Abstract
‘G’ antigen belongs to the Rh family and it was first described by Allen and Tippet in 1958. Various anti-D, anti-C, and anti-G antibody combinations can be found in patients. Ruling out the presence of anti-D is important for administering RhIg prophylaxis in RhD-negative pregnant women to prevent hemolytic disease of fetus and newborn (HDFN). RhIg prophylaxis is not indicated in the presence of an anti-D antibody. Time-to-time monitoring and follow-up of cases of RhD-negative pregnant women with a multi-disciplinary approach including an obstetrician, neonatologist, and transfusion medicine specialist helps diagnose, manage, and monitor HDFN in such cases. This case report emphasizes the need for proper antibody identification (anti-G) and managing HDFN (with intrauterine transfusions and exchange transfusion) during the perinatal period.
Introduction
‘G’ antigen shares epitope with both D and C antigen and is present on most D-positive and all C-positive RBC’s [1]. Anti-G antibody, therefore, may be formed by all D-negative, G-negative patients. This alloantibody may be formed through pregnancy, transfusion or transplant with exposure to ‘C’ antigen positive RBC. On antibody identification testing, anti-G reacts as though if it is a mixture of anti-C and anti-D antibodies. However, distinction of anti-G from mixture of anti-D and anti-C is important in obstetric patients [1]. Patients with anti-G with or without anti-C are eligible for RhIg prophylaxis to prevent hemolytic disease of fetus and newborn (HDFN). On the other hand, RhIg is not helpful in those who have already developed anti-D alloantibody.
Patient with unexpected antibody (example: anti-C, anti-D) require active regular monitoring and possible interventions like intra-uterine transfusion and exchange transfusion for successful management of pregnancy and neonate. We would like to report one such case of successful management of an obstetric patient with multiple alloantibodies (anti-D, anti-C and anti-G) and her newborn from a fetal medicine, transfusion medicine and neonatologists’ perspectives.
Case Report
A 34-year-old woman was referred to Fetal Medicine center at 16 weeks gestation with a positive Indirect Coomb’s Test (ICT) report. Patient’s and her husband’s blood group were A Rh (D) neg and O Rh(D) pos, respectively. She was gravida five with 2 healthy children delivered at term, one medical termination of pregnancy (surgical method) and one missed miscarriage. Although she received post-partum Anti-D after the term deliveries, prophylactic Anti-D was not received in the latter 2 pregnancies (MTP and miscarriage).
The couple was counseled at length about the possibility of fetal anemia and the need for strict monitoring. Fetal surveillance was done by middle cerebral artery peak systolic velocity (MCA-PSV). The MCA-PSV exceeded 1.5 MoM (multiples of the median) at 26 weeks and 5 days necessitating need for intra-uterine transfusion.
Advanced immunohematology work up identified alloantibodies with specificity of anti-D and -C antibodies with titers 2048 and 512, respectively. Subsequent, adsorption-elution studies confirmed third alloantibody (anti-G).
Multi-disciplinary team comprising specialists from Fetal Medicine, Transfusion medicine and Neonatology was formed. Transfusion Medicine ensured that appropriate blood unit {O Rh (D and C) negative, less than 5-days old, additive solution depleted, leukodepleted, irradiated, crossmatch compatible, and hematocrit (75–80%)} was provided.
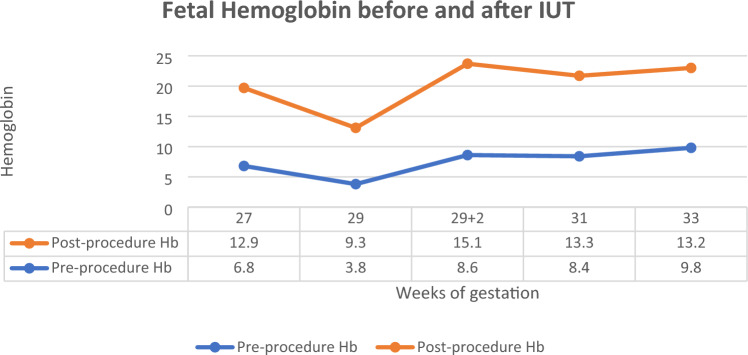
First IUT was performed at 27 weeks gestation. A follow-up after 1 week was suggested however the patient followed up after 2 weeks and MCA-PSV > 1.5 MoM along with fetal hydrops was observed. In order to avoid overload, one IUT was performed the same day and the subsequent one after 2 days. The rate of Hb decline between first and second IUT was 0.5 g/dl. Once hydrops resolved, further requirement was at 2 weeks interval (at 31 and 33 weeks). Overall, 5 intra-uterine transfusions were given (Fig. 1, Table 1).
Fig. 1.
Pre-and post-procedure fetal Hb with each IUT
Table 1.
