Abstract
Background:
In the Latarjet procedure, the ideal placement of the coracoid graft in the medial-lateral position is flush with the anterior glenoid rim. However, the ideal position of the graft in the superior-inferior position (sagittal plane) for restoring glenohumeral joint stability is still controversial.
Purpose:
To compare coracoid graft clockface positions between the traditional 3 to 5 o'clock and a more inferior (for the right shoulder) 4 to 6 o'clock with regard to glenohumeral joint stability in the Latarjet procedure.
Study Design:
Controlled laboratory study.
Methods:
A total of 10 fresh-frozen cadaveric shoulders were tested in a dynamic, custom-built robotic shoulder model. Each shoulder was loaded with a 50-N compressive load while an 80-N force was applied in the anteroinferior axes at 90° of abduction and 60° of shoulder external rotation. Four conditions were tested: (1) intact, (2) 6-mm glenoid bone loss (GBL), (3) Latarjet procedure fixed at 3- to 5-o’clock position, and (4) Latarjet procedure fixed at 4- to 6-o’clock position. The stability ratio (SR) and degree of lateral humeral displacement (LHD) were recorded. A 1-factor random-intercepts linear mixed-effects model and Tukey method were used for statistical analysis.
Results:
Compared with the intact state (1.77 ± 0.11), the SR was significantly lower after creating a 6-mm GBL (1.14 ± 0.61, P = .009), with no significant difference in SR after Latarjet 3 to 5 o'clock (1.51 ± 0.70, P = .51) or 4 to 6 o'clock (1.55 ± 0.68, P = .52). Compared with the intact state (6.48 ± 2.24 mm), LHD decreased significantly after GBL (3.16 ± 1.56 mm, P < .001) and Latarjet 4 to 6 o'clock (5.48 ± 3.39 mm, P < .001). Displacement decreased significantly after Latarjet 3 to 5 o'clock (4.78 ± 2.50 mm, P = .04) compared with the intact state but not after Latarjet 4 to 6 o'clock (P = .71).
Conclusion:
The Latarjet procedure in both coracoid graft positions (3-5 and 4-6 o’clock) restored the SR to the values measured in the intact state. A more inferior graft position (fixed at 4-6 o’clock) may improve shoulder biomechanics, but additional work is needed to establish clinical relevance.
Clinical Relevance:
An inferior coracoid graft fixation, the 4- to 6-o’clock position, may benefit in restoring normal shoulder biomechanics after the Latarjet procedure.
Keywords: biomechanics, bone-block position, coracoid graft position, Latarjet procedure, shoulder instability, stability ratio
A solid body of evidence demonstrates favorable long-term clinical outcomes and low rates of recurrent instability for coracoid transfer during the Latarjet procedure.1-3,8,11 This surgery is widely regarded as the gold standard for the surgical treatment of recurrent shoulder instability with concomitant critical glenoid bone loss (GBL). Despite novel surgical techniques relying on free bone block transfers,8,25,30 the clinical relevance of the Latarjet procedure persists due to its biomechanically advantageous dynamic sling effect with well-documented, long-term outcomes.19,32
While clinical outcomes have been reported to be favorable, 2 enabling return-to-play rates up to 94% to 97%1,5 and sustained long-term success,11,19 meta-analyses data report failure rates of up to 6.2%3,8 and complication rates as high as 16.1%. 3 Factors predictive of successful outcome include patient-specific factors4,7 as well as technical factors such as fixation type, 23 number of screws, 7 positioning of screws,23,26 handling of the subscapularis muscle, 2 capsular management, 2 bone block orientation, 17 and bone block positioning.7,13 In particular, the coracoid graft position represents a cornerstone of successful results across all technical variations of the Latarjet procedure, as it influences both glenohumeral stability and osseous union7,10,19 as well as progression to osteoarthritis.10,19 While convincing evidence suggests a fixation of the bone block flush with the glenoid cartilage in the mediolateral orientation,7,9,19 evidence on the optimal position of the bone block on the glenoid clockface is still up for debate. Grafts malpositioned too superior or too inferior on the sagittal plane have been associated with recurrent instability.7,13 While previous biomechanical evidence confirms the greatest effect on the restoration of shoulder stability with a coracoid graft position at 4 o'clock, 21 it remains unclear whether a more superior coracoid graft position at 3 o'clock or inferior position at 6 o'clock is superior in restoring glenohumeral instability.
The aim of this biomechanical investigation was to compare a coracoid graft clockface position between the traditional position of 3- to 5-o’clock and a more inferior coracoid graft position of 4- to 6-o’clock (on the glenoid surface) with regard to glenohumeral joint stability in the Latarjet procedure. It was hypothesized that a coracoid bone block position between 4 and 6 o'clock would be superior in restoring glenohumeral stability compared with the traditional 3- to 5-o’clock position.
