Abstract
Introduction:
Congenital anomalies of the kidney and urinary tract (CAKUT) represent a wide range of disorders that result from developmental abnormalities of the kidneys, urinary collecting tract, and lower urinary tract. There has been extensive development in approaches to the management of stones in normal kidneys with the advent of retrograde intra-renal surgeries (RIRS)/ureteroscopies, extracorporeal shock wave lithotripsy (ESWL) percutaneous nephrolithotomy (PCNL), and minimally invasive surgery (laparoscopy/robotics). However, the management of stones in CAKUT is not straightforward and is often challenging for urologists. There are no clear guidelines available to help navigate stone management in such patients.
Materials and methods:
The aim of this literature review was to focus on stone management in anomalous kidneys. Most common abnormalities were considered. The studies were very heterogeneous with different approaches. The methodology involved evaluating studies looking into individual surgical approaches to the management of stones in these anomalous kidneys as well as looking at different approaches to stone management, in particular renal abnormality.
Results:
We found RIRS is a feasible approach in most stones with sizes <20 mm and PCNL holds the upper hand in stones more than 20 mm. However, ESWL, laparoscopy, and robotics have their places in managing some of these cases.
Conclusion:
We concluded that stones in anomalous kidneys can be challenging but can be managed safely. There is no straightforward answer to the right technique but rather the right planning based on the anatomy of the kidney in terms of vascularity and drainage, stone size and density, and expertise available.
Keywords: anomalous kidneys, extracorporeal shock wave lithotripsy, kidney stones, percutaneous nephrolithotomy, ureteroscopies
Introduction
The management of stones in the urinary tract has evolved rapidly over the last century with surgical techniques becoming more minimally invasive in the shape of ureteroscopies, extracorporeal shock wave lithotripsy, lasers, and laparoscopy. Less than 4% of patients with urinary stones are estimated to undergo open surgery in reference centers. 1 However, managing stones in kidneys with anomalies still poses a challenge even to experienced urologists.
Congenital abnormalities affecting the kidneys or other structures of the urinary tract are referred to as congenital anomalies of the kidney and urinary tract (CAKUT). The abnormalities are broadly classified as abnormalities in structure, renal vasculature, number, position, and renal fusion. In this review, kidneys with abnormalities in terms of position and fusion will be considered. In terms of position, abnormalities include non-rotation, mal-rotation, and ectopia (under-ascent or over-ascent). Renal fusion anomalies include horseshoe kidneys and crossed renal fused ectopic kidneys. It is noteworthy that these kidneys often have a higher stone formation rate as compared to normal kidneys due to aberrant renal anatomy, altered drainage (renal pelvis in abnormal location, ureter being inserted in high position), and recurrent infections. 2 Stones in anomalous kidneys do not differ from normal kidney stones and calcium oxalate is present as a major constituent of these. 3
The approaches to managing these kidney stones are not straightforward and often can be confusing as there are no specific algorithms and often the surgeon needs to manage each case individually.4,5 In this review, the main aim was to perform a narrative review of stone management in common types of anomalous kidneys.
Materials and methods
Evidence acquisition
Inclusion criteria included – stone management in anomalous kidneys including
Horseshoe kidneys (HSK),
Crossed fused renal ectopia (CFRA),
Mal-rotated kidneys (MRK), and
Pelvic kidneys (PK).
Exclusion criteria included the following:
Stone management in other CAKUT anomalies other than the above four.
Studies with less than 20 patients, and
Studies with patients aged less than 18.
Search strategy
We followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA). National Library of Medicine (PubMed/Medline), Elsevier, and Google Scholar databases were electronically searched with the terms ‘Anomalous Kidneys’, ‘Stones’, ‘Horseshoe kidneys, ‘Malrotated kidneys, ‘pelvic ectopic kidneys’, ‘crossed ectopic kidneys’, ‘crossed fused renal ectopia’, ‘Percutaneous Nephrolithotomy’, ‘Ureteroscopy’, ‘Extracorporeal shockwave lithotripsy’, ‘Laparoscopy’. Boolean operators were used including and/or.
Study selection
We used Rayyan software (a free web tool designed to help researchers speed up the process of screening and selecting studies) to aid in the process of duplicate removal, and initial screening, and facilitate author collaboration. After deleting duplicates, following the inclusion and exclusion criterion, studies were shortlisted. Full-text papers of the shortlisted studies were reviewed by the SQ3R (Survey, Question, read, recite, review) technique.
Data extraction
The data extraction was carried out in two parts: surgical procedures and stone management in anomalous kidneys and different approaches to stones in a particular abnormality.
