Abstract
The global invasive meningococcal disease (IMD) landscape changed considerably during the COVID-19 pandemic, as evidenced by decreased incidence rates due to COVID-19 mitigation measures, such as limited social contact, physical distancing, mask wearing, and hand washing. Vaccination rates were also lower during the pandemic relative to pre-pandemic levels. Although policymakers may have shifted their focus away from IMD vaccination programs to COVID-19 vaccination programs, strong arguments support implementation and prioritization of IMD vaccination programs; IMD cases have increased in some countries and IMD rates may even have exceeded pre-pandemic levels. Additional concerns include increased susceptibility due to vaccination coverage gaps, increased incidence of other respiratory pathogens, immunity debt from lockdown restrictions, and increased IMD epidemiologic variability. The full range of benefits of widely available and effective meningococcal vaccines needs to be considered, especially in health technology assessments, where the broad benefits of these vaccines are neither accurately quantified nor captured in implementation policy decisions. Importantly, implementation of meningococcal vaccination programs in the current IMD climate also appeals to broader healthcare principles, including preparedness rather than reactive approaches, generally accepted benefit–risk approaches to vaccination, historical precedent, and the World Health Organization's goal of defeating meningitis by 2030. Countries should therefore act swiftly to bolster existing meningococcal vaccination strategies to provide broad coverage across age groups and serogroups given the recent increases in IMD incidence.
Keywords: COVID-19, Epidemiology, Immunization programs, Incidence, Vaccines
Key Summary Points
| The COVID-19 pandemic has affected invasive meningococcal disease (IMD) globally. |
| Recent increases in IMD cases have been observed, most of which were meningococcal serogroup B. |
| Implementation and prioritization of IMD vaccination programs is necessary. |
| Health technology assessments need to consider the full range of meningococcal vaccination benefits. |
| The increasing number of IMD cases highlights the need for preparedness by implementing vaccination programs now instead of reactively. |
Introduction
Invasive meningococcal disease (IMD), caused by invasion of Neisseria meningitidis into a normally sterile site in the body, most often manifests as meningitis or septicemia [1]. IMD is characterized by its rapid and severe clinical course, typically commencing with nonspecific symptoms before progressing to a potentially life-threatening illness within hours [2]. Cases are sometimes fatal, with an estimated 8.3% overall case fatality rate [3], and many survivors experience long-term sequelae and short- and long-term reduced health-related quality of life (QoL) [4].
Although IMD cases are relatively rare [5], the capacity of meningococci for continued antigenic change causes a constantly evolving epidemiology characterized by unpredictable outbreaks [6–8]. For example, IMD caused by serogroup W (MenW) was infrequent before 2000, but emergence of hypervirulent clonal complex 11 strains led to marked global increases [9]. Additionally, after implementation of successful serogroup A (MenA) vaccination programs in Africa, serogroup C (MenC), W, and X outbreaks and epidemics were observed [6]. The inherent unpredictability of IMD was further observed in the United Kingdom (UK), where serogroup B (MenB) and MenC caused epidemics for many years during the 1990s, followed by the emergence of MenW in 2013 [10, 11].
Given clinical and epidemiologic factors, the World Health Organization (WHO) has established a goal of defeating meningitis by 2030; vaccination is a key step toward achieving this goal, based on robust evidence of effectiveness of currently available meningococcal vaccines [12, 13]. Infants, toddlers, and adolescents/young adults are prime targets for vaccination due to higher rates of IMD within those age groups [13, 14], which maximizes direct and indirect conjugate vaccine–mediated IMD protection [15]. The predominant serogroup(s) causing disease vary among countries because of factors such as natural temporal fluctuations, location, and available public health interventions [15]. In this context, current vaccination programs vary by country according to targeted age groups and covered serogroups [13, 15].
The global IMD landscape changed considerably during the COVID-19 pandemic [16]. IMD incidence rates decreased globally in connection with COVID-19 mitigation measures, such as limiting social contact, physical distancing, mask wearing, and hand washing [16, 17]. Simultaneously, 2020 childhood vaccination rates in general were much lower than pre-pandemic rates worldwide [18]. During the pandemic, many parents delayed or canceled scheduled meningococcal vaccination appointments for their children [19]. However, a resurgence in IMD has recently been observed in several countries, such as England and France [20, 21]. Therefore, using a preparedness approach with well-tolerated and effective vaccines should be considered during this time of increasing IMD cases. A meningococcal vaccination program is also a key component of the WHO’s initiative to defeat meningitis by 2030, with goals that include improving QoL after meningitis due to any cause, eliminating bacterial meningitis epidemics, and reducing IMD cases, disability, and deaths [12]. Here, we outline arguments supporting the implementation of IMD vaccination programs in the current climate of IMD resurgence and increased incidence rates as a crucial approach in moving toward the WHO goal of defeating meningitis. This article is based on previously conducted studies and does not contain data from any new studies with human participants or animals performed by any of the authors.
Invasive Meningococcal Disease Epidemiology in the Covid-19 Era
Lockdown Restriction Effects
In many countries, IMD incidence rates decreased after the onset of the COVID-19 pandemic [16]. Notably, IMD rates were already decreasing in many regions before the pandemic due to combined effects of vaccination programs and secular trends [13]. Pandemic-associated incidence reductions varied across countries; given the caveat that countries differed in COVID-19 mitigation measures and surveillance programs [22], the largest decreases generally occurred in countries with established meningococcal vaccination programs. For example, in Spain, which has a comprehensive vaccination program that includes infant and toddler MenC vaccination and adolescent meningococcal serogroups A, C, W, and Y (MenACWY) vaccination, a single case of IMD was reported by Week 31 of 2021 compared with 24 cases in 2018 and 21 in 2019 [23]. In Poland, which recommends MenC vaccination for those aged 2 months to 19 years, 62 cases were observed by Week 39 of 2021 compared with 116 and 121 in 2018 and 2019, respectively [23, 24]. In South America in 2020, Brazil and Chile reported reductions of 65.0% and 91.3%, respectively, of confirmed IMD cases in 2019 [19]. Brazil’s vaccination program includes infant, toddler, and adolescent MenC vaccination and adolescent MenACWY vaccination, whereas Chile’s immunization program includes MenACWY vaccination in 12-month-olds and MenACWY or MenB vaccination for at-risk populations [25, 26].
As with IMD, meningococcal carriage rates were initially expected to decrease during the pandemic. However, the evidence regarding meningococcal carriage during the COVID-19 pandemic is conflicting. In a review of COVID-19–related childhood immunity debt, lockdown measures were associated with decreased asymptomatic meningococcal carriage [17]. Alternatively, a study of Australian university students found meningococcal carriage rates were higher after COVID-19 containment measures (3.7% in February/March 2020 versus 6.8% in August/September 2020); however, these rates might also relate to students being locked down in residence halls, thereby increasing close contacts [27]. The role of reduced incidence of seasonal respiratory viruses, particularly influenza, during the first 2 years of the pandemic as a contributing factor to the decrease of IMD rates also deserves in-depth studies.