Methods
Specimen Preparation
A total of 10 fresh-frozen cadaveric shoulders from 7 men and 3 women (mean age, 52.4 years; range, 41-65 years) were tested in this study. The specimens were first donated to a tissue bank for medical research and subsequently purchased by our institution. Specimens were excluded based on age >65 years, history of shoulder surgery, osteoarthritis, degenerative joint disease, or healed fracture malunions. The shoulders were thawed at room temperature overnight before testing. Institutional review board approval was not required for the use of cadaveric specimens at our institution.
Skin, subcutaneous tissue, and all muscle distal to the deltoid were removed. The capsule, rotator cuff musculature, and insertion of coracobrachialis and short head of biceps were left intact on the humerus to restore the sling effect. 32 For the scapula, the clavicle was removed, and the origins of the rotator cuff muscles were left intact. The medial aspect of the scapula was potted in a rectangular mold with polymethyl methacrylate (PMMA; Fricke Dental) with the medial border of the scapula parallel to the horizontal plane. The lateral shaft of the humerus was potted 10 mm below the coracobrachialis and the short head of biceps inserted in a cylindrical mold. The specimens were moistened by spraying saline solution every 20 minutes throughout preparation and testing and immediately before any test. Each scapula was clamped rigidly to a custom fixture mounted to a 6-axis universal force-torque sensor (ATI, Apex) on a pedestal. Each humerus was clamped rigidly to a custom fixture mounted to the end effector of a 6-degrees of freedom (DOF) robot (KUKA KR60) (Figure 1). SimVITRO software was used to control the robot. A joint coordinate system was established by digitizing landmarks using a coordinate measuring machine (Romer Absolute arm, Hexagon Metrology) according to the standards of the International Society of Biomechanics. 29
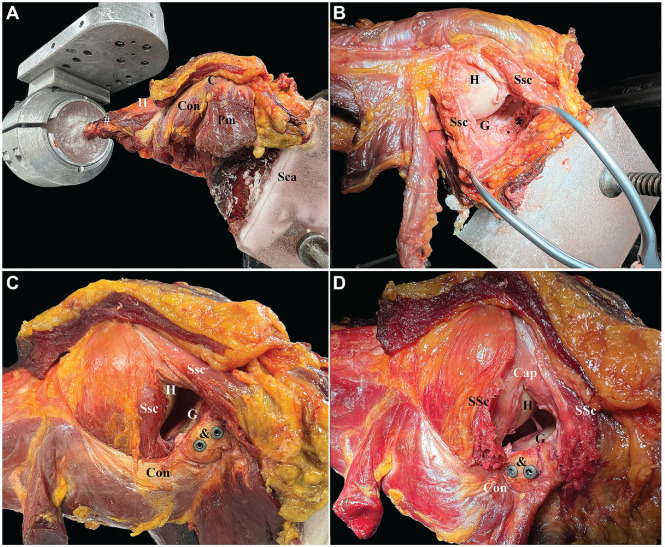
Figure 1.
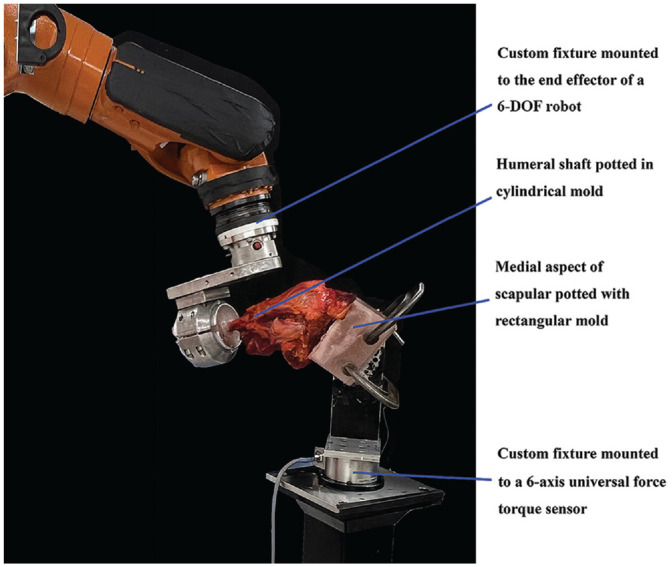
Testing setup. The medial aspect of the scapula was potted in a rectangular mold with polymethyl methacrylate with the medial border of the scapula parallel to the horizontal plane. The lateral shaft of the humerus was potted 10 mm below the coracobrachialis and the short head of biceps was inserted in a cylindrical mold. Each scapula was rigidly clamped to a custom fixture mounted to a 6-axis universal force-torque sensor on a pedestal. Each humerus was clamped rigidly to a custom fixture mounted to the end effector of a 6-degrees of freedom (DOF) robot.
