Abstract
Alcohol-related liver disease (ALD) is the leading indication for liver transplantation in the United States, but disparities for women with ALD exist. We sought to characterize trends in ALD hospitalizations and mortality among women. Using the National Inpatient Sample, we evaluated ALD and non-ALD discharges from 2003-2017. Multivariable logistic regression was used to evaluate mortality. ALD increased more rapidly among women, with alcohol hepatitis (AH) rising the most. When stratified by age and sex, changes in alcohol related cirrhosis (AC) and AH were greater in women in nearly all age groups. Similar increases were present when stratified by race, notably for Native American and Asian women. AH mortality increased in women in almost all age groups. While ALD remains predominantly male, discharges and mortality have disproportionately increased among women, particularly in young women and Native Americans. These findings shed light on populations in need of intensive public health interventions.
Keywords: Alcohol Related Liver Disease, Alcohol Related Hepatitis, National Inpatient Sample, Hospitalized Women
INTRODUCTION:
Alcohol-related liver disease (ALD) represents a spectrum disease ranging from fatty liver to advanced cirrhosis. ALD is now the most common indication for liver transplant in the United States (US) and represents an important public health problem.1 It is increasingly well recognized that ALD disproportionately affects women because of increased physiologic vulnerability to alcohol’s toxic effects as well as to disproportionate increases in rates of heavy alcohol use amongst women.2–4 Despite well-documented rising rates of ALD mortality among US women5, fewer studies have evaluated the intersection between sex, race, and age on ALD epidemiology and inpatient burden. Our goal was to specifically characterize the burden of ALD hospitalizations and mortality among women in the US as well as to define trends in ALD discharges and mortality for intersections of sex, age, and race.
METHODS:
This study evaluated data from the National Inpatient Sample (NIS), the largest all-payer inpatient care database in the US. Using NIS “core” and “severity” data files for years 2003 through 2017, we defined three discharge subpopulations based on ICD-9 and ICD-10 code algorithms for AC, alcoholic hepatitis (AH) and non-alcohol-related cirrhosis, as previously published6. For our primary analysis we defined total ALD discharges as a combination of AC and AH discharges. We then analyzed subpopulations of AC alone and AH alone. Weighted and unweighted counts and marginal rates of discharges and in-hospital deaths were calculated for each disease subpopulation and year and reported per 100,000 discharges or deaths per year. Weighted trends in discharges and mortality were calculated for each disease group of interest against year and also reported as discharges or deaths per 100,000 discharges or deaths per year. Logistic regression, controlling for age, insurance status, income, race/ethnicity, year and chronic liver disease complications, was used to identify associations with mortality during hospital discharges for each population. We also calculated the marginal odds ratios between each explanatory factor in the logistic regression models and in-hospital mortality. Statistical analysis was performed using R and Python. IRB approval was waived for this study.
RESULTS:
There were 382.2 discharges per 100,000 total all-cause discharges in 2003 and 358.0 discharges for every 100,000 discharges in 2017. Of all-cause discharges, 225.3 and 201.9/100,000 were women, respectively. Female ALD discharges made up 6.4 and 12.0/100,000 of the discharges in 2003 and 2017, respectively (Table 1). While ALD discharges increased among both sexes, they increased to a greater extent in women compared to men, (87.5% vs 57.8%). AH discharges rose most with a relative increase of 125.8% (16.2/100,000 in 2003 to 36.5/100,000 in 2017) for women compared to 89.4% for men. When stratified by sex and age (Figure 1), the relative changes in AC and AH discharges were greater in women compared to men across all age groups, except for AC discharges among men ≥ 65. Most notably, women <34 had a 205.8% relative increase in total ALD discharges compared to 104.5% among men. In particular, women <34 had an increase in AC discharges of 145.6% (vs 40.9% among men) and AH discharges of 264.6% (vs 167.2% among men). When stratified by race, ALD discharges were greater for women among all race/ethnicities, but particularly for Native American women with an increase of 1,014% (341 in 2013 to 3,800 in 2017) and Asian women with an increase of 234%, driven primarily by AC discharge increases (323 in 2013 to 1,080 in 2017) (Figure 1).