Invasive Meningococcal Disease Epidemiology in the Post–Covid-19 Era
Return to Pre-pandemic Behavior Effects
As expected, easing of COVID-19 lockdown restrictions has been associated with increased IMD rates in several countries. Incidence of meningococcal disease increased in 2022 in the United States (US), following a decline in IMD rates during 2020−2021 [28]. In England, IMD cases dropped steeply in March 2020 but substantially increased from September through November 2021 after in-person learning resumed in schools and universities; nearly all new cases were MenB [20]. Importantly, case numbers among 15- to 19-year-olds during this period exceeded pre-pandemic levels, and 41.5% of IMD cases occurred in this age group compared with 11.8% in 2018 and 14.3% in 2019 [20]; currently, no MenB vaccination program exists for this age group in the UK. In France, lockdown measures during COVID-19 were associated with more than 2 years of reduced IMD incidence [21]. However, case numbers in December 2022 exceeded pre-pandemic levels. The majority of cases were MenB (53%) and were mainly observed among infants and those 15–24 years old [21]. Importantly, MenB rates in December 2020 were higher than pre-pandemic levels, especially among 15- to 24-year-olds [21]. This is of notable concern because France lacks a mandatory MenB vaccination program for adolescents/young adults (although vaccination is recommended in those at high risk of contracting the disease) [23, 29, 30], and occurrence of MenB disease in this age group may indicate the emergence of hypervirulent strains [31]. Moreover, health officials in Brazil have emphasized the importance of meningococcal vaccination among children and adolescents due to a recent MenC outbreak in São Paulo [32].
The epidemiology of IMD after the return to pre-pandemic behaviors in countries with vaccination programs likely depends on the serogroups that these vaccination programs cover. For instance, the swift and steep MenB case increase observed in England in 2021 may reflect a combination of high carriage and transmission primarily in adolescents/young adults, and may indicate a need for an adolescent MenB vaccination program [20]. Similarly, the increase in MenB cases in France in December 2022 further highlights the need for an adolescent MenB vaccination program [21, 23]. Importantly, recent reports of meningococcal outbreaks (e.g., the MenC outbreak in Florida among gay and bisexual men and the IMD outbreak in the Democratic Republic of Congo) and rising case numbers (e.g., MenB cases among adolescents/young adults in England) show that IMD is a continued public health threat [20, 33, 34]. Furthermore, the inherent unpredictability of IMD [6] raises concerns that serogroup distribution may change in post-pandemic periods, potentially limiting effectiveness of existing vaccination programs and leading to more complicated and costly outbreak management.
Although the effect of lifting COVID-19 mitigation measures on meningococcal carriage rates is not established, the capability for meningococcal carriage to rise rapidly with increased social activity was documented before COVID-19 emergence. A study of British university students found that meningococcal carriage increased from 6.9% on the first day of classes to 23.1% three days later, with average carriage rates among students living in catered halls increasing from 13.9% in October to 34.2% in December [35]. A more recent study of students newly admitted to a university dormitory in South Korea also reported an increase in meningococcal carriage rates over time, from 2.7% at baseline to 6.3% at 1 month and to 11.8% at 3 months [36]. Furthermore, studies have established that visits to bars or other crowded venues and kissing are significant risk factors for meningococcal acquisition [35, 37, 38].
Gaps in Vaccination Coverage and Immunity Debt
As physical distancing measures have abated, immune protection against IMD may have declined relative to pre-pandemic levels because of decreased vaccine uptake and increased susceptibility to infectious diseases in the post-pandemic period, termed “immunity debt” [17, 39, 40]. Reductions in sales of recommended pediatric vaccines in the US, including non-influenza and measles-containing vaccines, further illustrate the effects of the COVID-19 pandemic [41]. Overall doses ordered were lower in 2020 than in 2019, with the decrease in orders more prominent among those aged 24 months to 18 years [41]. The reduction in routine pediatric vaccine sales, and similar trends in reduced dose administration, highlight the vulnerability of US children to vaccine-preventable disease outbreaks [41]. Similar findings were observed in California, USA, where human papillomavirus vaccine uptake among 9- to 12-year-olds fell in March/April 2020; in May 2020, however, uptake rates increased to similar levels observed in 2019 [42]. MenC vaccine uptake among French infants during the first lockdown was lower than expected for the first dose given to 5-month-olds (10.9% decline) and the booster given to 12-month-olds (20.7%), with overall 2.8% and 13.8% declines, respectively, through Q4/2020 [43]. The meningococcal vaccination rate decline during the pandemic is further evidenced by survey results indicating that 50% of parents in eight countries (Argentina, Australia, Brazil, France, Germany, Italy, UK, US) delayed or canceled meningococcal vaccination appointments during the pandemic, with main reasons including lockdowns, concerns of catching COVID-19, or needing to care for someone with COVID-19 [44].
The overall decrease in exposure to pathogens during the pandemic may also lead to immunity debt, possibly resulting from impaired adaptive immunity against specific infectious agents and decreased innate immunity because of lack of immune stimulation [17, 39]. This may invite rebounds in IMD and other vaccine-preventable infectious diseases, as described below [17, 39]. Therefore, relevant and current seroepidemiology data, especially following the COVID-19 pandemic, are needed to help estimate or model the epidemiologic implications of COVID-19 on IMD.
Changing Epidemiology of Other Respiratory Infectious Diseases
Concerns surrounding changes in infectious disease epidemiology in the post-pandemic period are not unique to IMD. In Australia, following relaxations in physical distancing measures, cases of respiratory syncytial virus (RSV) drastically increased beginning in September 2020, far exceeding annual peaks observed in 2012−2019, with median patient age significantly higher than in previous years (18.4 vs. 7.3−12.5 months; P < 0.001) [45]. France and the US also observed delayed RSV seasonality in 2021 [46, 47]. Conversely, in a New York hospital, the median age among those < 18 years old testing positive for RSV was 6 months in 2021 versus 17 months in 2019−2020; additionally, 81% of those admitted were moved to the intensive care unit compared with 45% in the 2019−2020 season [48]. Similarly, an increase in childhood invasive pneumococcal disease cases was observed in England after COVID-19 restrictions were lifted [49]. For respiratory infections, immunity debt may be contributing to this increased potential for more epidemics and higher case numbers [49, 50]. These findings collectively suggest that infectious diseases can increase rapidly following easing of lockdown restrictions; furthermore, reemergence may cause epidemiologic changes or case number increases, which may then exert pressure on healthcare systems. Additionally, infection rate increases for other respiratory pathogens may directly potentiate IMD increases. For example, historical evidence on individual and population levels link IMD with prior influenza infection [51].
Preparedness Against Invasive Meningococcal Disease
Meningococcal Vaccination Program Effectiveness
Abundant real-world evidence supports the effectiveness of meningococcal vaccination programs. Successful vaccination programs have been comprehensively reviewed elsewhere [13]; here, we discuss several notable or recent examples. A > 99.9% decrease in confirmed MenA cases was observed across nine African countries following implementation of MenA conjugate vaccination programs beginning in 2010 (Fig. 1A) [52]. In England, the introduction of a MenC vaccination program in 1999 for infants, with a one-time catch-up for children up to 18 years old, was associated with a 93.1% decrease in MenC cases from 1998/1999 to 2003/2004 [53–55]. In 2009, 10 years following the introduction of the MenC vaccination program, a study estimated that 9000 MenC cases had been avoided, resulting in a cumulative savings of £75 million [56]. In 2013, a MenC booster dose was recommended for teenagers aged 14 years to improve protection against MenC disease and to maintain high levels of herd protection, with 97.1% reduction in MenC cases persisting through 2019/2020 (Fig. 1B) [53–55]. In 2015, the single MenC dose for adolescents was replaced by the MenACWY vaccine to combat steep MenW disease increases, with an estimated effectiveness of 94% against MenCWY disease (no cases of diseases by MenA were reported/identified) [57]. Similarly, 2018 implementation of toddler and adolescent MenACWY programs in the Netherlands to address increasing MenW disease rates was associated with 85% and 50% reductions in MenCWY cases in vaccine-eligible and ineligible cohorts, respectively (no cases of diseases by MenA were reported/identified) [58].
