2011.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Corder E.H., Saunders A.M., Risch N.J., Strittmatter W.J., Schmechel D.E., Gaskell P.C., Jr., Rimmler J.B., Locke P.A., Conneally P.M., Schmader K.E., et al. Protective effect of apolipoprotein e type 2 allele for late onset Alzheimer disease. Nat. Genet. 1994;7:180–184. doi: 10.1038/ng0694-180. [DOI] [PubMed] [Google Scholar]
- 18.Panza F., Solfrizzi V., Torres F., Mastroianni F., Colacicco A.M., Basile A.M., Capurso C., D’Introno A., Del Parigi A., Capurso A. Apolipoprotein E in Southern Italy: Protective effect of epsilon 2 allele in early- and late-onset sporadic Alzheimer’s disease. Neurosci. Lett. 2000;292:79–82. doi: 10.1016/S0304-3940(00)01447-6. [DOI] [PubMed] [Google Scholar]
- 19.Mayeux R., Saunders A.M., Shea S., Mirra S., Evans D., Roses A.D., Hyman B.T., Crain B., Tang M.X., Phelps C.H. Utility of the apolipoprotein E genotype in the diagnosis of Alzheimer’s disease. Alzheimer’s disease centers consortium on apolipoprotein E and Alzheimer’s disease. N. Engl. J. Med. 1998;338:506–511. doi: 10.1056/NEJM199802193380804. [DOI] [PubMed] [Google Scholar]
- 20.Lozupone M., Imbimbo B.P., Balducci C., Lo Vecchio F., Bisceglia P., Latino R.R., Leone M., Dibello V., Solfrizzi V., Greco A., et al. Does the imbalance in the apolipoprotein E isoforms underlie the pathophysiological process of sporadic Alzheimer’s disease? Alzheimer’s Dement. 2023;19:353–368. doi: 10.1002/alz.12728. [DOI] [PubMed] [Google Scholar]
- 21.Serrano-Pozo A., Das S., Hyman B.T. APOE and Alzheimer’s disease: Advances in genetics, pathophysiology, and therapeutic approaches. Lancet Neurol. 2021;20:68–80. doi: 10.1016/S1474-4422(20)30412-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reiman E.M., Arboleda-Velasquez J.F., Quiroz Y.T., Huentelman M.J., Beach T.G., Caselli R.J., Chen Y., Su Y., Myers A.J., Hardy J., et al. Exceptionally low likelihood of Alzheimer’s dementia in APOE2 homozygotes from a 5000-person neuropathological study. Nat. Commun. 2020;11:667. doi: 10.1038/s41467-019-14279-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Salvadó G., Grothe M.J., Groot C., Moscoso A., Schöll M., Gispert J.D., Ossenkoppele R., Alzheimer’s Disease Neuroimaging Initiative Differential associations of APOE-ε2 and APOE-ε4 alleles with PET-measured amyloid-β and tau deposition in older individuals without dementia. Eur. J. Nucl. Med. Mol. Imaging. 2021;48:2212–2224. doi: 10.1007/s00259-021-05192-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Therriault J., Benedet A.L., Pascoal T.A., Mathotaarachchi S., Chamoun M., Savard M., Thomas E., Kang M.S., Lussier F., Tissot C., et al. Association of Apolipoprotein E 4 With Medial Temporal Tau Independent of Amyloid-β. JAMA Neurol. 2020;77:470–479. doi: 10.1001/jamaneurol.2019.4421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Krasemann S., Madore C., Cialic R., Baufeld C., Calcagno N., El Fatimy R., Beckers L., O’Loughlin E., Xu Y., Fanek Z., et al. The TREM2-APOE Pathway Drives the Transcriptional Phenotype of Dysfunctional Microglia in Neurodegenerative Diseases. Immunity. 2017;47:566–581.e9. doi: 10.1016/j.immuni.2017.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen Y., Hong T., Chen F., Sun Y., Wang Y., Cui L. Interplay between microglia and Alzheimer’s disease-focus on the most relevant risks: APOE genotype, sex and age. Front. Aging Neurosci. 