Table 1:
Weighted Trends in Alcohol-Related liver Disease Discharges and Deaths Over Time
| 2003 | 2017 | |||||
|---|---|---|---|---|---|---|
| Discharges | Total | % | Total | % | Absolute Change | Relative Change |
| TOTAL | 38,220,591 | 100% | 35,798,453 | −2,422,138 | −6.34% | |
| ALD | 239,807 | 0.63% | 392,980 | 1.10% | 153,173 | 63.87% |
| AC | 181,676 | 0.48% | 281,490 | 0.79% | 99,814 | 54.94% |
| AH | 58,131 | 0.15% | 111,490 | 0.31% | 53,359 | 91.79% |
| Non-AC | 190,090 | 0.50% | 335,375 | 0.94% | 145,285 | 76.43% |
| Gender | ||||||
| Female | 22,533,664 | 100% | 20,186,250 | −2,347,414 | −10.42% | |
| ALD | 63,973 | 0.28% | 119,950 | 0.59% | 55,977 | 87.5% |
| AC | 47,796 | 0.21% | 83,420 | 0.41% | 35,624 | 74.5% |
| AH | 16,177 | 0.07% | 36,350 | 0.18% | 20,353 | 125.8% |
| Non-AC | 94,147 | 0.42% | 158,230 | 0.78% | 64,083 | 68.1% |
| Male | 15,686,927 | 100% | 15,612,203 | −74,724 | −0.48% | |
| ALD | 175,834 | 1.12% | 277,530 | 1.78% | 101,696 | 57.8% |
| AC | 133,880 | 0.85% | 198,070 | 1.27% | 64,190 | 47.9% |
| AH | 41,954 | 0.27% | 79,460 | 0.51% | 37,506 | 89.4% |
| Non-AC | 95,943 | 0.61% | 177,145 | 1.13% | 81,202 | 84.6% |
| Deaths | ||||||
| TOTAL | 849,267 | 698,690 | −150,577 | −17.7% | ||
| ALD | 20,394 | 2.4% | 17,430 | 2.49% | −2,964 | −14.5% |
| AC | 18,201 | 2.14% | 14,330 | 2.05% | −3,871 | −21.3% |
| AH | 2193 | 0.26% | 3100 | 0.44% | 907 | 41.4% |
| Non-AC | 15,335 | 1.81% | 12,295 | 1.76% | −3,040 | −19.8% |
| Gender | ||||||
| Female | 431,985 | 331,730 | −100,255 | −23.2% | ||
| ALD | 5364 | 1.24% | 5265 | 1.59% | −99 | −1.9% |
| AC | 4684 | 1.08% | 4275 | 1.29% | −409 | −8.7% |
| AH | 680 | 0.16% | 990 | 0.30% | 310 | 45.6% |
| Non-AC | 6866 | 1.59% | 5550 | 1.67% | −1316 | −19.2% |
| Male | 417,282 | 366,960 | −50,322 | −12.1% | ||
| ALD | 15,030 | 3.6% | 12,760 | 3.48% | −2270 | −15.1% |
| AC | 13,517 | 3.24% | 10,650 | 2.9% | −2867 | −21.2% |
| AH | 1513 | 0.36% | 2110 | 0.57% | 597 | 39.5% |
| Non-AC | 8470 | 2.03% | 6745 | 1.84% | −1725 | 20.4% |
ALD: alcohol-related liver disease; AC: alcohol-related cirrhosis; AH: alcoholic hepatitis
Figure 1:
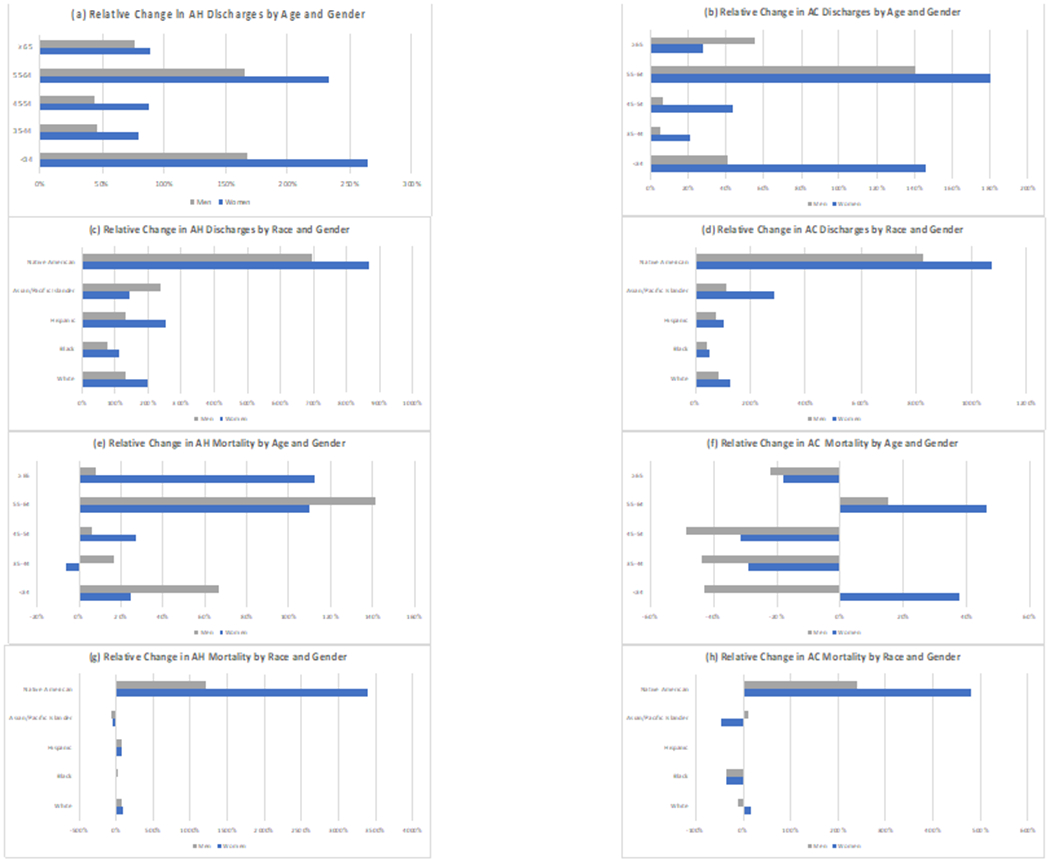
Relative Percentage Change (2003-2017) in Alcohol-Related Cirrhosis and Alcoholic Hepatitis Discharges and Mortality Stratified by Gender, Age, and Race/Ethnicity
