Abstract
Background:
In spite of, the need for evidence-based intervention on the potential harmful effects of self-medication practices during pregnancy, there is no systematic review and meta-analysis study regarding self-medication practices in Ethiopia. Therefore, the aim of this study is to determine prevalence of self-medication practice and associated factors among pregnant women in Ethiopia.
Method:
We used PubMed, the Cochrane Library, Google Scholar, the Wiley Online Library, and African Journals Online to choose important studies. The I-squared statistic method was used to check for heterogeneity between studies. Random effect model was used to estimate the pool prevalence of self-medication among pregnant women. Publication bias was determined by the funnel plot and Egger’s test.
Result:
A total of 11 studies with 4643 study participants were included in this review. The finding from the current meta-analysis showed that the overall prevalence of self-medication practice among pregnant women is 33.92% (95% CI: 23.15–44.70, I² value = 80.9%). First trimester of pregnancy (OR: 2.24, 95% CI: 1.44–3.47), women who faced health problems during pregnancies at the moment (OR: 5.7, 95% CI: 3.92–8.29), previous self-medication practice (OR: 13.07, 95% CI: 5.14–33.25) and previous pregnancy-related problems (OR: 2.065, 95% CI: 1.44–2.96) were positively associated with self-medication practice among pregnant women.
Conclusion:
The prevalence of self-medication practices among pregnant women is found to be high. Self-medication practices of the pregnant women were significantly higher among women who were in first-trimester pregnancy, encountered illness during pregnancy, previous self-medication history, and previous pregnancy-related problems.
Prospero registration number: CRD42023394907.
Keywords: Self-medication, pregnant women, associated factors, Ethiopia
Background
World Health Organization defined self-medication as the act of using medications intermittently or continuously by patients or individuals to treat self-diagnosed disorders or symptoms on their own initiative without getting advice from healthcare providers. 1 It also includes the utilization of herbal and cultural medicines. 2 If people practiced without the advice of health professionals, self-medication could lead to severe health complications and a waste of medical resources.3,4
Pregnancy is a special physiological condition where drug treatment presents a special concern because the physiology of pregnancy affects the pharmacokinetics of medications used, and certain medications can directly reach the fetus through the placenta and cause harm. 5 However, many pregnant women practiced self-harming with medications (Premaquine, sulfonamides, chloramphenicol, and warfarin).6–8 Identifying the harmful effects of self-medications among pregnant women may contribute to achieving good birth outcomes. 5 Self-medications is practiced throughout the world and among individuals of different ages, even though the magnitude shows a discrepancy.9,10 Self-medication practice results in a consequence of increase in burdens on healthcare systems and increase costs for treatment of complication related to self-medication practice. 11 The fact that certain drugs given during pregnancy may prove harmful to the unborn child is one of the classic problems in medical treatment approaches.
The effects of unselective drugs or substances during pregnancy can cause harm to the fetus by interfering with normal growth and development, impacting the growth of the baby’s organs, impacting the placenta, which is a source of food and nutrients, increasing the risk of pre-term birth, and increasing the risk of the fetus withdrawing from substances and needing medication after they are born.6,12,13 It has been reported that pregnant women’s exposure to drugs without proper counseling from healthcare providers causes more than 10% of birth defects. 14 Therefore, unless absolutely necessary, drugs should be avoided during pregnancy.5,15 Despite this fact, there is a high level of self-medication use during pregnancy. 16 Currently, evidence shows that using self-medication during pregnancy is on the rise globally. A recent global study, for instance, found the pooled prevalence of self-medication during pregnancy to be 32% (95% CI: 22%–44%). 17 Another review focused on low- and middle-income countries found that self-medication during pregnancy could be as high as 93%. 18 The prevalence of self-medication during pregnancy varies across different studies, which ranged from 15.5% to 70%.19,20 There are different reasons for self-medication among pregnant women in different countries.
It includes inherent cultural and socioeconomic differences, disparities in healthcare systems and access to healthcare, plus drug dispensing policies, lack of access to healthcare services, unregulated distribution of medicines, patients’ attitudes toward healthcare providers, socioeconomic factors, a poor healthcare system, the cost of the drugs, educational level, age, income, education level, satisfaction, and the beliefs of people toward medication and disease.11,20–22 However, the generalizability of these accounts to Ethiopia is problematic since these reviews did not include any primary research on self-medication during pregnancy in Ethiopia. In spite of, the need for evidence-based intervention on the potential harmful effects of self-medication practices during pregnancy,23,24 there is no public health policy on self-medication during pregnancy in the country, and there is no systematic review and meta-analysis study regarding self-medication practices during pregnancy in Ethiopia. Moreover, there is little awareness about the impact of self-medication practices among pregnant mothers in developing countries, including Ethiopia. 25 Hence, the pooled prevalence of self-medication practice and its contributors will be provided information for health policymakers and relevant stakeholders to develop strategies to prevent the risks associated with self-medication practice during pregnancy.
Moreover, this pooled study may help stakeholders design an evidence-based intervention and remove guild liens for pregnant women. Therefore, this study tried to show the burden of self-medication at the national level and associated factors among pregnant women in Ethiopia.