Fig. 1.
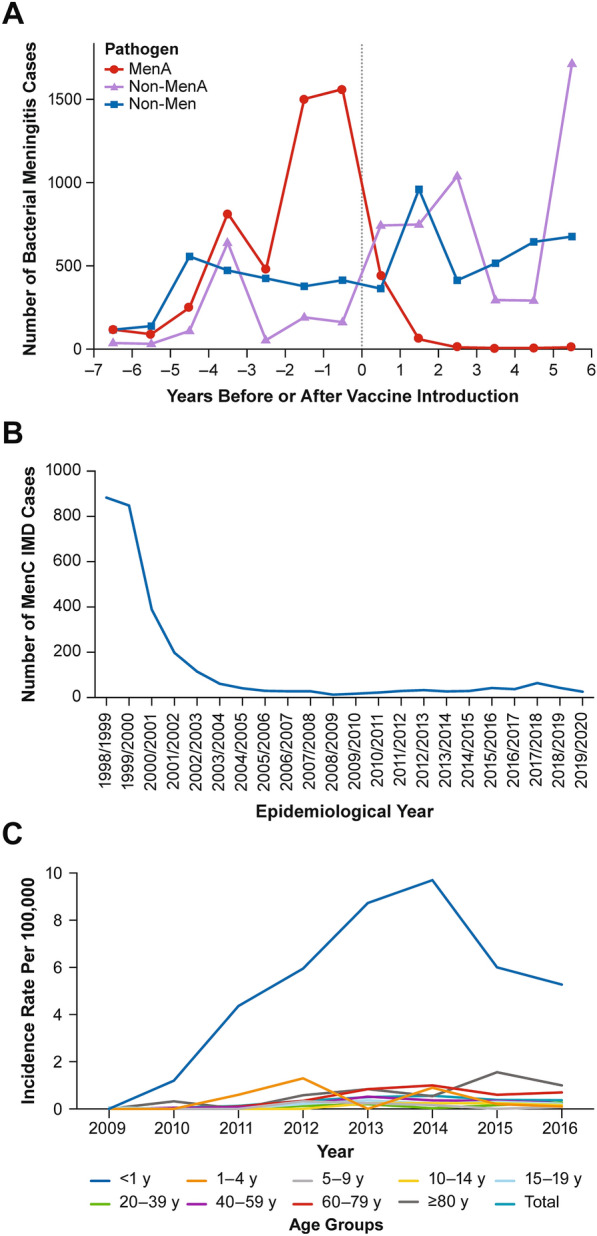
Examples of IMD epidemiology before and after implementation of mass vaccination programs including: A MenA cases in 9 African countries (reproduced with permission from Trotter and colleagues) [52], B MenC cases in England [54], and C MenW incidence by age group in Chile (reproduced with permission from Villena and colleagues) [59]. IMD invasive meningococcal disease, MenA meningococcal serogroup A, MenC meningococcal serogroup C, MenW meningococcal serogroup W, Non-MenA other meningococcal serogroups, Non-Men pathogens other than Neisseria meningitidis
Outside Europe, a MenACWY vaccination campaign to combat rising MenW disease rates was initiated in Chile in 2012 for those 9 months to 4 years old, with routine vaccination for 12-month-olds introduced in 2014 [59]. By 2016, a 92.3% MenW disease reduction was observed among 1- to 4-year-olds, the age group that was targeted by the vaccination program (Fig. 1C) [59]. Interestingly, no early indirect effects of the toddler vaccination were observed in 2012–2014, emphasizing the importance of including adolescents (the age groups that usually have the highest carriage rates) in the vaccination programs to achieve indirect protection [59, 60].
Holistic Approach to the Value of Preventive Meningococcal Vaccination
Although initial cost-effectiveness studies have generally reported MenB vaccination strategies to be cost-ineffective [61], existing health technology assessments generally fail to capture the full range of vaccination benefits [62–64]. For example, although previous cost-effectiveness studies have found MenB vaccination cost-effective only at low prices or cost-ineffective, a recent analysis found a 4-component vaccine that protects against MenB and is cost-effective in England when considering additional aspects of the disease (i.e., 5 “disease burden categories”) for a comprehensive analysis of the broad burden of MenB [65]. Similar findings were observed in Germany, where the 4-component MenB vaccine was found to be more cost-effective when considering broader aspects, such as the quality-adjusted life-years effect on patients and caregivers [66]. Additionally, a systematic review found that the effect of IMD sequelae is underestimated because of underreporting and the small available dataset, particularly regarding the real rate of long-term sequelae, but such evaluations are warranted in economic assessments of vaccination programs [67]. Moreover, a recent review of the impact of cost-effectiveness analyses on vaccine policy decisions in the UK, the US, the Netherlands, and Canada reported that vaccine availability, serogroup incidence over time, and the disastrous nature of IMD mainly drive vaccine recommendations, whereas traditional cost-effectiveness analyses did not play a major role in recommendations, in part because they tend to underestimate the value of vaccination against IMD (i.e., not considering risk reduction for both the vaccinee and their close contacts) [55].
Although calculating the costs of vaccination programs is relatively straightforward, the calculation of benefits is less so, and economists traditionally focus on a narrow range of implications for these programs (e.g., medical costs avoided with children not getting sick) [68]. Other burdens, such as cognitive or psychological problems, family or legal burdens, adaptive measures, concern about meningococcal disease, and social crisis management, are less easily quantifiable and are consistently neglected in cost-effectiveness analyses [69]. Indeed, assessment of indirect costs associated with IMD is highly dependent on sequelae severity, and varies among and within countries. These costs may largely affect low-income countries because a disproportionately large portion of household annual income may be needed to cover costs of utilized resources [69]. Policymakers should therefore consider outcomes to determine the full public health value of vaccines in evidence-based decision-making, including broader, non-health effects, such as social and economic benefits; reductions in disease incidence, transmission, and size/frequency of outbreaks; health system stabilization; and a more balanced view of cost-effectiveness data that balances value, access and profit, and public good [70].
Proper valuation of vaccination is not a purely academic exercise because the process by which the value of vaccination is estimated has consequences for vaccine cost and policy, which in turn have effects on personal health and well-being, especially in disadvantaged groups [71]. Given that health technology assessments do not consider the broader benefits of vaccination consistently, five priority areas for improvement have been suggested: broader healthcare cost offsets, effect on caregiver QoL, transmission value, prevention of antimicrobial resistance, and macroeconomic effects [72, 73]. Suggestions for future policy-oriented vaccination studies include evaluating the impact of vaccination on school attendance, educational achievement, cognitive development, employment (including hours worked and earnings), and the development of a calibrated epidemiologic/economic model to estimate vaccination value [71]. The use of experimental and observational studies may be another way to address gaps in evidence that link vaccination to economic benefits other than direct health benefits and reduced medical costs [74].
