Abstract
Objective Pterion is an “H” shaped formation of sutures located in the temporal fossa of the skull. It is an important anatomical landmark and a craniometric point. The thinness of the skull and its inner relation with the middle meningeal artery make this anatomical landmark clinically significant. Variations in the pterion are imperative, especially for neurosurgeons in order to have the most suitable craniometric point to be minimally invasive.
Materials and Methods One hundred pterions were studied to report the variations in the type and location of the pterion. Murphy's classification was used to classify the pterion into four types on the basis of bone articulation-sphenoparietal, frontotemporal, stellate, and epipteric.
Results All four types of pterions were observed, sphenoparietal being the most common. No significant gender difference was observed in terms of type and laterality of various pterions. The mean distance between the center of pterion to the superolateral point of zygomaticotemporal (PZT) suture and the anterolateral point of the frontozygomatic (PFZ) suture were 3.91 ± 3.79 cm and 3.68 ± 3.79 mm, respectively. Correlation analysis showed a strong positive relation between PZT and PFZ sutures.
Conclusion Accurate data on the morphology and morphometry of bony anatomical points are crucial, while performing intracranial surgery using them as recognizable landmarks. The morphometric parameters may help in determining the soundness of the pterion as an identifiable landmark for performing interventions like burr hole and other neurosurgical procedures in this area.
Keywords: cranial sutures, craniotomy, burr hole, pterion, middle meningeal artery
Introduction
Floor of the temporal fossa in the skull is formed by greater wing of sphenoid, frontal bone, parietal bone, and squamous part of the temporal bone. Here, these four bones meet at an H-shaped junction of the sutures termed the pterion. 1 2 Being covered superficially by scalp and the origin of the temporalis muscle with temporalis fascia, it is neither visible nor palpable from the surface. 3 The pterion serves as an important anatomical, surgical landmark, and craniometric point. Usually, the center of the pterion is approximately present 3.5 cm behind and 1.5 cm above the frontozygomatic suture. It is surface marked at the meeting point of a thumb behind the frontal process of the zygomatic bone and two fingers above the zygomatic arch. 4 Clinically, pterion is an important landmark as it marks the position of the anterior branch of the middle meningeal artery, lateral sulcus of the brain, and Broca's motor speech area. 5 6 Thickness of the skull in this region of the pterion is relatively less, making it a fragile point 7 a trivial blow in this region may rupture the middle meningeal artery. The topographic location of the pterion is important for a neurosurgeon in order to have the most suitable bony aperture to be minimally invasive. 6 Cosmetically also, the pterional approach is favored for its skin incision being behind the hairline, appropriate size bone flap, and the osteoplastic craniotomy preventing some of the postoperative temporalis atrophy. In the absence of neuronavigation devices to achieve optimum craniotomy, neurosurgeons have to rely on anatomical knowledge of variations in the pterion and the external landmarks around it. The pterion can be located on radiography, but the knowledge of variations in its sutural pattern is important in the interpretation of computed tomography (CT) scans and radiographs in patients presenting with traumatic head injury where the radiologists need to differentiate between sutural bones and fractures. Forensic scientists and anthropologists also use pterion as an anterolateral landmark to determine the age of skeletal remains. 8 9 Based on the articulation of constituent bones, researchers have classified the pterion into various types. The most commonly used classification is the one coined by Murphy in 1956, describes four types of the pterion: (i) sphenoparietal (SP), (ii) frontotemporal (FT), (iii) stellate (S), and (iv) epipteric (E). 10 In E variant, the Wormian bone present is also called pterion ossicle, E bone, or flower's bone. 11 These sutural bones in E type of pterion might lead to difficulty in making radiological decision. In neurosurgery, placement of a burr hole over the anterior junction of E bone for the evacuation of extradural hematoma may cause inadvertent penetration into orbit. 12
Pterion, as a neurosurgical landmark, exhibits variations in its sutural pattern and topographic location among different ethnic groups and gender. 13 Such variations are of paramount importance in clinics. In view of this, this study was undertaken to define the type and topographic location of pterion in the dry human skulls of the north Indian origin.
Materials and Methods
One hundred pterions obtained from 56 completely ossified adult skulls of unknown age and sex from south East Asian ethnicity were studied. The study protocol was reviewed and duly approved by institutional ethics committee vide reference no: AIMSR/MC/Estt/04/2k18/923. Out of 56 skulls, 44 were intact, while 12 were skull hemi sections (six of each side). The sutural pattern of pterion was carefully observed and typified using Murphy's classification. 10 According to this classification, pterion was classified into four types ( Fig. 1 ).