2021;13:631827. doi: 10.3389/fnagi.2021.631827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chung W.S., Verghese P.B., Chakraborty C., Joung J., Hyman B.T., Ulrich J.D., Holtzman D.M., Barres B.A. Novel allele-dependent role for APOE in controlling the rate of synapse pruning by astrocytes. Proc. Natl. Acad. Sci. USA. 2016;113:10186–10191. doi: 10.1073/pnas.1609896113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Blanchard J.W., Bula M., Davila-Velderrain J., Akay L.A., Zhu L., Frank A., Victor M.B., Bonner J.M., Mathys H., Lin Y.T., et al. Reconstruction of the human blood-brain barrier in vitro reveals a pathogenic mechanism of APOE4 in pericytes. Nat. Med. 2020;26:952–963. doi: 10.1038/s41591-020-0886-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Riphagen J.M., Ramakers I.H.G.M., Freeze W.M., Pagen L.H.G., Hanseeuw B.J., Verbeek M.M., Verhey F.R.J., Jacobs H.I.L. Linking APOE-ε4, blood-brain barrier dysfunction, and inflammation to Alzheimer’s pathology. Neurobiol. Aging. 2020;85:96–103. doi: 10.1016/j.neurobiolaging.2019.09.020. [DOI] [PubMed] [Google Scholar]
- 30.Strittmatter W.J., Saunders A.M., Schmechel D., Pericak-Vance M., Enghild J., Salvesen G.S., Roses A.D. Apolipoprotein e: High-avidity binding to beta-amyloid and increased frequency of type 4 allele in late-onset familial alzheimer disease. Proc. Natl. Acad. Sci. USA. 1993;90:1977–1981. doi: 10.1073/pnas.90.5.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fagan A.M., Holtzman D.M. Astrocyte lipoproteins, effects of ApoE on neuronal function, and role of ApoE in amyloid-beta deposition in vivo. Microsc. Res. Tech. 2000;50:297–304. doi: 10.1002/1097-0029(20000815)50:4<297::AID-JEMT9>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 32.Tokuda T., Calero M., Matsubara E., Vidal R., Kumar A., Permanne B., Zlokovic B., Smith J.D., Ladu M.J., Rostagno A., et al. Lipidation of apolipoprotein e influences its isoform-specific interaction with Alzheimer’s amyloid beta peptides. Biochem. J. 2002;348:359–365. doi: 10.1042/bj3480359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Deane R., Sagare A., Hamm K., Parisi M., Lane S., Finn M.B., Holtzman D.M., Zlokovic B.V. ApoE isoform-specific disruption of amyloid beta peptide clearance from mouse brain. J. Clin. Investig. 2008;118:4002–40013. doi: 10.1172/JCI36663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Castellano J.M., Kim J., Stewart F.R., Jiang H., DeMattos R.B., Patterson B.W., Fagan A.M., Morris J.C., Mawuenyega K.G., Cruchaga C., et al. Human ApoE isoforms differentially regulate brain amyloid-beta peptide clearance. Sci. Transl. Med. 2011;3:89ra57. doi: 10.1126/scitranslmed.3002156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huang Y.A., Zhou B., Wernig M., Sudhof T.C. ApoE2, ApoE3, and ApoE4 differentially stimulate APP transcription and A-β secretion. Cell. 2017;168:427.e21–441.e21. doi: 10.1016/j.cell.2016.12.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sala Frigerio C., Wolfs L., Fattorelli N., Thrupp N., Voytyuk I., Schmidt I., Mancuso R., Chen W.T., Woodbury M.E., Srivastava G., et al. The Major Risk Factors for Alzheimer’s Disease: Age, Sex, and Genes Modulate the Microglia Response to Aβ Plaques. Cell Rep. 2019;27:1293–1306.e6. doi: 10.1016/j.celrep.2019.03.099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shi Y., Holtzman D.M. Interplay between innate immunity and Alzheimer disease: APOE and TREM2 in the spotlight. Nat. Rev. Immunol. 2018;18:759–772. doi: 10.1038/s41577-018-0051-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhao N., Liu C.C., Van Ingelgom A.J., Linares C., Kurti A., Knight J.A., Heckman M.G., Diehl N.N., Shinohara M., Martens Y.A., et al. APOE ε2 is associated with increased tau pathology in primary tauopathy. Nat. Commun. 