Results
Study selection results
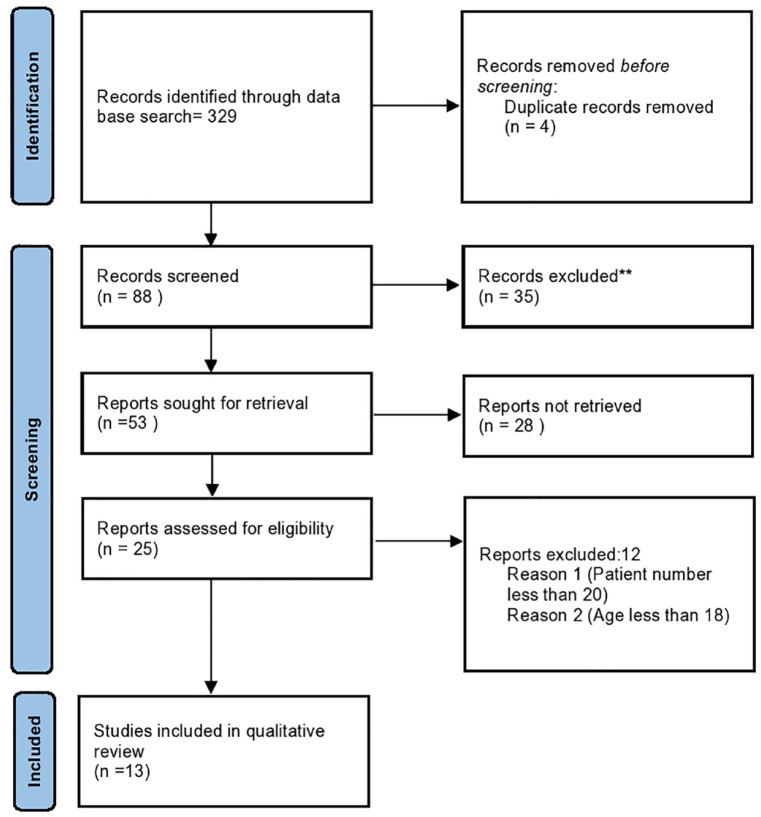
In the initial search, 327 studies were identified. After removing duplicates and unrelated studies, a total of 186 studies were shortlisted. Finally, 51 studies were screened, 28 were excluded, and 23 were assessed for eligibility. After applying the exclusion criterion, 11 studies were included in the review. The PRISMA flow chart is provided in Figure 1.
Figure 1.
PRISMA flowchart.
PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-analyses.
Study characteristics
Studies were grouped based on the study’s aim, methodology used, and total number of studies. The summary is given in Table 1.
Table 1.
Study characteristics.
| Study aim | Methodology | Number |
|---|---|---|
| RIRS in anomalous kidneys | Retrospective | Total 3, including 1 review |
| PCNL in anomalous kidneys | Retrospective | Total 2 |
| ESWL in anomalous kidneys | Retrospective | Total 2 |
| Comparative studies in stone management in anomalous kidneys | Retrospective | Total 2 |
| Stone management in HSK | Retrospective | Total 3, including 1 review |
| Stone management in CFRE | Retrospective | Total 1, review |
CFRE, crossed fused renal ectopia; ESWL, extracorporeal Shockwave lithotripsy; HSK, horseshoe kidneys; PCNL, percutaneous nephrolithotomy; PK, pelvic kidneys; RIRS, retrograde intra-renal surgery.
Surgical approaches to stone management in anomalous kidneys
RIRS in anomalous kidney stone management
A recent study of 414 patients has found that retrograde intra-renal surgery (RIRS) in patients with anomalous kidneys is a safe and effective treatment with an acceptable complication rate in experienced hands. 6 A review including 14 studies, with 413 patients has found that RIRS was able to achieve an initial stone-free rate (SFR) in the range of 76.6% (n = 322) and a final SFR in the range of 82.3% (n = 340), associated with the low risk of major complications (only 2.4% were Clavien–Dindo ⩾ III). 7 In another study, including 25 patients, the results were similar with good SFR and minimal complications. 8 Table 2 summarizes these results.
Table 2.
RIRS/ureteroscopy in anomalous kidney stone management.
