For functional tricuspid regurgitation during mitral valve repair: Put a ring on it!
Central Message.
For patients with moderate or worse tricuspid regurgitation, tricuspid valve repair is safe, improves survival, and should be performed at the time of mitral valve surgery.
Functional, or secondary, tricuspid regurgitation (TR) is a condition that commonly accompanies mitral valve disease. Despite strong evidence for the benefit of tricuspid valve repair at the time of mitral valve surgery, adoption of concomitant tricuspid valve repair at the time of mitral valve surgery is low. Here, we provide an overview of functional TR, operative strategies to intervene on TR, and a summary of outcomes for concomitant tricuspid valve repair at the time of mitral valve surgery.
Pathophysiology, Presentation, and Diagnosis of Functional TR
Functional TR occurs in the setting of right ventricular remodeling. Right ventricular remodeling occurs due to right ventricular volume or pressure overload, such as in the setting of pulmonary hypertension and/or left-sided valve disease. Right ventricular remodeling results in tricuspid annular dilation and/or leaflet tethering with resulting TR.
Most commonly, functional TR is diagnosed by echocardiogram during evaluation of left-sided valve disease. Functional TR is typically asymptomatic until it has progressed to decreased right ventricle function. Once right ventricular dysfunction is present, patients may present with edema, abdominal fullness, fatigue, and decreased exercise tolerance. Right ventricular dysfunction can lead to end-organ damage, such as liver dysfunction and/or renal failure. Development of moderate or worse TR influences quality of life, and is an independent predictor of long-term mortality.
Natural History of TR After Mitral Valve Surgery
For many years, conservative management was believed to be the best management strategy for tricuspid valve disease.1 It was proposed that functional TR would improve on its own by fixing the mitral valve disease and removing the right ventricular volume overload.1,2 Select patients with preoperative TR may never progress to severe TR, particularly after mitral valve intervention.2 However, in patients with advanced TR and known risk factors for TR progression such as annular dilation, atrial fibrillation, and pulmonary hypertension, TR can and does persist and progress after mitral valve intervention.
In a trial by Gammie and colleagues3 randomizing patients with moderate TR to either receive a tricuspid valve repair at the time of mitral intervention or conservative management, 6% of patients who did not receive tricuspid valve repair developed severe TR at 2 years, compared with 0.6% of patients who received a tricuspid valve repair. In a review of patients undergoing mitral valve repair with a dilated tricuspid annulus, 48% of patients undergoing isolated mitral valve surgery developed worsening TR by at least 2 grades, compared with 2% of patients who had concomitant tricuspid valve repair.4 This extends beyond degenerative mitral valve disease, and in a review of patients with rheumatic mitral disease, functional TR progressed in 13% of patients.5 For most patients, mitral valve surgery does not fix functional TR.
Current Guidelines and Practice
Presently, tricuspid valve intervention is recommended at the time of left-sided valve surgery if patients have severe TR (Class 1) or progressive TR with annular dilation (>4.0 cm) and/or signs of right heart failure (Class 2a).6 The importance of intervention on the tricuspid valve has been increasingly recognized, and the rate of tricuspid valve surgery has recently increased. Indications for tricuspid valve repair at the time of left-sided valve surgery are likely expanding to include moderate TR.
Despite the evidence for the importance of tricuspid valve intervention at the time of left-sided valve surgery, concomitant adoption has been low. Rate of concomitant tricuspid repair during mitral valve surgery for patients with moderate or worse TR and/or a dilated annulus has ranged from 5% to 75%.3 Patients left with TR who later require reoperation for tricuspid valve disease have poor outcomes. Redo surgery for tricuspid valve disease is consistently among the highest-risk cardiac operations, with significant perioperative mortality ranging from 10% to 35%.3 The high-risk nature of redo surgery for tricuspid valve disease underscores the importance of tricuspid valve repair at the time of left-sided valve surgery.
Unique Consideration: Isolated Dilated Annulus With a Competent Valve
Patients with a dilated tricuspid annulus (>4.0 cm) but a competent valve are an area of controversy for tricuspid valve repair. Several groups have found that patients with an isolated dilated annulus have a higher incidence of progression of TR.4,7,8 However, other studies have found that there is no difference in long-term survival or TR progression for patients with an isolated dilated annulus with and without tricuspid annuloplasty.9 Our group routinely performs tricuspid annuloplasty for annulus >4.0 cm, regardless of the degree of TR. The role of the dilated annulus will be an area that will continue to evolve as we learn more about functional TR.