Surgical Technique
The surgical procedure was performed by 3 certified orthopaedic and orthopaedic trauma surgeons for all specimens (P.G., M.D.H., and R.-O.D.H.). Four conditions were tested: (1) intact, (2) 6-mm GBL, (3) Latarjet procedure fixed at 3- to 5-o’clock position, and (4) Latarjet procedure fixed at 4- to 6-o’clock position (Figure 2).
Figure 2.
Right cadaveric shoulder demonstrating the surgical technique in each testing state. (A) Intact state; the coracoid process, C, and the conjoint tendon, Con, were identified. The coracobrachialis and short head of biceps insertion and attachment, #, were left intact to maintain the sling effect. (B) In the GBL state, a 6-mm defect was planned and cut from the 3-o’clock position (right shoulder) parallel to the long axis of the glenoid (G). For the Latarjet procedure fixed at (C) 3- to 5-o’clock position and (D) 4- to 6-o’clock position, the coracoid bone block (&) was fixed using 2 3.75-mm cannulated, partially threaded titanium screws. The capsule (Cap) and subscapularis tendon (SSc) were repaired with No. 2 nonabsorbable suture after completing in each state. GBL, glenoid bone loss; H, humerus; Sca, medial border of scapular; Pm, pectoralis minor.
Intact State
The coracoid process and conjoint tendon were identified. The coracobrachialis and short head of biceps insertion and attachment were left intact to maintain the sling effect. The coracoacromial ligament and pectoralis minor were transected from the coracoid, leaving only the conjoint tendon (Figure 2A).
Glenoid Bone Loss
The subscapularis tendon (SSc) was identified. Next, the SSc split between the upper one-third and lower two-thirds of the SSc was created sharply along its fiber from the humeral insertion to the musculotendinous junction. The anterior capsule was then identified carefully and opened in a horizontal fashion to facilitate glenoid exposure. To stimulate a critical-size glenoid defect, a 6-mm defect was planned and cut from the 3-o’clock position (right shoulder), parallel to the long axis of the glenoid, using an oscillating saw (Figure 2B). 24 The 6-mm defect of the glenoid width was demonstrated biomechanically in a previous study to be the critical size of the glenoid defect. 33 After creating sufficient GBL, the capsule and SSc were repaired with No. 2 nonabsorbable suture (FiberWire Suture, Arthrex)
Latarjet Procedure Fixed at 3- to 5-o’clock position
A coracoid graft was harvested at the level 23 mm proximal to the anterior tip of the coracoid process using an oscillating saw with the conjoint tendon left attached. The inferior edge of the coracoid was corticated to facilitate graft fixation. The screw positions were determined by dividing the lower-half glenoid (below 3 o’clock) into 4 quadrants (Q1-Q4), starting from the 3-o’clock position for the right shoulder (Figure 3). Thereafter, the coracoid bone block was fixed into the standard 3- to 5-o’clock position (right shoulder and superior position) using 2 3.75 mm–cannulated, partially threaded titanium screws with washers (Arthrex) at the location of Q1 and Q2 (Figure 2C and Figure 3).
Figure 3.
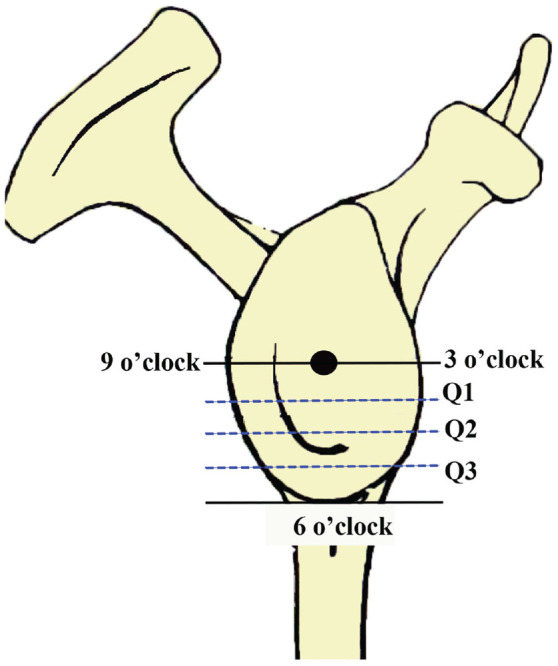
Schematic drawing of the glenoid of a right shoulder. Screw positions were determined by dividing the glenoid into 4 quadrants (Q) starting from the 3-o’clock position. Next, the coracoid bone block was fixed into the standard 3- to 5-o’clock position at the location of Q1 and Q2, while the coracoid bone block was fixed at the location of Q2 and Q3 for the Latarjet procedure fixed at the 4- to 6-o’clock position.
Latarjet Procedure Fixed at 4- to 6-o’clock position
The coracoid bone block was fixed at the 4- to 6-o’clock position (right shoulder and inferior position) using 2 3.75 mm–cannulated, partially threaded titanium screws with washers (Arthrex) at locations Q2 and Q3 (Figure 2D and Figure 3).