| Study | Characteristics | Procedure/results | Conclusion |
|---|---|---|---|
| Garcia (2021) 6 | Aim To analyze the trends and outcomes of RIRS (retrograde intrarenal surgery) for the treatment of urolithiasis in anomalous kidneys in a large international multicenter series. Study Retrospective-multicentric |
Patients 414, males = 227, females = 137 HSK = 119, EK = 102, MRK = 69, Diverticular calculus = 50 Stone characteristics Size Avg. 13.9 mm (±6) Procedure In 249 cases (60.14%), a disposable scope was used, and a reusable scope in 165 (39.85%) cases A preoperative stent was reported in 46.6% UAS was used in 90% of cases Holmium: Yttrium-almuniuim-garnet laser was used in 391 (94.4%) patients and a thulium fiber laser in 23 (5.6%) The mean operative time was 65.3 min Post-op stenting was performed in 392 (94.7%) patients Our series had a single-stage SFR of 79.2% Complications Hematuria (10.9%), upper urinary tract perforation, or a ureteral injury 1.9% and 1.7%, respectively Surgery abandonment in 4.3% |
RIRS in patients with anomalous kidneys is a safe and effective treatment with an acceptable complication rate in experienced hands. The SFR is expected to be high when careful case selection is made and when patients are treated in high-volume centers with experienced surgeons |
| Lavan (2019) 7 | Aim Role of ureteroscopy in the management of stones in anomalous kidneys Study Systemic review 14 Studies, 13 retrospectives, 1 prospective |
Patients 413 (30.5) had a previous endourological procedure HSK = 204, EK = 117, MRK = 86, CFRE = 2, Others = 4 Stone characteristics Size Avg. 16 mm Stone location (lower pole 34.6%, pelvic 31%, multiple locations 18.9%) Procedure Ureteroscopies only Flexible URS was used in 90% of cases A preoperative stent was reported in 26.4% UAS was reported in 11 studies Holmium laser was used in 12 out of 13 studies The mean operative time was 61.3 min (range: 14–185 min) Post-op stenting was done in all patients in 6 studies in others it was variable (46.2–84%) The initial and final SFR was 76.6% (n = 322) and 82.3% (n = 340), respectively Overall, 71 (17.2%) Complications Complications were reported of which 61 (14.8%) were Clavien–Dindo ⩽ II, and 10 (2.4%) were Clavien–Dindo ⩾ III |
Ureteroscopy in patients with anomalous kidneys can be technically challenging, advancements in endourological techniques have made it a safe and effective procedure. In these patients, the stone-free rates are good with a low risk of major complications |
| Ugurlu (2014) 8 | Aim Ureteroscopy in the management of anomalous kidney stones Study Retrospective |
Patients 25 (17 males, 8 females) Lumbar ectopic: 7, pelvic ectopic: 6, HSK: 3, mal-rotated kidney: 4, CFRE: 1, Others: 4 Stone characteristics Size 194.4 mm2 Location (lower calyx 14, middle calyx 4, upper calyx 7, pelvis 7) Procedure RIRS with holmium laser Complications Renal colic/urosepsis/pyelonephritis (1 each case) |
F-URS with holmium laser lithotripsy is a very effective therapy for most stones in anomalous kidneys due to its less invasive nature, repeatable applicability, and acceptable complication rates |
CFRE, crossed fused renal ectopia; EK, ectopic kidney; ESWL, extracorporeal shock wave lithotripsy; HSK, horseshoe kidneys; MRK, Mal-rotated kidneys; RIRS, retrograde intra-renal surgery; UAS, ureteral access sheath; URS, ureterorenoscopy.
PCNL in anomalous kidney stone management
Percutaneous nephrolithotomy (PCNL) is often used in surgical procedures in patients with anomalous kidneys; however, it often requires careful preoperative planning and may even need close collaboration with other branches like radiology. Although the complication rate may be more than RIRS and in PKs, laparoscopic-assisted PCNL may be indicated, PCNL is the choice of treatment in stones with sizes >2 cm.9,10 Summarized results are shown in Table 3.
Table 3.
PCNL in anomalous kidney stone management.
| Study | Characteristics | Procedure/results | Conclusion |
|---|---|---|---|
| Prakash (2017) 10 | Aim PCNL in anomalous kidneys Study Retrospective |
Patients Patients 86 Male/female: 58/28 Bifid system: 40 HSK: 20, MRK: 8, PK: 8, CFRE: 4, crossed ectopia: 6 Stone characteristics Size: 4.4 cm ± 1.6 Location: pure pelvic 50, calyceal 26, complex 15 Procedure PCNL Complications Clavien–Dindo Grade 1–16, Grade 2–15, Grade 3–0, Grade 4–3 |
PCNL in the anomalous kidney is a safe and feasible procedure like a normally located kidney but requires careful preoperative planning and one has to be vigilant for all possible intraoperative and postoperative complications |
| Gupta (2009) 9 | Aim PCNL in anomalous kidneys Study Retrospective |
Patients Patients 46 (52 renal units) Male/female: 28/18 HSK: 31, MRK: 7, PK: 4, CFRE: 4 Stone characteristics Size: 2.4 cm, Avg. Location: pure pelvic 26, pelvicalyceal 14, calyceal 12 Procedure PCNL/Relook PCNL in 7 Complications Minimal |
PCNL is technically very challenging in anomalous kidneys because the abnormal pelvicalyceal system results in difficulty in access. We recommend PCNL as the modality of choice for anomalous kidneys with larger stones (2 cm) or ESWL refractory stones. Laparoscopic assistance improves the safety of PCNL in pelvic ectopic kidneys and should be used for such conditions |
CFRE, crossed fused renal ectopia; HSK, horseshoe kidneys; MRK, Mal-rotated kidneys; PCNL, percutaneous nephrolithotomy; PK, pelvic kidney.