With regard to government budgeting, vaccination program costs may be accurately estimated, with the maximum budget estimated at 100% uptake; however, budgeting for treatment of vaccine-preventable diseases may be more difficult due to variable costs [56]. The cost of disease prevention through vaccination is relatively low given the associated benefits, and, thus, return-on-investment analyses that better estimate short-term vaccination benefits may complement cost-effectiveness analyses [56]. Consideration of all vaccination-related competing priorities (e.g., health, economic growth, equity, education) is necessary for government healthcare budgeting decisions and broader interventions [56, 75].
Disparities in vaccine uptake among socioeconomic and demographic groups because of limitations in access to healthcare and healthcare providers increase risks of IMD. In the US, coverage of ≥1 dose of MenACWY vaccine among 13- to 17-year-olds ranged from 86.1% to 91.6% in 2020 among those with annual incomes below the poverty line, with rates similar to those at or above the poverty line (85.6%–90.2%) [76]. However, coverage rates for ≥2 doses were 47.4%–48.6% versus 50.2%–61.2%, respectively. Similarly, a cross-sectional study of 16- to 18-year-olds in the Philadelphia immunization registry in 2015–2017 reported a significant difference in MenB vaccination coverage by socioeconomic status, where MenB vaccine recipients were more likely to live in a neighborhood with a median income of > US$100,000 compared with < $20,000 (P < 0.0001) [77]. Additionally, sequelae of IMD may affect people from low-income backgrounds unequally because resources for IMD survivors may require a large portion of their household income [69].
Many low- and middle-income countries (LMICs) have limited access to some vaccines and therapeutics [78–80]. Limited access to healthcare and vaccination may also lead to epidemics and outbreaks in such low-income regions [81]. Meningococcal vaccination in LMICs may only be available through external support, such as Gavi, the Vaccine Alliance, to fund purchases of vaccines [78, 80]. In a systematic review describing investment cases for vaccines and immunization programs, the authors reported that the investment cases identified research and development gaps in LMICs, including the need for funds to support clinical trials and purchases of vaccines [82]. The withdrawal of Gavi support in LMICs transitioning to fully self-financing may potentially lead to additional funding gaps experienced by some countries [80].
A 2020 publication presented a taxonomy for MenB vaccine evaluation that includes internalized and externalized health and non-health benefits (Table 1), with the goal of comprehensively accounting for the devastating nature of IMD and the corresponding protective impact of vaccination [64]. The authors suggested the need to evaluate more broadly the cost of IMD and the cost benefits of MenB vaccination [64]. A modeling study that assessed the effect of MenB vaccination among college students demonstrated that MenB vaccination not only lowered MenB incidence and number of outbreaks but also reduced costs associated with MenB outbreaks [83]. In a systematic review and synthesis of published evidence [84], mean healthcare costs associated with acute infection in 2014 international dollars were reported at I$50,796 in the US. Notably, the healthcare costs of IMD were higher than those estimated for influenza and RSV infections, with $15,163 and $16,034 (2013 US dollars), respectively, in hospitalized US adults aged ≥60 years [85]. These findings illustrate the high burden of IMD on healthcare costs compared with other infections and the importance of preventing IMD disease. Importantly, most IMD analyses focus only on acute infection costs, and a broader analysis should incorporate direct costs of both acute and long-term phases, including all expenses relevant to recovery from infection [64].
Table 1.
Taxonomy of MenB vaccination benefitsa adapted from Stawasz and colleagues (adapted with permission under the CC-BY license) [64]
| Health benefits | Social/economic benefits | |
|---|---|---|
| Internalized |
Direct health gains (I) Household health externalities (I; F) Prevention and amelioration of comorbidities (I) Reductions in nosocomial infections (H; I) |
Education gains (I) Labor market productivity gains (I) Nonmarket productivity and leisure gains (I) Caregiver productivity and leisure gains (F) Risk reduction gains (C; I) |
| Externalized | Full public health benefits (B) |
Healthcare cost savings (C; I) Social preference fulfillment (C) Outbreak control gains (C; H) Litigation mitigation (F; H; I) Macroeconomic gains (B; C; I) Institutional disruptions (C; F; I) Equity gains (C; F; I) Health system efficiency gains (H) |
B broader society, C communities, F families, H healthcare/hospital, I individuals, MenB meningococcal serogroup B
aLetters presented in parentheses denote the group(s) potentially affected by the corresponding benefit. Italicized benefits categories comprise narrow benefits. All other listed benefits are broad benefits
The uptick in IMD cases following lockdown restriction relaxations, as demonstrated in some countries [20, 21, 86], will result in lives lost and other far-reaching negative consequences for infected individuals and the broader community. The recent increases in IMD cases highlight the importance of vaccination programs and the need to be proactive during this post-pandemic era. Experts have thus called upon policymakers to implement preventive vaccination programs to provide protection from these outcomes [17, 39].
Broader Context of Preventive Meningococcal Vaccination
The COVID-19 pandemic triggered a global reckoning surrounding disease control strategies. One key learning is the importance of a preparedness rather than a reactive approach to public health policy and prevention, with analyses underscoring the chronic underinvestment in healthcare infrastructure and lack of early and comprehensive virus containment measures as major contributors to poor pandemic outcomes [87–89].
Many meningococcal vaccination campaigns were implemented in response to increased IMD rates [13]; however, using a preparedness approach with vaccines that are well tolerated and effective during times of IMD resurgence should be considered from a disease and case minimization context. Another broader consideration in meningococcal vaccination program implementation is that the programs are an important component of achieving the WHO’s Defeating Meningitis by 2030 Global Roadmap, which includes the goals of eliminating bacterial meningitis epidemics, reducing vaccine-preventable bacterial meningitis cases by 50% and deaths by 70%, reducing disability, and improving QoL after meningitis due to any cause [12].
The results discussed here do not consider the effect of COVID-19 on IMD epidemiology due to underlying uncertainties in disease unpredictability. Estimating the epidemiologic implications of COVID-19 for the level and future trajectory of IMD should be considered at least at the regional level; however, current seroepidemiology to guide these models is unavailable. Future work should consider evaluations of post-pandemic catch-up meningococcal vaccination options, including vaccination programs that may have improved following the pandemic.
Conclusions
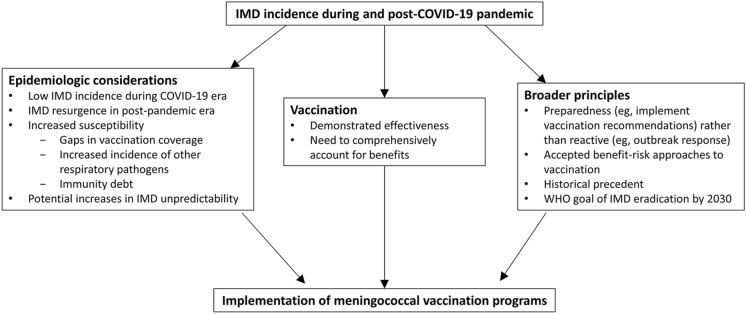
The resurgence of IMD incidence in some countries following relaxation of physical distancing and lockdown restriction measures implemented due to the COVID-19 pandemic presents a critical opportunity for implementation of meningococcal vaccination programs. Figure 2 reviews the manifold arguments supporting this conviction. Evidence suggests that IMD incidence in the post-pandemic era has increased and exceeded pre-pandemic levels in some countries, with added concerns including increased susceptibility because of vaccination coverage gaps, increased incidence of other respiratory pathogens, immunity debt from lockdown restrictions, and increased IMD epidemiologic variability. Vaccines targeting the ACWY and B serogroups are widely available and demonstrably effective in many global regions. Given the often devastating nature of IMD, the full range of benefits of these vaccines, including the variant control value of meningitis vaccination, should be considered in health technology assessments. However, vaccines have wide-ranging benefits that are rarely accurately quantified and not captured in implementation policy decisions. Given that traditional cost-effectiveness analyses of vaccination programs may have a limited role in individual country recommendations for IMD vaccination, in part because these traditional evaluations lack broader value assessments of vaccines, analyses that consider the broad benefits of vaccines are needed. Implementation of meningococcal vaccination programs in the current IMD climate also appeals to broader healthcare principles, including preparedness rather than reactive approaches, generally accepted benefit–risk approaches to vaccination, historical precedent, and the WHO goal of defeating meningitis by 2030.