Biomechanical Testing
Each specimen underwent biomechanical testing in 4 states: (1) intact, (2) (GBL), (3) Latarjet procedure fixed at 3- to 5-o’clock position, and (4) Latarjet procedure fixed at 4- to 6-o’clock position. During all tests, the shoulder joint was maintained in 90° of humerothoracic abduction. This position corresponded to 53° of elevation, 58° of external rotation, and -18° of the plane of elevation in the glenohumeral coordinate system, as described by Ludewig et al. 16 In the native state, each specimen underwent an initial test to determine the appropriate amount of anterior and inferior displacement for future tests. In this test, a 50 N compressive load was maintained while an 80 N force was applied in the sagittal plane at a 45° angle between the anterior and inferior axes. The corresponding anterior and inferior displacements were recorded. Then, in each state of measurement (GBL, Latarjet procedure fixed at 3 to 5 o'clock and 4 to 6 o’clock), including intact state, a dislocation test was performed at the position of the initial test. In this test, a 50-N compressive load was maintained while the joint was driven in position control to the previously recorded positions on the anterior and inferior axes. The amount of force (anteroinferior force) needed to translate the shoulder throughout this motion was recorded. This methodology was used to measure shoulder stability based on the amount of force needed to cause a dislocation event, while ensuring that testing remained nondestructive to match the repeated measures design of our experiment.
Outcome Measures
Two outcome measures were analyzed. The first was the amount of lateral displacement of the humeral head that occurred during the dislocation. For this measurement, the seated position of the humerus in the glenoid represented 0 mm of lateral translation. As the humerus dislocated, it could not travel in a straight line anteriorly and was instead forced laterally to maintain a constant compression force of 50 N. Therefore, lateral displacement represents the height of the glenoid rim that needed to be overcome by the humerus for the shoulder to dislocate, so higher lateral translation represents more stability.20,32 The second was the stability ratio (SR), which was the amount of anteroinferior force needed to dislocate the shoulder divided by the amount of compressive force. The reason for calculating this value is that the stability of the shoulder joint depends on the amount of compression applied.6,31 With more compression, the joint requires more force in the sagittal plane to dislocate. In the dislocation test, the target compression force was set to 50 N, but based on the system dynamics and the control algorithm, the actual compressive force did not track 50 N perfectly. By looking only at the total amount of force in the sagittal plane, the dislocation force recorded would depend on the speed of the motion and the efficacy of the control algorithm at tracking 50 N of compressive load. By normalizing the sagittal plane load to the compressive load, we obtain an SR, which is less dependent on the specific parameters of our control algorithm and our specific testing setup and more generalizable to any amount of compressive force.
Statistical Analysis
To match the repeated measures design of the study, 1-factor random-intercepts linear mixed effects models were used to compare specimen states. A separate model was made for each of the 2 primary outcome measures: lateral humeral head displacement (mm) and force ratio. An unstructured covariance matrix was assumed for all linear mixed effects models. Estimated marginal means were reported, and Tukey's method was used to make all pairwise comparisons among the 4 shoulder states. Residual diagnostics were inspected to ensure model fit and those assumptions were met. The statistical software R Version 4.0.0 was used for all plots and analyses (accessed May 20, 2020; R Core Team; with additional packages lmer and emmeans). The required sample size was calculated under experimental conditions of small effect size (0.26), an average correlation of 0.8, and an alpha of 0.05. A minimum of 8 specimens was needed to show a significant difference in the outcome variables with a power of 80%. P values <.05 were considered statistically significant.
Results
SR decreased significantly (P = .009) after creating a 6-mm glenoid bone defect (1.14 ± 0.61) compared with the intact state (1.77 ± 0.11). Compared with the intact state, there was no significant difference in SR between Latarjet fixed at 3- to 5-o’clock position (1.51 ± 0.70) and 4- to 6-o’clock position (1.55 ± 0.68) (P = .51 and P = .62, respectively). Furthermore, there was no significant difference between the 2 coracoid graft positions, Latarjet fixed at 3- to 5-o’clock and 4- to 6-o’clock positions (P = .99) (Figure 4).
Figure 4.
