Abstract
Introduction
Technology to enhance hypertension management is increasingly used in primary care; however, it has not been evaluated in an Asian primary care setting. We aimed to understand the clinical impact and cost-effectiveness of a technology-enabled home blood pressure monitor when deployed in primary care, and patients’ perspectives about the technology.
Methods
A quasi-experimental cohort study was conducted in a polyclinic in Singapore. In total, 120 patients with hypertension were assigned to the telemonitoring intervention group. Patients received a home blood pressure device connected to the clinical care team's dashboard through a mobile gateway. Tele-consultations and nurse-led tele-support were carried out using established clinical protocols. In total, 120 patients assigned to the control group continued to receive usual care in the polyclinic. Clinical outcomes, cost-effectiveness, and patient satisfaction were measured 6 months after recruitment.
Results
In total, 217 patients completed 6 months of follow-up. Telemonitoring intervention patients had significantly increased odds of having controlled blood pressure by a factor of 2.69 (p = 0.01), with the greatest improvement in those whose blood pressure was uncontrolled at baseline (p < 0.05). The incremental cost-effectiveness ratios for all patients was S$23,935.14/quality-adjusted life year (<1 gross domestic product per capita), which was very cost-effective based on World Health Organization cost-effectiveness thresholds. There was greater satisfaction in telemonitoring intervention group relating to the convenience of recording and sharing blood pressure measurements with the health care team, consultation advice received, understanding by the health care team of their condition, and were more motivated to monitor their blood pressure.
Discussion
Telemonitoring with tele-consultation improved blood pressure control and was more cost-effective than usual care. Patients receiving telemonitoring intervention were also more motivated and satisfied with their care.
Keywords: Telemedicine, hypertension, blood pressure monitoring, cost-effectiveness, primary health care
Introduction
Hypertension is one of the most common chronic diseases managed by primary care physicians. 1 Hypertension leads to significant morbidity, mortality, and health care cost as it is a risk factor for many other chronic diseases such as ischemic heart disease, heart failure, stroke, and end-stage renal failure.2,3 Technology to aid and enhance the management of hypertension is increasingly used to meet rising demands on primary care systems.
The use of technology to enhance hypertension management in primary care has been evaluated in several settings with various telemedicine interventions. Telemonitoring can contribute to significant reductions in blood pressure (BP), decrease all-cause and hypertension-related hospitalizations, reduce all-cause mortality, cost, and improve quality of life (QoL). 4 Additionally, technology-enabled BP self-monitoring interventions have shown better BP control outcomes with the addition of nurse-led tele-support, physician intervention and medication review (i.e. tele-treatment).4–6 In a recent study, intensive home BP telemonitoring intervention (TI) with pharmacist management showed a reduction in BP with sustained effects of up to 24 months. 7 However, few studies have combined BP telemonitoring with tele-consultation or reported cost-effectiveness analysis.
The effect of technology-enabled hypertension management has not been evaluated in an Asian primary care setting. This trial aimed to understand the clinical impact and cost-effectiveness of a technology-enabled home BP monitoring system with tele-consultation when deployed in the primary care setting, as well as the experiences and perspectives of patients about the technology.
Methods
Design
This study was an open-label, parallel, quasi-experimental study conducted in one polyclinic where patients are cared for by teamlets, each comprising two family physicians, one care manager (CM) who is a nurse trained in chronic disease management, and one care coordinator (CC) who is a layperson trained in care coordination.
Participants
We included patients with hypertension or hypertension with hyperlipidemia, aged ≥21 years, and who were able and willing to use telemedicine devices. Patients with a history of type 2 diabetes mellitus or chronic kidney disease stage III or worse were excluded. Patients under the care of one teamlet were allocated to the TI group, while those under the care of the other teamlet were allocated to the usual care (UC) group. The target sample size was 120 patients in each group. Eligible patients who expressed interest during their consultations were referred to the research coordinator who explained the study to them and obtained written informed consent. Participants were followed up for 6 months, and the duration of the whole trial was 1 year.
Interventions
TI group: patient-led telemonitoring for BP levels
A Bluetooth-enabled home BP monitor (TaiDoc Technology FORA P20b Blood Pressure Monitoring System) and mobile data network connecting gateway device (Phicomm C230) were loaned to each participant. Both the BP monitor and gateway device were registered with the Singapore Health Sciences Authority and approved for local use by the Infocomm Media Development Authority, respectively. Participants were asked to monitor their BP at least once weekly using the devices, which automatically uploaded measured BP readings to a web-based portal for collation and prioritized readings on a dashboard for clinical management. Tele-consultations and CM-led tele-support, including titration of medications over the phone, were carried out using established clinical protocols.
UC group: Usual care
Participants in the UC group continued to be followed up and managed as per usual clinical care, without additional BP TI.
