Abstract
BACKGROUND:
Work relative value unit (wRVU) is a tool for assessing surgeons’ performance, compensation, and productivity. It appears that wRVU for cardiovascular procedures does not consider complexity and its value for lengthy operations is low. The aim of the study is to determine wRVU for cardiovascular procedures in Iran according to the proposed approach.
MATTERIALS AND METHODS:
This study was conducted as a mixed method in teaching hospitals in Tabriz in the period of September 2020 to December 2021. According to Hospital Information System and expert opinions, six procedures in cardiovascular surgery were included in the study. They were compared with 18 procedures in neurosurgery, orthopedics, and otorhinolaryngology in terms of the operation time and wRVU/min. Then, we calculated new wRVUs for the selected procedures based on surgeons’ opinions, time measurements, and anesthetists’ points of view by content analysis in qualitative and statistical analysis in quantitative parts.
RESULTS:
Among the six cardiac procedures, the wRVU for five was under-estimated. The wRVU/min value ranged from 0/28 to 1/15 in the studied procedures. Findings demonstrate no significant relationship between the length of operations and the wRVU announced by the Ministry of Health and Medical Education (P value >0/05). Compared to studied procedures in four specialties, thoracoabdominal aortic aneurysm repair has the longest surgery time at 417 minutes. According to anesthesiologists, cardiovascular; orthopedics; ear, nose, and tongue; and neurosurgery specialties obtained 4/2, 2/9, 2/8, and 4, respectively, in terms of surgery duration, complexity, risk, and physical effort.
CONCLUSION:
Despite policymakers’ attempts to bring justice to payments, it seems that there has been little progress in paying cardiovascular surgeons. Improper payment to cardiovascular surgeons will affect the future of the workforce in this specialty. Today, the need to reconsider the wRVUs in heart specialty is felt more than before.
Keywords: Cardiovascular surgical procedures, compensation, relative value scales, surgeons
Introduction
The concept of health service valuation goes back to the 1980s when Medicare sought a strategy to deal with an unexpected increase in health care expenses. At this time, a team directed by Hsiao at Harvard's School of Public Health developed a new approach called resource-based relative value unit (RBRVS) that assigned a value to each procedure based on the resources utilized.[1] The current procedural terminology (CPT) code was specified for any procedure.
The central component of the consumed resources for any services was the physician's work, known as the work relative value unit (wRVU). The metrics measures wRVU via time, technical skill, mental effort, and the stress load of surgeons. The amount of wRVU for each service was calculated according to the experts’ panels; additionally, operation time was obtained from databases.[2] Finally, a schedule of wRVUs for over 7000 procedures across all specialties was provided. Compensation for surgeons is calculated as the wRVU of the procedure performed multiplied by a conversion factor1. The US wRVU book has been translated and localized for use in Iran. The members of specialist surgical associations determined the wRVUs for surgical procedures.
Although wRVU was originally developed to measure surgeons’ work, it evolved into a tool for assessing surgeons’ performance, compensation, and eventually productivity. Although the primary goal of the RBRVS was to decrease health care expenditures, a second purpose was to narrow the income gap between general practitioners and specialists.[3] At first, the notion seemed reasonable and interesting, but Medicare's restricted budget raised general practitioners’ salaries and then lowered specialists’ compensation. This could affect the equity and fairness of surgeons’ compensation. Although it has been almost three decades since the RVU book was published, there is still debate on how surgery procedures should be evaluated. Importantly, the wRVU does not consider the procedure's complexity.[4,5] wRVUs for lengthy operations are low compared to shorter,[6] particularly cardiovascular surgeries which include more complex and lengthy procedures. Although studies have shown that a large part of a surgeon's time is spent providing pre- and post-operative care, especially in cardiac surgeries, this is not considered in RVU.[7] Considering that cardiovascular diseases are the leading cause of mortality, unfair assessment of the surgeons’ work drives medical students to choose residency programs in specialties with higher RVUs. It causes serious challenges for the health system and cardiovascular workforce in the future. Few studies have addressed wRVUs in cardiovascular procedures, and all use retrospective data.[8] Thus, this study aims to determine the wRVU of cardiovascular procedures in Iran based on timing in operation rooms and experts’ opinions.
Materials and Method
Study design and setting
The study was conducted in Tabriz teaching hospitals, and the proposed model by the authors was used to determine the cardiac wRVUs.
Finally, the research team compared the new values from wRVU to those listed in the US RVU schedule and the localized wRVU by the Ministry of Health and Medical Education (MoHME) in cardiovascular surgery. The study process is shown in Flowchart 1.