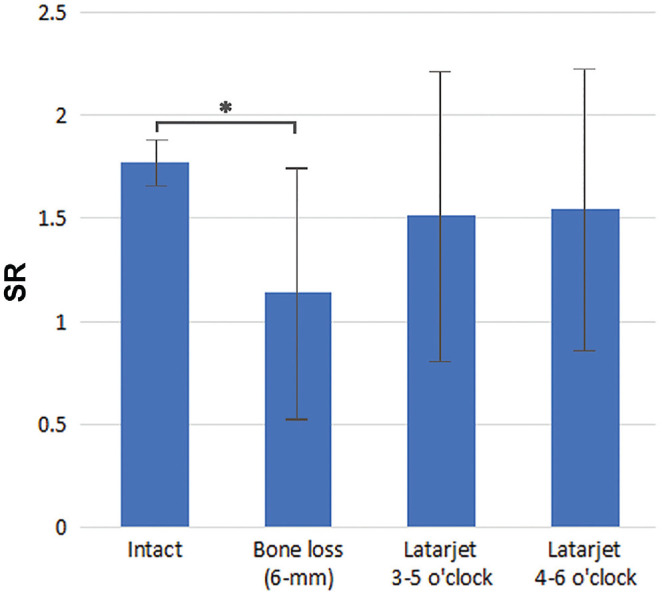
Graph showing mean SR at each testing state. Error bars represent standard deviations. *Statistically significant difference compared with the intact state (P < .05). SR, stability ratio.
The lateral humeral displacement (LHD) decreased significantly in the GBL state (3.16 ± 1.56 mm) compared with the intact state (6.48 ± 2.24 mm; P < .001) and the Latarjet fixed at 4- to 6-o’clock position (5.84 ± 3.39 mm; P < .001). The LHD decreased significantly after the performance of the Latarjet procedure fixed at 3- to 5-o’clock position (4.78 ± 2.50 mm; P = .04) compared with the intact state but not with the Latarjet procedure fixed at 4- to 6-o’clock position (P = .71). There was no significant difference in LHD between the 2 coracoid graft positions, Latarjet fixed at 3- to 5-o’clock and 4- to 6-o’clock positions (P = .32) (Figure 5).
Figure 5.
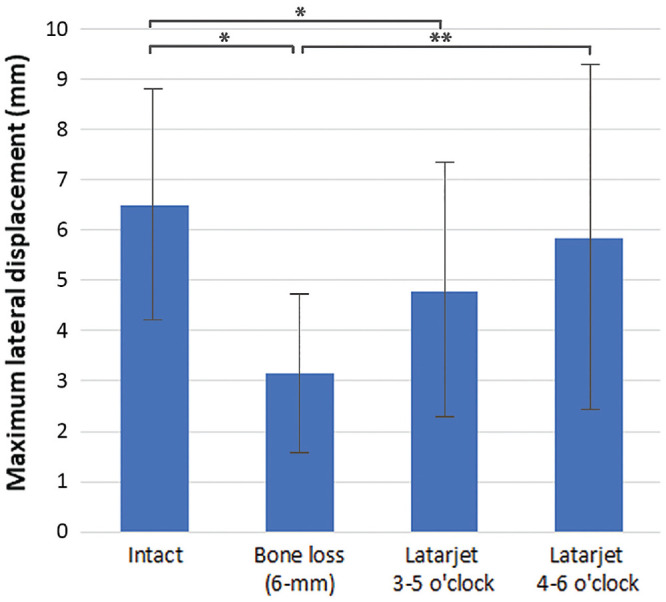
Graph showing the mean LHD at each testing state. Error bars represent standard deviations. Statistically significant difference compared with *intact state and **bone loss state (P < .05). LHD, lateral humeral displacement.
Discussion
The most important finding of this study was that the Latarjet procedure in both coracoid graft positions (3-5 and 4-6 o’clock) restored the SR to the values measured in the intact state (1.51 ± 0.70, P = .51 and 1.55 ± 0.68, P = .52, respectively). The LHD decreased significantly after the GBL state (3.16 ± 1.56 mm, P < .001) and the Latarjet procedure fixed at the standard 3- to 5-o’clock position (4.78 ± 2.50 mm, P = .04) compared with the intact state (6.48 ± 2.24 mm); however, the LHD was restored to the intact level after the Latarjet procedure fixed at the 4- to 6-o’clock position (P = .71). Thus, in terms of the SR, both coracoid graft positions restored shoulder stability to close to the native state. With the more inferior position, the Latarjet procedure fixed at the 4- to 6-o’clock position may improve the shoulder biomechanics in terms of LHD.
The fundamental purpose of the Latarjet procedure is to provide shoulder stability through the triple blocking effect, which includes the sling effect from the conjoint tendon on the subscapularis tendon, the ligament effect after repairing the coracoacromial ligament into the capsule, and the bone effect by restoring the glenoid arc.19,22 However, a biomechanical evaluation of glenohumeral instability has several limitations due to missing muscle forces and capsuloligamentous laxity in cadaveric models. In the presented study, the 6-axis Kuka robot imitated the so-called abduction and external rotation (ABER) shoulder position in all planes. Further, the SR calculated through the peak translation force divided by the applied compressive force represents the glenohumeral joint stability provided by the bony structures.