Demographic data, patient service use in the preceding 6 months, patient's QoL using the five-level EQ-5D version (EQ-5D-5L), 8 and baseline office BP were collected upon enrolment and at 6 months for both groups. A satisfaction survey was included in the 6-month questionnaire to assess the acceptability of this intervention versus UC, patients' satisfaction with their care, consultations, convenience, and motivation to self-monitor BP.
Statistical analysis
The primary outcome measure was BP, including a difference in BP over time. Controlled BP was defined as <140/90 mm Hg, above which was deemed as uncontrolled. Descriptive statistics for mean BP at each time point, the difference in BP between time points, and the proportion of patients with controlled BP were recorded and differences were analyzed with Chi-square and analysis of variance (ANOVA) tests. Generalized estimating equations (GEEs) and linear regression models were used to assess differences in BP between baseline and 6 months, for the TI group relative to the UC group. Age at study enrolment, gender, and ethnicity were also included as covariates in adjusted models.
The secondary outcomes were QoL, cost-effectiveness, and patient satisfaction with the intervention. For economic evaluation, a visit was defined as hypertension-related as long as at least one hypertension-related service was engaged, even if the primary diagnosis for the visit was not hypertension. Direct medical cost for each participant was examined by extracting actual cost data using service codes for face-to-face (FF) consultations, tele-consultations, laboratory tests, and medications from the polyclinic's administrative and clinical databases. EQ-5D-5L scores were converted to utility values to generate quality-adjusted life years (QALYs). QALY over the half-year period after study recruitment for each participant was used as the outcome variable. The difference in QALYs between TI group and UC group was calculated using t-test, adjusting for baseline BP, age, gender, and ethnicity. The first incremental cost-effectiveness ratio (ICER) calculated was incremental cost over the incremental probability of having controlled BP status, and the second was the incremental cost over incremental QALY. Lastly, Chi-square analysis was used to test patient satisfaction (strongly agree vs. other responses) between TI and UC groups.
Statistical significance was set at p < 0.05. All statistical analyses were performed using STATA (Stata Statistical Software: Release 15. College Station, TX: StataCorp LP).
This study is reported according to the Consolidated Standards of Reporting Trial (CONSORT) guidelines.
Results
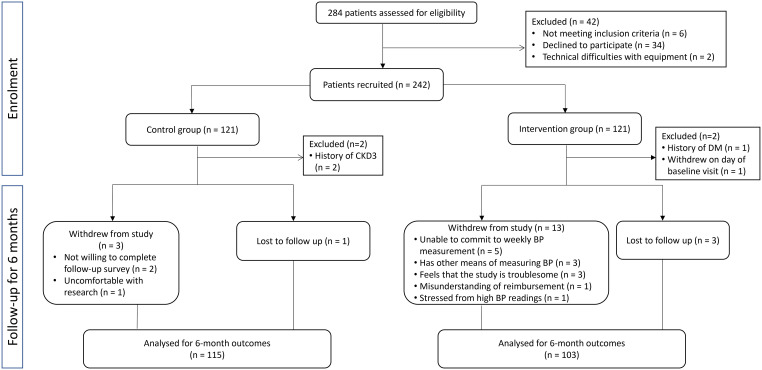
The study flow diagram is in Figure 1. Patient recruitment occurred from September 2018 to March 2019. Out of 284 patients approached and assessed for eligibility, 121 participants were recruited into UC and TI groups, respectively, with a final response rate of 85.2%. In total, 115 participants from the UC group and 103 participants from the TI group remained in the trial after 6 months (combined lost-to-follow-up and withdrawal rate of 9.9%). Among patients who withdrew from the study, those from the intervention group remained in the trial for a mean duration of 94.1 days (SD = 66.8 days, range = 17–163 days), while those from the control group remained in the trial for a mean duration of 185 days (SD = 2.6 days, range = 182–187 days). The final sample for primary outcome analysis was 102 patients due to the availability of office BP records.
Figure 1.
Consolidated Standards of Reporting Trial (CONSORT) flow diagram of participant recruitment.
The baseline characteristics of the study participants are shown in Table 1. Patients in the TI group were younger (56.3 vs. 59.9 years, p = 0.007). Patients recruited to the TI group had a higher baseline systolic BP (SBP) (135.0 vs. 130.7, p = 0.012) and diastolic BP (DBP) (78.7 vs. 72.8, p < 0.001). There was a greater proportion of patients with uncontrolled hypertension in the TI group compared to the UC group at baseline (39.5% vs. 17.7%, p < 0.001).
Table 1.