Flowchart 1.
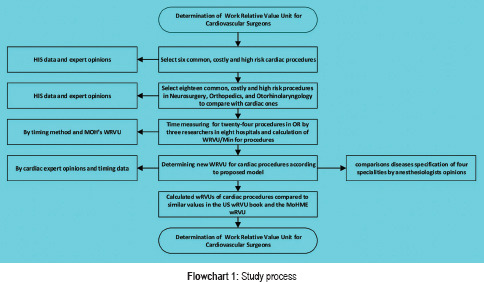
Study process
To develop a model for assessing surgeons’ wRVU, a comprehensive review and expert panels including surgeons and policymakers were organized. Based on the model, it was revealed that three items are essential in measuring a surgeon's work in the operation room (OR): disease specification, patient condition, and the surgeon's characteristics. The criteria and their importance are presented in parentheses in Figure 1. In this study, to measure wRVUs, the research team evaluated the disease specification in the selected cardiovascular procedures.[9]
Figure 1.
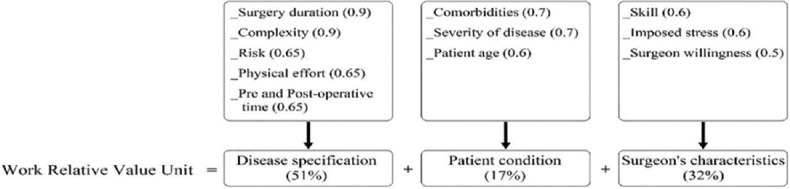
Proposed model of work relative value unit
Study participants and sampling
The views of cardiovascular surgeons were employed in the qualitative part of the study to gather data on the complexity, physical effort, stress, and pre- and post-operation time of selected procedures.
Twenty-six cardiovascular surgeons from all over the country participated in this study, and all were members of the Iranian Heart Association. An expert panel and semi-structured interviews were used to collect data. The sampling was purposive, and participants were chosen based on their interest, at least 5 years of professional experience as a surgeon, and knowledge of the RVU method.[10]
Additionally, to make comparisons across various specialties, the views of 30 anesthesiologists, who were not interested but were familiar with RVU, were employed.
The study was conducted at eight teaching hospitals in Tabriz from September 2020 to December 2021. Because of the small population, sampling was not performed, and all university teaching hospitals were included in the study.
The study procedures include six common, expensive, and high-risk cardiovascular surgery procedures. The received data from the Hospital Information System were used for identifying common and costly procedures in the period from September 2018 to September 2019. Also, high-risk operations were specified according to expert panels and surgeons’ opinions in the cardiovascular specialty. Similar procedures in other specialties (neurosurgery, orthopedics, and otorhinolaryngology) were selected in the same way.
Finally, in cardiovascular surgery, two procedures were chosen as the most common operations: coronary artery bypass graft surgery (CABG) with three and fewer grafts and CABG with four and more grafts with, respectively, 727 and 124 times a year.
Two procedures, aortic valve replacement with cardiopulmonary bypass with prosthetic valve (AVR) and mitral valve replacement with cardiopulmonary bypass (MVR), were selected as two expensive procedures.
On expert opinions, the thoracoabdominal aortic aneurysm repair with graft and with or without cardiopulmonary bypass (TAA repair) and ascending aorta graft with cardiopulmonary bypass and with aortic root replacement using valved conduit and coronary reconstruction (Bentall, David and Yacoub method) (AAG) are two high-risk procedures in cardiovascular surgery.
Data collection tool and technique
The data gathering was divided into two phases: quantitative and qualitative. The complexity, physical effort, risk, and length of pre- and post-care were assessed based on experts’ opinions. The timing technique was applied to measure the length of procedures in the operation room in hospitals.
The pilot measurements revealed that timing each procedure with four repeats by three researchers is acceptable.[11] Timings for 24 procedures were measured with four repeats by three researchers in eight hospitals. The researchers took the time of surgery from incision to closure (skin to skin) and did not include anesthetization. The intra-service period for a procedure was determined by taking the median of the time reported by the researchers. The Intra Class Coefficient was used to assess the interior agreement. The ICC value was 0.94 (0.90–0.97).
Microsoft Excel 2013 was used for data entry and creating the visuals. SPSS version 26 was applied for reliability and statistical analysis, whereas Pass. 15.05 software determined the number of trials in the measurement. Content analysis approach was used for qualitative analysis.