Fig. 2.
Summary of arguments supporting implementation of meningococcal vaccination programs in the context of IMD incidence in the COVID-19 pandemic and post-pandemic eras. IMD invasive meningococcal disease, WHO World Health Organization
Countries must act swiftly to bolster existing meningococcal vaccination strategies to provide broad coverage across age groups and serogroups. Ultimately, implementation of comprehensive meningococcal vaccination programs is necessary to prepare for IMD incidence fluctuations in the post-pandemic era, as demonstrated by the increases in IMD incidence in some countries following relaxation of the COVID-19 pandemic control measures.
Acknowledgments
Medical Writing/Editorial Assistance.
Editorial/medical writing support was provided by Judith Kandel, PhD, of ICON (Blue Bell, PA, USA) and was funded by Pfizer Inc.
Author Contributions
All authors contributed to the study conception, design, and methodology. Katharina Schley contributed to formal analysis and investigation, resources, and data curation. Supervision was performed by Apostolos Charos and Paul Balmer. Funding acquisition was performed by Apostolos Charos, Katharina Schley, Jamie Findlow, and Paul Balmer. All authors contributed to drafting and critical revision of the manuscript and have read and approved the final version for submission and publication.
Funding
This study and the Rapid Service Fee were sponsored by Pfizer Inc.
Data availability
This article is based on published literature and therefore does not contain any applicable data sets.
Declarations
Conflict of Interest
Marco A.P. Safadi has received research grants and consultancy fees from Pfizer, GlaxoSmithKline, AstraZeneca, Janssen, and Sanofi Pasteur. David M. Salisbury has received consultancy fees from Pfizer, GlaxoSmithKline, AstraZeneca, Janssen, and Sanofi Pasteur. Paolo Bonanni has received research grants and consultancy fees from Pfizer, GlaxoSmithKline, AstraZeneca, Janssen, Sanofi Pasteur, MSD, Seqirus, and Moderna. Federico Martinón-Torres has received honoraria from GSK group of companies, Pfizer Inc, Sanofi, MSD, Seqirus, Biofabri, and Janssen for taking part in advisory boards and expert meetings and for acting as a speaker in congresses outside the scope of the submitted work. He has also acted as principal investigator in randomized controlled trials of the aforementioned companies and Ablynx, Gilead, Regeneron, Roche, Abbott, Novavax, and MedImmune, with honoraria paid to his institution. Peter C. Richmond’s institution has received research grants and consultancy fees for participation in scientific advisory boards from Pfizer, GlaxoSmithKline, Sanofi, and Janssen. Katharina Schley, Apostolos Charos, Paul Balmer, and Jamie Findlow are employees of Pfizer and may hold stock or stock options. David E. Bloom has worked on research grants or received travel support or honoraria from Pfizer, Merck, GSK, Moderna, Bavarian Nordic, Janssen, and Sanofi.
Ethical Approval
This article is based on previously conducted studies and does not contain any new data from studies with human participants or animals performed by any of the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dwilow R, Fanella S. Invasive meningococcal disease in the 21st century—an update for the clinician. Curr Neurol Neurosci Rep. 2015;15:2. doi: 10.1007/s11910-015-0524-6. [DOI] [PubMed] [Google Scholar]
- 2.Thompson MJ, Ninis N, Perera R, et al. Clinical recognition of meningococcal disease in children and adolescents. Lancet. 2006;367:397–403. doi: 10.1016/S0140-6736(06)67932-4. [DOI] [PubMed] [Google Scholar]
- 3.Wang B, Santoreneos R, Giles L, Haji Ali Afzali H, Marshall H. Case fatality rates of invasive meningococcal disease by serogroup and age: a systematic review and meta-analysis. Vaccine. 2019;37:2768–82. doi: 10.1016/j.vaccine.2019.04.020. [DOI] [PubMed] [Google Scholar]
- 4.Olbrich KJ, Muller D, Schumacher S, et al. Systematic review of invasive meningococcal disease: sequelae and quality of life impact on patients and their caregivers. Infect Dis Ther. 2018;7:421–438. doi: 10.1007/s40121-018-0213-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Acevedo R, Bai X, Borrow R, et al. The Global Meningococcal Initiative meeting on prevention of meningococcal disease worldwide: epidemiology, surveillance, hypervirulent strains, antibiotic resistance and high-risk populations. Expert Rev Vaccines. 2019;18:15–30. doi: 10.1080/14760584.2019.1557520. [DOI] [PubMed] [Google Scholar]
- 6.Soumahoro L, Abitbol V, Vicic N, Bekkat-Berkani R, Safadi MAP. Meningococcal disease outbreaks: a moving target and a case for routine preventative vaccination. Infect Dis Ther. 2021;10:1949–1988. doi: 10.1007/s40121-021-00499-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harrison LH, Jolley KA, Shutt KA, et al. Antigenic shift and increased incidence of meningococcal disease. J Infect Dis. 2006;193:1266–1274. doi: 10.1086/501371. [DOI] [PubMed] [Google Scholar]
- 8.Swartley JS, Marfin AA, Edupuganti S, et al. Capsule switching of Neisseria meningitidis. Proc Natl Acad Sci USA. 1997;94:271–276. doi: 10.1073/pnas.94.1.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tzeng YL, Stephens DS. A narrative review of the W, X, Y, E, and NG of meningococcal disease: emerging capsular groups, pathotypes, and global control. Microorganisms. 2021;9:519. doi: 10.3390/microorganisms9030519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miller E, Salisbury D, Ramsay M. Planning, registration, and implementation of an immunisation campaign against meningococcal serogroup C disease in the UK: a success story. Vaccine. 2001;20:S58–67. doi: 10.1016/S0264-410X(01)00299-7. [DOI] [PubMed] [Google Scholar]
- 11.Knol MJ, Hahne SJM, Lucidarme J, et al. Temporal associations between national outbreaks of meningococcal serogroup W and C disease in the Netherlands and England: an observational cohort study. Lancet Public Health. 2017;2:e473–e482. doi: 10.1016/S2468-2667(17)30157-3. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization. Defeating meningitis by 2030: a global road map. Jun 24, 2021. Available at: https://www.who.int/publications/i/item/9789240026407. Accessed 21 Dec 2022.