Participant baseline characteristics.
| UC (N = 119) | TI (N = 119) | p value | |
|---|---|---|---|
| Male, n(%) | 71(59.7) | 68(57.1) | 0.693 |
| Ethnicity, n(%) | 0.125 | ||
| Chinese | 102(85.7) | 103(86.6) | |
| Malay | 5(4.2) | 11(9.2) | |
| Indian | 7(5.9) | 4(3.4) | |
| Others | 5(4.2) | 1(0.8) | |
| Age, mean (SD), years | 59.9(10.6) | 56.3(9.8) | 0.007** |
| BMI, mean (SD), kg/m2 | 26.7(5.4) | 26.1(3.1) | 0.303 |
| Highest level of education, n(%) | 0.299 | ||
| Primary | 27(22.7) | 18(15.1) | |
| Secondary | 45(37.8) | 41(34.5) | |
| Pre-University | 22(18.5) | 30(25.2) | |
| Tertiary | 25(21.0) | 30(25.2) | |
| Type of housing, n(%) | 0.097 | ||
| Public housing 1–3 rooms | 36(30.3) | 26(22.0) | |
| Public housing 4–5 rooms and executive flat | 63(52.9) | 61(51.3) | |
| Private housing | 6(5.0) | 16(13.6) | |
| Condominiums | 14(11.8) | 15(12.7) | |
| Family history of CVD, n(%) | 94(79.0) | 89(74.8) | 0.442 |
BMI: body mass index; CVD: cardiovascular disease; SD: standard deviation; TI: telemonitoring intervention; UC: usual care.
**p < 0.01.
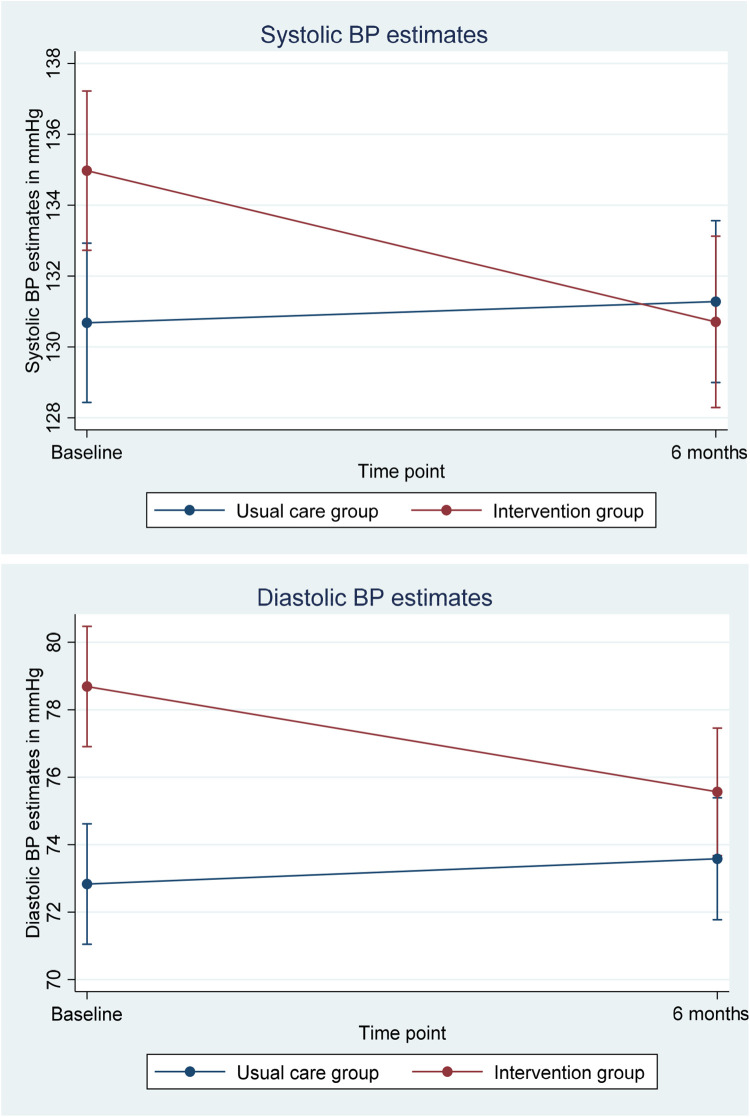
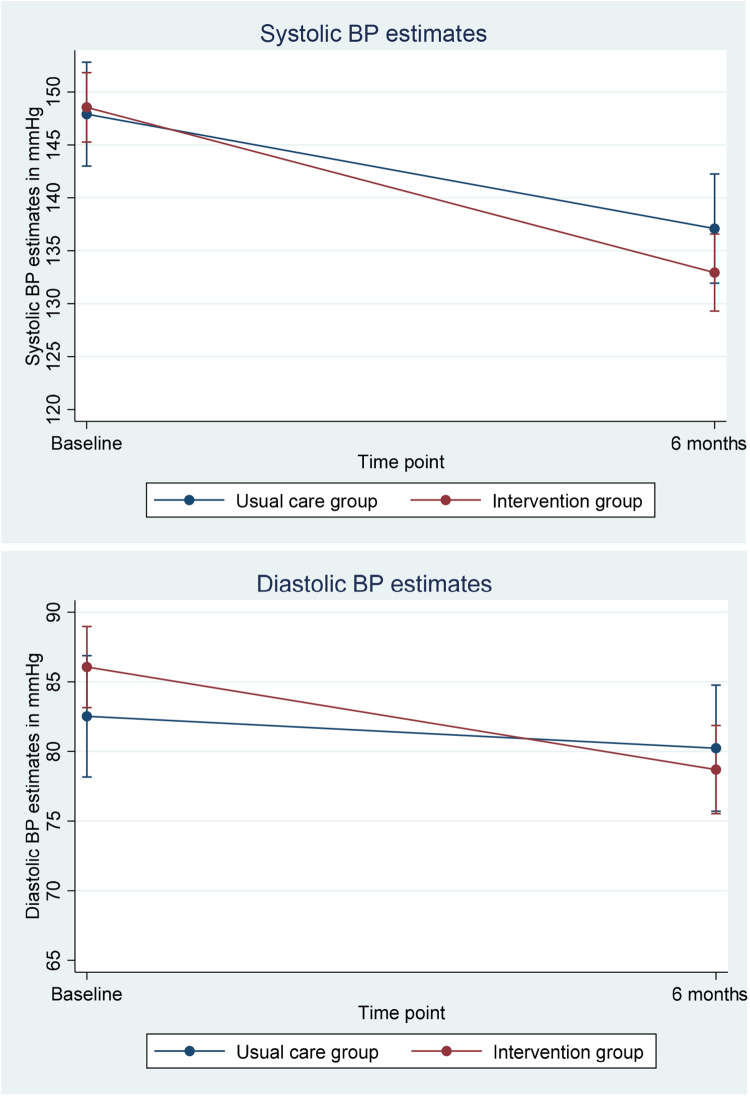
At 6 months of follow-up, there was no significant difference in SBP (130.4 vs. 131.2, p = 0.62) and DBP (75.1 vs. 73.6, p = 0.26) between the two groups (Figure 2). SBP and DBP over 6 months for patients with uncontrolled baseline BP (Figure 3). There was no difference in the proportion of patients with uncontrolled hypertension in the TI group compared to the UC group at 6 months of follow-up (23.5% vs. 21.7%, p = 0.75) (Table 2).
Figure 2.
Systolic BP and diastolic BP of UC and TI groups over 6 months. BP: blood pressure; UC: usual care; TI: telemonitoring intervention.
Figure 3.
Systolic and diastolic blood pressure (BP) over 6 months for patients with uncontrolled baseline BP.
Table 2.