Fig. 1.
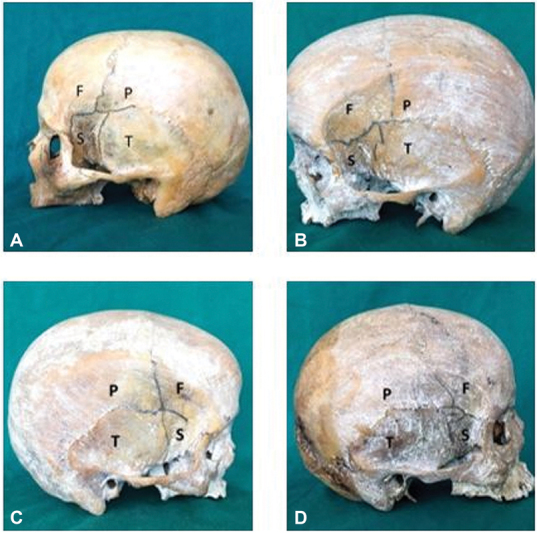
Various types of pterions as per Murphy's classification. ( A ) Sphenoparietal, ( B ) frontotemporal, ( C ) stellate, ( D ) epipteric.
(i) SP—greater wing of sphenoid articulates with parietal bones to form letter H ( Fig. 1A ).
(ii) FT—frontal and squamous part of temporal bones are in direct contact ( Fig. 1B ).
(iii) S—characterized by the articulation of frontal, parietal, temporal and sphenoid bone at a point to form letter K ( Fig. 1C ).
(iv) E—defined by the presence of a small sutural bone articulating at pterion ( Fig. 1D ).
For the morphometric measurements, the center of pterion was marked first ( Fig. 2 ). Three different readings at different points of time were taken by the same observer and the mean of them was considered as the final for data analysis ( Fig. 3 ). Digital vernier calipers (Mitutoyo Corporation, Kawasaki, Kanagawa 213-0012, Japan) with least count of 0.01 mm were used for data collection. Depending on its distance from the zygomatic arch, the pterion has been classified as high pterion (> 40 mm) and low pterion (< 40 mm) and that from frontozygomatic suture as anterior pterion (< 30 mm) and posterior pterion (> 30 mm). 14 The linear distances between the center of pterion to the most anterolateral point on frontozygomatic (PFZ) suture and to the superolateral point on zygomaticotemporal (PZT) suture were measured carefully.
Fig. 2.
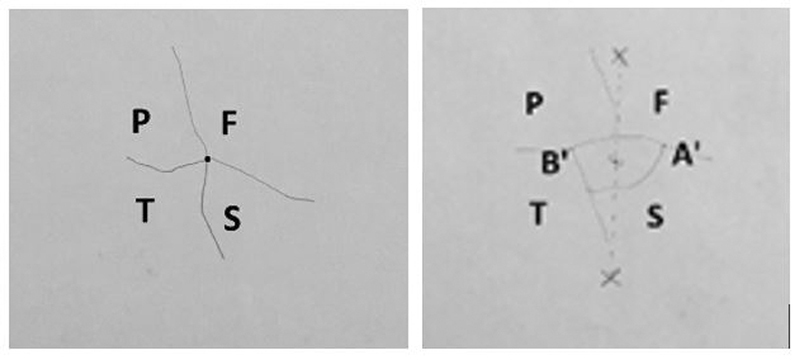
Marking of the center of stellate and epipteric pterion for morphometry.
Fig. 3.
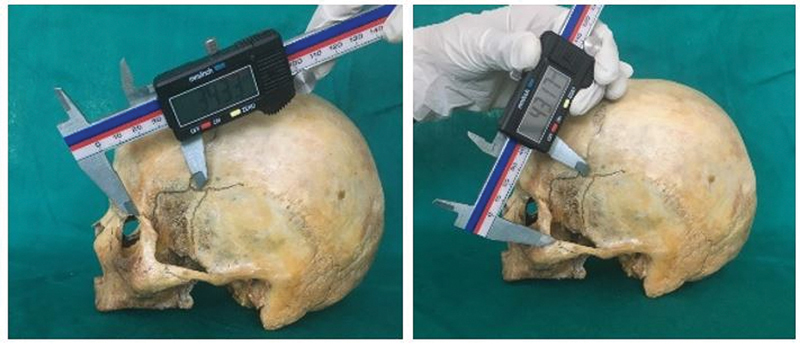
Measurements of the distance from the center of the pterion to points on the frontozygomatic and zygomaticotemporal suture.