2018;9:4388. doi: 10.1038/s41467-018-06783-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lozupone M., Panza F. Impact of apolipoprotein E isoforms on sporadic Alzheimer’s disease: Beyond the role of amyloid beta. Neural Regen. Res. 2024;19:80–83. doi: 10.4103/1673-5374.375316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Foraker J., Millard S.P., Leong L., Thomson Z., Chen S., Keene C.D., Bekris L.M., Yu C.E. The APOE Gene is Differentially Methylated in Alzheimer’s Disease. J. Alzheimer’s Dis. 2015;48:745–755. doi: 10.3233/JAD-143060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rueter J., Rimbach G., Huebbe P. Allelic variation within the major APOE CpG island affects its methylation in the brain of targeted replacement mice expressing human APOE. Biochim. Biophys. Acta Gene Regul. Mech. 2023;1866:194942. doi: 10.1016/j.bbagrm.2023.194942. [DOI] [PubMed] [Google Scholar]
- 42.Lefterov I., Fitz N.F., Lu Y., Koldamova R. APOEε4 and risk of Alzheimer’s disease—Time to move forward. Front. Neurosci. 2023;17:1195724. doi: 10.3389/fnins.2023.1195724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sullivan P.M., Mezdour H., Aratani Y., Knouff C., Najib J., Reddick R.L., Quarfordt S.H., Maeda N. Targeted replacement of the mouse apolipoprotein E gene with the common human APOE3 allele enhances diet-induced hypercholesterolemia and atherosclerosis. J. Biol. Chem. 1997;272:17972–17980. doi: 10.1074/jbc.272.29.17972. [DOI] [PubMed] [Google Scholar]
- 44.Livingston G., Huntley J., Sommerlad A., Ames D., Ballard C., Banerjee S., Brayne C., Burns A., Cohen-Mansfield J., Cooper C., et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396:413–446. doi: 10.1016/S0140-6736(20)30367-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Reas E.T., Laughlin G.A., Bergstrom J., Kritz-Silverstein D., Barrett-Connor E., McEvoy L.K. Effects of APOE on cognitive aging in community-dwelling older adults. Neuropsychology. 2019;33:406–416. doi: 10.1037/neu0000501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mahley R.W. Apolipoprotein E: Cholesterol transport protein with expanding role in cell biology. Science. 1988;240:622–630. doi: 10.1126/science.3283935. [DOI] [PubMed] [Google Scholar]
- 47.Siest G., Pillot T., Regis-Bailly A., Leininger-Muller B., Steinmetz J., Galteau M.M., Visvikis S. Apolipoprotein E: An important gene and protein to follow in laboratory medicine. Clin. Chem. 1995;41:1068–1086. doi: 10.1093/clinchem/41.8.1068. [DOI] [PubMed] [Google Scholar]
- 48.Seripa D., Franceschi M., Matera M.G., Panza F., Kehoe P.G., Gravina C., Orsitto G., Solfrizzi V., Di Minno G., Dallapiccola B., et al. Sex differences in the association of apolipoprotein e and angiotensin-converting enzyme gene polymorphisms with healthy aging and longevity: A population-based study from Southern Italy. J. Gerontol. A Biol. Sci. Med. Sci. 2006;61:918–923. doi: 10.1093/gerona/61.9.918. [DOI] [PubMed] [Google Scholar]
- 49.Seripa D., Panza F., Franceschi M., D’Onofrio G., Solfrizzi V., Dallapiccola B., Pilotto A. Non-apolipoprotein E and apolipoprotein E genetics of sporadic Alzheimer’s disease. Ageing Res. Rev. 2009;8:214–236. doi: 10.1016/j.arr.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 50.Mahley R.W., Rall S.C., Jr. Apolipoprotein E: Far more than a lipid transport protein. Annu. Rev. Genom. Hum. Genet. 2000;1:507–537. doi: 10.1146/annurev.genom.1.1.507. [DOI] [PubMed] [Google Scholar]
- 51.Yanagisawa K. Cholesterol and pathological processes in Alzheimer’s disease. J. Neurosci. Res. 2002;70:361–366. doi: 10.1002/jnr.10348. [DOI] [PubMed] [Google Scholar]
