Abstract
INTRODUCTION
Preeclampsia affects 2%–8% of all pregnancies worldwide and can have a multiorgan impact, including the liver, kidneys, brain, and vascular system.1 Preeclampsia and its spectrum of hypertensive diseases of pregnancy contribute to a significant burden of maternal morbidity and mortality globally.2 Concomitantly, for the developing fetus, preeclampsia can lead to growth restriction, modulate fetal oxygenation/nutrient transfer, and precipitate preterm birth and its associated morbidities.1 In the pregnant person, the sequelae of systemic inflammation, hepatic necrosis, and respiratory distress syndrome are responsible for preeclampsia-related mortality.3 Currently, the only treatment option is delivery, which necessitates a balance between continued fetal development and maternal risk of disease progression. Herein, we aim to elucidate the involvement of the liver and the mechanism of preeclampsia-induced liver injury.
DEFINITION OF PREECLAMPSIA
The diagnosis of preeclampsia is made with new-onset hypertension and proteinuria, with hypertension defined as a systolic blood pressure (BP) > 140 and or a diastolic BP >90 mm Hg, and proteinuria with a urine protein to creatinine ratio of 0.3 or greater, or 300 mg or greater in a 24-hour urine specimen.4 New-onset hypertension is defined as elevated BP on 2 occasions at least 4 hours apart after 20 weeks of gestation in a patient with previously normal BP.
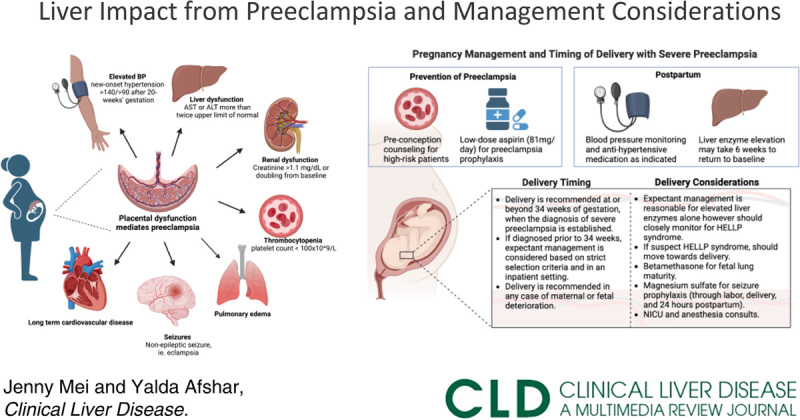
Preeclampsia is further defined as with or without severe features.4 Severe features can be defined by BP of > 160/ > 110 that are sustained over 15 minutes or occurring on 2 occasions at least 4 hours apart. Severe preeclampsia can occur with or without proteinuria. In the absence of proteinuria, severe preeclampsia can also be defined by the new onset of any of the following (Figure 1):
Liver injury, reflected by elevated liver enzymes to twice the upper limit of normal, can progress to impaired liver function;
Thrombocytopenia with platelet count <100 × 109/L;
Renal insufficiency with serum creatinine concentrations > 1.1 mg/dL or a doubling of the baseline serum creatinine level in the absence of other renal disease;
Pulmonary edema;
New-onset headache unresponsive to medication or visual symptoms.
FIGURE 1.
Diagnosing preeclampsia. This illustration depicts how preeclampsia is diagnosed, as well as various sequelae that can occur in different organs affected by preeclampsia. Abbreviations: ALT, alanine transaminase; AST, aspartate aminotransferase; BP; blood pressure.
Early-onset preeclampsia is diagnosed before 34 weeks of pregnancy, while late-onset is diagnosed at 34 weeks or later.5 Early-onset is less common and accounts for 5%–20% of preeclampsia; however it bodes increased maternal and fetal risk and is also associated with a higher incidence of HELLP (hemolysis, elevated liver enzymes, and low platelets) syndrome and eclampsia. There is a body of literature that believes the pathophysiology of early-onset and late-onset preeclampsia are distinct; however, that is beyond the scope of this review.
HELLP syndrome is a pregnancy-associated liver disease characterized by the pathology listed above.4 These symptoms may or may not present with hypertension or proteinuria, but HELLP is considered a severe complication of preeclampsia. HELLP syndrome is also a predisposing factor to the development of eclampsia, new-onset grand mal seizure activity, and/or coma in the setting of preeclampsia.