Data Analysis
The descriptive statistics in form of mean and percentages for each measurement were carried out using Microsoft Excel 2010 version for windows. Correlation analysis was performed between PFZ and PZT sutures using the SPSS 16.0 software version for windows 10 (SPSS Inc., Chicago, Illinois, United States).
Results
All four types of the sutural pattern of pterion were observed with SP as the commonest (89%), followed by FT, S (4% each), and E as the rarest (3%). Based on the distance from the superolateral PZT suture, most of the pterions were of posterior variety, while based on the distance from the anterolateral PFZ suture, 58% were of low variety and 42% of high variety. Among 44 intact skulls, 39 (88.64%) have shown bilateral symmetry and five (11.36%) have shown asymmetry in pterion type. In asymmetrical skulls, the combination varies with SP being the most common in combination. In hemi sections, bilateral symmetry could not be determined. The linear distances (mm) between the center of pterion and defined PZT and PFZ sutures were almost the same on both sides of the skull with the right showing slightly higher values than the left side for both the landmarks. The difference in values among the sides was statistically insignificant for both distances (PZT, PFZ; Table 1 ). However, Pearson correlation analysis between PZT and PFZ sutures showed a strong correlation ( r = 0.79, p < 0.01; ( Fig. 4 ).
Table 1. Linear distance (mm) from the pterion to the points on sutures.
| Distances (in cm) | Total n = 100 |
Right side n = 50 |
Left side n = 50 |
|||
|---|---|---|---|---|---|---|
| Range | Mean ± SD | Range | Mean ± SD | Range | Mean ± SD | |
| Distance between center of pterion to superolateral PZT suture | 2.74–4.85 | 3.91 ± 3.79 | 3.36–4.85 | 3.97 ± 4.05 | 2.74–4.56 | 3.85 ± 3.45 |
| Distance between center of pterion to anterolateral PFZ suture | 2.42–4.94 | 3.68 ± 3.79 | 2.65–4.74 | 3.74 ± 4.51 | 2.42–4.94 | 3.63 ± 4.42 |
Abbreviations: PFZ, point on frontozygomatic; PZT, point on zygomaticotemporal; SD, standard deviation.
Fig. 4.
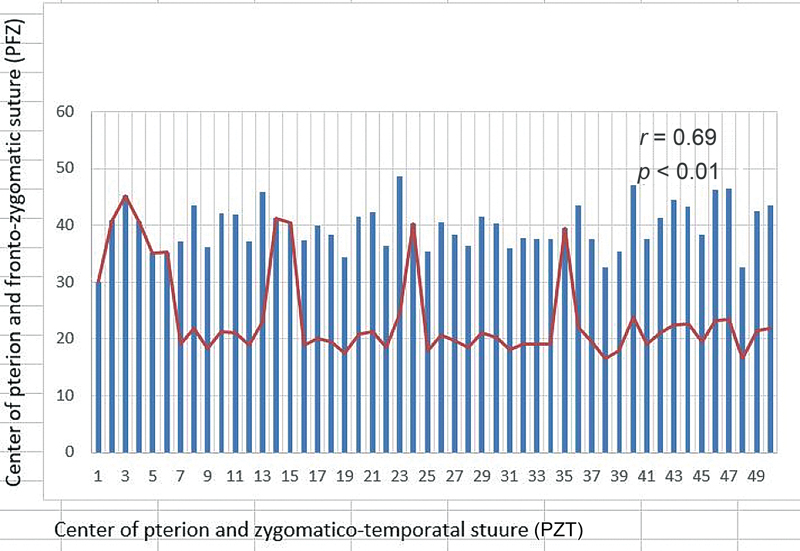
Statistical analysis showing the correlation between the distance of pterion from point of frontozygomatic (PFZ) and zygomaticotemporal (PZT) sutures.
Discussion
Pterion has always been considered a crucial anatomical surface landmark in neurosurgery. To date, various researchers have studied this sutural point to determine its morphological variations in different ethnic groups with their existing relationship to the surrounding bony landmarks ( Table 2 ).