- 13.Parikh SR, Campbell H, Bettinger JA, et al. The everchanging epidemiology of meningococcal disease worldwide and the potential for prevention through vaccination. J Infect. 2020;81:483–498. doi: 10.1016/j.jinf.2020.05.079. [DOI] [PubMed] [Google Scholar]
- 14.Burman C, Serra L, Nuttens C, et al. Meningococcal disease in adolescents and young adults: a review of the rationale for prevention through vaccination. Hum Vaccin Immunother. 2019;15:459–469. doi: 10.1080/21645515.2018.1528831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martinon-Torres F, Taha MK, Knuf M, et al. Evolving strategies for meningococcal vaccination in Europe: overview and key determinants for current and future considerations. Pathog Glob Health. 2022;116:85–98. doi: 10.1080/20477724.2021.1972663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brueggemann AB, Jansen van Rensburg MJ, Shaw D, et al. Changes in the incidence of invasive disease due to Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria meningitidis during the COVID-19 pandemic in 26 countries and territories in the Invasive Respiratory Infection Surveillance Initiative: a prospective analysis of surveillance data. Lancet Digit Health. 2021;3:e360–70. doi: 10.1016/S2589-7500(21)00077-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cohen R, Ashman M, Taha MK, et al. Pediatric Infectious Disease Group (GPIP) position paper on the immune debt of the COVID-19 pandemic in childhood, how can we fill the immunity gap? Infect Dis Now. 2021;51:418–423. doi: 10.1016/j.idnow.2021.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.UNICEF. COVID-19 pandemic leads to major backsliding on childhood vaccinations, new WHO, UNICEF data shows. July 15, 2021. Available at: https://www.unicef.org/press-releases/covid-19-pandemic-leads-major-backsliding-childhood-vaccinations-new-who-unicef-data. Accessed 21 Dec 2022.
- 19.Alderson MR, Arkwright PD, Bai X, et al. Surveillance and control of meningococcal disease in the COVID-19 era: a Global Meningococcal Initiative review. J Infect. 2022;84:289–296. doi: 10.1016/j.jinf.2021.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Clark SA, Campbell H, Mensah AA, et al. An increase in group B invasive meningococcal disease among adolescents and young adults in England following easing of COVID-19 containment measures. SSRN Electron J. 2022 doi: 10.2139/ssrn.3998164. [DOI] [Google Scholar]
- 21.Santé publique France. [Epidemiological situation of invasive meningococcal infections in France. Update as of December 31, 2022]. Available at: https://www.santepubliquefrance.fr/maladies-et-traumatismes/maladies-a-prevention-vaccinale/infections-invasives-a-meningocoque/documents/bulletin-national2/situation-epidemiologique-des-infections-invasives-a-meningocoque-en-france.-point-au-31-decembre-2022#:~:text=Avec%2084%20cas%20d'IIM,et%20mars%20selon%20la%20saison. Accessed 1 Mar 2023.
- 22.Han E, Tan MMJ, Turk E, et al. Lessons learnt from easing COVID-19 restrictions: an analysis of countries and regions in Asia Pacific and Europe. Lancet. 2020;396:1525–1534. doi: 10.1016/S0140-6736(20)32007-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.European Centre for Disease Prevention and Control. Meningococcal disease: recommended vaccinations. Available at: https://vaccine-schedule.ecdc.europa.eu/Scheduler/ByDisease?SelectedDiseaseId=48&SelectedCountryIdByDisease=-1. Accessed 21 Dec 2022.
- 24.Jolley KA, Bray JE, Maiden MCJ. Open-access bacterial population genomics: BIGSdb software, the PubMLST.org website and their applications. Wellcome Open Res. 2018;3:124–8. doi: 10.12688/wellcomeopenres.14826.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aparecido Nunes A, De De Jesus Lopes Abreu A, Cintra O, et al. Meningococcal disease epidemiology in Brazil (2005–2018) and impact of MenC vaccination. Vaccine. 2021;39:605–16. doi: 10.1016/j.vaccine.2020.11.067. [DOI] [PubMed] [Google Scholar]
- 26.Graña MG, Cavada G, Vasquez M, et al. Modeling the public health impact of different meningococcal vaccination strategies with 4CMenB and MenACWY versus the current toddler MenACWY National Immunization Program in Chile. Hum Vaccin Immunother. 2021;17:5603–5613. doi: 10.1080/21645515.2021.1996808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McMillan M, Wang B, Koehler AP, Sullivan TR, Marshall HS. Impact of meningococcal B vaccine on invasive meningococcal disease in adolescents. Clin Infect Dis. 2021;73:e233–e237. doi: 10.1093/cid/ciaa1636. [DOI] [PubMed] [Google Scholar]
- 28.Rubis A. Epidemiology of meningococcal disease in the United States. Presented at: Advisory Committee on Immunization Practices Meeting, February 23, 2023; Atlanta, GA, USA.
- 29.Ministère de la Santé et de la Prévention. Calendrier des vaccinations et recommandations vaccinales 2023. Available at: https://sante.gouv.fr/IMG/pdf/calendrier_vaccinal_maj-juin23.pdf. Accessed 14 Jun 2023.
- 30.Haute Autorité de Santé. Stratégie de vaccination pour la prévention des infections invasives à méningocoques : Le sérogroupe B et la place de BEXSERO®. Available at: https://www.has-sante.fr/jcms/p_3066921/fr/strategie-de-vaccination-pour-la-prevention-des-infections-invasives-a-meningocoques-le-serogroupe-b-et-la-place-de-bexsero#:~:text=Depuis%202013%2C%20l'utilisation%20de,%2C%20%C3%A9pid%C3%A9mie%2C%20hyperend%C3%A9mie%20localis%C3%A9e. Accessed 14 Jun 2023.
- 31.Stefanelli P, Fazio C, Vacca P, et al. An outbreak of severe invasive meningococcal disease due to a capsular switched Neisseria meningitidis hypervirulent strain B:cc11. Clin Microbiol Infect. 2019;25:111.e1–e4. doi: 10.1016/j.cmi.2018.07.014. [DOI] [PubMed] [Google Scholar]
- 32.Outbreak News Today. Meningococcal disease outbreak in São Paulo, Health officials reinforce importance of vaccination. Available at: http://outbreaknewstoday.com/meningococcal-disease-outbreak-in-sao-paulo-health-officials-reinforce-importance-of-vaccination-61531/. Accessed 2 Mar 2023.
- 33.US Centers for Disease Control and Prevention. Meningococcal disease outbreak among gay, bisexual men in Florida, 2021–23. Available at: https://www.cdc.gov/meningococcal/outbreaks/FL2022.html. Accessed 12 Sep 2023.