- 52.Ordovas J.M., Lopez-Miranda J., Mata P., Perez-Jimenez F., Lichtenstein A.H., Schaefer E.J. Gene-diet interaction in determining plasma lipid response to dietary intervention. Atherosclerosis. 1995;118:S11–S27. doi: 10.1016/0021-9150(95)90069-1. [DOI] [PubMed] [Google Scholar]
- 53.Grimm M.O.W., Michaelson D.M., Hartmann T. Omega-3 fatty acids, lipids, and ApoE lipidation in Alzheimer’s disease: A rationale for multi-nutrient dementia prevention. J. Lipid Res. 2017;58:2083–2101. doi: 10.1194/jlr.R076331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bos M.M., Noordam R., Blauw G.J., Slagboom P.E., Rensen P.C.N., van Heemst D. The ApoE ε4 Isoform: Can the Risk of Diseases be Reduced by Environmental Factors? J. Gerontol. A Biol. Sci. Med. Sci. 2019;74:99–107. doi: 10.1093/gerona/gly226. [DOI] [PubMed] [Google Scholar]
- 55.Brooks-Wilson A.R. Genetics of healthy aging and longevity. Hum. Genet. 2013;132:1323–1338. doi: 10.1007/s00439-013-1342-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sebastiani P., Gurinovich A., Nygaard M., Sasaki T., Sweigart B., Bae H., Andersen S.L., Villa F., Atzmon G., Christensen K., et al. APOE alleles and extreme human longevity. J. Gerontol. A Biol. Sci. Med. Sci. 2018;74:44–51. doi: 10.1093/gerona/gly174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Smith J.D. Apolipoproteins and aging: Emerging mechanisms. Ageing Res. Rev. 2002;1:345–365. doi: 10.1016/S1568-1637(02)00005-3. [DOI] [PubMed] [Google Scholar]
- 58.Feng J., Xiang L., Wan G., Qi K., Sun L., Huang Z., Zheng C., Lv Z., Hu C., Yang Z. Is APOE ε3 a favorable factor for the longevity: An association study in Chinese population. J. Genet. 2011;90:343–347. doi: 10.1007/s12041-011-0075-9. [DOI] [PubMed] [Google Scholar]
- 59.Paik Y.K., Chang D.J., Reardon C.A., Walker M.D., Taxman E., Taylor J.M. Identification and characterization of transcriptional regulatory regions associated with expression of the human apolipoprotein E gene. J. Biol. Chem. 1988;263:13340–13349. doi: 10.1016/S0021-9258(18)37710-X. [DOI] [PubMed] [Google Scholar]
- 60.Lambert J.C., Perez-Tur J., Dupire M.J., Galasko D., Mann D., Amouyel P., Hardy J., Delacourte A., Chartier-Harlin M.C. Distortion of allelic expression of apolipoprotein E in Alzheimer’s disease. Hum. Mol. Genet. 1997;6:2151–2154. doi: 10.1093/hmg/6.12.2151. [DOI] [PubMed] [Google Scholar]
- 61.Mui S., Briggs M., Chung H., Wallace R.B., Gomez-Isla T., Rebeck G.W., Hyman B.T. A newly identified polymorphism in the apolipoprotein E enhancer gene region is associated with Alzheimer’s disease and strongly with the epsilon 4 allele. Neurology. 1996;47:196–201. doi: 10.1212/WNL.47.1.196. [DOI] [PubMed] [Google Scholar]
- 62.Lambert J.C., Berr C., Pasquier F., Delacourte A., Frigard B., Cottel D., Pérez-Tur J., Mouroux V., Mohr M., Cécyre D., et al. Pronounced impact of Th1/E47cs mutation compared with-491 AT mutation on neural APOE gene expression and risk of developing Alzheimer’s disease. Hum. Mol. Genet. 1998;7:1511–1516. doi: 10.1093/hmg/7.9.1511. [DOI] [PubMed] [Google Scholar]
- 63.Lambert J.C., Brousseau T., Defosse V., Evans A., Arveiler D., Ruidavets J.B., Haas B., Cambou J.P., Luc G., Ducimetière P., et al. Independent association of an APOE gene promoter polymorphism with increased risk of myocardial infarction and decreased APOE plasma concentrations-the ECTIM study. Hum. Mol. Genet. 2000;9:57–61. doi: 10.1093/hmg/9.1.57. [DOI] [PubMed] [Google Scholar]
- 64.Lambert J.C., Pasquier F., Cottel D., Frigard B., Amouyel P., Chartier-Harlin M.C. A new polymorphism in the APOE promoter associated with risk of developing Alzheimer’s disease. Hum. Mol. Genet. 1998;7:533–540. doi: 10.1093/hmg/7.3.533. [DOI] [PubMed] [Google Scholar]