Mean BP and proportion of patients with controlled versus uncontrolled BP at baseline and 6 months.
| UC (N = 115) | TI (N = 102) | p value | |
|---|---|---|---|
| Mean baseline BP | |||
| Systolic, mm Hg | 130.7 | 135.0 | 0.012* |
| Diastolic, mm Hg | 72.8 | 78.7 | <0.001*** |
| Uncontrolled, n(%) | 21(17.7) | 47(39.5) | |
| Controlled, n(%) | 98(82.4) | 72(60.5) | <0.001*** |
| Total | 119 | 119 | |
| Mean 6 months BP | |||
| Systolic, mm Hg | 131.2 | 130.4 | 0.621 |
| Diastolic, mm Hg | 73.6 | 75.1 | 0.260 |
| Uncontrolled, n(%) | 25(21.7) | 24(23.5) | |
| Controlled, n(%) | 90(78.3) | 78(76.5) | 0.753 |
BP: blood pressure; TI: telemonitoring intervention; UC: usual care.
*p < 0.05, ***p < 0.001.
GEE models showed that both SBP and DBP decreased significantly in the TI group over 6 months compared to the UC group. After adjusting for baseline characteristics, the beta coefficient for SBP in the TI group was 4.05 (p = 0.01) and 4.34 for DBP (p < 0.001).
There were significant differences in SBP and DBP at 6 months of follow-up after adjusting for differences in characteristics in both groups, favoring patients in the TI group. Using a linear regression model, we found statistically significant improvements for SBP (beta coefficient: 4.56, p = 0.03) and DBP (beta coefficient: 3.55, p = 0.009) for the TI group compared to the UC group after adjusting for age, gender, ethnicity, time in study, and baseline EQ-5D scores.
The improvement in BP outcomes was greatest among patients with uncontrolled BP at baseline. Among patients with uncontrolled BP at baseline, 60.5% had controlled BP by 6 months in the TI group compared to 52.6% in the UC group (p = 0.02) (Table 3). When controlled BP was analyzed as a binary variable, the adjusted GEE model showed that at the 6-month mark, those in the TI group were significantly more likely to have controlled BP with an odds ratio of 2.69 (95% CI = 1.27–5.73, p = 0.010).