- 34.Okonji OC, Rackimuthu S, Gangat SA, et al. Meningitis during COVID -19 pandemic in the Democratic Republic of Congo: a call for concern. Clin Epidemiol Glob Health. 2022;13:100955. doi: 10.1016/j.cegh.2021.100955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Neal KR, Nguyen-Van-Tam JS, Jeffrey N, et al. Changing carriage rate of Neisseria meningitidis among university students during the first week of term: cross sectional study. BMJ. 2000;320:846–849. doi: 10.1136/bmj.320.7238.846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Choi H, Lee HM, Lee W, et al. Longitudinal study of meningococcal carriage rates in university entrants living in a dormitory in South Korea. PLoS ONE. 2021;16:e0244716. doi: 10.1371/journal.pone.0244716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McMillan M, Walters L, Mark T, et al. B Part of It study: a longitudinal study to assess carriage of Neisseria meningitidis in first year university students in South Australia. Hum Vaccin Immunother. 2019;15:987–994. doi: 10.1080/21645515.2018.1551672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Watle SV, Caugant DA, Tunheim G, et al. Meningococcal carriage in Norwegian teenagers: strain characterisation and assessment of risk factors. Epidemiol Infect. 2020;148:e80. doi: 10.1017/S0950268820000734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cohen R, Pettoello-Mantovani M, Somekh E, Levy C. European pediatric societies call for an implementation of regular vaccination programs to contrast the immunity debt associated to coronavirus disease–2019 pandemic in children. J Pediatr. 2022;242:260–1.e3. doi: 10.1016/j.jpeds.2021.11.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Billard MN, Bont LJ. Quantifying the RSV immunity debt following COVID-19: a public health matter. Lancet Infect Dis. 2023;23:3–5. doi: 10.1016/S1473-3099(22)00544-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Santoli JM, Lindley MC, DeSilva MB, et al. Effects of the COVID-19 pandemic on routine pediatric vaccine ordering and administration—United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:591–593. doi: 10.15585/mmwr.mm6919e2. [DOI] [PubMed] [Google Scholar]
- 42.Chao CR, Xu L, Cannizzaro N, et al. Trends in HPV vaccine administration and HPV vaccine coverage in children by race/ethnicity and socioeconomic status during the COVID-19 pandemic in an integrated health care system in California. Vaccine. 2022;40:6575–6580. doi: 10.1016/j.vaccine.2022.09.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Taine M, Offredo L, Drouin J, et al. Mandatory infant vaccinations in France during the COVID-19 pandemic in 2020. Front Pediatr. 2021;9:666848. doi: 10.3389/fped.2021.666848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.GlaxoSmithKline. Half of parents surveyed either cancelled or delayed their child’s scheduled meningitis vaccination during the COVID-19 pandemic – GSK survey shows. March 21, 2021. Available at: https://www.gsk.com/en-gb/media/press-releases/half-of-parents-surveyed-either-cancelled-or-delayed-their-child-s-scheduled-meningitis-vaccination-during-the-covid-19-pandemic-gsk-survey-shows-1/. Accessed 21 Dec 2022.
- 45.Foley DA, Yeoh DK, Minney-Smith CA, et al. The interseasonal resurgence of respiratory syncytial virus in Australian children following the reduction of coronavirus disease 2019-related public health measures. Clin Infect Dis. 2021;73:e2829–e2830. doi: 10.1093/cid/ciaa1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Delestrain C, Danis K, Hau I, et al. Impact of COVID-19 social distancing on viral infection in France: a delayed outbreak of RSV. Pediatr Pulmonol. 2021;56:3669–3673. doi: 10.1002/ppul.25644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Olsen SJ, Winn AK, Budd AP, et al. Changes in influenza and other respiratory virus activity during the COVID-19 pandemic—United States, 2020–2021. MMWR Morb Mortal Wkly Rep. 2021;70:1013–1019. doi: 10.15585/mmwr.mm7029a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Agha R, Avner JR. Delayed seasonal RSV surge observed during the COVID-19 pandemic. Pediatrics. 2021;148:e2021052089. doi: 10.1542/peds.2021-052089. [DOI] [PubMed] [Google Scholar]
- 49.Bertran M, Amin-Chowdhury Z, Sheppard CL, et al. Increased incidence of invasive pneumococcal disease among children after COVID-19 pandemic, England. Emerg Infect Dis. 2022;28:1669–1672. doi: 10.3201/eid2808.220304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hatter L, Eathorne A, Hills T, Bruce P, Beasley R. Respiratory syncytial virus: paying the immunity debt with interest. Lancet Child Adolesc Health. 2021;5:e44–e45. doi: 10.1016/S2352-4642(21)00333-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Brundage JF. Interactions between influenza and bacterial respiratory pathogens: implications for pandemic preparedness. Lancet Infect Dis. 2006;6:303–312. doi: 10.1016/S1473-3099(06)70466-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Trotter CL, Lingani C, Fernandez K, et al. Impact of MenAfriVac in nine countries of the African meningitis belt, 2010–15: an analysis of surveillance data. Lancet Infect Dis. 2017;17:867–872. doi: 10.1016/S1473-3099(17)30301-8. [DOI] [PubMed] [Google Scholar]
- 53.Gray SJ, Trotter CL, Ramsay ME, et al. Epidemiology of meningococcal disease in England and Wales 1993/94 to 2003/04: contribution and experiences of the Meningococcal Reference Unit. J Med Microbiol. 2006;55:887–896. doi: 10.1099/jmm.0.46288-0. [DOI] [PubMed] [Google Scholar]
- 54.UK Health Security Agency. Meningococcal disease: laboratory-confirmed cases in England in 2020 to 2021. Available at: https://www.gov.uk/government/publications/meningococcal-disease-laboratory-confirmed-cases-in-england-in-2020-to-2021. Accessed 12 Sep 2023.
- 55.Huang L, Mauskopf J, Farkouh R, Masaquel C. Use of cost-effectiveness analyses for decisions about vaccination programs for meningococcal disease in the United States, United Kingdom, the Netherlands, and Canada. Expert Rev Vaccines. 2021;20:59–72. doi: 10.1080/14760584.2021.1878030. [DOI] [PubMed] [Google Scholar]
- 56.Carroll S, Rojas AJ, Glenngård AH, Marin C. Vaccination: short- to long-term benefits from investment. J Mark Access Health Policy. 2015 doi: 10.3402/jmahp.v3.27279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Campbell H, Andrews N, Parikh SR, et al. Impact of an adolescent meningococcal ACWY immunisation programme to control a national outbreak of group W meningococcal disease in England: a national surveillance and modelling study. Lancet Child Adolesc Health. 2022;6:96–105. doi: 10.1016/S2352-4642(21)00335-7. [DOI] [PubMed] [Google Scholar]
- 58.Ohm M, Hahne SJM, van der Ende A, et al. Vaccine impact and effectiveness of meningococcal serogroup ACWY conjugate vaccine implementation in the Netherlands: a nationwide surveillance study. Clin Infect Dis. 2022;74:2173–2180. doi: 10.1093/cid/ciab791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Villena R, Valenzuela MT, Bastias M, Santolaya ME. Meningococcal invasive disease by serogroup W and use of ACWY conjugate vaccines as control strategy in Chile. Vaccine. 2019;37:6915–6921. doi: 10.1016/j.vaccine.2019.09.050. [DOI] [PubMed] [Google Scholar]
- 60.Instituto de Salud Publica (Chile). Informe de Resultados de Vigilancia de Laboratorio: Enfermedad Invasora Neisseria meningitidis 2020. Available at: https://www.ispch.cl/wp-content/uploads/2021/02/Informe-Neisseria-meningitidis-SE-1-53-2020-v1-1.pdf. Accessed 20 May 2022.