Ethical consideration
The research with ethics code IR. TBZMED. REC.1397.960 was a part of a dissertation. Participation was entirely voluntary, and informed consent was obtained. The surgery duration was recorded in the OR without obtaining any personal information about the patients. In addition, confidentiality was ensured throughout the study.
Results
Demographic characteristics of the participants: The average of participant age was M = 59 (SD = 8.35), and the work experience was M = 21 (SD = 7.61). All the surgeons worked at heart teaching hospitals around the country and did not have a private office. Furthermore, none of them had administrative positions in any organization or MoHME. In addition, males made up 92% of the cardiac surgeons who took part in the research.
Quantitative results
wRVU/Minute
Eighteen orthopedic; ear, nose, and tongue (ENT); and neurosurgery procedures were timed in the same way as the cardiovascular procedures. The results indicate that of the 24 selected operations, the longest operation time is for the thoracoabdominal aortic aneurysm repair and the shortest is related to tracheostomy in ENT.
To compare wRVU across operations, the wRVU/min metric was applied, which highlighted the value of the surgeon's work in each specialty for any minute spent in the OR. The maximum amount of wRVU for a minute was associated with orthopedic scoliosis deformity, whereas the lowest amount of wRVU was related to primary rhinoplasty.
Following the statistical analysis, the results demonstrate that there is no significant relationship between the length of operations and the wRVU announced by MoHME (P value >0.05), and the Pearson correlation coefficient was obtained at 0.10.
Also, wRVU/min values ranged from 0.28 to 1.15 in the studied procedures. As a result, surgeons in different specializations are compensated differently for each minute spent in the OR. The operation time, wRVU, and the wRVU/min for all the procedures are presented in Table 1.
Table 1.
wRVU and operation time for procedures of orthopedics, cardiovascular surgery, otorhinolaryngology, and neurosurgery
| Procedures | Localized wRVU | Median Operative Time (minute) | wRVU/min |
|---|---|---|---|
| Orthopedic Surgery | |||
| – Closed treatment of distal radial fracture or epiphyseal separation | 28 | 41 | 0/68 |
| – Repair, extensor tendon, finger, primary or secondary; without or with free graft, each tendon | 12/8 | 33 | 0/39 |
| – Arthrodesis, posterior, for scoliosis deformity, up to 70 degree | 290 | 252 | 1/15 |
| – Arthrodesis, posterior, for scoliosis deformity, more than 70 degree | 340 | 313 | 1/09 |
| – Total knee arthroplasty primary or with revision | 80 | 128 | 0/63 |
| – Open treatment of tibial fracture, proximal (plateau); unicondylar, bicondylar, with or without internal fixation | 53 | 146 | 0/36 |
| Cardiovascular Surgery | |||
| – CABG with three or fewer grafts | 180 | 238 | 0/76 |
| – CABG with four or more grafts | 200 | 271 | 0/74 |
| – Aortic valve replacement with cardiopulmonary bypass with a prosthetic valve | 115 | 241 | 0/48 |
| – Mitral valve replacement, with cardiopulmonary bypass | 110 | 194 | 0/56 |
| – Repair of the thoracoabdominal aortic aneurysm with graft, with or without cardiopulmonary bypass | 260 | 417 | 0/62 |
| – Ascending aorta graft, with cardiopulmonary bypass, with aortic root replacement as Bentall, David and Yacoub procedure | 220 | 396 | 0/56 |
| Otorhinolaryngology Surgery | |||
| – Tracheostomy; planned or emergency procedure | 16 | 28 | 0/57 |
| – Rhinoplasty, primary | 40/3 | 145 | 0/28 |
| – Excision of parotid tumor or parotid gland; total, with dissection and preservation of facial nerve | 100 | 158 | 0/63 |
| – Sinusotomy, unilateral or bilateral, three or more paranasal sinuses (frontal, maxillary, ethmoid, sphenoid) | 80 | 146 | 0/55 |
| – Laryngectomy; total, with radical neck dissection | 130 | 312 | 0/42 |
| Pharyngolaryngectomy, with radical neck dissection; without reconstruction | 150 | 345 | 0/43 |
| Neuro Surgery | |||
| – Decompression procedure, percutaneous, of nucleus pulposus of intervertebral disc | 35 | 97 | 0/36 |
| – Lumbar discectomy with or without laminectomy 1 interspace | 75 | 72 | 1/04 |
| – Craniectomy, suboccipital with cervical laminectomy for decompression of medulla and spinal cord, with or without dural graft (e.g., Arnold–Chiari malformation) | 106 | 132 | 0/80 |
| – Vertebral corpectomy (vertebral body resection), partial or complete, combined thoracolumbar approach with decompression of spinal cord, lower thoracic or lumbar; single segment | 123 | 181 | 0/68 |
| – Surgery of complex intracranial aneurysm, intracranial approach; carotid circulation | 158 | 236 | 0/67 |
| – Craniectomy for excision of brain tumor, infratentorial or posterior fossa; except meningioma, cerebellopontine angle tumor, or midline tumor at base of skull (61518) | 133 | 184 | 0/72 |
Qualitative results
Complexity, risk, and physical effort in cardiovascular procedures
Except for time, the other metrics used to measure the surgeons’ work in the proposed model are subjective parameters. Therefore, to measure these parameters, the opinions of cardiovascular surgeons were employed. We asked the participating surgeons to rank six cardiovascular surgeries’ complexity, risk, and physical effort. The scoring range was 1 to 5.