Methods
Study design: Systematic review and meta-analysis study was conducted.
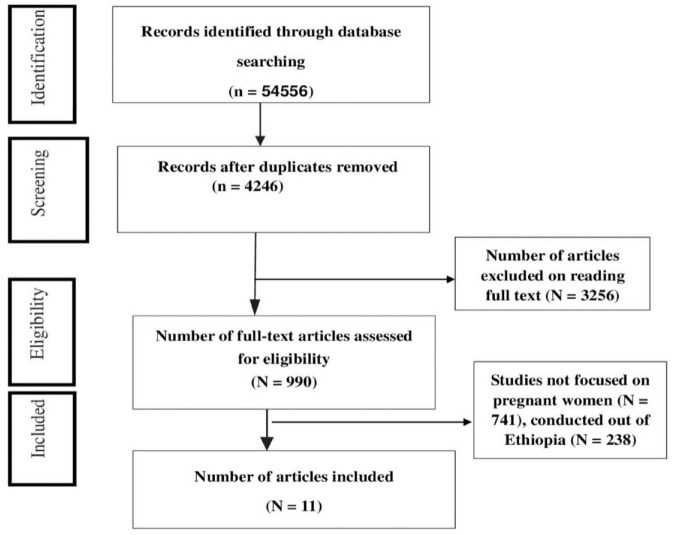
Search engine and protocol: The articles were searched via using PubMed, Cochrane Library, Google scholar, African Journals Online, and Wiley Online Library in Ethiopia from December 30 to January 30, 2023. A manual search was also done for gray studies available on Ethiopian university shelves and institutional repositories but no study found. The search style was limited to full texts of article, freely available articles, conducted on humans, and published by English language only 35 . Endnote X 7 citation manager software was utilized to collect, and remove duplicate studies. During searching, medical subheading terms (“self-medication practice,” “pregnant women,” “associated factors,” and “Ethiopia”) were used (Figure 1).
Figure 1.
PRISMA flow diagram for selection of the included studies.
Eligibility criteria: Inclusion criteria for our study were observational studies including cross-sectional studies that report prevalence and associated factors of self-medication among pregnant women in Ethiopia, studies published in peer-reviewed journals, gray literature, and articles published in English language from starting to January 30, 2023. The study was excluded studies that were not freely accessible, case series, letters, comments, and editorials, and/or failed to report the outcome variable (i.e., self-medication practice).
Outcome of interest: The outcome variable of the study is prevalence and associated factors of self-medication practice of among pregnant women.
Study selection: All identified articles were sent into EndNote version 7, and duplicates were deleted. Full titles and abstracts were then screened by two reviewers (YAF and WCT) for assessment. The entire documents of selected articles were assessed in addition for the inclusion criteria by two reviewers (YAF and DGH).
Quality assessment and data extraction: After identifying included articles, two authors (SSW and BAM) performed data extraction independently.
Information from the included studies (author, publication year, region, study area, study design, sample size, sampling technique, prevalence of self-medication practice, and associated factors) were collected. After finishing data extraction by the two authors the third author (WCT) cross-checked for data similarity.
Disagreements that arose during data extraction were resolved by group communications. The quality of each articles were checked by Newcastle–Ottawa scale adapted for cross-sectional studies for quality check. 26 The tool contains three main parts. The first part of the tool has five stars, and assesses the methodological quality of each study (i.e., sampling technique, sample size, response rate, and ascertainment of the risk factor or exposure). The second part of the tool assesses the comparability of the study with a possibility of two stars. The last component of the instrument measures the outcomes and statistical tests of the primary study with a possibility of three stars. Finally, studies included in this systematic review and meta-analysis have to high-quality scores (>6 out of 10 stars). Moreover, quality assurance checks were performed by two authors (WCT and BBY). Controversy related to articles was collectively resolved by all authors.
Publication bias and heterogeneity: We used Cochran’s Q and the I-squared statistics (0%–25%: might not be important, 25%–50%: may represent moderate heterogeneity, 50%–75%: may represent substantial heterogeneity, 75%–100%: considerable heterogeneity) to determine heterogeneity between studies. 27 We explored sources of heterogeneity through subgroup analysis by region and sampling technique and found heterogeneity in sampling technique. Sensitivity analysis and subgroup analysis were also performed for the effect of each study on the overall estimate. Funnel plots and Egger’s test were used to check the presence or absence of Publication bias. 28
Analysis of data: We used a random-effects model to pool the prevalence of self-medication practice because of the observation of heterogeneity across the included articles. 29 The pooled estimate (i.e., prevalence of self-medication practice) with a 95% confidence interval (CI) was done and presented using a forest plot graph. All statistical analysis techniques were performed using software STATA version 11 (StataCorp LLC, TX, USA). 6
Result
Selection of studies: We used the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) checklist for the reporting of the study findings. 30 The first search identified 54,556 articles, which were imported in citation manager software (EndNote X 7.0). Studies were found from PubMed (579,267), Cochrane Library (601), Google Scholar (25,100), Wiley Online Library (216), and African Journals Online (574). Of them, 50,310 duplicate studies were identified and deleted. By reviewing the articles and based on the predefined criteria, 11 articles were included for the final analysis.