The accurate placement of the coracoid bone graft relative to the glenoid margin is one of the key elements for a successful Latarjet procedure. There are increased redislocation rates for graft placement in too medial a position (>1 cm) and increased osteoarthritis rates associated with placing the graft too lateral a position. 10 The ideal position of the graft in the medial-lateral position is flush with the anterior glenoid rim. However, the ideal position of the graft in the superior-inferior position (sagittal plane) for restoring glenohumeral joint stability is still not well studied. Historically, technical paradigms suggested a strictly anterior coracoid graft position of the graft on the glenoid clockface. 15 Many studies recommend positioning the graft below the equator (3 o'clock, right shoulder) or between 2 and 5 o'clock (right shoulder) in the sagittal position, matching the typical direction of instability as well as associated GBL and cartilage injury.12-14,18,27 Nourissat et al 21 compared the Bristow-Latarjet coracoid graft position between the 3-, 4-, and 5-o’clock position (medial, anteroinferior, and inferior positions) and showed that the anterior displacement was significantly lower in the 4-o’clock position compared with the 3- or 5-o’clock position in adduction and external rotation position (P = .03). However, they did not reach statistical significance in the ABER shoulder position, which is the most common position for dislocation. 21 Their result also demonstrated less inferior displacement in the 4-o’clock position compared with the 3- or 5-o’clock position (P = .032). 21 However, the 3-o’clock graft position in their study was higher than the equator (3 o’clock), and the inferior end of the 5-o’clock graft position was placed between the 5- and 6-o’clock positions. In the present study, the lower half of the glenoid was divided into 4 quadrants for screw positions to facilitate coracoid placement according to clockface positions. This was done to ensure the coracoid graft was placed in the 3- to 5- and 4- to 6-o’clock positions. The findings from the present study also show that there was no significant difference in SR between the standard 3- to 5-o’clock and 4- to 6-o’clock position in the vulnerable ABER shoulder position.
There have been reports showing that a more superior graft position may provide superior clinical results in hyperlaxity patients due to a more pronounced sling effect.21,34 Gasbarro et al 7 retrospectively reviewed all revision cases (83 patients) after primary coracoid process transfer, showing that placing the screw inferior to the 5-o’clock position increased the risk of failure (17 out of 83 patients). However, this conclusion was drawn based on the case series, and there was no direct comparison between the ideal graft position and the inferior graft position. In the present study, it was demonstrated that there was no difference in the SR between these 2 positions (3- to 5- and 4- to 6-o’clock positions). Additional clinical evidence in terms of clinical outcomes and risks of failure is needed to confirm the favorable results reported after a more inferior graft position (4- to 6-o’clock position); in particular, the effect of the more inferior graft position and corresponding decreased tension on the conjoint tendons and its possible neurologic effects should be investigated. Recently, a biomechanical study by Wermers et al 28 showed that, apart from the glenoid defect size, glenoid concavity was a significant predictor of SR. Therefore, corporate glenoid concavity and the defect size for clinical decision-making for recurrent shoulder instability may be helpful.
Limitations
The current study had several limitations. First, the SR was selected as the primary outcome and the means of evaluating shoulder stability. Besides the capsuloligamentous complex and muscle activities, bony stability is one of the stabilizing mechanisms of the shoulder. There was no load in the muscle to reflect the in vivo muscle activity in this cadaveric study and only one level of subscapularis split. Moreover, the laxity of the joints was not standardized. However, we reduced these confounders by repairing the shoulder capsule and subscapularis tendon in each testing state to restore the integrity of the capsuloligamentous complex. Second, the sling effect is one of the key factors critical to the success of the Latarjet procedure. There was no load applied to the conjoint tendon or subscapularis muscle to avoid damage inflicted by loading the cadaveric shoulder with in vivo forces. Despite that, the insertions of the coracobrachialis and short head of biceps at the coracoid process, as well as the attachment of the coracobrachialis at the humerus, were preserved while repairing the subscapularis tendon to restore the sling effect of the Latarjet procedure. Finally, this study investigated the SR and the degree of humeral displacement at the time zero. Additional in vivo studies may be beneficial to understand the effects such as outcomes, impingement symptoms, or risk of failure after inferior coracoid graft position at the 4- to 6-o’clock position in the Latarjet procedure.
Conclusion
The Latarjet procedure in both coracoid graft positions (3- to 5- and 4- to 6-o’clock positions) restored the SR to the values measured in the intact state. A more inferior graft position (fixed at 4-6 o’clock) may improve shoulder biomechanics, but additional work is needed to establish clinical relevance.
Acknowledgments
The authors thank the Steadman Philippon Research Institute Digital Media for the illustrations as well as Suchitphon Chanchoo and Narumol Sudjai from the Faculty of Medicine at Siriraj Hospital Mahidol University for the statistical analysis.
Footnotes
Final revision submitted April 21, 2023; accepted May 19, 2023.