There were 8.5 deaths for every 100,000 deaths (8.5/100,000) in 2003 and 7.0 deaths for every 100,000 deaths in 2017 (4.3 and 3.3/100,000 deaths among women) (Table 1). Total female and male ALD deaths decreased (−1.85% and −15.1%), driven by a decrease in AC deaths. AH deaths increased for both women and men (45.6% and 39.5%, respectively) (Table 1). When stratified by age (Figure 1), AH mortality increased among all age groups and sex, except women aged 35-44. AH mortality increases among women exceeded men for ages ≥65 (112.1% vs 8.2%) and 45-54 (26.9% vs 5.9%). In contrast, AC mortality decreased for all women except the ages of <34 and 55-64 (increase of 37.9% and 46.1%, respectively). When stratified by race/ethnicity, ALD mortality increased notably among the Native American populations, especially for women (594%) compared to men (318%). These rates were similar when categorized by AH and AC mortality (Figure 1). In multivariate analysis, stratified by AC vs AH, there was no significant difference in odds of death due to AH between sex (p=0.52), but there was an 8% decrease in odds of death due to AC among women compared to men (p<0.01).
DISCUSSION:
This study of the US inpatient population showed an increasing burden of ALD discharges and mortality for young women of all races/ethnicities. While ALD remains a predominantly male disease, women are catching up, as ALD discharges increased more rapidly among women compared to men. Furthermore, despite an overall decrease in AC mortality, AH mortality has been increasing in women. Significant increases in alcohol use among women may be driving these findings.4 Women are more susceptible to ALD at lower levels of consumption with more rapid development of liver disease complications and death.3 These increases in ALD discharges and AH mortality among women, if persistent, will result in increased AC deaths, suggestions that have been corroborated by projections of future ALD burden.7 Taken together, all of these findings may explain why the gap between death rates due to ALD among women and men continues to narrow.8
Similar to prior reports5, we found that AC discharges and mortality among women <34 progressed at an unprecedented rate. We noted both a marked increase in AC discharges and mortality among young women compared to men, a trend likely fed by high rates of alcohol misuse and AUD amongst high school and college age women4, 9, 10 However, despite an overall decrease in ALD mortality among older women, AH specific mortality in women >65 had a relative percentage increase of 112%, emphasizing that future public health interventions should not be limited to young women.