The term “complexity” refers to the difficulty and high mental attention required to complete an operation. Physical effort refers to the surgeon's difficult position during surgery to access the section they want to perform. Risk refers to the mortality rate in a surgery.
All the surgeon's actions were documented to establish the duration of pre- and post-operation time. Before the operation, the work included participating in counseling sessions or committees held for a patient; examining the electrocardiogram, computed tomographies, magnetic resonance imaging, and echocardiography; and laboratory tests.
Surgeons give post-operative care in the intensive care unit immediately after the operation, complete the patient record, and visit patients daily while staying in the hospital.
Surgeons were asked about the time assigned for each service. The median was estimated based on the pre-and post-operative times declared by each surgeon. The variation in pre- and post-operation times among the procedures was associated with the patient's length of stay in the hospital. The score of the procedures’ specifications according to the surgeon's point of view and time measurements is summarized in Table 2.
Table 2.
Procedure’s specifications based on expert opinion and timing technique
| Procedure | Complexity (1-5) | Physical effort (1-5) | Risk (1-5) | Operation time (minute) | Pre- and post-operation (minute) |
|---|---|---|---|---|---|
| CABG with three or fewer grafts | 3 | 4 | 3 | 238 | 90 |
| CABG with four or more grafts | 3/5 | 4 | 3 | 271 | 100 |
| AVR1 | 4 | 4 | 4 | 241 | 90 |
| MVR2 | 3/5 | 3/5 | 3 | 194 | 90 |
| TAA repair3 | 5 | 5 | 5 | 417 | 430 |
| AAG4 | 5 | 5 | 5 | 396 | 360 |
1Aortic valve replacement with cardiopulmonary bypass with a prosthetic valve, 2Mitral valve replacement, with cardiopulmonary bypass, 3Repair of the thoracoabdominal aortic aneurysm with graft, with or without cardiopulmonary bypass, 4Ascending aorta graft, with cardiopulmonary bypass, with aortic root replacement as Bentall, David and Yacoub procedure
Because the unit of time in this research differed from the unit of other parameters, we defined the time unit in the range of 1 to 5 to determine the wRVU for the chosen procedures. As a result, according to experts, every 1 minute was considered 0.01 units.
As the wRVU is a relative concept and is based on comparisons between various procedures and even different specialties, to establish wRVUs in cardiovascular operations, we compare the selected procedures with ENT, orthopedic, and neurosurgery specialties.
Therefore, anesthesiologists were asked to compare the six cardiovascular procedures with 18 procedures in the three mentioned specialties regarding time, complexity, physical effort, and risk. Finally, the mean score achieved by anesthesiologists was considered in the form of a coefficient in calculating the wRVUs of cardiovascular operations.
According to anesthesiologists, cardiovascular, orthopedics, ENT, and neurosurgery specialties obtained 4/2, 2/9, 2/8, and 4, respectively, in terms of surgery duration, complexity, risk, and physical effort. The scale was from 1 to 5. The participating anesthesiologists were chosen from nine teaching hospitals. They had the experience of attending the surgery of all the procedures in all specialties and were not interested in determining the wRVUs of surgical groups.
The greatest calculated wRVU is related to the TAA repair, whereas the least amount of wRVU is related to CABG three graft and fewer in cardiovascular procedures. Table 3 summarizes the wRVUs for the six procedures based on data received from cardiovascular surgeons, anesthesiologists, and time measurements labeled as new work RVU.
Table 3.