Summary of primary studies: A total of 11 studies with 4643 study participants were included in the review with the response rate of 98.98%. Of these, all 11 studies were included to estimate prevalence of self-medication practice among pregnant mothers. Regarding study designs, all (100%) of studies are cross-sectional and regarding to quality assessment all studies have high quality assessed by Newcastle–Ottawa scale. The number of study participants per articles ranged from 195 to 1121. The prevalence of self-medication practice was reported from various regions in Ethiopia; three studies were from Amhara,2,7,31 one from Addis Ababa, 5 four from Oromia,15,25,32,33 one from South, 34 one from Tigray, 6 and one from Harari. 20 With regard to the sampling technique, six studies used simple random sampling, one study used systematic random sampling, two used multistage sampling techniques, one study used consecutive sampling, and one study used purposive sampling method
Table 1.
Summary of studies included in the systematic review and meta-analysis of prevalence of self-medication practice among pregnant women in Ethiopia, 2023.
| Author | Pub year | Region | Study area | Study design | Sample size | Sampling technique | Prevalence |
|---|---|---|---|---|---|---|---|
| k/mariam G, et al. 5 | 2018 | Addis Ababa | Adiss Ababa | Cross sectional | 634 | Multi stage sampling | 26.6 |
| Gedefaw A et al. 2 | 2015 | Amhara | Bahirdar | Cross sectional | 518 | Multi stage sampling | 25.1 |
| Ake S and Yimam 34 | 2021 | South Ethiopia | Gedeo | Cross sectional | 360 | Systematic random sampling | 40.4 |
| Zewudie et al. 25 | 2018 | Oromia | Goba | Cross sectional | 323 | Simple random sampling | 15.5 |
| Fasel D et al. 7 | 2020 | Amhara | Gondar | Cross sectional | 400 | Simple random sampling | 44.8 |
| Jambo A and Mengistu 20 | 2018 | Harari | Harar | Cross sectional | 247 | Simple random sampling | 69.7 |
| Seid M et al. 15 | 2020 | Oromia | Jimma | Cross sectional | 1121 | Consecutive sampling | 27 |
| Tuha et al. 31 | 2020 | Amhara | Kemisie | Cross sectional | 223 | Simple random sampling | 26.9 |
| Wakjira G et al. 32 | 2019 | Oromia | Nekemte | Cross sectional | 195 | Purposive sampling | 21.5 |
| Niriayo et al. 6 | 2021 | Tigray | Mekelle | Cross sectional | 262 | Simple random sampling | 40.8 |
| Gemechu G 33 | 2020 | Oromia | Shashemane | Cross sectional | 360 | Simple random sampling | 27.7 |
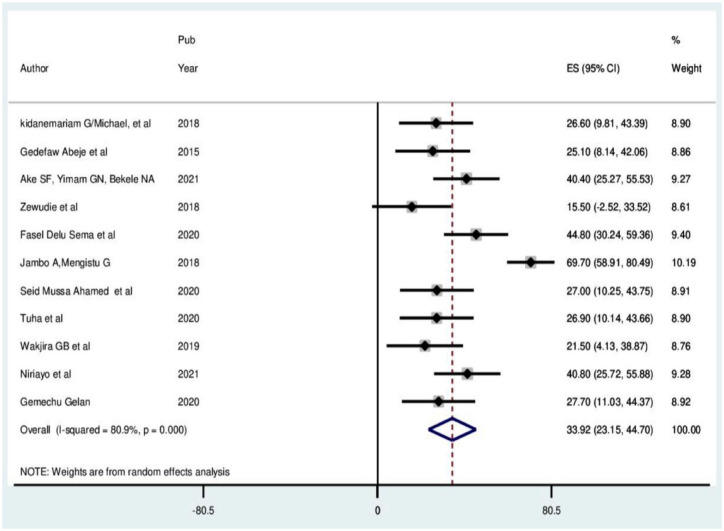
Self-medication practice: The current meta-analysis showed that the overall prevalence of self-medication practice among pregnant mothers is 33.923 % (95% CI: 23.15–44.70, I² = 80.9%); (Figure 2).
Figure 2.
Forest plot of the pooled prevalence of self-medication practice among pregnant.
