Abstract
A 63-year-old male patient recovering from dengue came to our department for contrast-enhanced computed tomography (CECT) for the evaluation of abdominal pain. An ultrasound performed in the periphery diagnosed him with a rectus abscess. The CECT evaluation done in our department clarified that the collection in his rectus sheath was hemorrhagic and not infective, as previously thought. The patient was managed conservatively and recovered without complications.
Like most infectious diseases, dengue is a disease of tropical countries. System-wise data collection processes are inadequate in many developing countries, which means complications and adverse effects of common diseases are not adequately captured. Furthermore, resource limitations restrict the availability of more expensive diagnostic tests to central locations. Peripherally located regions with lower purchasing capacity have greater access to relatively inexpensive tests. This causes deficits in the management of some common disease entities, like dengue.
Considering these issues, it is important to optimize healthcare testing for low-resource settings. This can only be achieved with adequate sensitization of healthcare providers in diagnosis and management.
Keywords: affordable healthcare, health promotion in medical imaging, dengue virus infection, complications of dengue fever, dengue fever/complications
Introduction
Febrile patients with severe musculoskeletal pain often go unrecognized in emergency departments due to inadequate sensitivity towards muscle sheath hematomas associated with the presentation of dengue fever. A patient who presents with a fever of unknown origin and an exudative muscle collection on ultrasound can be incorrectly diagnosed as having a musculoskeletal abscess.
Dengue is a disease of the tropics [1,2]. Hemorrhage is a known side effect of dengue fever, leading to the formation of hematomas [3]. However, the management of dengue patients often overlooks musculoskeletal hematomas, especially in those with pyrexia of unknown origin (PUO). Increased sensitivity to the presence of hematomas in fever cases related to dengue will improve the diagnosis of this complication on ultrasound, especially in low-resource settings.
We will present a case of rectus sheath hematoma in a PUO patient, diagnosed as an abscess in the periphery.
Case presentation
A 63-year-old male subject recovering from dengue came to our department with a complaint of pain and tenderness in the right-sided anterior abdominal wall. The patient was febrile (101°F) at the time of contrast computed tomography (CT) evaluation in our center. He also had raised blood glucose levels (275 mg/dl) and a decreasing platelet count (56,000/ml) at the time of the scan. An ultrasound in the periphery revealed gall bladder wall edema, minimal ascites, and right pleural effusion. Furthermore, the ultrasound revealed a collection in the right rectus muscle. Considering the subject’s clinical symptoms of high fever with abdominal pain, they considered the exudative collection to favor an infective abscess. Prior medical history included uncontrolled diabetes and essential hypertension.
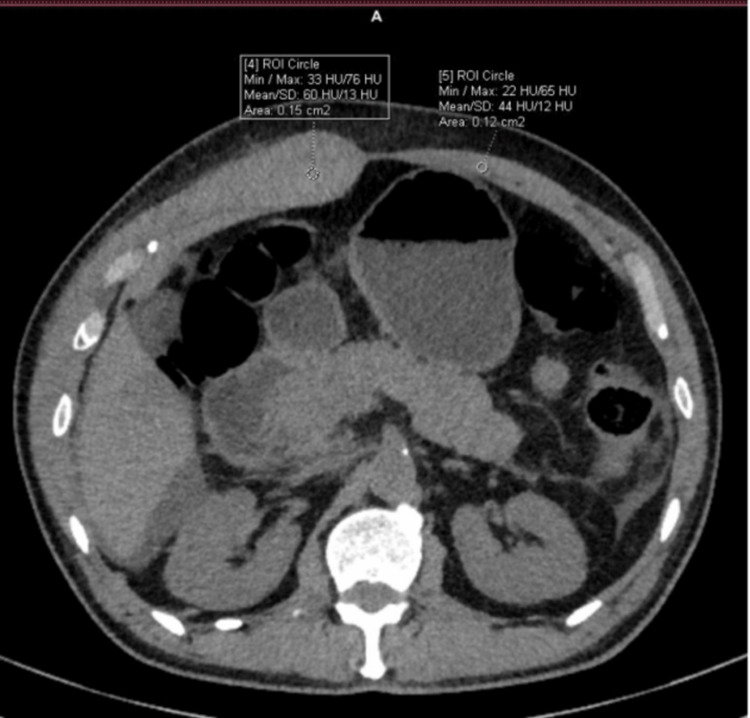
A CECT done in the department corroborated ultrasound findings of gall bladder wall edema and right pleural effusion. Minimal perihepatic-free fluid was also seen. In addition, the right rectus sheath appeared thickened (27mm vs. 7mm on the left) (Figure 1) and hyperdense (HU 60) (Figure 2) compared to the left rectus sheath (HU 44). Moreover, there was a non-enhancing hypodense collection within the muscle. Based on CECT, the patient was diagnosed as having rectus sheath hematoma, likely due to dengue coagulopathy.