Work relative value unit in cardiovascular procedures
| Procedure | National code | New work RVU In range of (1-73/7) | US work RVU In range of (1-69/03) | localized work RVU In range of (1-340) |
|---|---|---|---|---|
| CABG with three or fewer grafts | 3012151 | 39/17 | 34/98-38/45-43/98 | 180 |
| CABG with four or more grafts | 3012202 | 47/54 | 45/37-48/08-49/76 | 200 |
| AVR1 | 3010653 | 48/49 | 41/32 | 115 |
| MVR2 | 3011204 | 40/80 | 50/93 | 110 |
| TAA repair3 | 3014405 | 73/70 | 69/03 | 260 |
| AAG4 | 3014426 | 71/00 | 58/79-60/08 | 220 |
1CABG with three or fewer grafts, 2CABG with four or more grafts, 3AVR, 4MVR, 5TAA repair, 6AAG. 1Aortic valve replacement with cardiopulmonary bypass with a prosthetic valve, 2Mitral valve replacement, with cardiopulmonary bypass, 3Repair of the thoracoabdominal aortic aneurysm with graft, with or without cardiopulmonary bypass, 4Ascending aorta graft, with cardiopulmonary bypass, with aortic root replacement as Bentall, David and Yacoub procedure
The study's wRVU results are compared to similar values in the US wRVU book and the wRVU declared by MoHME in Figure 2. Findings show that wRVUs were under-estimated for five cardiovascular operations. The considerable disparity between the calculated wRVUs and the existing wRVUs provided by MoHME is because of two valve replacements: aortic and mitral. Figure 2.
Figure 2.
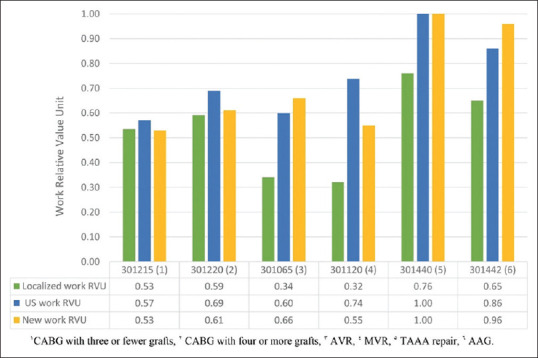
Work relative value unit comparative chart
Discussion
The study findings indicate that wRVUs for long procedures are estimated lower. It may affect surgeons’ willingness to perform simpler and shorter procedures, which might disappoint surgeons who perform lengthily.
The research undertaken by Ramirez et al.[12] discovered that cardiac procedures had the greatest complexity according to the National Surgical Quality Improvement Program (NSQIP), and although the quantity of physician effort is closely connected to patient complexity, this is not taken into account in wRVU.
The operation time for AVR and MVR was 241 and 194 minutes in the current study, respectively; however, Childers et al.[13] reported that they lasted 186 and 233 minutes, according to the NSQIP database.
Because of the operation time difference, the wRVU of AVR is more than that of the mitral. In comparison, the value of the MVR is higher than the AVR in the US RVU book. It should be highlighted that both these procedures were conducted in an open method in Iran. The AVR operation has the lowest wRVU/min, which means that the assigned value to each minute of the surgeon's work was the lowest.
According to the surgeons’ opinions and time measurements, the CABG with three grafts and fewer had the lowest amount of wRVU among the investigated operations in cardiovascular. The data in the US RVU book are identical to ours; however, the results in the MoHME are different, with mitral valve replacement having the lowest wRVU.
Erratic changes that deviate from the scientific approach based on unrealistic and speculative timing have resulted in inaccurate estimations of wRVUs and disrupted the structure of relative values in the heart specialty. Through national codes rather than CPT codes in cardiovascular procedures, sometimes, two or three codes have merged, which vary in the amount of work and time. CABG is one of the procedures resulting from merging three codes. The difference between CABG one graft and CABG three crafts is nine units in the US wRVU book; after applying the conversion factor and at the time of payment to surgeons, it would be about $325.
According to the current study, each extra graft in the CABG surgery lasted approximately 20 minutes. However, the distinction between surgeons’ work and the spent time is neglected. Therefore, it seems rational for a surgeon to prefer simpler and shorter procedures in the same condition.