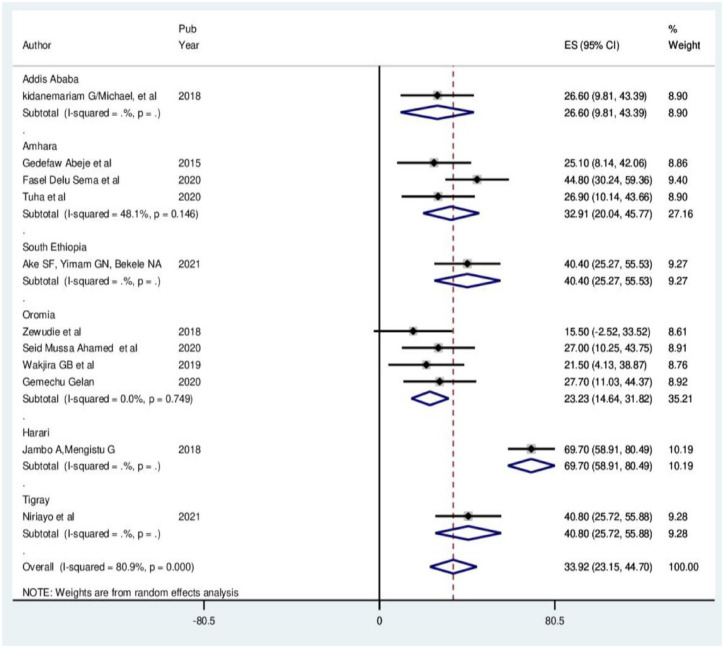
Subgroup analysis: To explore the origin of heterogeneity across the included articles, subgroup analysis was done by regions (Figure 3) and sampling technique (Figure 4).
Figure 3.
Subgroup analysis of included articles by region in meta-analysis.
Figure 4.
Subgroup analysis of included articles by sampling technique in meta-analysis.
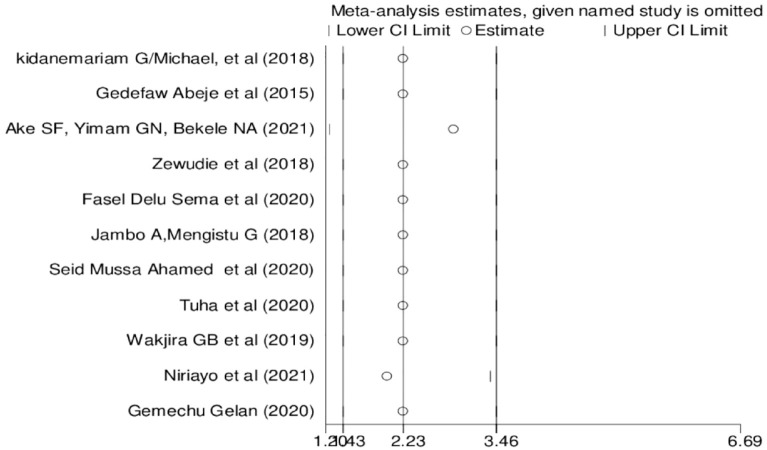
Sensitivity: The sensitivity analysis using the random-effect model revealed that no single study influenced the overall pooled prevalence (Figure 5).
Figure 5.
Results of the sensitivity analysis of the 11 studies.
Publication bias: As shown in Figure 6, the visual inspection of the funnel plot showed that there was publication bias among the included studies, as illustrated by the asymmetrical observation of the funnel plot. Likewise, the result of Egger’s test was statistically significant for the presence of publication bias (p < 0.000).
Figure 6.
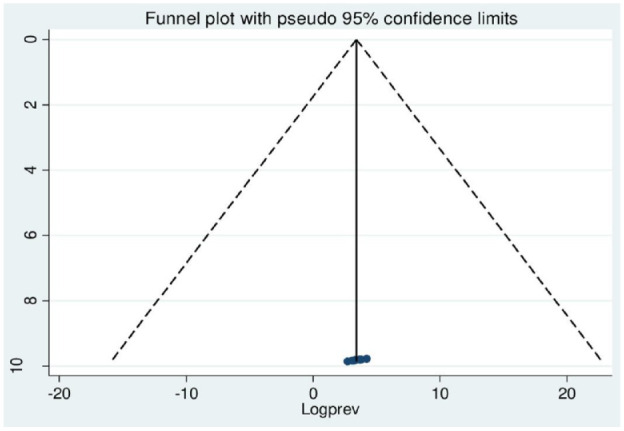
Funnel plot assessed for publication bias in 11 studies.
Factors associated with self-medication practice among pregnant mothers: Based on this meta-analysis, self-medication practice among pregnant women in the Ethiopia setting was associated with gestational age, illness during current pregnancy, previous pregnancy self-medication history, and previous pregnancy-related problems.
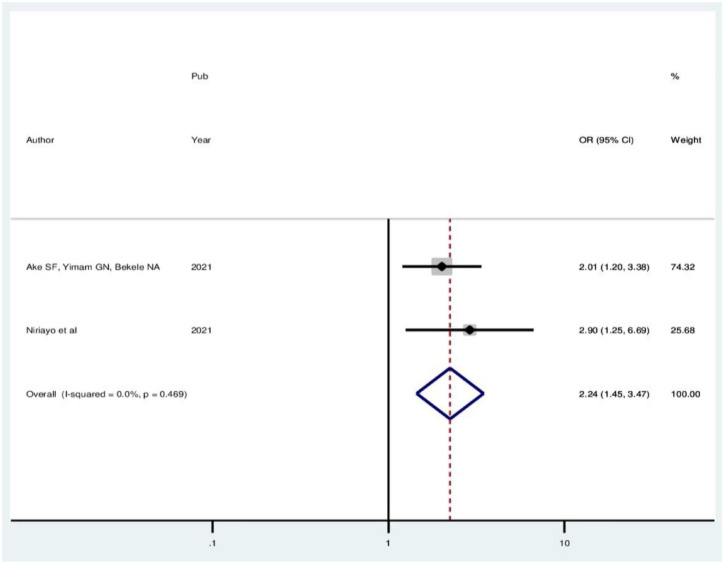
In this review, the pooled odds ratio estimate of self-medication practice in two studies showed that pregnant women in their first trimester of pregnancy were about 2.24 (OR: 2.24, 95% CI: 1.44–3.47) times more likely to practice self-medication compared to women in their third trimester of pregnancy. In this meta-analysis, included studies were characterized with no existence of heterogeneity (I2 = 0.0%, p = 0.469); (Figure 7).