Operative Technique
Annuloplasty Strategy
Several strategies exist for tricuspid valve annuloplasty, and include suture-based annuloplasty (ie, the Kay or DeVega approach) or ring annuloplasty. Although suture annuloplasty essentially eliminates the risk of tricuspid valve endocarditis and ring dehiscence, prior work has routinely found that suture annuloplasty has a higher rate of recurrent TR than ring annuloplasty. At 15 years postoperatively, Tang and colleagues10 found that 82% of those repaired with an annuloplasty ring versus just 39% of patients repaired with a suture-based approach had freedom from recurrent TR. Because of the higher rate of recurrence with suture annuloplasty, we advocate for ring annuloplasty.
Next, surgeons must decide between a flexible and a rigid annuloplasty ring. A flexible ring reduces the dilated annulus, whereas a rigid or semirigid ring conforms the annulus to restore a more normal 3-dimensional shape.11 Although a rigid ring has been shown to reduce the motion of the annulus in a beating heart, studies have consistently found that a rigid or semirigid ring offers better freedom from recurrent TR than a flexible ring.12 Based on this evidence, we recommend placement of an annuloplasty ring, and prefer a rigid ring over a flexible ring.
Annuloplasty Stitch Placement
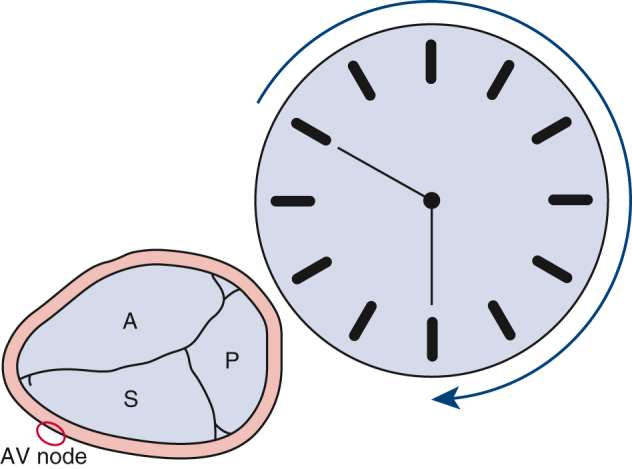
We advocate for and teach the 10-stitches-in-10-minutes approach to tricuspid valve annuloplasty. Looking at the tricuspid annulus as a clock face, from a surgeon’s view, 10 horizontal mattress stitches are placed in the annulus going from 10 o’clock to 6 o’clock (Figure 1). This approach allows placement of an annuloplasty band while widely avoiding the atrioventricular node, which is located roughly at 8 o’clock. Annuloplasty stitches must be placed in the annulus and not on the leaflet or the atria to avoid annuloplasty ring dehiscence. This standardized approach enables us to quickly teach and perform tricuspid annuloplasty, and minimizes risk of damage to the atrioventricular node.
Figure 1.
Stitches should be placed in the annulus clockwise from the 10 o’clock to 6 o’clock positions, avoiding the atrioventricular (AV) node at the 8 o’clock position. A, Anterior leaflet; P, posterior leaflet; S, septal leaflet.
Ring Size
Our group routinely does not size the tricuspid annuloplasty ring for functional TR. Instead, we always use either a size 26 mm or a size 28 mm ring.13 Prior work suggests that a normal tricuspid annular dimension is 2.8 ± 0.5 cm.14 Although it may appear that a 26 mm or 28 mm ring is undersizing the valve, for functional TR, the dilated annulus is being restored to its normal dimensions.15 There is no evidence that placement of this standard ring size leads to tricuspid stenosis.15
Leaflet Augmentation
Some groups perform augmentation of the anterior leaflet with a pericardial patch when there is significant leaflet tethering and annular dilation.16,17 Leaflet augmentation increases the zone of coaptation, which may protect against recurrent TR.16,17 There are several small case series that report on this technique describing excellent freedom from recurrent TR at midterm follow-up.16,17 However, when faced with a tricuspid valve that has such extensive disease that it requires leaflet augmentation, our group prefers to perform tricuspid valve replacement because it is a durable intervention with proven long-term outcomes.