It also occurs with the CABG with four grafts and more. Considering that time is the only objective parameter in estimating the wRVUs, accurate time measuring might be the first step toward establishing fair wRVUs. Evidence reveals that operation times utilized to determine wRVUs for various surgical procedures are not actual and are based on estimation.[14,15,16,17]
Comparison of cardiovascular procedures with other specialties demonstrates that TAA repair surgery is valued less than scoliosis in orthopedics. Although the highest wRVU among over 7000 operations in the US RVU book is associated with TAA repair surgery, it seems that the Iranian Heart Association has not properly assessed it. Lengthy operation times and complications such as stroke, access site complications, paraplegia, endoleaks, device migration, persistent aneurysm sac enlargement, and graft collapse need skilled surgeons in operation.[18,19,20,21,22,23,24,25]
Patients who have underwent TAA repair surgery are more likely to have co-morbidities, including pre-operative acute renal failure and peripheral vascular disease (PVD).[26]
The mortality rate for elective and urgent TAA repair cases was reported to be 10% and 35%, respectively, in earlier studies conducted in Germany.[27,28]
The long hospital stay after a surgery means more extended postoperative care for the patients. Accordingly, TAA repair is risky, complex, and major surgery for patients and surgeons, which should be financially compensated. Applying personal changes under the heading of localization and relying on surgeons who had administrative positions and were not involved in clinical activities for years to determine a surgeon's work have resulted in mis-evaluation in cardiovascular wRVUs.
Few studies have addressed the wRVUs of the heart specialty, which may be attributed to the American Heart Association's effort to update cardiovascular WRVUs. However, the updates of WRVUs were not applied in Iran. It has resulted in a gap between the MoHME wRVUs and the US WRVU amounts in cardiovascular surgeries.
The wRVU was determined based on the disease's characteristics, including the duration of surgery, complexity, risk, physical effort, and the surgeon's pre- and post-operation times. It is suggested that the wRVUs would be raised up to 49% according to the patient condition and the surgeon's characteristics.
Improper payment to cardiovascular surgeons would have several consequences, including an increase in the average age of cardiovascular surgeons, informal payment and surgeon-induced demands, a reduction in surgeon satisfaction and burnout, and finally an increase in the community's burden of cardiovascular disease.[29,30]
Given that cardiovascular diseases (CVDs) were the leading cause of death in Iran, accounting for 46% of all deaths and 20–23% of disease burden, in the US, the disease burden of CVD is similar. Policymakers need to re-consider payment regulations to attract and retain cardiovascular surgeons and encouraging medical students for this speciality.[8,31] Although we just measured disease specifications for procedures in this study, it is suggested that future studies address patients’ conditions and the characteristics of the surgeon of cardiac procedures to establish equity in payments to provide services to patients with severe conditions. It is also advised to determine the wRVU of all cardiac procedures with the proposed model in this study.
Limitations and Recommendation
Our study has such limitations. First, wRVU in Iran is specified based on national codes, making it difficult to compare the procedures with the US RVU schedules. In some procedures, there are minor differences in the description of the procedures in national codes and CPTs. Second, the study's hospitals were teaching hospitals, which may not represent all hospitals well because of their educational nature and referral cases. Third, this study did not address the differences between patients’ conditions and surgeons’ skills. Fourth, because most of the metrics of wRVU were measured subjectively and based on the experts’ opinions, obtained wRVU values may be different in other contexts or countries. Despite limitations, the present study is the first to investigate the wRVU of cardiac procedures by timing technique and anesthesiologist opinions as non-beneficial experts in the surgery.
The study found that cardiac wRVUs are not calculated based on operation duration and pre-post operation time; therefore, it is recommended that policymakers and health economists consider these measurable parameters in wRVU calculation and also apply anesthesiologists’ opinions as non-beneficiary to modify wRVU cross-specializations.
Conclusions
According to the policymakers’ role in shaping human resource regulations in the health system, adopting appropriate policies to properly evaluate cardiovascular surgeons’ performance is essential to promoting public health, service quality, and patient accessibility. Paying attention to the modification and updating of the cardiovascular's wRVU structure by health policymakers can affect the planning for human resources in the future in this sector. Also, the fair and rational assessment of the cardiovascular surgeons’ performance by reducing illegal patient receipts leads to increasing justice and cost reduction in the health system.
Ethics approval
The manuscript is a part of PhD thesis by the Ethics Committee of Tabriz University of Medical Sciences and approved by Reg. No.: IR.TBZNED.REC.1396.960.
Consent to participate
Participation in this study was optional and the participants could withdraw from the study at any time. Also, the participants’ information was kept confidential.
Consent for publication
We give consent to the publication of the study and the supplemental material of us.
Financial support and sponsorship
It is supported by the Research Deputy of Tabriz University of Medical Science.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We would like to thank the professionals that took part in this research with the ethics code IR. TBZMED. REC.1397.960 and Research Deputy of the Tabriz University of Medical Science for providing financial support.
