Introduction
Sirenomelia or ‘Mermaid Syndrome’ is a rare congenital anomaly showing partial or complete fusion of lower limb bones. It is associated with oligohydramnios, renal agenesis, and incomplete development of the genitourinary system. Sirenomelia is often associated with thoracolumbar spinal anomalies, sacrococcygeal agenesis, genitourinary, and anorectal atresia. Mermaid syndrome, being a rare anomaly, is found in about 0.8–1 case/100,000 births with male predilection, with around 300 cases studied in the literature. Its aetiology is difficult to define, and this syndrome in itself is difficult to distinguish from caudal regression syndrome or VACTERL (vertebral anomalies, anal atresia, cardiac anomalies, tracheal anomalies, oesophageal atresia, renal agenesis, and limb deformities) [1, 2].
Case Report
Case 1
A 30-year primigravida, registered pregnancy, presented with anomaly scan of 19 weeks 5 days with bilateral renal agenesis, absent bladder, single lower limb, probability of fused femur, two leg bones, and anhydramnios. She had no significant medical or surgical history. This was a spontaneous conception with no history of diabetes mellitus. There was no history of drug intake. Her blood sugars in the present pregnancy were normal. On explaining the poor prognosis of the foetus, the couple opted for medical termination of pregnancy which was done with two doses of Tab. Misoprostol 400 µg given 4 h apart. The patient aborted en sac.
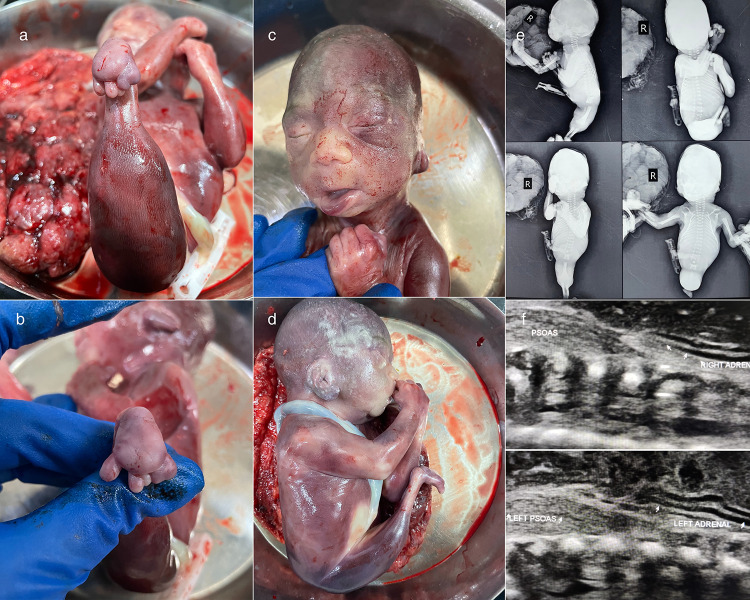
The foetus delivered had a single lower limb, with one foot and fused toes. There was a skeletal deformity at level of sacrum, no external genitalia were seen, thus sex could not be determined. The baby showed features of Potter facies with low set ears, prominent epicanthal folds, flattened nose, and recessed chin. These findings were consistent with bilateral renal agenesis and anhydramnios in the antenatal scan (Fig. 1).
Fig. 1.
a Single fused lower limb, b fused toes, c and d features of Potter facies, e fused femur and two unfused bones, and f bilateral renal agenesis and lying down adrenals
A babygram was done which showed a single femur and two lower limb bones which were unfused. The sacral bone was not formed completely, and the remaining pelvic bone was absent. The other bony structures were normal. A postnatal ultrasound examination of the foetus showed bilateral lying down adrenals with bilateral renal agenesis. The patient denied foetal autopsy. The patient was asked to follow up after 6 weeks, and an oral glucose tolerance test (OGTT) was done which was normal.
Case 2
A 20-year second gravida, previous normal vaginal delivery, 39 weeks of gestation was referred for intrauterine growth restriction, severe oligohydramnios. The patient had pain in abdomen and white per vaginal discharge for 1 day. Antenatal profile was incomplete with neither blood sugars nor detailed malformation scan.
The Doppler findings on referral were an estimated foetal weight less than 1st centile, low middle cerebral artery pulsatality index, suggestive of late-onset intrauterine growth restriction, severe oligohydramnios, and brain-sparing effect.
An emergency lower segment caesarean section was done for foetal distress. A 01.342-kg baby with Apgar score of 1/10 was born. The neonate was put on invasive ventilation and inotropes but succumbed on day 1 of life. External genitalia were absent, and a single lower limb was present. Anal opening was absent, and a spinal defect could be seen in lumbar region (Fig. 2). The patient denied an autopsy and further investigations of the neonate. The patient was followed up with an oral glucose tolerance test after 6 weeks which was normal.
Fig. 2.
a Fused lower limb with absent external genitalia and b absent anal opening
Discussion
Sirenomelia is a combination of congenital malformations such as fused lower limb, bilateral renal agenesis, and other genitourinary anomalies. It was first described by Rocheus in 1542. Some have deemed sironemelia a severe form of caudal regression syndrome [1]. Sirenomelia is shown to portray strong association with maternal diabetes mellitus though our cases did not have deranged blood sugar levels. It is theorized that the oxygen-free radicals due to maternal deranged sugars could be teratogenic. Exposure to teratogens, retinoic acid, and maternal age of 20 and greater than 40 years are known risk factors [3].