Table 3.
Changes in BP control over 6 months.
| UC group, n(%) | ||||
|---|---|---|---|---|
| 6 months BP | p value | |||
| Controlled | Uncontrolled | |||
| Baseline BP | Controlled | 80(83.3) | 16(16.7) | |
| Uncontrolled | 10(52.6) | 9(47.4) | 0.327 | |
| TI group, n(%) | ||||
| 6 months BP | p value | |||
| Controlled | Uncontrolled | |||
| Baseline BP | Controlled | 55(85.9) | 9(14.1) | |
| Uncontrolled | 23(60.5) | 15(39.5) | 0.020* | |
BP: blood pressure; TI: telemonitoring intervention; UC: usual care.
*p < 0.05.
Economic evaluation
QALY was measured in both UC and TI groups at baseline and at 6 months. The mean score increased from 0.89 at baseline to 0.93 at 6 months follow-up in the UC group, and from 0.90 to 0.94 in the TI group. Regression adjusting for baseline utility measurement, SBP, and DBP showed that the QALY over the half-year intervention period was higher for the TI group by 0.002 (p = 0.571). However, the differences in measurements between the UC and TI groups were not significant.
The mean frequency of tele-consultations of the TI group was 1.7 tele-consults (SD = 1.35, range = 0–6). The number of FF consultations and tele-consultations, cost of laboratory tests and medications at baseline and at 6 months were compared for both groups in the comparison of the direct medical cost. The number of FF consultations were similar for the TI and UC groups, but there was significantly more (1.7 vs. 0.2) hypertension-related tele-consultations during the 6-month intervention period (p < 0.01) (Table 4).
Table 4.
Number of hypertension-related polyclinic visits.
| Time point | UC group (N = 115) | TI group (N = 103) | p value | Difference-in-differences |
|---|---|---|---|---|
| Hypertension-related visit: Tele-consultation (by nurses only) | ||||
| 6 months before intervention | 0 | 0 | 0.29† | |
| 6 months during intervention | 0.2 | 1.7 | 0.01* | |
| Difference | 0.2 | 1.7 | 1.5† | |
| p value | <0.01**† | <0.01**† | <0.01**† | |
| Hypertension-related visit: Face-to-face visit (with physician and/or nurse) | ||||
| 6 months before intervention | 2.5 | 2.5 | 0.95 | |
| 6 months during intervention | 3.2 | 3.6 | 0.11 | |
| Difference | 0.7 | 1.1 | 0.4 | |
| p value | <0.01** | <0.01** | 0.27 | |
| Hypertension-related visit: Both | ||||
| 6 months before intervention | 2.5 | 2.5 | 0.99 | |
| 6 months during intervention | 3.3 | 5.2 | <0.01** | |
| Difference | 0.8 | 2.7 | 1.9 | |
| p value | <0.01** | <0.01** | <0.01** | |
All p values were generated from Poisson regression, except for those labeled with the symbol “†” which were generated by transformed visit using log(visit + 1) with the standard t-test. TI: telemonitoring intervention; UC: usual care.
*p < 0.05, **p < 0.01.
Compared to the 6-month period before the intervention, the direct medical cost related to hypertension increased more for TI group (S$119.95) compared to UC group (S$96.97). Further analysis was done with generalized linear regression using gamma distribution and log-link controlling for age, gender, and ethnicity. The TI group had higher direct medical cost due to the intervention; however, it was not statistically significant. The higher direct medical cost in the TI group was mainly driven by cost from nurse-related visits, which showed a statistically significant difference compared to the UC group (+$18.17, p = 0.02). The cost of (a) tele-vital signs monitoring (VSM) subscription and (b) Bluetooth BP device were considered when calculating ICER. This cost applied to all the patients in TI group. Over the 6-month intervention period, the cost of tele-VSM was S$42 per patient and the cost of Bluetooth BP device was S$16.67 per patient.
Table 5 shows the ICER analysis using all patients; patients with controlled baseline BP and patients with uncontrolled baseline BP. The results suggest that the programme costs S$468.57 to prevent one incidence of uncontrolled BP. We assumed that Singapore's gross domestic product (GDP) per capita in 2018 was US$58,000 = S$78,000.9,10 As the ICERs for all patients, patients with controlled and uncontrolled BP, at baseline were S$23,935.14/QALY, S$24,973.08/QALY, and S$19,710.29/QALY, respectively (all <1 GDP per capita), TI was very cost-effective based on World Health Organization cost-effectiveness thresholds. 11
Table 5.