- 65.Bullido M.A.J., and Valdivieso F. Apolipoprotein E gene promoter polymorphisms in Alzheimer’s disease. Microsc. Res. Tech. 2000;50:261–267. doi: 10.1002/1097-0029(20000815)50:4<261::AID-JEMT2>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 66.Lumsden A.L., Mulugeta A., Zhou A., Hypponen E. Apolipoprotein E (APOE) genotype-associated disease risks: A phenome-wide, registry-based, case-control study utilising the UK biobank. eBioMedicine. 2020;59:102954. doi: 10.1016/j.ebiom.2020.102954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Artiga M.J., Bullido M.J., Frank A., Sastre I., Recuero M., García M.A., Lendon C.L., Han S.W., Morris J.C., Vázquez J., et al. Risk for Alzheimer’s disease correlates with transcriptional activity of the APOE gene. Hum. Mol. Genet. 1998;7:1887–1892. doi: 10.1093/hmg/7.12.1887. [DOI] [PubMed] [Google Scholar]
- 68.Sims R., van der Lee S.J., Naj A.C., Bellenguez C., Badarinarayan N., Jakobsdottir J., Kunkle B.W., Boland A., Raybould R., Bis J.C., et al. Rare coding variants in PLCG2, ABI3, and TREM2 implicate microglial-mediated innate immunity in Alzheimer’s disease. Nat. Genet. 2017;49:1373–1384. doi: 10.1038/ng.3916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lee E.G., Tulloch J., Chen S., Leong L., Saxton A.D., Kraemer B., Darvas M., Keene C.D., Shutes-David A., Todd K., et al. Redefining transcriptional regulation of the APOE gene and its association with Alzheimer’s disease. PLoS ONE. 2020;15:e0227667. doi: 10.1371/journal.pone.0227667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Medvedeva Y.A., Fridman M.V., Oparina N.J., Malko D.B., Ermakova E.O., Kulakovskiy I.V., Heinzel A., Makeev V.J. Intergenic, gene terminal, and intragenic CpG islands in the human genome. BMC Genom. 2010;11:48. doi: 10.1186/1471-2164-11-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Maunakea A.K., Nagarajan R.P., Bilenky M., Ballinger T.J., D’Souza C., Fouse S.D., Johnson B.E., Hong C., Nielsen C., Zhao Y., et al. Conserved role of intragenic DNA methylation in regulating alternative promoters. Nature. 2010;466:253–257. doi: 10.1038/nature09165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gellersen H.M., Guell X., Sami S. Differential vulnerability of the cerebellum in healthy ageing and Alzheimer’s disease. Neuroimage Clin. 2021;30:102605. doi: 10.1016/j.nicl.2021.102605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yu C.E., Cudaback E., Foraker J., Thomson Z., Leong L., Lutz F., Gill J.A., Saxton A., Kraemer B., Navas P., et al. Epigenetic signature and enhancer activity of the human APOE gene. Hum. Mol. Genet. 2013;22:5036–5047. doi: 10.1093/hmg/ddt354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hendrich B., Bird A. Identification and characterization of a family of mammalian methyl-CpG binding proteins. Mol. Cell. Biol. 1998;18:6538–6547. doi: 10.1128/MCB.18.11.6538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cedar H., Bergman Y. Programming of DNA methylation patterns. Annu. Rev. Biochem. 2012;81:97–117. doi: 10.1146/annurev-biochem-052610-091920. [DOI] [PubMed] [Google Scholar]