Footnotes
Conversation factor was 34.89$ in the US for 2021
References
- 1.Hayon S, Deal A, Tan HJ, Namboodri B, Gan Z, Wood C, et al. Is the relative value of surgeon effort equal across surgical specialties? Surgery. 2020;168:365–70. doi: 10.1016/j.surg.2020.04.018. [DOI] [PubMed] [Google Scholar]
- 2.Meyr AJ, Mateen S, Skolnik J, Van JC. Evaluation of the relationship between aspects of medical complexity and work relative value units (wRVUs) for foot and ankle surgical procedures. J Foot Ankle Surg. 2021;60:448–54. doi: 10.1053/j.jfas.2020.06.022. [DOI] [PubMed] [Google Scholar]
- 3.Childers CP, Gibbons MAM. Work relative value units: Winners and losers during the past 20 years. J Am Coll Surg. 2020;231:S154. [Google Scholar]
- 4.Doval AF, Nguyen-Lee JJ, Beal LL, Zheng F, Echo A. Does complexity relate to compensation? A comparison of relative value units in initial versus recurrent inguinal hernia repair. Hernia. 2020;24:245–50. doi: 10.1007/s10029-019-02020-9. [DOI] [PubMed] [Google Scholar]
- 5.Ramirez JL, Gasper WJ, Seib CD, Finlayson E, Conte MS, Sosa JA, et al. Patient complexity by surgical specialty does not correlate with work relative value units. Surgery. 2020;168:371–8. doi: 10.1016/j.surg.2020.03.002. [DOI] [PubMed] [Google Scholar]
- 6.Orr RD, Sodhi N, Dalton SE, Khlopas A, Sultan AA, Chughtai M, et al. What provides a better value for your time? The use of relative value units to compare posterior segmental instrumentation of vertebral segments. Spine J. 2018;18:1727–32. doi: 10.1016/j.spinee.2018.01.026. [DOI] [PubMed] [Google Scholar]
- 7.Childers CP, Maggard-Gibbons M. Assessment of the contribution of the work relative value unit scale to differences in physician compensation across medical and surgical specialties. JAMA Surg. 2020;155:493–501. doi: 10.1001/jamasurg.2020.0422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sarrafzadegan N, Mohammmadifard N. Cardiovascular disease in Iran in the last 40 years: Prevalence, mortality, morbidity, challenges and strategies for cardiovascular prevention. Arch Iran Med. 2019;22:204–10. [PubMed] [Google Scholar]
- 9.Forootan S, Hajebrahimi S, Janati A, Najafi B, Asghari-Jafarabadi M. Development of a local model for measuring the work of surgeons. Turk J Surg. 2021;37:371–8. doi: 10.47717/turkjsurg.2021.5473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kirchherr J, Charles K. Enhancing the sample diversity of snowball samples: Recommendations from a research project on anti-dam movements in Southeast Asia. PLoS One. 2018;13:e0201710. doi: 10.1371/journal.pone.0201710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Borg DN, Bach AJE, O’Brien JL, Sainani KL. Calculating sample size for reliability studies. PM and R. 2022;14:1018–25. doi: 10.1002/pmrj.12850. [DOI] [PubMed] [Google Scholar]
- 12.Ramirez JL, Lopez J, Sanders K, Schneider PA, Gasper WJ, Conte MS, et al. Understanding value and patient complexity among common inpatient vascular surgery procedures. J Vasc Surg. 2021;74:1343–53. doi: 10.1016/j.jvs.2021.03.036. [DOI] [PubMed] [Google Scholar]
- 13.Childers CP, Tang AB, Maggard-Gibbons M. Association of implicit intensity values incorporated into work RVUs with objective measures. Am J Surg. 2020;219:976–82. doi: 10.1016/j.amjsurg.2019.09.022. [DOI] [PubMed] [Google Scholar]
- 14.Uppal S, Rice LW, Spencer RJ. Discrepancies created by surgeon self-reported operative time and the effects on procedural relative value units and reimbursement. Obstet Gynecol. 2021;137:182–8. doi: 10.1097/AOG.0000000000004467. [DOI] [PubMed] [Google Scholar]
- 15.Chan DC, Huynh J, Studdert DM. Accuracy of valuations of surgical procedures in the medicare fee schedule. N Engl J Med. 2019;380:1546–54. doi: 10.1056/NEJMsa1807379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith KA, Oakley G, Alt JA, Orlandi RR. An analysis of RUC methodology for determining the RVU valuation of sinus surgery. Int Forum Allergy Rhinol. 2019;9:479–85. doi: 10.1002/alr.22283. [DOI] [PubMed] [Google Scholar]