ESWL in anomalous kidney stone management
Extracorporeal shockwave lithotripsy (ESWL) is still one of the modalities being used in patients with stones in anomalous kidneys. Studies have revealed that it can be used effectively in stones with <20 mm but the number of sessions may range somewhat between 1 and 6.11,12 Renal colic was reported to be the most common complication in these two studies. In addition to stone size, stone burden, and location, drainage along with the degree of the anomaly has been found to impact treatment success with ESWL.11,12 Summarized results are given in Table 4.
Table 4.
ESWL in anomalous kidney stone management.
| Study | Characteristics | Procedure/results | Conclusion |
|---|---|---|---|
| Tunc (2004) 11 | Aim ESWL in anomalous kidneys Study Retrospective |
Patients 150 (93 males and 57 females) Duplex kidneys: 57, HSK: 45, MRK: 30, PK/CRE:14 Stone characteristics Size: 10–30 mm average Site: upper calyx: 10, middle calyx: 5, lower calyx: 14, renal pelvis: 55, multi-calyceal 27, Others ureteric 39 Procedure Shock Wave Lithotripsy with sessions varying from 1 to 4, SFR 1 session in 58% and 4 sessions in 19% Complications Renal colic in 40 (26.6%) patients, Acute pyelonephritis in eight (5.3%) cases and stone-street formation in six (4%) |
In conclusion, considering the low morbidity and high success rate, SWL is an effective method for stones < 20 mm in all anomalous kidneys, with stone burden, stone localization, and severity of the anomaly seeming to be the main parameters impacting treatment success |
| Sheir (2003) 12 | Aim ESWL in anomalous kidneys Study Retrospective |
Patients 198 (169 males and 29 females) HSK: 49, MRK: 120, Duplex: 29 Stone characteristics Size: 11–20 mm average Site: upper calyx: 16, middle calyx: 16, lower calyx: 70, renal pelvis: 71, multi-calyceal 25 Procedure SWL with sessions varying from 1 to 6 1 session in 35% and 6 sessions in 5.6% Complications Hematuria, renal colic, Steinstrasse, no perirenal hematoma |
ESWL is an effective and reliable treatment method in patients with congenital urinary system anomalies. Stone burden (size and number) is the most significant factor influencing the stone-free rate. ESWL should be the primary method of therapy in such patients, especially when the stones are <20 mm. The use of prone positioning may facilitate stone localization, and the use of second-generation lithotripters improves the treatment of these patients with multiple sessions |
CFRE, crossed fused renal ectopia; EK, ectopic kidney; ESWL, extracorporeal shock wave lithotripsy; HSK, horseshoe kidneys; MRK, Mal-rotated kidneys; PCNL, percutaneous nephrolithotomy; PK, pelvic kidney; RIRS, retrograde intra-renal surgery; SFR, stone-free rate; URS, ureterorenoscopy.
Comparison of different techniques in anomalous kidney stone management
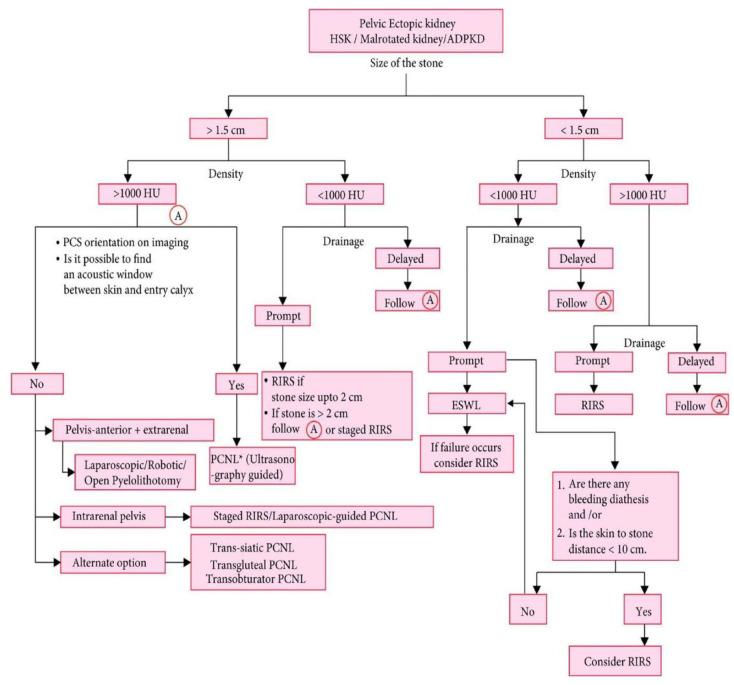
A recent study comparing different techniques has revealed that RIRS, PCNL, and laparoscopy are effective ways of managing stones in anomalous kidneys but RIRS is safe and satisfactory with small- and medium-sized calculi. 4 However, a more recent study comparing different techniques has found that stone size (</>1.5 cm), stone density (</>1000 HU) [and kidney anatomy (regarding drainage) are essential in determining the management of stones in these kidneys]. 2 In the same study, they provided an algorithm for the management of these kidney stones (Figure 2). A multi-centric study in 2022 has concluded that both PCNL and RIRS are safe and feasible options in any anomaly, but PCNL provides better SFR, especially in HSK and ectopic kidneys and those with higher stone volumes. 13 Summarized results are given in Table 5.