Figure 1. Non contrast CT image of subject showing abdominal wall.
CT: computed tomography
Figure 2. Right rectus sheath shows collection on CECT.
CECT: contrast-enhanced computed tomography
The patient was managed conservatively with pain management and fluid replacement. The hematoma resolved in a few days, along with the resolution of symptoms.
Discussion
Rectus sheath hematomas are very painful and sometimes form a palpable lump. They will often not cross the midline [2]. Ultrasound findings will mimic any exudative collection with echoes within the collection. However, thin septae and echogenic clots may suggest the diagnosis of hemorrhage. CT has a hyperdense pattern of intramuscular collection, with no enhancement in contrast. CT is the usual mode for a final confirmatory diagnosis of rectus hematoma.
A literature review on Pubmed yielded fourteen [3-16] articles regarding rectus muscle hematoma in dengue patients. Most of these were case reports. Muscle hematoma has since been recognized as an often occult cause of severe abdominal pain in dengue patients.
A total of ten case reports of abdominal wall hematomas in dengue patients were identified among the fourteen articles in the National Medical Library [4-13]. Nine of these were in the rectus sheath and one in the psoas muscle (n = 10). All these reports were from South Asia: India (n = 5), Sri Lanka (n = 2), Pakistan (n = 1), Indonesia (n = 1), and Singapore (n = 1). These locations represent the areas where dengue is more common and patients are more likely to suffer complications due to a lack of timely diagnosis. The mean age of the patients was 60, with 60% (n = 6) females and 40% (n = 4) males.
At least five of these patients were diagnosed with dengue only after the onset of abdominal pain (lower abdomen-3, upper abdomen-2) due to the hematoma. All five had been having PUO. The remaining five patients were being treated for or recovering from dengue and developed severe abdominal pain (lower abdomen-3, upper abdomen-2) caused by the hematoma.
Repetitive vomiting was the most common cause of precipitating hematoma formation (n = 4). Sixty percent of patients (n = 6) had lower abdominal pain. Three patients from the unrecognized febrile dengue group had co-morbid conditions of hypertension and diabetes. One had adenomyosis with accompanying anemia. One last patient was on warfarin post-surgery for aortic stenosis [12].
The final diagnosis was made based on CT-based investigations in the majority of these (non-contrast CT-4, CECT-1, CT angiography-1) cases.
Hematoma patients are managed conservatively with rest, fluid replacement, and pain relief. In contrast to this, abscesses need to be further managed with culture and sensitivity, fluid evaluation, and then antibiotics and drainage. Early recognition of a hematoma will spare the patients these unnecessary investigations and reduce the cost burden of the disease.
Conclusions
Dengue is predominantly a disease in tropical countries. System-wise data collection processes are inadequate in many developing countries, causing inefficient data collection on associations, comorbidities, and complications of infectious diseases. Furthermore, resource limitations result in the concentration of more expensive diagnostic tests in central locations. Peripherally located regions with lower purchasing capacity have greater access to inexpensive tests. This causes deficits in the management of some common disease entities, like dengue. Considering these issues, it is important to optimize healthcare testing for low-resource settings. Achieving this requires adequately sensitizing healthcare providers.
In patients who have had an untreated viral pattern of fever (high-grade fever with muscle and joint pain and lymphocyte predominance on blood count), we suggest that abdominal pain and guarding should prompt a search for muscle hematoma formation. Musculoskeletal hematomas are easy to diagnose on ultrasound when there is a degree of suspicion for them. This is especially true for anterior wall/rectus sheath hematomas, which are easily visualized with superficial ultrasound probes. Increased sensitivity to the presence of musculoskeletal hematomas in PUO patients during dengue season will improve the diagnosis of this complication on ultrasound. This is especially true for settings where ultrasound is the main workhorse for diagnosis.
Acknowledgments
Dr. Mudit Arora for help with the case selection. Dr. Komal Chamaria for support.
The authors have declared that no competing interests exist.
Author Contributions
Concept and design: Pragya Sinha
Acquisition, analysis, or interpretation of data: Pragya Sinha, Virendra S. Chauhan
Drafting of the manuscript: Pragya Sinha, Virendra S. Chauhan
Critical review of the manuscript for important intellectual content: Pragya Sinha, Virendra S. Chauhan
Supervision: Virendra S. Chauhan
Human Ethics
Consent was obtained or waived by all participants in this study. Saral Department of Radiology Review Board issued approval NA. We confirm that no identifying text or image was used in this work and that informed consent has been obtained from the patient.