Table 2. Comparison of the percentage of the pterion types in various population groups by various authors.
| Authors and year of study | Study population | Sample size | Type of pterion (%) | |||
|---|---|---|---|---|---|---|
| SP | FT | S | E | |||
| Saxena et al (2003) 9 | North India | 203 | 84.72 | 10.01 | 5.17 | 0 |
| Oguz et al (2004) 15 | Turkish | 26 | 88 | 10 | 0 | 2 |
| Mwachaka et al (2009) 16 | Kenya | 79 | 66 | 15 | 12 | 7 |
| Adejuwon et al (2013) 17 | Nigeria | 62 | 86.1 | 8.3 | 5.6 | 0 |
| Ruiz et al (2016) 18 | Brazil | 55 | 99 | 5 | 2 | 4 |
| Chaijaroonkhanarak et al (2017) 19 | Thai | 55 | 87.27 | 4.55 | 0 | 8.18 |
| Yameen et al (2018) 3 | North India | 35 | 98.57 | 0 | 1.4 | 0 |
| Sarvaiya et al (2019) 20 | Western India | 326 | 80.21 | 5.22 | 3.68 | 10.89 |
| Present study | North India | 100 | 89 | 4 | 4 | 3 |
Abbreviations: E, epipteric; FT, frontotemporal; S, stellate; SP, sphenoparietal.
Presently, we reported SP type of pterion in 89% of the skulls, making this the most common variety in our study population and relatively higher than the Nigerian, Kenyan, and Thai populations. 16 17 19 Interestingly, we reported all four varieties of pterion, contrary to the absence of FT, 3 E, 3 9 17 and S 15 19 types in a few populations. In the Thai population, the E type was further classified into the uniepipteric and multiepipteric on the basis of the number of interposing bones within the pterion, among which the uniepipteric was reported more frequently. 19 In this study, only uniepipteric type (3%) was reported.
Currently, the linear distances (mm) between the center pterion and defined PZT and PFZ sutures were almost the same on both sides of the skull with the right showing slightly higher values than the left side for both the landmarks. The difference in values among the sides was statistically insignificant for the both distances (PZT, PFZ). The PZT suture was nearly identical on both the right and left side. Oguz et al 15 studied 26 Turkish skulls and found the mean PZT: 3.3 ± 0.40 cm on right and 3.4 ± 0.39 cm on left, whereas PFZ suture was 4.0 ± 0.39 cm on right and 3.8 ± 0.25 cm on left. This study and most of the literature reviewed showed that this distance is slightly less or equal to 4 cm that indicates the low type of pterion to be common among populations. 14 15 21 22 In a record on the South Indian population, 14 the distance between pterion and the zygomaticotemporal suture was measured to be 4.0 ± 0.43 cm on the right side and 3.9 ± 0.36 cm on the left side, which is the highest value quoted but still falls in low type of pterion classification.
In this study, 96% of the pterions were posteriorly placed that corresponds with reports from various other ethnic groups. Sarvaiya et al 20 reported the topographic location of pterion as 3.0 ± 0.39 cm on the right side and 2.9 ± 0.38 cm on the left side from the frontozygomatic suture, which was slightly anteriorly placed in comparison to most of the studies. This may be due to a difference in the PFZ suture from where the measurements were taken. The pterion parameters in the present population differ from a few population groups and are analogous to some. Such might be due to genetic, ethnic, and environmental factors.
In present observation, approximately 90% of the pterion were of SP variety and rest make the other varieties. Moreover, this prevalence has also been maintained even in asymmetrical combinations. Also, almost 100% of the pterion in populations can be inferred to be located as low and posterior. The low type of position has been seen to be more constant because of the lesser range of variations among various populations. It lies within 3.6 to 4 cm from the palpable superior border of the zygomatic arch in most ethnic groups. The position of pterion from the palpable frontozygomatic process has been found to be mostly posterior, but it seems to be a less consistent palpable landmark as the values among populations range between 2.9 ± 0.38 and 3.8 ± 0.31 cm.
A burr hole over the SP point in FT approaches aiming to simultaneously expose the anterior and middle fossae is a safe and viable alternative. On average, this point is located 2.17 ± 0.31 cm posterior and 4.76 ± 0.17 cm superior to the frontozygomatic suture over the greater wing of the sphenoid. 23 Thus, the role of landmarks in the positioning of burr holes in relation to pterion is crucial for neurosurgeons, as they have been developing surgical approaches attempting to achieve maximal surgical exposure with minimal brain retraction.