- 17.Chakiryan NH, Jiang DD, Gillis KA, Chen Y, Acevedo AM, Sajadi KP. RUC operative time estimates are inaccurate, resulting in decreased work RVU assignments for longer urologic procedures. Urology. 2020;142:94–8. doi: 10.1016/j.urology.2020.05.004. [DOI] [PubMed] [Google Scholar]
- 18.Chen SW, Lee KB, Napolitano MA, Murillo-Berlioz AE, Sattah AP, Sarin S, et al. Complications and management of the thoracic endovascular aortic repair. Aorta (Stamford) 2020;8:49–58. doi: 10.1055/s-0040-1714089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jordan WD, Desai N, Letter AJ, Matsumura JS. Long-term outcomes of the conformable TAG thoracic endoprosthesis in a prospective multicenter trial. J Vasc Surg. 2021;74:1491–8. doi: 10.1016/j.jvs.2021.04.063. [DOI] [PubMed] [Google Scholar]
- 20.Beropoulis E, Fazzini S, Austermann M, Torsello GB, Damerau S, Torsello GF. Long-term results of thoracic endovascular aortic repair using a low-profile stent-graft. J Endovasc Ther. 2020;28:56–62. doi: 10.1177/1526602820952416. [DOI] [PubMed] [Google Scholar]
- 21.Swerdlow NJ, Wu WW, Schermerhorn ML. Open and endovascular management of aortic aneurysms. Circ Res. 2019;124:647–61. doi: 10.1161/CIRCRESAHA.118.313186. [DOI] [PubMed] [Google Scholar]
- 22.Sattah AP, Secrist MH, Sarin S. Complications and perioperative management of patients undergoing thoracic endovascular aortic repair. J Intensive Care Med. 2018;33:394–406. doi: 10.1177/0885066617730571. [DOI] [PubMed] [Google Scholar]
- 23.Terzi F, Rocchi G, Fattori R. Current challenges in endovascular therapy for thoracic aneurysms. Expert Rev Cardiovasc Ther. 2016;14:599–607. doi: 10.1586/14779072.2016.1141677. [DOI] [PubMed] [Google Scholar]
- 24.Jeon YH, Bae CH. The risk factors and outcomes of acute kidney injury after thoracic endovascular aortic repair. Korean J Thorac Cardiovasc Surg. 2016;49:15–21. doi: 10.5090/kjtcs.2016.49.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Teixeira PG, Woo K, Beck AW, Scali ST, Weaver FA. Association of left subclavian artery coverage without revascularization and spinal cord ischemia in patients undergoing thoracic endovascular aortic repair: A Vascular Quality Initiative® analysis. Vascular. 2017;25:587–97. doi: 10.1177/1708538116681910. [DOI] [PubMed] [Google Scholar]
- 26.Isaac T, Gilani S, Kleiman NS. When prevention is truly better than cure: Contrast-associated acute kidney injury in percutaneous coronary intervention. Methodist Debakey Cardiovasc J. 2022;18:73–85. doi: 10.14797/mdcvj.1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mkalaluh S, Szczechowicz M, Dib B, Weymann A, Szabo G, Karck M. Open surgical thoracoabdominal aortic aneurysm repair: The Heidelberg experience. J Thorac Cardiovasc Surg. 2018;156:2067–73. doi: 10.1016/j.jtcvs.2018.05.081. [DOI] [PubMed] [Google Scholar]
- 28.Gombert A, Frankort J, Keszei A, Müller O, Benning J, Kotelis D, et al. Outcome of elective and emergency open thoraco-abdominal aortic aneurysm repair in 255 cases: A retrospective single centre study. Eur J Vasc Endovasc Surg. 2022;63:578–86. doi: 10.1016/j.ejvs.2022.02.003. [DOI] [PubMed] [Google Scholar]
- 29.Rosner MH, Falk RJ. Understanding work: Moving beyond the RVU. Clin J Am Soc Nephrol. 2020;15:1053–5. doi: 10.2215/CJN.12661019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lewis SJ, Mehta LS, Douglas PS, Gulati M, Limacher MC, Poppas A, et al. Changes in the professional lives of cardiologists over 2 decades. J Am Coll Cardiol. 2017;69:452–62. doi: 10.1016/j.jacc.2016.11.027. [DOI] [PubMed] [Google Scholar]
- 31.Abdalla M, Kovach N, Liu C, Damp JB, Jahangir E, Hilliard A, et al. The importance of global health experiences in the development of new cardiologists. J Am Coll Cardiol. 2016;67:2789–97. doi: 10.1016/j.jacc.2015.10.089. [DOI] [PMC free article] [PubMed] [Google Scholar]