Figure 7.
Forest plot showing the pooled odds ratio of the association between first-trimester pregnancy and self-medication practice.
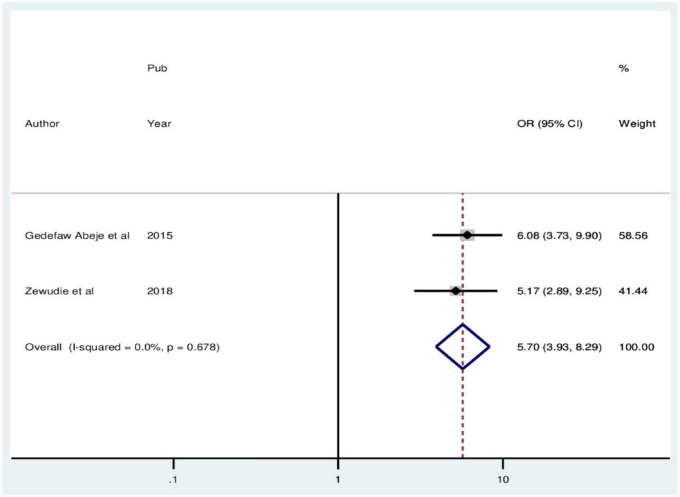
In this meta-analysis, the pooled odds ratio estimate of self-medication practice in two studies showed that pregnant women who experienced health problems during pregnancies at the moment were 5.7 times more likely to use self-medication compared to their counterparts (OR: 5.7, 95% CI: 3.92–8.29). In this meta-analysis, included studies were characterized with no existence of heterogeneity (I2 = 0.0%, p = 0.678). Thus, a fixed effect model analysis was used (Figure 8).
Figure 8.
Forest plot showing the pooled odds ratio of the association between health problems during pregnancy and self-medication practice.
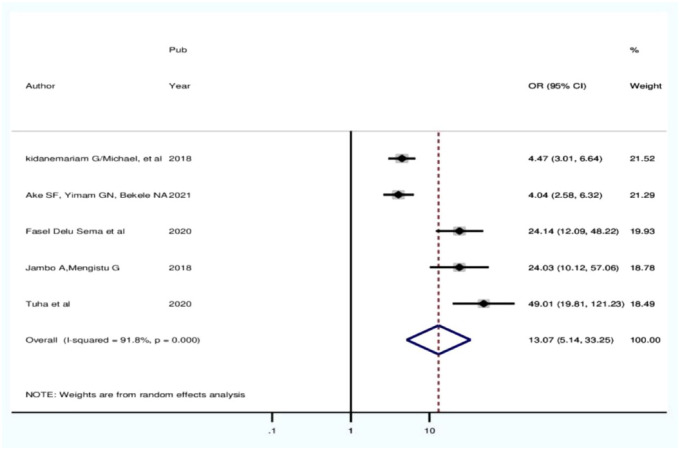
In current review, the pooled odds ratio estimate of self-medication practice in five included studies showed that pregnant women who had previous self-medication practice were about 13.07 times more likely to practice self-medication compared with their counterparts (OR: 13.07, 95% CI: 5.14–33.25). In this meta-analysis, included studies were characterized with existence of heterogeneity (I2 = 91.8%, p > 0.000). Thus, a random effect model analysis was used (Figure 9).
Figure 9.
Forest plot showing the pooled odds ratio of the association between pregnant women who had previous self-medication practice.