Outcomes of Concomitant Tricuspid Valve Repair
Perioperative Outcomes
There is no increased operative mortality as a result of adding tricuspid valve repair during mitral valve surgery.8,18 In a series of 110 matched patients undergoing mitral valve repair, the operative mortality for patients undergoing isolated mitral valve repair was 8.5% versus 2% for those undergoing mitral valve repair with concomitant tricuspid valve repair (P = .20).4 Other work by Chikwe and colleagues8 similarly found that concomitant tricuspid valve repair conferred no increased risk of operative mortality. Concomitant tricuspid valve repair is safe and does not increase the risk of short-term mortality.
Pacemaker Risk
An important risk factor of tricuspid valve repair with mitral valve surgery is the risk of damage to the atrioventricular node with resulting complete heart block. The atrioventricular node is located in the triangle of Koch, which is defined by the ostium of the coronary sinus, the tendon of Todaro, and the septal leaflet of the tricuspid valve. Rate of new heart block and permanent pacemaker placement after tricuspid valve repair are highly variable, ranging from 2% to as high as 20%.19 Increased risk of pacemaker implantation may be a leading cause of low adoption of concomitant tricuspid valve repair during mitral valve surgery.
However, select high-volume centers report no increased risk of pacemaker with concomitant tricuspid repair versus mitral surgery alone.8 At our institution, pacemaker rate of mitral valve repair and concomitant tricuspid valve repair is similar to our pacemaker rate after mitral valve surgery alone.20 Our low pacemaker placement rate may be due to our operative technique, which widely avoids the atrioventricular node and our practices postoperatively, which gives patients time to recover their native rhythm. Many patients have temporary atrioventricular block postoperatively due to swelling around the atrioventricular node that resolves as the heart recovers from surgery and diuresis. Because of this, we ensure that patients are diuresed to their dry weight and typically wait at least 1 week postoperatively before evaluating a patient for pacemaker implantation. Adoption of this approach to pacemaker implantation may result in decreased pacemaker rate at other centers.
Right-Sided Remodeling
Many patients with preoperative functional TR have some degree of right ventricular dysfunction and right-sided dilation. Annular dilation seen with functional TR results in ventricular dysfunction, and TR results in a volume load of the right atrium resulting in right atrial dilation. Fortunately, tricuspid repair leads to sustained improvements in right ventricular function and can restore right-sided structures to normal dimensions.8,21 Elimination of TR removes the volume load on the right atrium, and with an annuloplasty ring restoring the anatomy of the annulus, the ventricle is able to function more normally. Tricuspid valve repair leads to sustained improvement in right-sided remodeling and function.
Recurrent TR and Development of Tricuspid Stenosis
Incidence of recurrent TR and tricuspid stenosis after tricuspid valve repair is low.4,8 Recurrent TR after tricuspid valve repair ranges from 0.6% to 2%.3,4 When compared with patients who did not receive tricuspid valve repair at the time of mitral surgery, patients with tricuspid valve repair have significantly lower incidence of development of recurrent TR. Restoring the annulus to a normal size does not result in tricuspid stenosis, with no difference in the tricuspid gradient among patients who received tricuspid annuloplasty versus conservative management.8 Tricuspid valve repair is a durable intervention for functional TR and does not lead to tricuspid stenosis.
Long-Term Survival
Patients with preoperative TR who undergo tricuspid valve repair at the time of mitral surgery have superior long-term survival than those who are managed conservatively. Among patients undergoing left-sided valve surgery with preoperative TR, those left with residual TR had significantly worse long-term survival than those who had no TR.22 Although some studies have found no difference in long-term survival between medical management and surgical management of severe TR,23 these studies are primarily limited to patients undergoing surgery for isolated TR, which is known to be a high-risk population not comparable to those who undergo mitral valve surgery and receive a concomitant tricuspid valve repair. If patients with TR are intervened upon at the time of mitral valve surgery—before they develop severe TR and/or undergo surgery for isolated tricuspid disease—they can have equivalent survival to those who underwent isolated mitral valve repair and normal life expectancy may be restored.24,25 Patients with moderate or worse TR undergoing mitral valve surgery clearly have a survival benefit from concomitant tricuspid repair.
Conclusions
Tricuspid valve repair at the time of mitral surgery is safe and leads to excellent freedom from recurrent TR and improves long-term survival. The risk of permanent pacemaker placement can be mitigated by avoiding the area of the atrioventricular node and giving sufficient time for diuresis and cardiac tissue recovery before evaluation for a pacemaker. Patients with moderate or worse TR who are undergoing mitral valve surgery should receive tricuspid valve repair. Put a ring on it!