HEPATIC CONSEQUENCES FROM PREECLAMPSIA
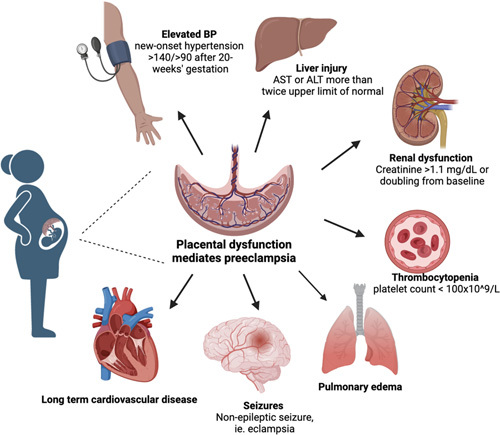
Despite the prevalence and clinical burden of preeclampsia, the pathophysiology remains elusive. Currently, there is a general consensus that preeclampsia is a consequence or result of vascular placental invasion (Figure 2).6 The first stage relates to abnormal placentation, deficient trophoblast invasion, and insufficient remodeling of uterine spiral arteries, which lead to decreased placental perfusion. There is then a release of antiangiogenic factors, which contributes to vascular remodeling in the first half of pregnancy. Subsequently, the second stage entails alterations in maternal vascular functions, which lead to vascular narrowing, edema, and platelet destruction, predisposing to multiorgan damage.
FIGURE 2.
Preeclampsia and the liver. This illustration depicts the impact of preeclampsia on the liver and the subsequent effects of the liver changes on the pregnancy.
Elevated liver enzymes in preeclampsia are hypothesized to occur due to endothelial cell disruption, leading to decreased prostacyclin levels and increased thromboxane levels. This results in vasoconstriction of hepatic blood vessels, causing hepatic hypoxia and leading to necrosis, hepatocyte degeneration, and the resulting elevated liver enzymes.3
Aspartate aminotransferase and alanine transaminase levels with severe preeclampsia and HELLP syndrome can reach the hundreds (usually up to 400 U/L); however, they rarely reach levels in the thousands. Aspartate aminotransferase is more likely to be increased relative to alanine transaminase with preeclampsia.4
Elevations in lactate dehydrogenase due to hepatic damage and hemolysis may also occur, especially in HELLP syndrome. Bilirubin may be increased in the setting of hemolysis. In cases of severe hepatic damage, coagulopathy may occur with reduced production of coagulation factors.
Liver histology in preeclampsia patients shows deposits of microvesicular fat, ischemia, and periportal hemorrhage with fibrinogen deposition.7 These findings signal the result of endothelial cell injury and exposure to subendothelial collagen. Fibroscan studies also show increased fibrosis in preeclamptic patients compared with normotensive controls, and alterations in lipid metabolism leading to increased steatosis seen on biopsy.8
Subcapsular hematoma
HELLP syndrome is associated with a rare but life-threatening complication called a subcapsular hematoma, which can result in hepatic rupture in the setting of disseminated intravascular coagulopathy. This complicates up to 1.6% of HELLP syndrome cases, often involving the right lobe of the liver and preceded by parenchymal hemorrhage.9 Maternal mortality ranges from 17% to 59% when this complication occurs. Autopsy findings in these settings demonstrate subcapsular or intrahepatic hemorrhage and hepatocellular necrosis.
Portable ultrasound is a reasonable initial screening modality to establish a diagnosis quickly; CT imaging is more definitive. Management includes aggressive supportive care, blood transfusions, and serial imaging. Surgical intervention is reserved for those with increasing hematoma size, hemodynamic instability, or rupture, and it mostly entails packing to control bleeding.
Very rarely, liver transplantation has been necessitated in cases of HELLP syndrome. Studies evaluating these populations show mixed data on graft survival, and further studies are needed.
PREGNANCY MANAGEMENT AND TIMING OF DELIVERY
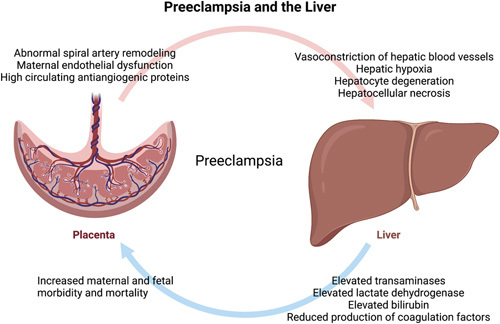
The below considerations on prevention, timing of delivery, and postpartum considerations for preeclampsia are depicted in Figure 3.
FIGURE 3.
Prevention, pregnancy management, and postpartum considerations for preeclampsia. This figure depicts management considerations for the prevention of preeclampsia, the timing of delivery, and postpartum care for patients with severe preeclampsia.