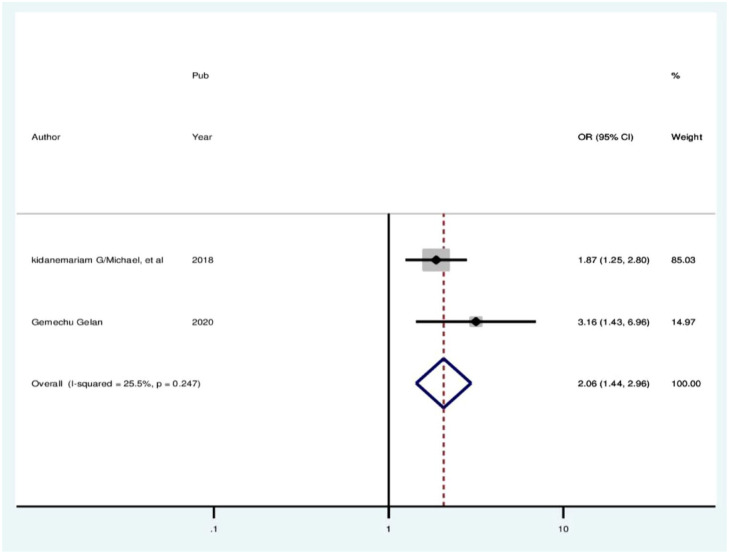
In the current analysis, the pooled odds ratio estimate of self-medication practice in two studies showed that pregnant women who encountered previous pregnancy-related problems were about 2.065 times more likely to practice self-medication compared with their counterparts (OR: 2.065, 95% CI: 1.44–2.96). In this meta-analysis, included studies were characterized with no existence of heterogeneity (I2 = 25.5%, p = 0.247). Thus, a fixed effect model analysis was used (Figure 10).
Figure 10.
Forest plot showing the pooled odds ratio of the association between previous pregnancy-related problem and self-medication practice.
Discussion
In the present review, the pooled prevalence of self-medication among pregnant women in Ethiopia was estimated to be 33.92% (95% CI: 23.14–44.70, I2 = 80.9%). The overall pool prevalence of self-medication practice among pregnant women found in our review was lower than that reported in Iran 38.46%, 32%, and 43.5%.35–37
The above disparities could be differences in over-the-counter medication patterns and medication prescription systems in different countries. For instance, in some African countries, all medications can be bought without medical prescription. Other reasons for the relatively high prevalence of self-medication in our study are the high costs of frequent medical visits, inadequate healthcare insurance coverage, and over-the-counter sale of most medications in drug stores, previous history of taking some medications, and inattentiveness to symptoms. 35
In this analysis, the pooled estimate of two studies showed that pregnant women in their first trimester of pregnancy were about 2.24 times more likely to practice self-medication compared to women in their third trimester of pregnancy. This study is consistent with study conducted in Tanzania. 13 The possible justification for higher self-medication practice during first trimester of pregnancy could be due to the more frequent occurrence of symptoms and/or illnesses including morning sickness, headache, and fever in the first trimester than other trimester during pregnancy. Also, this might be due to the fact that initial discomforts associated with new pregnancy and most symptoms of pregnancy-related illness are during the first stage of pregnancy. Moreover, pregnant women might be less careful in the last trimesters due to the assumptions of the maturity of the fetus. More importantly, this finding is worrisome as drug exposure in this period is more likely to cause congenital abnormalities. 24
In this analysis, the pooled estimate of two studies showed that pregnant women who experienced health problems during pregnancies at the moment were 5.7 times more likely to use self-medication compared to their current counterparts (OR: 5.7, 95% CI: 3.92–8.29). Similar finding is found from Congo. 38 This indicates that women who have any types of health problem during pregnancy may prefer self-medication to save time and other related factors. In the current analysis, the pooled estimate of five studies showed that pregnant women who had previous self-medication practice were about 13.07 times more likely to practice self-medication compared with their counterparts. This study was in congruence with studies done in Iran, the Democratic Republic of Congo. 38
This might be due to the presence of chronic disea-ses, previous exposure to medicines, pregnancy- and delivery-related problems, and poor awareness on risk of self-medications. Another possible reason could be that commonly used medicines outside pregnancy might create the impression that over-the-counter medicines are safe to use during pregnancy.
In the current meta-analysis, the pooled estimate in two studies showed that pregnant women who encountered previous pregnancy-related problems were about 2.065 times more likely to practice self-medication compared with their counterparts. This finding is similar with study conducted in Iran. 35 The possible explanation for this could be the previous experience of treating similar illness with self-medication and considering them as not serious.
Limitation of the review
This meta-analysis was limited to English-language articles with full-text articles readily available. Since the papers in this review were all cross-sectional, causality could not be proven. Additionally, this meta-analysis only included studies from a few regions, which may have an impact on the pool prevalence of self-medication.
Conclusion
The prevalence of self-medication practices among pregnant women is found to be high. Self-medication practices of the pregnant women during pregnancy were significantly higher among women who were first-trimester pregnancy, illness during pregnancy, previous pregnancy self-medication history and previous pregnancy-related problems.
Recommendation
Health institutions have to give health education about the risks associated with self-administered drugs to all pregnant women attending ANC services. Moreover, intervention programs should be designed to minimize the practice of self-medication during pregnancy.
Supplemental Material
Supplemental material, sj-doc-1-smo-10.1177_20503121231194429 for Self-medication practice and associated factors among pregnant women in Ethiopia: A systematic review and meta-analysis by Worku Chekol Tassew, Yeshiwas Ayal Ferede, Samson Sisay Woldie, Berhanu Wale Yirdaw, Habiba Fenta Hussien, Bimrew Bayuh Yimer, Dawit Gismie Hailemariam, Banchigizie Adane Mengistu and Agerie Mengistie Zeleke in SAGE Open Medicine
Acknowledgments
The authors would like to thank the authors of the included primary studies, which used as source of information to conduct this systematic review and meta-analysis.