One or more of the authors has declared the following potential conflict of interest or source of funding: this research was supported by the Steadman Philippon Research Institute. R.-O.D.H. and M.-C.R. have received grant support from AGA. P.J.M. has received consulting and nonconsulting fees from Arthrex; research support from Arthrex, Ossur, Siemens, and Smith & Nephew; royalties from Arthrex, Medbridge, and Springer; and stock or stock options from VuMed. M.T.P. has received royalties from Anika Therapeutics, Arthrex, and Arthrosurface; consulting fees from Arthrex, Zimmer Biomet Holdings, and JRF Ortho; nonconsulting fees from Arthrex and Arthrosurface; and honoraria from Flexion Therapeutics and JRF Ortho. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Abdul-Rassoul H, Galvin JW, Curry EJ, Simon J, Li X. Return to sport after surgical treatment for anterior shoulder instability: a systematic review. Am J Sports Med. 2019;47(6):1507-1515. [DOI] [PubMed] [Google Scholar]
- 2. Arner JW, Tanghe K, Shields T, et al. Shoulder Latarjet surgery shows wide variation in reported indications, techniques, perioperative treatment, and definition of outcomes, complications, and failure: a systematic review. Arthroscopy. 2022;38(2):522-538. [DOI] [PubMed] [Google Scholar]
- 3. Cho CH, Na SS, Choi BC, Kim DH. Complications related to Latarjet shoulder stabilization: a systematic review. Am J Sports Med. 2021:3635465211042314. [DOI] [PubMed] [Google Scholar]
- 4. Domos P, Lunini E, Walch G. Contraindications and complications of the Latarjet procedure. Shoulder Elbow. 2018;10(1):15-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ernat JJ, Rakowski DR, Hanson JA, et al. High rate of return to sport and excellent patient-reported outcomes after an open Latarjet procedure. J Shoulder Elbow Surg. 2022;31(8):1704-1712. [DOI] [PubMed] [Google Scholar]
- 6. Fukuda K, Chen CM, Cofield RH, Chao EY. Biomechanical analysis of stability and fixation strength of total shoulder prostheses. Orthopedics. 1988;11(1):141-149. [DOI] [PubMed] [Google Scholar]
- 7. Gasbarro G, Giugale JM, Walch G, Lin A. Predictive surgical reasons for failure after coracoid process transfers. Orthop J Sports Med. 2016;4(12):2325967116676795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gilat R, Haunschild ED, Lavoie-Gagne OZ, et al. Outcomes of the Latarjet procedure versus free bone block procedures for anterior shoulder instability: a systematic review and meta-analysis. Am J Sports Med. 2021;49(3):805-816. [DOI] [PubMed] [Google Scholar]
- 9. Hovelius L, Olofsson A, Sandström B, et al. Nonoperative treatment of primary anterior shoulder dislocation in patients forty years of age and younger. A prospective twenty-five-year follow-up. J Bone Joint Surg Am. 2008;90(5):945-952. [DOI] [PubMed] [Google Scholar]
- 10. Hovelius L, Sandström B, Olofsson A, Svensson O, Rahme H. The effect of capsular repair, bone block healing, and position on the results of the Bristow-Latarjet procedure (study III): long-term follow-up in 319 shoulders. J Shoulder Elbow Surg. 2012;21(5):647-660. [DOI] [PubMed] [Google Scholar]
- 11. Imam MA, Shehata MSA, Martin A, et al. Bankart repair versus Latarjet procedure for recurrent anterior shoulder instability: a systematic review and meta-analysis of 3275 shoulders. Am J Sports Med. 2021;49(7):1945-1953. [DOI] [PubMed] [Google Scholar]
- 12. Kany J, Flamand O, Grimberg J, et al. Arthroscopic Latarjet procedure: is optimal positioning of the bone block and screws possible? A prospective computed tomography scan analysis. J Shoulder Elbow Surg. 2016;25(1):69-77. [DOI] [PubMed] [Google Scholar]
- 13. Kordasiewicz B, Małachowski K, Kiciński M, et al. Intraoperative graft-related complications are a risk factor for recurrence in arthroscopic Latarjet stabilisation. Knee Surg Sports Traumatol Arthrosc. 2019;27(10):3230-3239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kraeutler MJ, McCarty EC, Belk JW, et al. Descriptive epidemiology of the MOON shoulder instability cohort. Am J Sports Med. 2018;46(5):1064-1069. [DOI] [PubMed] [Google Scholar]
- 15. Latarjet M. [Technic of coracoid preglenoid arthroereisis in the treatment of recurrent dislocation of the shoulder] [Article in French]. Lyon Chir. 1958;54(4):604-607. [PubMed] [Google Scholar]