Figure 2.
Algorithm for an approach to stones in anomalous kidneys.
Table 5.
Comparative of surgical approaches for the management of stones in anomalous kidneys.
| Study | Characteristics | Procedure/results | Conclusion |
|---|---|---|---|
| Lim (2022) 13 | Aim To propose a framework that can aid urologists in making an informed choice between PCNL and RIRS in urolithiasis in anomalous kidneys Study Retrospective, 20 centers globally based on propensity score-matched pair analysis. (PSM) |
Patients Overall cohort Of the 569 patients, (males: 418, females: 151) HSK-288, EK-129, MRK-152 PSM Group – PCNL versus RIRS Of the 254 patients, (males: 200, females: 54) HSK-153, EK-42, MRK-59 Stone characteristics Size: single stone < 2cm – 230, single stone > 2 cm – 132, multiple stones – 207 PCM group – PCNL versus RIRS Size: single stone < 2 cm – 97, single stone > 2 cm – 45, multiple stones – 112 Procedure Overall: PCNL – 261, RIRS-308 PSM Group: PCNL – 12, RIRS-127 Complications Overall: sepsis – 9%, hematuria – 5.8%, operation abandonment – 2.75% PSM group: sepsis – 8%, hematuria – 4%, operation abandonment – 6.3% |
This study highlights that both PCNL and RIRS are safe and feasible options in any anomaly but PCNL provides better SFR especially in HSK and ectopic kidneys and those with higher stone volumes |
| Singh (2018) 2 | Aim Algorithm approach to compare different procedures for stones in anomalous kidneys Study Retrospective |
Patients Of the 179 patients, (males: 129, females: 50) 199 Renal units – HSK-85, PK+ Others – 47, MRK-33, ADPKD-14 Stone characteristics Size: 67–454.7 mm2 DSA (Avg. 204.36 mm2) Location: Pelvis: 90, calyxes: 66, Pelvis+ calyx: 27, Ureteric: 10 Procedure HSK: 10 RIRS; 67 PCNL; 7 ESWL 7; 1 LP MRK: 13 RIRS; 17 PCNL; 2 ESWL; 1 LP PK: 16 RIRS, 29 PCNL; 2 ESWL ADPKD: 3 RIRS; 6 PCNL; 3 ESWL; 2 LP Complications Scored 1–3 on CD Score, none had CD 4 complication |
The algorithm approach to stones was devised based on stone size (more or less 1.5 cm), density (more or less 1000 HU), and drainage of anomalous kidneys |
| Ergin (2017) 4 | Aim Compare different procedures Study Retrospective |
Patients Of the 178 patients (males: 110, females: 60) HSK-96, PK-42, MRK-40 Stone characteristics Size: 13.4–28.4 mm (Avg. 18.7 mm) Location: Pelvis: 79, upper calyx: 28, middle calyx: 36, lower calyx: 76 Procedure HSK: 36 RIRS; 60 PCNL MRK: 32 RIRS; 8 PCNL PEK: 33 RIRS, 9 Lap. Pyelolithotomy Complications Minimal with Laparoscopic procedure |
PCNL, laparoscopic pyelolithotomy, and RIRS are useful and effective treatment modalities for urinary stones in kidneys with abnormal anatomy. According to the results of our study, RIRS is safer and a more satisfactory minimally invasive modality, and it could be used in these kidneys with small- and medium-sized calculi |
ADPKD, adult polycystic kidney disease; CD, Clavien–Dindo complications; EK, ectopic kidney; ESWL, extracorporeal shock wave lithotripsy; HSK, horseshoe kidneys; LP, laparoscopic pyelolithotomy; MRK, Mal-rotated kidneys; PCNL, percutaneous nephrolithotomy; PK, pelvic kidney; RIRS, retrograde intra-renal surgery; SFR, stone-free rate; URS, ureterorenoscopy.
Stone management in horseshoe kidneys
Two recent studies have compared different techniques for the management of stones in HSK patients. One study compared RIRS with ESWL for stones in HSK management. This study established that RIRS is a feasible and sufficient option for stone management in HSK patients with sizes less than 2 cm. 14 In another study, RIRS was compared to PCNL in HSK patients with stones, they concluded that RIRS had almost similar stone clearance as that of PCNL with minimal complications. 15 Summarized results are given in Table 6.
Table 6.