ICER analysis.
| All patients | Controlled baseline BP | Uncontrolled baseline BP | |
|---|---|---|---|
| Change in direct medical cost | S$88.56 | S$64.67 | S$134.03 |
| Change in BP status (measured by the difference in probability in preventing uncontrolled BP) | 0.189 | NA | NA |
| Change in QALY | 0.0037 | 0.0026 | 0.0068 |
| ICER | |||
| Change in direct medical cost/change in BP status | S$ 468.57/BP controlled | NA | NA |
| Change in direct medical cost/change in QALY | S$23,935.14/QALY | S$24,873.08/QALY | S$19,710.29/QALY |
BP: blood pressure; ICER: incremental cost-effectiveness ratio; NA: not available; QALY: quality-adjusted life years.
Patient satisfaction
There was significantly greater satisfaction in the TI group with regard to the convenience of recording and sharing BP measurements with the health care team, consultation advice received, understanding by the health care team of their condition, and motivation to monitor BP weekly (Table 6). The proportion of patients in the TI group who strongly agreed that the intervention made it more convenient to record and share their BP with the care team was higher compared to the UC group (30.1% vs. 8.8%, p = 0.002). Patients in the TI group were more likely to perceive that the care team understood their condition well because of access to home BP measurements (17.5% vs. 4.6%, p = 0.014) and were more motivated to monitor their BP weekly (20.4% vs. 8.7%, p = 0.022). The mean frequency of home BP readings recorded was 3.14 readings per patient per week (SD = 4.553, range = 0–25) over the 6 months' period of follow-up, more than the minimum of once a week.
Table 6.
Satisfaction survey responses from participants.
| Response | UC group (N = 115) | TI group (N = 103) | p value |
|---|---|---|---|
| Convenient to attend polyclinic (UC)/phone consultation for medication review and adjustment (TI) a , n(%) | |||
| Others | 100(87.0) | 51(79.7) | 0.199 |
| Strongly agree | 15(13.0) | 13(20.3) | |
| Total | 115(100) | 64(100) | |
| Convenient to record BP and share with team (UC)/submit measurements by clicking submit (TI) b , n(%) | |||
| Others | 62(91.2) | 72(69.9) | 0.002** |
| Strongly agree | 6(8.8) | 31(30.1) | |
| Total | 68(100) | 103(100) | |
| Satisfied with polyclinic (UC)/phone consultation advice (TI) c , n(%) | |||
| Others | 102(88.7) | 45(70.3) | 0.001** |
| Strongly agree | 13(11.3) | 19(29.7) | |
| Total | 115(100) | 64(100) | |
| Care team understands condition well because of access to recordings taken at homed, n(%) | |||
| Other | 62(95.4) | 85(82.5) | 0.014* |
| Strongly agree | 3(4.6) | 18(17.5) | |
| Total | 65(100) | 103(100) | |
| Motivated to monitor BP weeklye, n(%) | |||
| Other | 84(91.3) | 82(79.6) | 0.022* |
| Strongly agree | 8(8.7) | 21(20.4) | |
| Total | 92(100) | 103(100) | |
BP: blood pressure; TI: telemonitoring intervention; UC: usual care.
Lower total numbers in the TI group as not all participants were required to take BP medications or had medication adjusted over the phone.
Lower total numbers in the UC group as not all participants were measuring BP at home or sharing BP measurements with the health care team.
Lower total numbers in the TI group as not all participants were required to receive phone consultation advice from the health care team.
Lower total numbers in UC group as not all participants were measuring BP at home or sharing BP measurements with the healthcare team.
Lower total numbers in UC group as not all participants were measuring BP at home.
*p < 0.05, **p < 0.01.
Discussion
Summary
This study is, to our knowledge, the first to evaluate the effects of a technology-enabled home BP monitor in primary care in Singapore on clinical outcomes, medical costs, and patient satisfaction. Our findings showed that the BP TI using a Bluetooth-enabled network-linked home BP monitor and tele-consultation is feasible and cost-effective to implement in an Asian primary care setting. This BP improvement was greater in those whose BP was uncontrolled at baseline than those whose BP was already controlled at baseline. TI patients were also more satisfied with this new model of care than UC group.