In our subgroup analysis, ALD discharges were greater for women among all race/ethnicities (excepting AH for Asian/Pacific Islander women). Our study not only supports previously published results that identify Hispanics as a population at substantially increased risk of developing ALD compared to non-Hispanic Whites and African Americans but sheds light on other at-risk race/ethnicities.8 In particular, we noted a dramatic relative percentage increase in both AH and AC related discharges and mortality among Native American women, both independently and compared to Native American men. While previous studies have highlighted AC and AUD as a leading cause of mortality among Native Americans, we are one of the first to highlight the increased burden of ALD among Native American women.11, 12
Our study has limitations that are inherent to the use of a large claims database. Reliance of ICD9/10 codes for identification of patients with ALD is subject to both misclassification bias and reporting error. Additionally, the NIS reports data per hospitalization and not individual, which does not allow for patient-level longitudinal analysis but does allow for more detailed analysis of inpatient burden. Our analysis is subject to confounding variables that we are unable to account for. However, our findings are in agreement with previously published epidemiological trends for AUD and ALD. The observational nature of this data is hypothesis generating and does not allow for causal inference.
In conclusion, with ALD and AUD rates climbing rapidly, a public health emergency is underway for women in the US. As the number of women with ALD continues to increase, primary preventive, gender-tailored interventions are urgently needed. Our results shed new light on subpopulations of women in need of intensive public health interventions.
Grant Support:
Dr. Mellinger is supported by an NIAAA K23 Career Development Award (AA026333).
Abbreviations:
- AC
alcohol-related cirrhosis
- AH
alcoholic hepatitis
- ALD
alcohol-related liver disease
- AUD
alcohol use disorder
- NIS
National Inpatient Sample
Footnotes
Conflicts of Interest:
MB: None
KS: None
JLM: None
References
- 1.Lee BP, Vittinghoff E, Dodge JL, et al. National Trends and Long-term Outcomes of Liver Transplant for Alcohol-Associated Liver Disease in the United States. JAMA Intern Med 2019;179:340–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guy J, Peters MG. Liver disease in women: the influence of gender on epidemiology, natural history, and patient outcomes. Gastroenterol Hepatol (N Y) 2013;9:633–9. [PMC free article] [PubMed] [Google Scholar]
- 3.Szabo G. Women and alcoholic liver disease - warning of a silent danger. Nat Rev Gastroenterol Hepatol 2018;15:253–254. [DOI] [PubMed] [Google Scholar]
- 4.Grant BF, Chou SP, Saha TD, et al. Prevalence of 12-Month Alcohol Use, High-Risk Drinking, and DSM-IV Alcohol Use Disorder in the United States, 2001-2002 to 2012-2013: Results From the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry 2017;74:911–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tapper EB, Parikh ND. Mortality due to cirrhosis and liver cancer in the United States, 1999-2016: observational study. BMJ 2018;362:k2817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mellinger JL, Shedden K, Winder GS, et al. The high burden of alcoholic cirrhosis in privately insured persons in the United States. Hepatology 2018;68:872–882. [DOI] [PubMed] [Google Scholar]
- 7.Julien J, Ayer T, Bethea ED, et al. Projected prevalence and mortality associated with alcohol-related liver disease in the USA, 2019-40: a modelling study. Lancet Public Health 2020;5:e316–e323. [DOI] [PubMed] [Google Scholar]
- 8.Yoon YH, Chen CM, Slater ME, et al. Trends in Premature Deaths From Alcoholic Liver Disease in the U.S., 1999-2018. Am J Prev Med 2020;59:469–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jones CM, Clayton HB, Deputy NP, et al. Prescription Opioid Misuse and Use of Alcohol and Other Substances Among High School Students - Youth Risk Behavior Survey, United States, 2019. MMWR Suppl 2020;69:38–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCance-Katz EF. The Substance Abuse and Mental Health Services Administration (SAMHSA): New Directions. Psychiatr Serv 2018;69:1046–1048. [DOI] [PubMed] [Google Scholar]
- 11.Sancar F, Abbasi J, Bucher K. Mortality Among American Indians and Alaska Natives. JAMA 2018;319:112. [DOI] [PubMed] [Google Scholar]
- 12.Moon AM, Yang JY, Barritt ASt, et al. Rising Mortality From Alcohol-Associated Liver Disease in the United States in the 21st Century. Am J Gastroenterol 2020;115:79–87. [DOI] [PubMed] [Google Scholar]