Stone management in HSK.
| Study | Characteristics | Procedure/results | Conclusion |
|---|---|---|---|
| Chen (2019) 14 | Aim URS versus ESWL in HSK for stones less than 2 cm in size Study Review, four retrospective studies |
Patients 127 (HSK only) Stone size Less than 2 cm Procedure ESWL = 62, URS = 67 Complications All studies reported no severe complications. However, renal colic episodes are more likely to occur in the SWL group |
For a stone <2 cm in HSK, ESWL, and URS are both safe treatment modalities URS alone is a more feasible and sufficient option for stone in HSK than ESWL with the possibility of a second session |
| Kartal (2019) 15 | Aim URS versus PCNL in HSK Study Retrospective |
Patients 49 patients (41 males, 8 females) Stone size 22.3–24.5 mm Stone location Pelvis: 15, calyx: 22, pelvis + calyx: 12 Procedure PCNL = 21 URS = 28 Complications CD grade 1–3, 14 patients CD grade 4, 1 patient |
Renal stones in the HSK anomaly can be treated with high rates of success using PCNL in a single session, and a similar success rate can be achieved by RIRS with acceptable re-treatment rates. Moreover, RIRS may be chosen to avoid complications associated with PCNL due to the minor character of the associated complications and its safe use on renal stones in the HSK anomaly |
CD, Clavien–Dindo complications; ESWL, extracorporeal shock wave lithotripsy; HSK, horseshoe kidneys; PCNL, percutaneous nephrolithotomy; RIRS, retrograde intra-renal surgery; SFR, stone-free rate; URS, ureterorenoscopy.
Stone management in crossed-fused renal ectopia
A single study, reviewing 35 CFRE cases with stones reported in the literature, has found that all methods have been used for management including open surgery as well. 16 Summarized results are given in Table 7.
Table 7.
Stone management in CFRE.
| Study | Characteristics | Procedure/results | Conclusion |
|---|---|---|---|
| Cao (2019) 16 | Aim Analysis of 35 cases of CFRE with stones Study Retrospective |
Patients 35 patients (the female-to-male ratio was 10:21) Site of fusion The ratio of the side of the ectopic kidney was 13:20 (left:right) Treatment options Open surgery in 4 patients, conservative therapy in 5, ESWL in 7, PCNL in 10, RIRS in 4 and laparoscopic pyelolithotomy in 1 However, the treatment method in five cases was not mentioned, and in three patients, ESWL failed, and a second surgery was required |
The choice of treatment in CFRE with stones relies on the vascular anatomy, the size of the stones, the extent of hydronephrosis, and the experience of the urologist |
CFRE, crossed fused renal ectopia; ESWL, extracorporeal shock wave lithotripsy; PCNL, percutaneous nephrolithotomy; RIRS, retrograde intra-renal surgery; URS, ureterorenoscopy.
Discussion
Congenital malformations of the urogenital system at birth account for about 10%. 17 Approximately 50% of these involve upper urinary tract abnormalities. 18 Of the various upper urinary tract anomalies, abnormalities of the kidney are predominant accounting for 20–30% of all detectable anomalies. 19 The prevalence of stones in anomalous kidneys is significantly higher compared to the general population. 5 However, the mechanism or mechanisms leading to the increased prevalence of stones in anomalous kidneys are not fully elucidated. However, urinary stasis appears to be the most common factor leading to increased stone formation in these anomalies. 20 Surgical intervention remains the most effective therapeutic intervention in managing symptomatic kidney stones. In the past, options were limited to open nephrolithotomy; however, it has since been superseded by minimally invasive methods such as PCNL, ESWL, and ureteroscopy/ureterorenoscopy (URS) However, at present still there is no clear superiority of one method over the other in treating stones in individuals with CAKUT. Often the treatment has to be innovative and individualized for the given patient. Although CAKUT includes a spectrum of abnormalities including the kidney’s number, ascent, form and fusion, ascent, rotational anomalies, renal vasculature, and the renal collecting system. 21 However, this review focused on those anomalies which are commonly encountered clinically.
HSK is present in 1 in 400–1600 births and is the most common renal fusion abnormality. 22 The incidence of stones in adult patients with HSK is as high as 36%.23,24 CFRE malformation of the kidney is estimated in autopsies in the range of 1 in 1000–2000 and about ~0.01% of live births. 25 From studies, only 35 patients with crossed renal ectopia having stones have been reported. 16 MK occurs in about 1 in 939 autopsies. It is further classified into non-rotation, incomplete rotation, reverse rotation, transverse rotation, or excessive rotation. 26 PK incidence is in the range of 1 in 5000 patients. Most of these patients remain asymptomatic, and clinical recognition is seen in the range of 1–10,000. 26
Although a multitude of studies are available dealing with the same topic, due to the heterogeneity of clinical presentation and non-availability of randomized controlled trials in anomalous kidneys, there is a lack of a consensus on an approach to stone management in such kidneys. 13
We found more and more cases can be managed with RIRS with minimal morbidity particularly if the size of stones is <20 mm. The advances in endourological instrumentation include smaller diameter disposable flexible ureteroscopes and advances in lasers, RIRS is considered an attractive option in challenging stone cases associated with anomalous kidneys. 13 PCNL still has a vital role in stones with sizes more than 20 mm. A recent multi-centric study concluded that both PCNL and RIRS are safe and feasible options in any anomaly, but PCNL provides better SFR, especially in HSK and ectopic kidneys and those with higher stone volumes. 13
It was also obvious that ESWL is not being employed for such stones with much enthusiasm. The reason was not clear, but it appears it is because of the overall decreased usage of ESWL in the management of kidney stones rather than his subset of patients. We found the algorithmic approach recommended in one of the comparative studies very useful for approaching these stones (Figure 2).