- 16. Ludewig PM, Phadke V, Braman JP, Hassett DR, Cieminski CJ, LaPrade RF. Motion of the shoulder complex during multiplanar humeral elevation. J Bone Joint Surg Am. 2009;91(2):378-389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mengers SRP, Knapik DM, Kaufman MW, et al. Clinical outcomes of the traditional Latarjet versus the congruent arc modification for the treatment of recurrent anterior shoulder instability: a meta-analysis. Orthop J Sports Med. 2021;9(10):23259671211030204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Minuesa-Asensio A, García-Esteo F, Mérida-Velasco JR, et al. Comparison of coracoid graft position and fixation in the open versus arthroscopic Latarjet techniques: a cadaveric study. Am J Sports Med. 2020;48(9):2105-2114. [DOI] [PubMed] [Google Scholar]
- 19. Mizuno N, Denard PJ, Raiss P, Melis B, Walch G. Long-term results of the Latarjet procedure for anterior instability of the shoulder. J Shoulder Elbow Surg. 2014;23(11):1691-1699. [DOI] [PubMed] [Google Scholar]
- 20. Nacca C, Gil JA, DeFroda SF, Badida R, Owens BD. Comparison of a distal tibial allograft and scapular spinal autograft for posterior shoulder instability with glenoid bone loss. Orthop J Sports Med. 2018;6(7):2325967118786697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nourissat G, Delaroche C, Bouillet B, Doursounian L, Aim F. Optimization of bone-block positioning in the Bristow-Latarjet procedure: a biomechanical study. Orthop Traumatol Surg Res. 2014;100(5):509-513. [DOI] [PubMed] [Google Scholar]
- 22. Patte D, Debeyre J. Luxations récidivantes de l’épaule. Encycl Med Chir Paris-Technique chirurgicale. 1980;44265(4):4.4-02. [Google Scholar]
- 23. Provencher MT, Aman ZS, LaPrade CM, et al. Biomechanical comparison of screw fixation versus a cortical button and self-tensioning suture for the Latarjet procedure. Orthop J Sports Med. 2018;6(6):2325967118777842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Provencher MT, Detterline AJ, Ghodadra N, et al. Measurement of glenoid bone loss: a comparison of measurement error between 45 degrees and 0 degrees bone loss models and with different posterior arthroscopy portal locations. Am J Sports Med. 2008;36(6):1132-1138. [DOI] [PubMed] [Google Scholar]
- 25. Provencher MT, Frank RM, Golijanin P, et al. Distal tibia allograft glenoid reconstruction in recurrent anterior shoulder instability: clinical and radiographic outcomes. Arthroscopy. 2017;33(5):891-897. [DOI] [PubMed] [Google Scholar]
- 26. Shin JJ, Hamamoto JT, Leroux TS, et al. Biomechanical analysis of Latarjet screw fixation: comparison of screw types and fixation methods. Arthroscopy. 2017;33(9):1646-1653. [DOI] [PubMed] [Google Scholar]
- 27. Souleiman F, Zderic I, Pastor T, et al. Cartilage decisively shapes the glenoid concavity and contributes significantly to shoulder stability. Knee Surg Sports Traumatol Arthrosc. 2022;30(11):3626-3633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wermers J, Schliemann B, Raschke MJ, et al. Glenoid concavity has a higher impact on shoulder stability than the size of a bony defect. Knee Surg Sports Traumatol Arthrosc. 2021;29(8):2631-2639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wu G, van der Helm FC, Veeger HE, et al. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion - Part II: shoulder, elbow, wrist and hand. J Biomech. 2005;38(5):981-992. [DOI] [PubMed] [Google Scholar]
- 30. Xiang M, Yang J, Chen H, et al. Arthroscopic autologous scapular spine bone graft combined with bankart repair for anterior shoulder instability with subcritical (10%-15%) glenoid bone loss. Arthroscopy. 2021;37(7):2065-2074. [DOI] [PubMed] [Google Scholar]
- 31. Yamamoto N, Itoi E, Abe H, et al. Effect of an anterior glenoid defect on anterior shoulder stability: a cadaveric study. Am J Sports Med. 2009;37(5):949-954. [DOI] [PubMed] [Google Scholar]
- 32. Yamamoto N, Muraki T, An KN, et al. The stabilizing mechanism of the Latarjet procedure: a cadaveric study. J Bone Joint Surg Am. 2013;95(15):1390-1397. [DOI] [PubMed] [Google Scholar]
- 33. Yamamoto N, Muraki T, Sperling JW, et al. Stabilizing mechanism in bone-grafting of a large glenoid defect. J Bone Joint Surg Am. 2010;92(11):2059-2066. [DOI] [PubMed] [Google Scholar]
- 34. Young AA, Baba M, Neyton L, Godeneche A, Walch G. Coracoid graft dimensions after harvesting for the open Latarjet procedure. J Shoulder Elbow Surg. 2013;22(4):485-488. [DOI] [PubMed] [Google Scholar]