anti-D and anti-C antibody titers, IUT volume with pre- and post- Hb and MCA-PSV during IUT period
| Weeks of gestation | 27 | 29 | 29 + 2 days | 31 | 33 |
|---|---|---|---|---|---|
| Anti-D titer | 2048 | 1024 | 1024 | 512 | 512 |
| Anti-C titer | 512 | 128 | 128 | 64 | 64 |
| Pre-Hb | 6.8 | 3.8 | 8.6 | 8.4 | 9.8 |
| Post-Hb | 12.9 | 9.3 | 15.1 | 13.3 | 18.2 |
| Pre MCA-PSV (cm/sec) | 52.6 | 80 | 60 | 62 | 55 |
| Post IUT MCA-PSV (cm/sec) | 31 | 48 | 26.2 | 40 | 34 |
| IUT (Volume of reconstituted blood) | 35 | 70 | 80 | 80 | 120 |
Male fetus (weight- 2.8 kg) was delivered at 34 weeks of gestation by elective caesarean section. Neonate developed respiratory distress syndrome (RDS) shortly after birth for which he was medically managed in neonatal intensive care unit (NICU). Cord blood hemoglobin and bilirubin were 15.8gm/dL and 6.28 gm/dL, respectively. History of Rh iso-immunization and rise in bilirubin (at 1 h-7.13 gm/dL and at 6 h-10.3 gm/dL) warranted exchange transfusion (ET). A double volume ET was performed with freshly reconstituted whole blood {450 ml, O Rh (D and C) neg with AB group plasma, leukodepleted, irradiated, and crossmatch compatible, hematocrit-55–60%}. Phototherapy was also initiated. Neonate was also infused IV immunoglobulins (Day 2 and 4) for mild decrease in post-ET bilirubin levels (10.1 gm/dL). Neonate was discharged on day 5, with hemoglobin of 19.5 gm/dL and bilirubin of 9.5 gm/dL, in stable condition.
Discussion
The present case report highlights the coordination between the Fetal medicine, transfusion medicine and Neonatologists for successful management and outcome of pregnancy complicated with hemolytic disease on fetus and newborn (HDFN) due to multiple alloantibodies (anti-D, anti-C and anti-G).
Transfusion Medicine Perspective
Anti-D, anti-C and anti-G antibodies have been implicated in HDFN. Anti-G and mixture of anti-D and anti-C share specificity pattern on immunohematological testing; therefore, it is important to differentiate between these. While pregnant women with anti-G and/or anti-C are candidates for receiving Rh immuno-prophylaxis (anti-D) to prevent HDFN, those with anti-D are not. To differentiate between these antibodies (Anti-G and mixture of anti-D and anti-C), blood center laboratory need to perform advanced immunohematology work-up including adsorption-elution using special phenotyped cells [2]. Like present case report, there have been previous reports on anti-G alone [2] and/or with mixture of anti-D and anti-C [3, 4].
Authors’ center was also able to provide appropriate blood component for IUT and ET (specification included: corresponding antigen {D, C, G} negative unit, leukoreduced, irradiated with desired hematocrit) as per the requirement of fetal medicine and neonate specialist.
Fetal Medicine Perspective
In management of Rh iso-immunized pregnancies, it is extremely important to have high index of suspicion based on past obstetric history. It is equally important to screen for irregular antibody as part of antenatal check-up. Fetal medicine experts confirm the diagnosis of HDFN with non-invasive investigation like middle cerebral artery peak systolic velocity (MCA-PSV) on USG. In present case report, fetal medicine expert promptly suspected HDFN and advised advanced immunohematological work-up and IUT. This new discipline of fetal medicine has the right training and experience to provide appropriate counseling to the patient and ensures appropriate management to the patient. Accessibility to fetal medicine expert, easier availability of MCA-PSV and IUT has ensured that severe manifestations of HDFN like hydrops fetalis are uncommon, especially in metropolitan cities.
Although Rh iso-immunization is amenable to treatment, Fetal Medicine specialists strongly advocate appropriate Anti-D prophylaxis as it significantly contributes to reduction of this condition thereby improving perinatal outcomes. Our patient did not receive Anti-D after first trimester MTP and miscarriage managed at two different centers. This highlights the need of awareness among obstetricians about Anti-D prophylaxis especially after early trimester pregnancy losses to reduce the incidence of Rh iso-immunization.
Neonatology Perspective
Fetal medicine expert and neonatologist work in tandem, managing HDFN before and after birth. In the present case, double volume ET was performed on day 0 by neonatologist in-view of clinical history of HDFN, anemia and rapidly rising bilirubin. Prompt recognition, and immediate intervention in terms of ET, phototherapy and other supportive treatment ensures favorable outcomes in such neonates.
Conclusion
Anti-‘G’ needs to be differentiated from anti-D and anti-C in all antenatal cases as this determines the pre-natal and post-natal RhIg prophylaxis.
Author Contributions
Authors hereby state that the concept of this study was done by AKT and PS, data collection was done by SS, GA, SG and manuscript writing by PS, SG, AKT and reviewed by all authors.
Funding
The authors declare no funding.
Conflict of interest
The authors declare no conflict of interest.
Ethical Approval/Informed Consent
The patient’s identifier was removed, complete confidentiality was maintained and Informed consent of the patient was obtained.
Footnotes
Pragya Silwal (MD, DNB) is an Senior Resident;Aseem K. Tiwari (MD) is a Director; Shreyasi Sharma (MD) is a Director; Geet Aggarwal (DNB) is an Associate Consultant ; Sunil Golia (MBBS) is a Junior Resident.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Harmening DM. Modern blood banking & transfusion practices. Philadelphia: F A Davis Company; 2019. pp. 149–172. [Google Scholar]
- 2.Das S, Shastry S, Murugesan M, Shastry S. What is it really? Anti-G or anti-D plus anti-C: clinical significance in antenatal mothers. Indian J Hemat Blood Transfus. 2017;33:259–263. doi: 10.1007/s12288-016-0729-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Makroo RN, Kaul A, Bhatia A, Agrawal S, Singh C, Karna P. Anti-G antibody in alloimmunized pregnant women: report of two cases. Asian J Transfus Sci. 2015;9(2):210. doi: 10.4103/0973-6247.162724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rai P, Sharma G, Singh D, Garg J. Approach to a pregnant woman with anti D+ anti C reactivity pattern: a diagnostic conundrum. J Clin Diagn Res JCDR. 2017;11(9):ED06. doi: 10.7860/JCDR/2017/27902.10550. [DOI] [PMC free article] [PubMed] [Google Scholar]