This literary review reveals that the approach to stones in anomalous kidneys is not straightforward and depends on multiple factors – anatomy of the kidney, stone location, stone size, stone density, and expertise available (both urological as well as radiological). As such, each case needs to be approached individually and planned carefully.
This review has many limitations. The studies/reviews involved are based mostly on retrospective data. The clinical entities as well as the procedures employed and differences in approaches are also variable and difficult to standardize. Also, some of the data used for some rare conditions is very old due to the rarity of anomalies.
Conclusion
We conclude that stones in anomalous kidneys can be challenging but can be managed safely. There is no straightforward answer to the right technique but rather the right planning based on the anatomy of the kidney in terms of vascularity and drainage, stone size and density, and expertise available. We found RIRS is a feasible approach in the majority of stones with sizes <20 mm and PCNL holds the upper hand in stones >20 mm. However, ESWL, laparoscopy, and robotics do have their places in the management of some of these cases.
Supplemental Material
Supplemental material, sj-docx-1-tau-10.1177_17562872231217797 for Challenges and options for management of stones in anomalous kidneys: a review of current literature by Mudassir Wani, Ahmed Haider Abdalla Mohamed, Gareth Brown, Seshadri Sriprasad and Sanjeev Madaan in Therapeutic Advances in Urology
Acknowledgments
None.
Footnotes
ORCID iDs: Mudassir Wani  https://orcid.org/0000-0001-8940-2310
https://orcid.org/0000-0001-8940-2310
Sanjeev Madaan  https://orcid.org/0000-0003-4220-5613
https://orcid.org/0000-0003-4220-5613
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Mudassir Wani, Department Of Urology, Cardiff, and Vale University Health Board, Cardiff, UK; Canterbury Christ Church University Faculty of Social and Applied Sciences, Chatham, UK.
Ahmed Haider Abdalla Mohamed, Department of Urology, Dartford, and Gravesham NHS Trust, Dartford, UK; Canterbury Christ Church University Faculty of Social and Applied Sciences, Chatham, UK.
Gareth Brown, Department of Urology, Royal Glamorgan Hospital, Rhondda Cynon Taff, UK.
Seshadri Sriprasad, Department of Urology, Dartford, and Gravesham NHS Trust, Dartford, UK; Canterbury Christ Church University Faculty of Social and Applied Sciences, Chatham, UK.
Sanjeev Madaan, Department of Urology, Dartford, and Gravesham NHS Trust, Darent Valley Hospital, Darenth Wood Road, Dartford, DA2 8DA, UK; Canterbury Christ Church University Faculty of Social and Applied Sciences, Chatham ME4 4UF, UK.
Declarations
Ethics approval and consent to participate: Not applicable.
Consent for publication: Not applicable.
Author contributions: Mudassir Wani: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Project administration; Resources; Software; Validation; Visualization; Writing – original draft; Writing – review & editing.
Ahmed Haider Abdalla Mohamed: Conceptualization; Investigation; Project administration.
Gareth Brown: Project administration; Supervision; Validation; Writing – review & editing.
Seshadri Sriprasad: Conceptualization; Project administration; Supervision; Validation.
Sanjeev Madaan: Project administration; Supervision; Validation; Writing – review & editing.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
The authors declare that there is no conflict of interest.
Availability of data and materials: Not applicable.