- 76.Ma Y., Smith C.E., Lai C.Q., Irvin M.R., Parnell L.D., Lee Y.C., Pham L., Aslibekyan S., Claas S.A., Tsai M.Y., et al. Genetic variants modify the effect of age on APOE methylation in the Genetics of Lipid Lowering Drugs and Diet Network study. Aging Cell. 2015;14:49–59. doi: 10.1111/acel.12293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wang S.C., Oelze B., Schumacher A. Age-specific epigenetic drift in late-onset Alzheimer’s disease. PLoS ONE. 2008;3:e2698. doi: 10.1371/journal.pone.0002698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lin L., Liu X., Cheng X., Li Y., Gearing M., Levey A., Huang X., Li Y., Jin P., Li X. MicroRNA-650 Regulates the Pathogenesis of Alzheimer’s Disease Through Targeting Cyclin-Dependent Kinase 5. Mol. Neurobiol. 2023;60:2426–2441. doi: 10.1007/s12035-023-03224-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.De Marco M., Clough P.J., Dyer C.E., Vince R.V., Waby J.S., Midgley A.W., Venneri A. Apolipoprotein E epsilon allele modulates the immediate impact of acute exercise on prefrontal function. Behav. Genet. 2014;45:106–116. doi: 10.1007/s10519-014-9675-5. [DOI] [PubMed] [Google Scholar]
- 80.Cook C.J., Fletcher J.M. Can education rescue genetic liability for cognitive decline? Social Sci. Med. 2015;127:159–170. doi: 10.1016/j.socscimed.2014.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Maddock J., Cavadino A., Power C., Hyppönen E. 25-hydroxyvitamin D, APOE ε4 genotype and cognitive function: Findings from the 1958 British birth cohort. Eur. J. Clin. Nutr. 2015;69:505–508. doi: 10.1038/ejcn.2014.201. [DOI] [PubMed] [Google Scholar]
- 82.Egert S., Rimbach G., Huebbe P. Symposium on ‘Metabolic flexibility in animal and human nutrition’ Session IV: Nutritional compounds for optimized healthspan and life performance: ApoE genotype: From geographic distribution to function and responsiveness to dietary factors. Proc. Nutr. Soc. 2012;71:410–424. doi: 10.1017/S0029665112000249. [DOI] [PubMed] [Google Scholar]
- 83.Panza F., La Montagna M., Lampignano L., Zupo R., Bortone I., Castellana F., Sardone R., Borraccino L., Dibello V., Resta E., et al. Vitamin D in the development and progression of alzheimer’s disease: Implications for clinical management. Expert Rev. Neurother. 2021;2:287–301. doi: 10.1080/14737175.2021.1873768. [DOI] [PubMed] [Google Scholar]
- 84.Suzuki K., Hirakawa A., Ihara R., Iwata A., Ishii K., Ikeuchi T., Sun C.K., Donohue M., Iwatsubo T., Alzheimer’s Disease Neuroimaging Initiative, Japanese Alzheimer’s Disease Neuroimaging Initiative Effect of apolipoprotein E ε4 allele on the progression of cognitive decline in the early stage of Alzheimer’s disease. Alzheimer’s Dement. 2020;6:e12007. doi: 10.1002/trc2.12007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Karlsson I.K., Ploner A., Wang Y., Gatz M., Pedersen N.L., Hagg S. Apolipoprotein E DNA methylation and late-life disease. Int. J. Epidemiol. 2018;47:899–907. doi: 10.1093/ije/dyy025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Shao Y., Shaw M., Todd K., Khrestian M., D’Aleo G., Barnard P.J., Zahratka J., Pillai J., Yu C.E., Keene C.D., et al. DNA methyla-tion of TOMM40-APOE-APOC2 in Alzheimer’s disease. J. Hum. Genet. 2018;63:459–471. doi: 10.1038/s10038-017-0393-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Mancera-Paez O., Estrada-Orozco K., Mahecha M.F., Cruz F., Bonilla-Vargas K., Sandoval N., Guerrero E., Salcedo-Tacuma D., Melgarejo J.D., Vega E., et al. Differential methylation in APOE (Chr19; exon four; from 44,909,188 to 44,909,373/hg38) and increased apolipoprotein E plasma levels in subjects with mild cognitive impairment. Int. J. Mol. Sci. 2019;20:1394. doi: 10.3390/ijms20061394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Liu J., Zhao W., Ware E.B., Turner S.T., Mosley T.H., Smith J.A. DNA methylation in the APOE genomic region is associated with cognitive function in African Americans. BMC Med. Genom. 