Footnotes
Authors’ contributions: HFH and YAF developed the protocol and were involved in the design, selection of the studies. BAM and SSW involved in data extraction. BWY, WCT, BBY, AMZ, and DGH were involved in statistical analysis, development of the initial drafts of the manuscript, quality assessment, statistical analysis, and revising the manuscript. WCT and AMZ prepared the final draft of the manuscript. All authors read and approved the final draft of the manuscript.
Availability of data and materials: All relevant data generated and analyzed in the analysis process is included in this article
Consent for publication: Not applicable.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics approval and consent to participate: Ethical approval not applicable.
Informed consent not applicable.
Funding: The authors received no financial suppport for the research, authorship, and/or publication of this article.
ORCID iDs: Worku Chekol Tassew  https://orcid.org/0000-0003-4589-5824
https://orcid.org/0000-0003-4589-5824
Yeshiwas Ayal Ferede  https://orcid.org/0000-0003-0180-5495
https://orcid.org/0000-0003-0180-5495
Samson Sisay Woldie  https://orcid.org/0000-0002-6880-0755
https://orcid.org/0000-0002-6880-0755
Berhanu Wale Yirdaw  https://orcid.org/0000-0003-0489-9634
https://orcid.org/0000-0003-0489-9634
Supplemental materials: Supplemental file 1: PRISMA checklist for meta-analysis of self-medication practice among pregnant women in Ethiopia.
Supplemental file 2: Methodological quality assessment of the included studies was performed using the modified Newcastle–Ottawa Scale (NOS).
Supplemental files 3 and 4: Author response for reviewers com-ments.
References
- 1. Yeika EV, Ingelbeen B, Kemah BL, et al. Comparative assessment of the prevalence, practices and factors associated with self-medication with antibiotics in Africa. Trop Med Int Health 2021; 26(8): 862–881. [DOI] [PubMed] [Google Scholar]
- 2. Abeje G, Admasie C, Wasie B. Factors associated with self medication practice among pregnant mothers attending antenatal care at governmental health centers in Bahir Dar city administration, Northwest Ethiopia, a cross sectional study. Pan Afr Med J 2015; 20: 276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Amaha MH, Alemu BM, Atomsa GE. Self-medication practice and associated factors among adult community members of Jigjiga town, Eastern Ethiopia. PLoS One 2019; 14(6): e0218772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Shafie M, Eyasu M, Muzeyin K, et al. Prevalence and determinants of self-medication practice among selected households in Addis Ababa community. PLoS One 2018; 13(3): e0194122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Beyene KGM, Beza SW. Self-medication practice and associated factors among pregnant women in Addis Ababa, Ethiopia. Trop Med Health 2018; 46(1): 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Niriayo YL, Mohammed K, Asgedom SW, et al. Self-medication practice and contributing factors among pregnant women. PLoS One 2021; 16(5): e0251725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sema FD, Addis DG, Melese EA, et al. Prevalence and associated factors of self-medication among pregnant women on antenatal care follow-up at University of Gondar Comprehensive Specialized Hospital in Gondar, Northwest Ethiopia: a cross-sectional study. Int J Reprod Med 2020; 2020: 2936862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Patel K, Patel H, Patel T, et al. Epidemiological study of corneal blindness: A prospective observational study at Sat Kaival Eye Hospital, Sarsa. J Med Scien and Health Care Resea. 2022; 1(1): 1–4. [Google Scholar]
- 9. Rutter P. Role of community pharmacists in patients’ self-care and self-medication. Integr Pharm Res Pract 2015; 4: 57–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. World Health Organization. Guidelines for the regulatory assessment of medicinal products for use in self-medication. Geneva: World Health Organization, 2000. [Google Scholar]
- 11. Alhomoud F, Aljamea Z, Almahasnah R, et al. Self-medication and self-prescription with antibiotics in the Middle East-do they really happen? A systematic review of the prevalence, possible reasons, and outcomes. Int J Infect Dis 2017; 57: 3–12. [DOI] [PubMed] [Google Scholar]
- 12. Wakjira GB, Boru BG, Labata BG. Prevalence of self-medication and its associated factors among pregnant women attending antenatal care at Nekemte referral hospital, Oromia Regional State, West Ethiopia. J Bioanal Biomed 2019; 11: 1–6. [Google Scholar]
- 13. Marwa KJ, Njalika A, Ruganuza D, et al. Self-medication among pregnant women attending antenatal clinic at Makongoro health centre in Mwanza, Tanzania: a challenge to health systems. BMC Pregnancy Childbirth 2018; 18(1): 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Nakamura MU KJL, Pasquale M. Use of drugs during pregnancy: benefit and cost. Rev Bras Ginecol Obstet 2008; 30(1): 1–4. [DOI] [PubMed] [Google Scholar]