References
- 1.Dengue and Severe Dengue. [ Nov; 2023 ];https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue 2023 9:2023. [Google Scholar]
- 2.Rectus sheath haematoma: a new set of diagnostic features. Maharaj D, Ramdass M, Teelucksingh S, Perry A, Naraynsingh V. Postgraduate Medical Journal. 2002;78:755–756. doi: 10.1136/pmj.78.926.755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clinical profiles of dengue infection during an outbreak in Northern India. Laul A, Laul P, Merugumala V, Pathak R, Miglani U, Saxena P. J Trop Med. 2016:5917934. doi: 10.1155/2016/5917934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Unusual surgical emergency in a patient of dengue haemorrhagic fever: spontaneous rectus sheath haematoma leading to abdominal compartment syndrome. Ghosh S, Singh R, Ghosh S, Chawla A. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6047707/ BMJ Case Rep. 2018:0. doi: 10.1136/bcr-2018-225936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abdominal mass and a forgotten haemorrhagic fever. Tong P, Yeoh CJ, Yong EL. Lancet. 2010;376:140. doi: 10.1016/S0140-6736(10)60671-X. [DOI] [PubMed] [Google Scholar]
- 6.An unusual cause of acute abdominal pain in dengue fever. Waseem T, Latif H, Shabbir B. Am J Emerg Med. 2014;32:819. doi: 10.1016/j.ajem.2014.01.011. [DOI] [PubMed] [Google Scholar]
- 7.Spontaneous arterial hemorrhage as a complication of dengue. Rao SV, Jacob GG, Raju NA, Ancheri SA. Indian J Crit Care Med. 2016;20:302–304. doi: 10.4103/0972-5229.182201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abdominal haematomas and dengue fever: two different cases of spontaneous psoas muscle haematoma and bilateral rectus sheath haematoma complicating dengue haemorrhagic fever. Bhat KJ, Shovkat R, Samoon HJ. https://pubmed.ncbi.nlm.nih.gov/26714517/ J Vector Borne Dis [Internet. 2015;52:339–341. [PubMed] [Google Scholar]
- 9.Dengue fever with rectus sheath hematoma: a case report. Sharma A, Bhatia S, Singh RP, Malik G. J Family Med Prim Care. 2014;3:159–160. doi: 10.4103/2249-4863.137665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spontaneous rectus sheath hematomas in dengue hemorrhagic fever: a case report. Nelwan EJ, Angelina F, Adiwinata R, Matondang S, Andriono P. IDCases. 2017;10:35–37. doi: 10.1016/j.idcr.2017.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dengue fever associated with a haematoma of the rectus abdominis muscle. Ganeshwaran Y, Seneviratne SM, Jayamaha R, De Silva AP, Balasuriya WK. Ceylon Med J. 2001;46:105–106. doi: 10.4038/cmj.v46i3.8139. [DOI] [PubMed] [Google Scholar]
- 12.Bilateral rectus sheath haematoma complicating dengue virus infection in a patient on warfarin for mechanical aortic valve replacement: a case report. Rosa CT, Navinan MR, Samarawickrama S, et al. BMC Res Notes [Internet. 2017;10:26. doi: 10.1186/s13104-016-2330-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Acute abdominal pain and dengue fever. Wiwanitkit V. Am J Emerg Med. 2014;32:679. doi: 10.1016/j.ajem.2014.03.012. [DOI] [PubMed] [Google Scholar]
- 14.Cerebral vasculitis and lateral rectus palsy - two rare central nervous system complications of dengue fever: two case reports and review of the literature. Herath HMM, Hewavithana JS, De Silva CM, Kularathna OAR, Weerasinghe NP. J Med Case Rep. 2018;12:100. doi: 10.1186/s13256-018-1627-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dengue and rectus sheath hematoma. Wiwanitkit S, Wiwanitkit V. J Family Med Prim Care. 2015;4:154. doi: 10.4103/2249-4863.152280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paralytic squint due to abducens nerve palsy: a rare consequence of dengue fever. Shivanthan MC, Ratnayake EC, Wijesiriwardena BC, Somaratna KC, Gamagedara LKGK. BMC Infect Dis. 2012;12:156. doi: 10.1186/1471-2334-12-156. [DOI] [PMC free article] [PubMed] [Google Scholar]