2018;11:43. doi: 10.1186/s12920-018-0363-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Mur J., McCartney D.L., Walker R.M., Campbell A., Bermingham M.L., Morris S.W., Porteous D.J., McIntosh A.M., Deary I.J., Evans K.L., et al. DNA methylation in APOE: The relationship with Alzheimer’s and with cardiovascular health. Alzheimer’s Dement. 2020;6:e12026. doi: 10.1002/trc2.12026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Heneka M.T., Carson M.J., El Khoury J., Landreth G.E., Brosseron F., Feinstein D.L., Jacobs A.H., Wyss-Coray T., Vitorica J., Ransohoff R.M., et al. Neuroinflammation in Alzheimer’s disease. Lancet Neurol. 2015;14:388–405. doi: 10.1016/S1474-4422(15)70016-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Griseta C., Battista P., Castellana F., Colonna I., Sciarra S., Zupo R., Bortone I., Lampignano L., Tirelli S., Bernardino G., et al. Serum levels of IL-6 are associated with cognitive impairment in the salus in apulia population-based study. Heliyon. 2023;9:e13972. doi: 10.1016/j.heliyon.2023.e13972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Shen B., Hernandez D.G., Chitrala K.N., Fanelli-Kuczmarski M.T., Noren Hooten N., Pacheco N.L., Mode N.A., Zonderman A.B., Ezike N., Evans M.K. APOE gene region methylation is associated with cognitive performance in middle-aged urban adults. Neurobiol. Aging. 2022;116:41–48. doi: 10.1016/j.neurobiolaging.2022.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mathys H., Davila-Velderrain J., Peng Z., Gao F., Mohammadi S., Young J.Z., Menon M., He L., Abdurrob F., Jiang X., et al. Single-cell transcriptomic analysis of Alzheimer’s disease. Nature. 2019;570:332–337. doi: 10.1038/s41586-019-1195-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Tulloch J., Leong L., Thomson Z., Chen S., Lee E.G., Keene C.D., Millard S.P., Yu C.E. Glia-specific APOE epigenetic changes in the Alzheimer’s disease brain. Brain Res. 2018;1698:179–186. doi: 10.1016/j.brainres.2018.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Di Lena P., Sala C., Prodi A., Nardini C. Missing value estimation methods for DNA methylation data. Bioinformatics. 2019;35:3786–3793. doi: 10.1093/bioinformatics/btz134. [DOI] [PubMed] [Google Scholar]
- 96.Slooter A.J.C., Cruts M., Kalmijn S., Hofman A., Breteler M.M., Van Broeckhoven C., van Duijn C.M. Risk estimates of dementia by apolipoprotein E genotypes from a population-based incidence study: The Rotterdam Study. Arch. Neurol. 1998;55:964–968. doi: 10.1001/archneur.55.7.964. [DOI] [PubMed] [Google Scholar]
- 97.Pogribny I.P., Vanyushin B.F. Age-related Genomic Hypomethylation. In: Tollefsbol T.O., editor. Epigenetics of Aging. Springer; Berlin/Heidelberg, Germany: 2009. pp. 11–27. [Google Scholar]
- 98.Cummings J.L., Osse A.M.L., Kinney J.W. Alzheimer’s Disease: Novel Targets and Investigational Drugs for Disease Modification. Drugs. 2023;83:1387–1408. doi: 10.1007/s40265-023-01938-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lozupone M., Dibello V., Sardone R., Castellana F., Zupo R., Lampignano L., Bortone I., Stallone R., Altamura M., Bellomo A., et al. The development of peptide- and oligonucleotide-based drugs to prevent the formation of abnormal tau in tauopathies. Expert Opin. Drug Discov. 2023;18:515–526. doi: 10.1080/17460441.2023.2200245. [DOI] [PubMed] [Google Scholar]
- 100.Costa D., Scognamiglio M., Fiorito C., Benincasa G., Napoli C. Genetic background, epigenetic factors and dietary interventions which influence human longevity. Biogerontology. 2019;20:605–626. doi: 10.1007/s10522-019-09824-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analyzed during the current review are available from the corresponding authors (M.L. and F.P.) upon reasonable request.