- 61.Nwogu IB, Jones M, Langley T. Economic evaluation of meningococcal serogroup B (MenB) vaccines: a systematic review. Vaccine. 2021;39:2201–2213. doi: 10.1016/j.vaccine.2021.02.049. [DOI] [PubMed] [Google Scholar]
- 62.Christensen H, Al-Janabi H, Levy P, et al. Economic evaluation of meningococcal vaccines: considerations for the future. Eur J Health Econ. 2020;21:297–309. doi: 10.1007/s10198-019-01129-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gras-Le Guen C, Vignier N, Kochert F, et al. Why should the meningococcal B vaccine be recommended, and therefore reimbursed, for infants in France? Infect Dis Now. 2021;51:407–409. doi: 10.1016/j.idnow.2021.05.001. [DOI] [PubMed] [Google Scholar]
- 64.Stawasz A, Huang L, Kirby P, Bloom D. Health technology assessment for vaccines against rare, severe infections: properly accounting for serogroup B meningococcal vaccination’s full social and economic benefits. Front Public Health. 2020;8:261. doi: 10.3389/fpubh.2020.00261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Beck E, Klint J, Neine M, Garcia S, Meszaros K. Cost-effectiveness of 4CMenB infant vaccination in England: a comprehensive valuation considering the broad impact of serogroup B invasive meningococcal disease. Value Health. 2021;24:91–104. doi: 10.1016/j.jval.2020.09.004. [DOI] [PubMed] [Google Scholar]
- 66.Scholz S, Schwarz M, Beck E, et al. Public health impact and cost-effectiveness analysis of routine infant 4CMenB vaccination in Germany to prevent serogroup B invasive meningococcal disease. Infect Dis Ther. 2022;11:367–387. doi: 10.1007/s40121-021-00573-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Shen J, Begum N, Ruiz-Garcia Y, et al. Range of invasive meningococcal disease sequelae and health economic application—a systematic and clinical review. BMC Public Health. 2022;22:1078. doi: 10.1186/s12889-022-13342-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bloom DE. The value of vaccination. In: Curtis N, Finn A, Pollard AJ, editors. Hot topics in infection and immunity in children VII. Advances in experimental medicine and biology. New York: Springer; 2011. pp. 1–8. [Google Scholar]
- 69.Martinón-Torres F. Deciphering the burden of meningococcal disease: conventional and under-recognized elements. J Adolesc Health. 2016;59:S12–20. doi: 10.1016/j.jadohealth.2016.03.041. [DOI] [PubMed] [Google Scholar]
- 70.Gessner BD, Kaslow D, Louis J, et al. Estimating the full public health value of vaccination. Vaccine. 2017;35:6255–6263. doi: 10.1016/j.vaccine.2017.09.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bloom DE, Brenzel L, Cadarette D, Sullivan J. Moving beyond traditional valuation of vaccination: needs and opportunities. Vaccine. 2017;35:A29–A35. doi: 10.1016/j.vaccine.2016.12.001. [DOI] [PubMed] [Google Scholar]
- 72.Bell E, Neri M, Steuten L. Towards a broader assessment of value in vaccines: the BRAVE way forward. Appl Health Econ Health Policy. 2022;20:105–117. doi: 10.1007/s40258-021-00683-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bloom DE, Cadarette D, Ferranna M. The societal value of vaccination in the age of COVID-19. Am J Public Health. 2021;111:1049–1054. doi: 10.2105/AJPH.2020.306114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jit M, Hutubessy R, Png ME, et al. The broader economic impact of vaccination: reviewing and appraising the strength of evidence. BMC Med. 2015;13:209. doi: 10.1186/s12916-015-0446-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bloom DE, Fan VY, Sevilla JP. The broad socioeconomic benefits of vaccination. Sci Transl Med. 2018;10:eaaj2345. doi: 10.1126/scitranslmed.aaj2345. [DOI] [PubMed] [Google Scholar]
- 76.Pingali C, Yankey D, Elam-Evans LD, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years—United States, 2020. MMWR Morb Mortal Wkly Rep. 2021;70:1183–1190. doi: 10.15585/mmwr.mm7035a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bart SM, Eberhart M, Feemster K. Impact of a Category B recommendation: meningococcal B (MenB) vaccine uptake among adolescents in Philadelphia County. Presented at: Pediatric Academic Societies, May 5–8, 2018; Toronto, ON, Canada.
- 78.Lancet Commission on COVID-19 Vaccines and Therapeutics Task Force Members Urgent needs of low-income and middle-income countries for COVID-19 vaccines and therapeutics. Lancet. 2021;397:562–4. doi: 10.1016/S0140-6736(21)00242-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Teresa Aguado M, Barratt J, Beard JR, et al. Report on WHO meeting on immunization in older adults: Geneva, Switzerland, 22–23 March 2017. Vaccine. 2018;36:921–931. doi: 10.1016/j.vaccine.2017.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sriudomporn S, Sim SY, Mak J, Brenzel L, Patenaude BN. Financing and funding gap for 16 vaccines across 94 low- and middle-income countries, 2011–30. Health Aff (Millwood) 2023;42:94–104. doi: 10.1377/hlthaff.2022.00343. [DOI] [PubMed] [Google Scholar]
- 81.Ducomble T, Gignoux E. Learning from a massive epidemic: measles in DRC. Lancet Infect Dis. 2020;20:542. doi: 10.1016/S1473-3099(20)30265-6. [DOI] [PubMed] [Google Scholar]
- 82.Sim SY, Jit M, Constenla D, Peters DH, Hutubessy RCW. A scoping review of investment cases for vaccines and immunization programs. Value Health. 2019;22:942–952. doi: 10.1016/j.jval.2019.04.002. [DOI] [PubMed] [Google Scholar]
- 83.Chung GS, Hutton DW. Epidemiological impact and cost-effectiveness of universal meningitis B vaccination among college students prior to college entry. PLoS ONE. 2020;15:e0239926. doi: 10.1371/journal.pone.0239926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wang B, Santoreneos R, Afzali H, Giles L, Marshall H. Costs of invasive meningococcal disease: a global systematic review. Pharmacoeconomics. 2018;36:1201–1222. doi: 10.1007/s40273-018-0679-5. [DOI] [PubMed] [Google Scholar]
- 85.Ackerson B, An J, Sy LS, et al. Cost of hospitalization associated with respiratory syncytial virus infection versus influenza infection in hospitalized older adults. J Infect Dis. 2020;222:962–966. doi: 10.1093/infdis/jiaa183. [DOI] [PubMed] [Google Scholar]
- 86.Middeldorp M, van Lier A, van der Maas N, et al. Short term impact of the COVID-19 pandemic on incidence of vaccine preventable diseases and participation in routine infant vaccinations in the Netherlands in the period March-September 2020. Vaccine. 2021;39:1039–1043. doi: 10.1016/j.vaccine.2020.12.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Jinjarak Y, Ahmed R, Nair-Desai S, Xin W, Aizenman J. Accounting for global COVID-19 diffusion patterns, January-April 2020. Econ Disaster Clim Chang. 2020;4:515–559. doi: 10.1007/s41885-020-00071-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Maani N, Galea S. COVID-19 and underinvestment in the public health infrastructure of the United States. Milbank Q. 2020;98:250–259. doi: 10.1111/1468-0009.12463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Sagan A, Webb E, McKee M, et al. Health systems resilience during COVID-19: lessons for building back better [Health Policy Series 56]. World Health Organization; The European Observatory on Health Systems and Policies. Available at: https://apps.who.int/iris/bitstream/handle/10665/348493/9789289051873-eng.pdf?sequence=2. Accessed 21 Dec 2022. [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This article is based on published literature and therefore does not contain any applicable data sets.