- 15. Ahmed SM, Sundby J, Aragaw YA, et al. Self-medication and safety profile of medicines used among pregnant women in a tertiary teaching Hospital in Jimma, Ethiopia: a cross-sectional study. Int J Environ Res Public Health 2020; 17(11): 3993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fekadu G, Dugassa D, Negera GZ, et al. Self-medication practices and associated factors among health-care professionals in selected hospitals of Western Ethiopia. Pat Pref Adher 2020; 14: 353–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Opoku R, Yar DD, Botchwey CO. Self-medication among pregnant women in Ghana: a systematic review and meta-analysis. Heliyon 2022; 8(10): e10777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Torres NF, Chibi B, Middleton LE, et al. Evidence of factors influencing self-medication with antibiotics in LMICs: a systematic scoping review protocol. Syst Rev 2018; 7(1): 102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sisay MMG, Edessa D. Epidemiology of self-medication in Ethiopia: a systematic review and meta-analysis of observational studies. BMC Pharmacol Toxicol 2018; 19(1): 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jambo A, Mengistu G, Sisay M, et al. Self-medication and contributing factors among pregnant women attending antenatal care at public hospitals of Harar Town, Ethiopia. Front Pharmacol 2018; 9: 1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Karimy M, Rezaee-Momtaz M, Tavousi M, et al. Risk factors associated with selfmedication among women in Iran. BMC Public Health 2019; 19(1): 1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bello FA, Morhason-Bello IO, Olayemi O, et al. Patterns and predictors of self-medication amongst antenatal clients in Ibadan, Nigeria. Niger Med J 2011; 52(3): 153–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ahmed SM, Sundby J, Aragaw YA, et al. Medicinal plants used among pregnant women in a tertiary teaching hospital in Jimma, Ethiopia: a cross-sectional study. BMJ Open 2021; 11(8): e046495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Dellicour S, Sevene E, McGready R, et al. First-trimester artemisinin derivatives and quinine treatments and the risk of adverse pregnancy outcomes in Africa and Asia: a meta-analysis of observational studies. PLoS Med 2017; 14(5): e1002290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Zewdie T, Azale T, Shimeka A, et al. Self-medication during pregnancy and associated factors among pregnant women in Goba Town, Southeast Ethiopia: a community based cross sectional study. BMC Res Note 2018; 11(1): 713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- 27. Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, et al. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods 2006; 11(2): 193. [DOI] [PubMed] [Google Scholar]
- 28. Egger M, Higgins JP, Smith GD, (eds). Systematic reviews in health research: Meta-analysis in context. Hoboken: John Wiley & Sons, 2022. [Google Scholar]
- 29. Borenstein M, Hedges LV, Higgins JP, et al. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods 2010; 1(2): 97–111. [DOI] [PubMed] [Google Scholar]
- 30. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Int Med. 2009; 151(4): W-65–W-94. [DOI] [PubMed] [Google Scholar]
- 31. Tuha A, Faris AG, Mohammed SA, et al. Self-medication and associated factors among pregnant women attending antenatal care at Kemisie General Hospital, North East Ethiopia. Patient Prefer Adherence 2020; 16: 1969–1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wakjira G, Boru B, Labata B. Prevalence of self-medication and its associated factors among pregnant women attending antenatal care at Nekemte Referral Hospital, Oromia Regional State, West Ethiopia. J Bioanal Biomed 2019; 11: 160–165. [Google Scholar]
- 33. Gelan G. Utilization and factors associated with self medication among pregnant women in Shashamane Town, Southern Ethiopia, 2020: a community based cross sectional study. Doctoral dissertation, HU, 2020. [Google Scholar]
- 34. Ake SF, Yimam GN, Bekele NA. Self-medication and its predictors among pregnant women in Gedeo zone, South Ethiopia. J Basic Clin Pharm 2021; 12(6): 60–66. [Google Scholar]
- 35. Rahmani A, Hamanajm SA, Fallahi A, et al. Prevalence of self-medication among pregnant women: a systematic review and meta-analysis. Iran J Nurs Midwifery Res 2019; 8(4): 169–175. [Google Scholar]
- 36. Ebrahimi H, Atashsokhan G, Amanpour F, et al. Self-medication and its risk factors among women before and during pregnancy. Pan Afr Med J 2017; 27(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mohseni M, Azami-Aghdash S, Sheyklo SG, et al. Prevalence and reasons of self-medication in pregnant women: a systematic review and meta-analysis. Int J Commun Based Nurs Midwifery 2018; 6(4): 272. [PMC free article] [PubMed] [Google Scholar]
- 38. Mbarambara PM, Songa PB, Wansubi LM, et al. Self-medication practice among pregnant women attending antenatal care at health centers in Bukavu, Eastern DR Congo. Int J Innov Appl Stud 2016; 16(1): 38. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-doc-1-smo-10.1177_20503121231194429 for Self-medication practice and associated factors among pregnant women in Ethiopia: A systematic review and meta-analysis by Worku Chekol Tassew, Yeshiwas Ayal Ferede, Samson Sisay Woldie, Berhanu Wale Yirdaw, Habiba Fenta Hussien, Bimrew Bayuh Yimer, Dawit Gismie Hailemariam, Banchigizie Adane Mengistu and Agerie Mengistie Zeleke in SAGE Open Medicine