Since the pterional approach can be modified and combined with other methods, 24 the knowledge of variations in the anatomy of pterion and its prevalence is important, especially in cases of E variety where the anterior-most point of junction of the four bones may be mistaken to be the pterion center resulting in orbital penetration. The thickness of the skull bones also shows ethnic and intersex variation. This study defines the location of the pterion center with respect to specific external landmarks in dry skulls of North Indian origin. Thorough knowledge of these dimensions will have neurosurgical implications in the resection of myriad intracranial tumors and circulatory aneurysms in this population. 23 25
Though the true determinants of the sutural pattern formed by the articulation of cranial bones are not fully known, MSX2 (on 5q35.2), a gene of the homeobox family may have some role. 26 The sutural pattern of pterion also gives a hint toward the volume of the brain as the development of the calvarium is tightly coordinated with the type of brain since the cranial sutures undergo a series of morphological changes from birth till childhood owing to the growth of the brain. 27 All these factors might cause ethnic and racial variations of sutural patterns in the skull.
Mild ethnic, genetic, and intersex variations in pterion are likely, as the breadth of the skull and the cranial index varies in diverse ethnic groups. Topography of pterion thus finds great application clinically and is used as an anterolateral landmark in “cranial suture closure methodology” for determination of age and sex. 26 28 The morphology of the pterion is therefore important for anatomists, radiologists, neurosurgeons, anthropologists, and forensic pathologists. 15 This necessitates that neurosurgeons and radiologists should know the presence and incidence of these structures in general and in their local population in particular. 8 9
Limitations
The pterion is also used for age estimation and sex determination of forensic and archaeological specimens; however, in this study, the age and sex of the dry skulls were not known, which is a limiting factor. Further, the morphometric variation in pterion needs to be explored in relation to the underlying anatomical position of the intracranial structures to help in navigating the operating instruments, which also was not taken in this study.
Conclusion
Accurate knowledge of the location of the pterion is important in relation to microsurgical interventions. Types and the position of the pterion vary among individuals and different racial groups and thus the need for accurate and up-to-date data while performing intracranial surgery guided by recognizable bony landmarks is essential. Therefore, preoperative radiographic assessment (CT images, magnetic resonance radiographs) of the pterion should be confirmed in light of the knowledge of known possible variations among populations in order to determine a safe location for performing surgical and microsurgical procedures in this area.
Funding Statement
Funding None.
Conflict of Interest None declared.
Authors' Contributions
N. Aggarwal helped in project development, data collection, and manuscript writing; Noopinder Kaur contributed to data collection and manuscript writing; A Patra was involved in data analysis and manuscript editing; Monika Gupta wrote the manuscript.
References
- 1.Seema D, Dakshayani K R, Sumanth M M. A morphometric study of pterion in adult human skulls. Int J Sci and Tech. 2013;9(01):112–115. [Google Scholar]
- 2.Snell R S. Philadelphia: Lippincott Williams & Wilkins; 2003. Clinical Anatomy by Regions. 7th ed; pp. 790–920. [Google Scholar]
- 3.Yameen M, Haider S S, Nagwani M et al. The morphological analysis of pterion in North Indian population. Eur J Med Res. 2018;5(02):1–4. [Google Scholar]
- 4.Halim A. New Delhi: CBS Publishers & Distributors; 1993. Surface and Radiological Anatomy. 2nd ed. [Google Scholar]
- 5.Bhargavi C, Saralaya V, Kishan K. Pterion. A site for neurosurgical approach. Int J Biomed Res. 2011;2(12):588–594. [Google Scholar]
- 6.Standring S, Ellis H, Healy J C, Johnson D, Williams A. Churchill Livingstone, London: Elsevier; 2005. Gray's Anatomy – The Anatomical Basis of Clinical Practice. 39th ed; pp. 455–459. [Google Scholar]