Foetus in case-1 showed features of Potter’s facies along with absent bilateral kidneys and absent liquor, suggestive of Potter’s syndrome. It occurs in the presence of Potter’s sequence with bilateral renal agenesis. Foetus in case-2 did not show these findings. Stocker and Heifetz classified sirenomelia into seven types by the degree of fusion of lower extremity bones. They took into consideration the presence or absence of femur, tibia, and fibula. According to this classification, the foetus in case-1 belongs to type V.
Even though the exact cause of mermaid syndrome is not known, two hypotheses of pathogenesis have been highlighted. The first is vascular steal hypothesis which implies that due to the limbs being fused, there is deficiency of blood supply, and nutrient deficiency leads to agenesis of midline structures which finally causes abnormal approximation of both lower limbs [1]. In the defective blastogenesis hypothesis, the primary defect is in the development of caudal mesoderm which is attributed to a teratogenic event occurring in the gastrulation stage. Such defect interferes with the formation of notochord, resulting in abnormal development of caudal structures. Recurrence has been noted in one family with two out of five children being affected in a report by Rudd and Kimek in 1990. Few cases of family history with anorectal and genitourinary malformation have been documented to be linked to sirenomelia. But evidence is conflicting with no consensus on recurrence rates [4].
Diabetes mellitus is associated with the development of multiple congenital malformations, including sirenomelia. Riazat et al. reported a grand multipara with gestational diabetes mellitus with poor control on insulin, at 38 weeks of gestation delivering a foetus of 02.43 kg with ambiguous genitalia, absent anal opening, and fused lower limbs with features of Potter facies. Her antenatal scan had severe oligohydramnios with absent left kidney and cystic dysplastic right kidney, cardiac malformations [2]. Diabetes, monozygotic twins, and teratogens such as lead, cocaine, tobacco, and maternal age less than 20 years have been reported to cause sirenomelia, but both of our cases did not have any identifiable risk factors [4].
Vasisht et al. presented a case of sirenomelia with the presence of congenital hydrocephalus. Antenatal scan corroborated the findings of foetal autopsy which showed bilateral dilatation of lateral ventricles with thinning of the cortex, hypoplastic lungs, dysplastic right kidney, and left renal agenesis [1]. Mohamud et al. described a case with twin gestation with one twin with sirenomelia. The literature has shown association with atrial and ventricular septal defects, neural tube defects, and holoprosencephaly [4].
Conclusion
Mermaid syndrome or sirenomelia is a rare congenital disorder with about 300 cases reported, about 14 coming from India. Being a disorder incompatible with life, ultrasonography and anomaly scan done in earlier gestation will aid in diagnosis. At later stages, oligohydramnios makes it a diagnostic dilemma. Women with a history and family history of genitourinary, anorectal malformations, and sirenomelia should undertake pre-conceptional counselling and register early in subsequent pregnancies and get ultrasound evaluation done. Diabetes is a well-documented risk factor, and women must be screened. Pre-conceptional counselling of overt diabetics with importance to glycosylated haemoglobin, good control of overt diabetes especially in early trimester is crucial. It is not a preventable disorder but early diagnosis through ultrasonography is a key to reduce both maternal and foetal morbidity.
Acknowledgement
Department of Radiology, Seth G S Medical College and KEM Hospital, Mumbai, India for the babygram and ultrasound images.
Declarations
Ethical Approval
All the authors declare that there are no personal or financial affiliations that have biased the case report. The ethical standards have been adhered to, and patient confidentiality has been maintained. Informed consent has been obtained from the patients. The participants have consented to the submission of the case report to the journal.
Footnotes
Madhura D. Mandlik (MBBS) is a Registrar; Kimaya A. Mali (MBBS, DGO, DNB, DFP) is an Assistant Professor; Ananya Bora (MBBS, MD, DNB) is an Assistant Professor; and Niranjan M. Mayadeo (MBBS, DGO, MD, FCPS, DNB, DFP, DICOG, MNAMS) is an Ex-Professor and Head of Department.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Vasisht P, Madakshira MG, Kakkar N, et al. Tale of a mermaid. Indian J Pathol Microbiol. 2019;62(4):611–3. doi: 10.4103/IJPM.IJPM_668_18. [DOI] [PubMed] [Google Scholar]
- 2.Riazat MI, Kewlani B, Abujennah J, et al. Sirenomelia (mermaid syndrome): a rare congenital disorder. BMJ Case Rep [Internet]. 2019 Nov;12(11). Available from: https://pubmed.ncbi.nlm.nih.gov/31767602/ [DOI] [PMC free article] [PubMed]
- 3.Zeki Yaşar M, Yusuf AA, Hassan FM, et al. Mermaid syndrome: a case report in Somalia. Ann Med Surg. 2022;76:103533. doi: 10.1016/j.amsu.2022.103533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boer LL, Morava E, Klein WM, et al. Sirenomelia: a multi-systemic polytopic field defect with ongoing controversies. Birth Defects Res. 2017;109(10):791–804. doi: 10.1002/bdr2.1049. [DOI] [PubMed] [Google Scholar]