Aspirin for preeclampsia prophylaxis
The only intervention thus far shown to decrease the risk for preeclampsia has been low-dose aspirin. The target population is patients with any high-risk factors for preeclampsia (prior affected pregnancy, multifetal gestation, renal disease, autoimmune disease, pre-gestational diabetes mellitus, chronic hypertension) or more than 1 moderate-risk factor (nulliparous, maternal age ≥ 35, body mass index ≥ 30, family history of preeclampsia, and sociodemographic factors). They should initiate low-dose (81 mg/day) aspirin between 12 and 28 weeks of gestation (ideally before 16 wk) and continue until delivery.10
Timing of delivery
Patients with gestational hypertension (new-onset hypertension without proteinuria) or preeclampsia without severe features (new-onset hypertension with proteinuria) can be reasonably expectantly managed until 37 weeks of gestation.4 However, for patients who meet criteria for preeclampsia with severe features as defined above and in Figure 1, including elevated liver enzymes to twice the upper limit of normal concentration, delivery is recommended at or beyond 34 weeks of gestation when the diagnosis is established.4
When preeclampsia with severe features is diagnosed before 34 weeks of gestation, expectant management is considered based on strict selection criteria and in an inpatient setting with appropriate resources for maternal and neonatal care. In general, delivery is recommended in any case of maternal or fetal deterioration. While worsening elevated liver enzymes alone do not preclude expectant management before 34 weeks, patients should be closely monitored for the development of HELLP syndrome, which does preclude expectant management and in which case delivery is recommended at the time of diagnosis.4
Intravenous magnesium sulfate is used intrapartum for seizure prophylaxis in patients with severe preeclampsia. It is continued throughout labor, delivery, and the immediate postpartum period.11
Postpartum Recovery
Magnesium sulfate should be continued for 24 hours in the immediate postpartum period for continued seizure prophylaxis. Patients with preeclampsia with severe features are also at higher risk for requiring anti-hypertensive medications for BP management. Elevated liver enzymes should improve soon after delivery, though it may take weeks to return to baseline. The disease process of preeclampsia can take up to 6 weeks to resolve, with many studies now showing a substantial increased risk for cardiovascular disease in these patients in subsequent years.
OTHER HEPATIC PATHOLOGY IN PREGNANCY
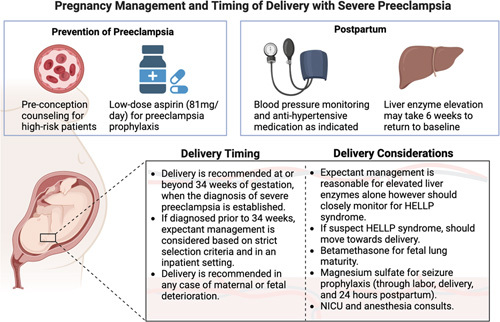
It is important to keep in mind that other hepatic disease processes can mimic preeclampsia as management can vary significantly; the so-called imitators of preeclampsia are specifically discussed below (Figure 4).
FIGURE 4.
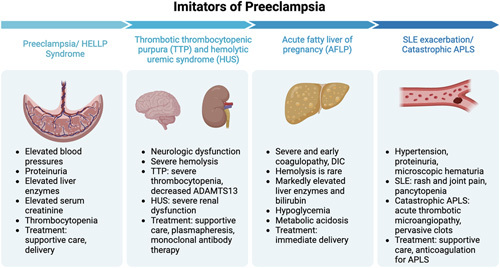
Differentiating preeclampsia/HELLP syndrome from imitators of preeclampsia. There are various imitators of preeclampsia that can impact the liver and are important to distinguish from preeclampsia as their treatment modalities vary greatly. These other disease processes include thrombotic thrombocytopenia purpura and hemolytic uremic syndrome, acute fatty liver of pregnancy, systemic lupus erythematous exacerbation, and catastrophic antiphospholipid antibody syndrome. Abbreviation: HELLP, hemolysis, elevated liver enzymes, and low platelets.
Thrombotic thrombocytopenia purpura and hemolytic uremic syndrome are usually notable for severe hemolysis, marked thrombocytopenia, and only mildly elevated liver enzymes. Patients can present with notable neurological dysfunction. ADAMTS13 activity is reduced in thrombotic thrombocytopenia purpura, while renal dysfunction is more common in hemolytic uremic syndrome. Prompt treatment is necessary to prevent multiorgan failure and death.
