We are reporting the first case of oxcarbazepine-induced immunoglobulin deficiency. Although this is known to be a rare adverse reaction to various pharmacologics (1, 4, 5), including the anticonvulsant carbamazepine (3, 6, 10, 11), it has not been previously described with oxcarbazepine.
A 49-year-old white female was referred for further investigation of low serum immunoglobulins found as part of an evaluation for chronic bacterial vaginitis and suspected immune deficiency. Her infectious history was significant for one episode of pneumonia, several episodes of sinusitis, and chronic bladder infections.
As a part of her immunologic evaluation, causes of secondary hypogammaglobulinemia were considered. She had no evidence of gastrointestinal protein loss and no evidence of malignancy and was not taking any immunosuppressive medications. She had been given oxcarbazepine (1,800-mg total daily dose), a derivative of the anticonvulsant carbamazepine, for chronic pain.
At referral, immunoglobulin levels were low (immunoglobulin G [IgG], 576 mg/dl; IgA, <11 mg/dl; IgM, <4 mg/dl) and she had a B-cell deficiency (1%, 18 B cells/mm3 [normal, 5 to 15%, 75 to 375 B cells/mm3]). She maintained positive (immune) IgG responses to measles, rubella, mumps, tetanus, and diphtheria. Antibody responses 1 month after pneumococcal vaccination were poor (protective antibody, 1.3 μg/ml, to only 2 out of 12 serotypes tested).
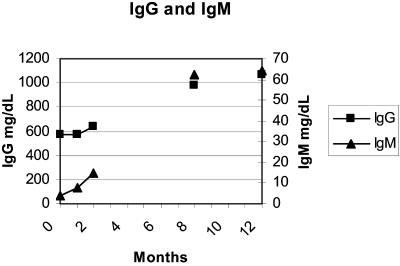
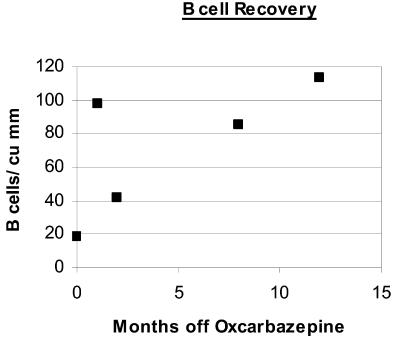
Suspecting a potential adverse reaction to oxcarbazepine, this medication was discontinued; immunoglobulin levels and B-cell numbers remained low for at least 2 months. Her IgG and IgM levels returned to normal after 8 months (IgG, 977 mg/dl; IgA, <7 mg/dl; IgM, 62 mg/dl), with normalized B-cell numbers (5%; 85 B cells/mm3), and remained normal at 12 months (IgG, 1,065 mg/dl; IgA, <15 mg/dl; IgM, 64 mg/dl; 113 B cells/mm3 [7%]), with protective antibody responses to 5 out of 12 pneumococcal serotypes (Fig. 1 and 2). She continued to have IgA deficiency. Her chronic pain returned with the discontinuation of oxcarbazepine.
FIG. 1.
Immunoglobulin level recovery after discontinuation of oxcarbazepine.
FIG. 2.
B-cell recovery after discontinuation of oxcarbazepine. cu, cubic.
The patient's initial evaluation suggested the possible diagnosis of the primary immunodeficiency common variable immune deficiency with hypogammaglobulinemia and specific antibody deficiency (8), but her moderately low IgG, with very low IgA, IgM, and B cells, was atypical for this diagnosis. This led us to suspect a potential secondary cause for these findings. The most likely cause was oxcarbazepine, derived from carbamazepine by the addition of an oxide to the middle ring, since the parent compound carbamazepine may lead to hypogammaglobulinemia. After discontinuing this drug, serum IgG and IgM levels increased, response to pneumococcal vaccination improved, and peripheral B-cell numbers normalized. It is unclear if persistent IgA deficiency in our patient was a pre-existing condition, possibly predisposing her to this adverse reaction to oxcarbazepine, or induced by the oxcarbazepine.