- 7.Shah A S, Shah S K, Bhaskar R et al. Morphometric study of pterion in adult dry skulls in Dakshina Kannada district Karnataka state, India. Int J Anat Res. 2015;3(04):1603–1606. [Google Scholar]
- 8.Rafi A, Sayeed S, Anwar M I. Cranial CT scan evaluation of morphological variations and location of pterion in Pakistani male population for lateral neurosurgical approach. Pak J Med Sci. 2020;36(03):310–315. doi: 10.12669/pjms.36.3.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saxena R C, Bilodi A K, Mane S S, Kumar A.Study of pterion in skulls of Awadh area–in and around Lucknow Kathmandu Univ Med J 200310132–33.(KUMJ) [PubMed] [Google Scholar]
- 10.Murphy T. The pterion in the Australian aborigine. Am J Phys Anthropol. 1956;14(02):225–244. doi: 10.1002/ajpa.1330140218. [DOI] [PubMed] [Google Scholar]
- 11.Saheb S H, Haseena S, Prasanna L C. Unusual Wormian bones at pterion – three case reports. J Biomed Sci and Res. 2010;2(02):116–118. [Google Scholar]
- 12.Kumar S, Anurag Munjal S, Chauhan P et al. Pterion its location and clinical implications – a study compared. J Evol Med Dent Sci. 2013;2(25):4599–4608. [Google Scholar]
- 13.Kamath V, Asif M, Bhat S et al. A study on the pterion position variation and its neurosurgical implications. J Anat Soc India. 2016;65(01):33–39. [Google Scholar]
- 14.Kalthur S G, Vangara S V, Kiruba L et al. Metrical and non-metrical study of the pterion in South Indian adult dry skulls with notes on its clinical importance. Marmara Med J. 2017;30:30–39. [Google Scholar]
- 15.Oguz O, Sanli S G, Bozkir M G, Soames R W. The pterion in Turkish male skulls. Surg Radiol Anat. 2004;26(03):220–224. doi: 10.1007/s00276-003-0210-2. [DOI] [PubMed] [Google Scholar]
- 16.Mwachaka P M, Hassanali J, Odula P. Sutural morphology of the pterion and asterion among the adult Kenyans. Braz J Morphol Sci. 2009;26(01):4–7. [Google Scholar]
- 17.Adejuwon S A, Olopade F E, Bolaji M. Study of the location and morphology of the pterion in adult nigerian skulls. ISRN Anat. 2013:403937. doi: 10.5402/2013/403937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ruiz C R, Souza G C, Scherb T O et al. Anatomical variations of pterion: analysis of the possible anatomical variations of pterion a human skull. J Morphol Sci. 2016;33(04):200–204. [Google Scholar]
- 19.Chaijaroonkhanarak W, Woraputtaporn W, Prachaney P et al. Classification and incidence of pterion patterns of Thai skulls. Int J Morphol. 2017;35(04):1239–1242. [Google Scholar]
- 20.Sarvaiya B J, Chaudhari J S, Fichadiya N C.Morphometric analysis of pterion in adult human dry skull in Gujarat region Int J Anat Res. 20197(1.2):6204–6210. [Google Scholar]
- 21.Gindha G S, Mir N S, Agarwal R. Morphometric study of pterion in dry human skull bone in north Indian population. Human Bio Rev. 2017;6(01):1–9. [Google Scholar]
- 22.Prasad H, Bezbaruah N K, Mishra A et al. Morphometric analysis of pterion: a clinic- anatomical study in north Indian dry skulls. Innovative Journal of Medical and Health Science. 2015;5(05):201–205. [Google Scholar]
- 23.Reis B L, Silveira R LD, Gusmão S NS. Sphenopterional point: strategic point for burr role placement in frontotemporal craniotomies. World Neurosurg. 2017;105:399–405. doi: 10.1016/j.wneu.2017.06.011. [DOI] [PubMed] [Google Scholar]
- 24.Kamath V G, Hande M. Reappraising the neurosurgical significance of the pterion location, morphology, and its relationship to optic canal and sphenoid ridge and neurosurgical implications. Anat Cell Biol. 2019;52(04):406–413. doi: 10.5115/acb.18.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.July J, Wahjoepramono E J. Singapore: Springer; 2019. Neurovascular Surgery - Surgical Approaches for Neurovascular Diseases. 1st ed. [Google Scholar]
- 26.Gupta R, Sinha M B, Aggarwal A et al. Landmarks for keyhole neurosurgical procedures through pterion. Int J Health Biomed Res. 2014;2(04):168–173. [Google Scholar]
- 27.Sindel A, Ogut E, Aytac G et al. Morphometric study of pterion. Int J Anat Res. 2016;4(01):1954–1957. [Google Scholar]
- 28.Nayak G, Mohanty B B, Das S R. Morphometric study of pterion and its clinical significance. Asian J Pharm Clin Res. 2017;10(10):142–144. [Google Scholar]