Acute fatty liver of pregnancy presents with severe and early coagulopathy or disseminated intravascular coagulopathy due to reduced production by the liver. Markedly elevated liver enzymes, more notable than with preeclampsia, are usually present. Hemolysis is rare, though elevated bilirubin is more common than in preeclampsia. Hypoglycemia may be present due to hepatic injury. Marked metabolic acidosis necessitates prompt delivery of the fetus.
Systemic lupus erythematous exacerbation can manifest with hypertension, proteinuria, and microscopic hematuria, similar to preeclampsia. Extrarenal manifestations, such as rash and joint pain, and pancytopenia with systemic lupus erythematous help differentiate the two processes. Catastrophic antiphospholipid antibody syndrome is a rare complication that causes acute thrombotic microangiopathy, which can affect the liver and lead to Budd-Chiari syndrome, liver necrosis, and infarcts. Prompt anticoagulation is a necessity in this life-threatening condition.
SUMMARY
Liver injury is an indicator of severe preeclampsia or HELLP syndrome with significant associated perinatal morbidity and mortality. Further research is needed to identify pregnant people at risk for developing these complications and more so, in understanding the biology of HDP and HELLP to modulate treatment and prevention.
Acknowledgments
ACKNOWLEDGMENTS
Figures 1, 3, and 4 were created with Biorender.com.
CONFLICTS OF INTEREST
Yalda Afshar consults for Mirvie. Jenny Y. Mei has no conflicts to report.
Footnotes
Abbreviations: ALT, alanine transaminase; AST, aspartate aminotransferase; BP, blood pressure; HELLP, hemolysis, elevated liver enzymes, and low platelets.
Contributor Information
Jenny Y. Mei, Email: JMei@mednet.ucla.edu.
Yalda Afshar, Email: yafshar@mednet.ucla.edu.
REFERENCES
- 1. Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R. Pre-eclampsia. Lancet. 2010;376:631–644. [DOI] [PubMed] [Google Scholar]
- 2. Duley L. The global impact of pre-eclampsia and eclampsia. Semin Perinatol. 2009;33:130–137. [DOI] [PubMed] [Google Scholar]
- 3. Alese MO, Moodley J, Naicker T. Preeclampsia and HELLP syndrome, the role of the liver. J Matern Fetal Neonatal Med. 2021;34:117–123. [DOI] [PubMed] [Google Scholar]
- 4. Gestational Hypertension and Preeclampsia: ACOG Practice Bulletin Summary, Number 222. Obstet Gynecol. 2020;135:1492–1495. [DOI] [PubMed] [Google Scholar]
- 5. Khodzhaeva ZS, Kogan YA, Shmakov RG, Klimenchenko NI, Akatyeva AS, Vavina OV, Kholin AM, et al. Clinical and pathogenetic features of early- and late-onset pre-eclampsia. J Matern Fetal Neonatal Med. 2016;29:2980–2986. [DOI] [PubMed] [Google Scholar]
- 6. Hammoud GM, Ibdah JA. Preeclampsia-induced liver dysfunction, HELLP syndrome, and acute fatty liver of pregnancy. Clin Liver Dis. 2014;4:69–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Minakami H, Oka N, Sato T, Tamada T, Yasuda Y, Hirota N. Preeclampsia: A microvesicular fat disease of the liver? Am J Obstet Gynecol. 1988;159:1043–1047. [DOI] [PubMed] [Google Scholar]
- 8. Carmiel Haggai M, Sgayer I, Bornstein J, Odeh M, Lowenstein L, Frank Wolf M. Liver stiffness and steatosis in preeclampsia as shown by transient elastography-a prospective cohort study. Am J Obstet Gynecol. 2022;227:515.e1–515.e9. [DOI] [PubMed] [Google Scholar]
- 9. Ditisheim A, Sibai BM. Diagnosis and management of HELLP syndrome complicated by liver hematoma. Clin Obstet Gynecol. 2017;60:190–197. [DOI] [PubMed] [Google Scholar]
- 10. US Preventive Services Task Force. Barry MJKW, Mangione CM, Cabana M, Caughey AB, Davis EM, et al. Aspirin Use to Prevent Preeclampsia and Related Morbidity and Mortality: US Preventive Services Task Force Recommendation Statement. JAMA. 2021;326:1186–1191. [DOI] [PubMed] [Google Scholar]
- 11. Altman D, Carroli G, Duley L, Farrell B, Moodley J, Neilson J, et al. Magpie Trial Collaboration Group . Do women with pre-eclampsia, and their babies, benefit from magnesium sulphate? The Magpie Trial: A randomised placebo-controlled trial. Lancet. 2002;359:1877–1890. [DOI] [PubMed] [Google Scholar]