The mechanism underlying this side effect remains unknown and has not been noted to have any relationship to dose or duration of anticonvulsant use in other medications. The serum half-life of oxcarbazepine is 2 h, and that of its 10-monohydroxy active metabolite is 9 h. A relatively prolonged time elapsed between drug elimination from the serum and B-cell recovery, suggesting indirect factors may play a role. Hypogammaglobulinemia may result from other anticonvulsants and anti-inflammatory medications, including valproic acid, phenytoin, gold, sulfasalazine, chloroquine, penicillamine, fenclofenac, hydantoin, zonisamide, lamotrigine, and cyclosporine A (1, 4, 5, 9).
As indications for anticonvulsant use are broadening with reports of efficacy in pain syndromes and psychiatric illnesses (2, 7), more cases of secondary hypogammaglobulinemia are likely to occur.
Secondary hypogammaglobulinemia should always be considered before diagnosing a primary immunodeficiency such as common variable immune deficiency and committing patients to lifelong immunoglobulin therapy.
REFERENCES
- 1.Basaran, N., F. Hincal, E. Kansu, and A. Ciger. 1994. Humoral and cellular immune parameters in untreated and phenytoin-or carbamazepine-treated epileptic patients. Int. J. Immunopharmacol. 16:1071-1077. [DOI] [PubMed] [Google Scholar]
- 2.Belmaker, R. H. 2004. Bipolar disorder. N. Engl. J. Med. 351:476-486. [DOI] [PubMed] [Google Scholar]
- 3.Castro, A. P., M. G. Redmershi, A. C. Pastorino, J. A. de Paz, A. B. Fomin, and C. M. Jacob. 2001. Secondary hypogammaglobulinemia after use of carbamazepine: case report and review. Rev. Hosp. Clin. Fac. Med. Sao Paulo 56:189-192. [DOI] [PubMed] [Google Scholar]
- 4.Garzon, P., S. Gonzalez-Cornejo, G. Hernandez-Hernandez, L. Aguirre-Portillo, C. Almodovar-Cuevas, and A. Navarro-Ruiz. 1986. Effects of antiepileptic drugs on concentration of serum proteins and immunoglobulins of epileptic patients. Gen. Pharmacol. 17:49-55. [DOI] [PubMed] [Google Scholar]
- 5.Hammarstrom, L., I. Vorechovsky, and D. Webster. 2000. Selective IgA deficiency (SIgAD) and common variable immunodeficiency (CVID). Clin. Exp. Immunol. 120:225-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hayman, G., and A. Bansal. 2002. Antibody deficiency associated with carbamazepine. BMJ 325:1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rogawski, M. A., and W. Loscher. 2004. The neurobiology of antiepileptic drugs for the treatment of nonepileptic conditions. Nat. Med. 10:685-692. [DOI] [PubMed] [Google Scholar]
- 8.Simonte, S. J., and C. Cunningham-Rundles. 2003. Update on primary immunodeficiency: defects of lymphocytes. Clin. Immunol. 109:109-118. [DOI] [PubMed] [Google Scholar]
- 9.Smith, J., T. Fernando, N. McGrath, and R. Ameratunga. 2004. Lamotrigine-induced common variable immune deficiency. Neurology 62:833-834. [DOI] [PubMed] [Google Scholar]
- 10.Spickett, G. P., M. M. Gompels, and P. W. Saunders. 1996. Hypogammaglobulinaemia with absent B lymphocytes and agranulocytosis after carbamazepine treatment. J. Neurol. Neurosurg. Psychiatry 60:459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van Ginneken, E. E. M., J. W. M. van der Meer, and P. M. Netten. 1999. A man with a mysterious hypogammaglobulinaemia and skin rash. Neth. J. Med. 54:158-162. [DOI] [PubMed] [Google Scholar]