Comparison with existing literature
These findings are in line with prior studies that have shown telemonitoring to improve patient outcomes.4–7 The unexpected finding that more visits overall, including FF and tele-consultations, and higher costs resulted for the TI group than the UC group seems counter-intuitive, given that the intervention aims to reduce clinic visits and costs for patients. This is likely because the intervention resulted in more frequent follow-up of patients by clinicians. The care team, possibly due to closer monitoring of TI patients with uncontrolled BP, had more tele-consultations to help with timely medication titration and BP lowering compared to the UC group. Similar results were found in the literature that home BP monitoring can lead to increased medication regimen intensity and higher health care cost.12,13 Most studies assessing home monitoring had a maximum 2-year study period, with the majority having less than 1 year of follow-up. This could limit insights into the long-term effects of home monitoring,13,14 as the major benefit of the intervention, i.e. reduced complications and hospitalizations, only become evident in the longer term. 15 Further, the management cost and cost of the telemonitoring equipment could offset the potential cost savings in the short run. With a longer follow-up period, the cost for the TI group could be lower due to patients' better management of BP and health care teams getting familiar with the new model of care.16,17
Patients assigned to the TI group expressed greater convenience sharing their BP readings, felt the teamlet better understood their condition and were more motivated to take BP readings at home. This is consistent with other studies demonstrating high patient satisfaction rates with telemonitoring systems for management of hypertension. 18 Using a digital intervention increased patient enablement while maintaining high self-reported adherence to the intervention.19,20 Telemonitoring coupled with phone consultations by the teamlet reinforced the perception that the care team was monitoring their condition, strengthened the patient–doctor relationship, and increased the patient's motivation to play an active role in the management of their hypertension.
Strengths and limitations
To our knowledge, this is the first study in Asian primary care setting to comprehensively evaluate the clinical outcomes, cost-effectiveness, and patient satisfaction of a TI for the management of hypertension. This study was a quasi-experimental study conducted in a real-world setting and demonstrated the feasibility of deploying telemonitoring for hypertension management in publicly funded primary care. A robust evaluation was conducted to adjust for differences in characteristics between both groups and potential confounders, allowing us to better appreciate the true effect of the intervention.
Participant assignment was not random and not concealed due to the nature of the intervention. While socio-economic status and educational level were measured, potential confounders such as information technology (IT) literacy were not measured and could not be adjusted for. Participants in both groups were also not ethnically or nationally representative, and so caution is advised in generalizing the findings from this study. IT-savvy patients may be more open to telemonitoring while IT-illiterate patients would decline to sign up, creating a selection bias in the patient selection process. The follow-up period of 6 months was short, and longer follow-up periods would determine long-term adherence to telemonitoring, clinical outcomes as well as cardiovascular complication rates.
The other limitations were that BP for each patient may be variable across different times of the day. As part of UC, the CMs and CCs advised participants to take home BP readings in the morning. We were also unable to verify if the patient was the person uploading the results. The care team reinforced to every patient that the readings would be used as part of clinical care, therefore patients were encouraged to ensure that home BP readings submitted were their own. The sharing of BP device with family members was also discouraged. We overcame these limitations by using office BP for the analysis, instead of the home BP readings submitted from the device.
The present study suggests that the implementation of BP telemonitoring combined with tele-consultations is associated with better clinical outcomes and is cost-effective in the Asian public primary care setting. The initial increase in the number of visits could be due to the fact that the health care team was still adapting to the newer model of care delivery through telemonitoring and therefore made more calls to ensure that patients were adapting well to the intervention. This, with time, may decrease as the team becomes more adept and familiar with this mode of care delivery. Patients are satisfied with telemonitoring for hypertension and are motivated to monitor their BP readings with the perception of continued monitoring by the care team. This suggests that telemonitoring reinforces the patient–provider relationship and will extend the teamlet's capability to provide ongoing care to their patient panel with hypertension, with the patient playing an active role in managing their medical condition. Cost-effectiveness analysis was conducted using the QALY to inform the direction of cost-effectiveness of the intervention and to determine if this intervention could be further adopted and scaled. However, the QALY benefits are best seen over a longer period of evaluation and will be considered for further monitoring in subsequent studies. Further to this, cost of care and funding models differ across primary care settings and further studies of telemonitoring in different primary care settings might be of value.
Conclusion
This study signals a promising start, especially in recent times where there is a strategic shift towards telemedicine given its potential to be the “new norm” in primary care to enable the continuation of clinical care delivery for patients with chronic disease when the need for safe distancing measures arises. Future studies might consider larger and more representative sample sizes, a randomized controlled trial design in various primary care settings and longer term follow-up to assess resource utilization and cardiovascular complications.
Acknowledgements
The research team are very grateful to the staff who helped with patient recruitment and study logistics, particularly Dr Ong Kah Pieng, Dr Tan Hue Min, Evonne Oh, and Nur Atiqah Binte Surya Akmaja. We would also like to thank all patients who participated in this study.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Ministry of Health Office for Healthcare Transformation, and the Ministry of Health's National Medical Research Council under the Centre Grant Programme (Ref No: NMRC/CG/C019/2017); and National Medical Research Council under the Centre Grant Programme - Singapore Population Health Improvement Centre (NMRC/CG/C026/2017_NUHS).
Ethical approval: Ethical approval was granted on 14 September 2018 by the National Healthcare Group Domain Specific Review Board (Reference number: 2018/00785).
Informed consent: Research coordinator who explained the study obtained written informed consent from the participants.
Trial registration: This study has been registered on ClinicalTrials.gov with Clinical trial registry ID: NCT03698890 (https://clinicaltrials.gov/ct2/show/NCT03698890).