References
- 1. Matlaga BR, Assimos DG. Changing indications of open stone surgery. Urology 2002; 59: 490–493. [DOI] [PubMed] [Google Scholar]
- 2. Singh AG, Jairath A, Balaji SS, et al. Changing trends in the endourological management of urolithiasis in anomalous kidneys. BJU Int 2018; 123: 318–327. [DOI] [PubMed] [Google Scholar]
- 3. Gupta M, Lee MW. Treatment of stones associated with complex or anomalous renal anatomy. Urol Clin N Am 2007; 34: 431–441. [DOI] [PubMed] [Google Scholar]
- 4. Ergin G, Kirac M, Unsal A, et al. Surgical management of urinary stones with abnormal kidney anatomy. Kaohsiung J Med Sci 2017; 33: 207–211. [DOI] [PubMed] [Google Scholar]
- 5. Raj GV, Auge BK, Assimos D, et al. Metabolic abnormalities associated with renal calculi in patients with horseshoe kidneys. J Endourology 2004; 18: 157–161. [DOI] [PubMed] [Google Scholar]
- 6. García Rojo E, Teoh JY, Castellani D, et al. Real-world global outcomes of retrograde intrarenal surgery in anomalous kidneys: a high volume international multicenter study. Urology 2022; 159: 41–47. [DOI] [PubMed] [Google Scholar]
- 7. Lavan L, Herrmann T, Netsch C, et al. Outcomes of ureteroscopy for stone disease in anomalous kidneys: a systematic review. World J Urol 2019; 38: 1135–1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ugurlu İM, Akman T, Binbay M, et al. Outcomes of retrograde flexible ureteroscopy and laser lithotripsy for stone disease in patients with anomalous kidneys. Urolithiasis 2014; 43: 77–82. [DOI] [PubMed] [Google Scholar]
- 9. Gupta NP, Mishra S, Seth A, et al. Percutaneous nephrolithotomy in abnormal kidneys: single-center experience. Urology 2009; 73: 710–714. [DOI] [PubMed] [Google Scholar]
- 10. Prakash G, Sinha R, Jhanwar A, et al. Outcome of percutaneous nephrolithotomy in anomalous kidney: is it different? Urol Ann 2017; 9: 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tunc L, Tokgoz H, Tan MO, et al. Stones in anomalous kidneys: results of treatment by shock wave lithotripsy in 150 patients. Int J Urol 2004; 11: 831–836. [DOI] [PubMed] [Google Scholar]
- 12. Sheir KZ, Madbouly K, Elsobky E, et al. Extracorporeal shock wave lithotripsy in anomalous kidneys: 11-year experience with two second-generation lithotripters. Urology 2003; 62: 10–15. [DOI] [PubMed] [Google Scholar]
- 13. Lim EJ, Teoh JY, Fong KY, et al. Propensity score-matched analysis comparing retrograde intrarenal surgery with percutaneous nephrolithotomy in anomalous kidneys. Minerva Urol Nephrol 2022; 74: 738–746. [DOI] [PubMed] [Google Scholar]
- 14. Chen H, Chen G, Pan Y, et al. No wound for stones <2 cm in horseshoe kidney: a systematic review of comparative studies. Urol Int 2019; 103: 249–255. [DOI] [PubMed] [Google Scholar]
- 15. Kartal I, Çakıcı MÇ, Selmi V, et al. Retrograde intrarenal surgery and percutaneous nephrolithotomy for the treatment of stones in horseshoe kidney; what are the advantages and disadvantages compared to each other? Cent European J Urol 2019; 72: 156–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cao Y, Zhang Y, Kang W, et al. Crossed-fused renal ectopia with renal calculi: two case reports and a review of the literature. Medicine (Baltimore) 2019; 98: e18165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Guarino N, Tadini B, Camardi P, et al. The incidence of associated urological abnormalities in children with renal ectopia. J Urol 2004; 172: 1757–1759. [DOI] [PubMed] [Google Scholar]
- 18. Macksood MJ, James RE., Jr. Giant hydronephrosis in ectopic kidney in a child. Urology 1983; 22: 532–535. [DOI] [PubMed] [Google Scholar]
- 19. Stonebrook E, Hoff M, Spencer JD. Congenital anomalies of the kidney and urinary tract: a clinical review. Curr Treat Options Pediatr 2019; 5: 223–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gambaro G, Fabris A, Puliatta D, et al. Lithiasis in cystic kidney disease and malformations of the urinary tract. Urol Res 2006; 34: 102–107. [DOI] [PubMed] [Google Scholar]
- 21. Wein AJ. Campbell-Walsh urology. 10th ed. Philadelphia: Elsevier Inc, 2012, p. 3123. [Google Scholar]
- 22. Weizer AZ, Silverstein AD, Auge BK, et al. Determining the incidence of horseshoe kidney from radiographic data at a single institution. J Urol 2003; 170: 1722–1726. [DOI] [PubMed] [Google Scholar]
- 23. Pawar AS, Thongprayoon C, Cheungpasitporn W, et al. Incidence and characteristics of kidney stones in patients with horseshoe kidney: a systematic review and meta-analysis. Urol Ann 2018; 10: 87–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Huang L, Lin Y, Tang Z, et al. Management of upper urinary tract calculi in crossed fused renal ectopic anomaly. Exp Ther Med 2018; 15: 371–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lim TJ, Choi SK, You HW, et al. Renal cell carcinoma in a right malrotated kidney. Korean J Urol 2011; 52: 792–794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gleason PE, Kelalis PP, Husmann DA, et al. Hydronephrosis in renal ectopia: incidence, etiology and significance. J Urol 1994; 151: 1660–1661. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-tau-10.1177_17562872231217797 for Challenges and options for management of stones in anomalous kidneys: a review of current literature by Mudassir Wani, Ahmed Haider Abdalla Mohamed, Gareth Brown, Seshadri Sriprasad and Sanjeev Madaan in Therapeutic Advances in Urology