ORCID iD: Sok Huang Teo https://orcid.org/0000-0002-8890-6450
References
- 1.Finley CR, Chan DS, Garrison S, et al. What are the most common conditions in primary care? Can Fam Physician 2018; 64: 832–840. [PMC free article] [PubMed] [Google Scholar]
- 2.Kannel WB. Blood pressure as a cardiovascular risk factor: prevention and treatment. JAMA 1996; 275: 1571–1576. [PubMed] [Google Scholar]
- 3.Lopez AD, Mathers CD, Ezzati Met al. et al. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet 2006; 367: 1747–1757. doi: 10.1016/S0140-6736(06)68770-9 [DOI] [PubMed] [Google Scholar]
- 4.Purcell R, McInnes S, Halcomb EJ. Telemonitoring can assist in managing cardiovascular disease in primary care: a systematic review of systematic reviews. BMC Fam Pract 2014; 15: 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duan Y, Xie Z, Dong F, et al. Effectiveness of home blood pressure telemonitoring: a systematic review and meta-analysis of randomised controlled studies. J Hum Hypertens 2017; 31: 427–437. [DOI] [PubMed] [Google Scholar]
- 6.Bosworth HB, Olsen MK, Grubber JM, et al. Two self-management interventions to improve hypertension control: a randomized trial. Ann Intern Med 2009; 151: 687–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Margolis KL, Asche SE, Dehmer SP, et al. Long-term outcomes of the effects of home blood pressure telemonitoring and pharmacist management on blood pressure among adults with uncontrolled hypertension. JAMA Netw Open 2018; 1: e181617. doi:10/1001/jamanetworkopen.2018.1617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Luo N, Wang P, Thumboo Jet al. et al. Valuation of EQ-5D-3L health states in Singapore: modeling of time trade-off values for 80 empirically observed health states. Pharmacoeconomics 2014; 32: 495–507. [DOI] [PubMed] [Google Scholar]
- 9.The World Bank Group. GDP Per capita (current US$) – Singapore. https://data.worldbank.org/indicator/NY.GDP.PCAP.CD?locations=SG (2020, accessed 17 August 2020)
- 10.Department of statistics, Singapore. Singapore economy. https://www.singstat.gov.sg/modules/infographics/economy (July 24, 2020, accessed 17 August 2020)
- 11.World Health Organization. The world health report 2002—reducing risks, promoting healthy life. Geneva, Switzerland: World Health Organization, 2002, p. 108. [Google Scholar]
- 12.Omboni S, Gazzola T, Carabelli Get al. et al. Clinical usefulness and cost effectiveness of home blood pressure telemonitoring: meta-analysis of randomized controlled studies. J Hypertens 2013: 31; 455–468. [DOI] [PubMed] [Google Scholar]
- 13.Magid DJ, Ho PM, Olson KL, et al. A multimodal blood pressure control intervention in 3 healthcare systems. Am J Manag Care 2011; 17: e96–e103. [PubMed] [Google Scholar]
- 14.Bosworth HB, Powers BJ, Olsen MK, et al. Home blood pressure management and improved blood pressure control: results from a randomized controlled trial. Arch Intern Med 2011; 171: 1173–1180. [DOI] [PubMed] [Google Scholar]
- 15.Madsen LB, Christiansen T, Kirkegaard Pet al. et al. Economic evaluation of home blood pressure telemonitoring: a randomized controlled trial. Blood Press 2011; 20: 117–125. [DOI] [PubMed] [Google Scholar]
- 16.Arrieta A, Woods JR, Qiao Net al. et al. Cost–benefit analysis of home blood pressure monitoring in hypertension diagnosis and treatment: an insurer perspective. Hypertension 2014; 64: 891–896. [DOI] [PubMed] [Google Scholar]
- 17.Funahashi J, Ohkubo T, Fukunaga H, et al. The economic impact of the introduction of home blood pressure measurement for the diagnosis and treatment of hypertension. Blood Press Monit 2006; 11: 257–267. [DOI] [PubMed] [Google Scholar]
- 18.Cottrell E, McMillan K, Chambers R. A cross sectional survey and service evaluation of simple telehealth in primary care: what do patients think? BMJ Open 2012; 2: e001392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McManus RJ, Little P, Stuart B. et al. Home and online management and evaluation of blood pressure (HOME BP) using a digital intervention in poorly controlled hypertension: randomised controlled trial. Br Med J 2021; 372: m4858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McManus RJ, Mant J, Franssen M. et al. Efficacy of self-monitored blood pressure, with or without telemonitoring, for titration of antihypertensive medication (TASMINH4): an unmasked randomised controlled trial. Lancet 2018; 391: 949–959. [DOI] [PMC free article] [PubMed] [Google Scholar]