Conflict of Interest Statement
Dr Bolling is a consultant for Medtronic, Gore, and Abbott. All other authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
Footnotes
Dr Wagner is supported by the National Clinician Scholars Program through the Institute for Healthcare Policy and Innovation, University of Michigan, Ann Arbor, Mich. Dr Fu is supported by the National Institutes of Health T32 Multidisciplinary Program in Lung Disease (T32HL007749).
IRB approval: Institutional Review Board approval was not applicable.
References
- 1.Braunwald N.S., Ross J., Morrow A.G. Conservative management of tricuspid regurgitation in patients undergoing mitral valve replacement. Circulation. 1967;35(4 Suppl):I63–I69. doi: 10.1161/01.cir.35.4s1.i-63. [DOI] [PubMed] [Google Scholar]
- 2.Yilmaz O., Suri R.M., Dearani J.A., Sundt T.M., Daly R.C., Burkhart H.M., et al. Functional tricuspid regurgitation at the time of mitral valve repair for degenerative leaflet prolapse: the case for a selective approach. J Thorac Cardiovasc Surg. 2011;142:608–613. doi: 10.1016/j.jtcvs.2010.10.042. [DOI] [PubMed] [Google Scholar]
- 3.Gammie J.S., Chu M.W.A., Falk V., Overbey J.R., Moskowitz A.J., Gillinov M., et al. Concomitant tricuspid repair in patients with degenerative mitral regurgitation. N Engl J Med. 2022;386:327–339. doi: 10.1056/NEJMoa2115961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dreyfus G.D., Corbi P.J., Chan K.M.J., Bahrami T. Secondary tricuspid regurgitation or dilatation: which should be the criteria for surgical repair? Ann Thorac Surg. 2005;79:127–132. doi: 10.1016/j.athoracsur.2004.06.057. [DOI] [PubMed] [Google Scholar]
- 5.Caldas M.M.C., Esteves W.A.M., Nascimento B.R., Hung J., Levine R., Silva V.R., et al. Clinical outcomes and progression rate of tricuspid regurgitation in patients with rheumatic mitral valve disease. Open Heart. 2023;10 doi: 10.1136/openhrt-2023-002295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Otto C.M., Nishimura R.A., Bonow R.O., Carabello B.A., Erwin J.P., III, Gentile F., et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021;143:e35–e71. doi: 10.1161/CIR.0000000000000932. [DOI] [PubMed] [Google Scholar]
- 7.Dreyfus G.D., Essayagh B., Benfari G., Dulguerov F., Haley S.R., Dommerc C., et al. Outcome of consistent guideline-based tricuspid management in patients undergoing degenerative mitral regurgitation correction. J Thorac Cardiovasc Surg Open. 2021;7:125–138. doi: 10.1016/j.xjon.2021.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chikwe J., Itagaki S., Anyanwu A., Adams D.H. Impact of concomitant tricuspid annuloplasty on tricuspid regurgitation, right ventricular function, and pulmonary artery hypertension after repair of mitral valve prolapse. J Am Coll Cardiol. 2015;65:1931–1938. doi: 10.1016/j.jacc.2015.01.059. [DOI] [PubMed] [Google Scholar]
- 9.Lee H., Jeong D.S., Kim W.S., Sung K., Carriere K.C., Park S.J., et al. Is prophylactic tricuspid annuloplasty beneficial for degenerative mitral valve repair? Ann Thorac Surg. 2021;111:1502–1511. doi: 10.1016/j.athoracsur.2020.07.037. [DOI] [PubMed] [Google Scholar]
- 10.Tang G.H.L., David T.E., Singh S.K., Maganti M.D., Armstrong S., Borger M.A. Tricuspid valve repair with an annuloplasty ring results in improved long-term outcomes. Circulation. 2006;114(1 Suppl):I577–I581. doi: 10.1161/CIRCULATIONAHA.105.001263. [DOI] [PubMed] [Google Scholar]
- 11.Izutani H., Nakamura T., Kawachi K. Flexible band versus rigid ring annuloplasty for functional tricuspid regurgitation. Heart Int. 2010;5 doi: 10.4081/hi.2010.e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Navia J.L., Nowicki E.R., Blackstone E.H., Brozzi N.A., Nento D.E., Atik F.A., et al. Surgical management of secondary tricuspid valve regurgitation: annulus, commissure, or leaflet procedure? J Thorac Cardiovasc Surg. 2010;139:1473–1482.e5. doi: 10.1016/j.jtcvs.2010.02.046. [DOI] [PubMed] [Google Scholar]
- 13.Huffman L.C., Nelson J.S., Lehman A.N., Krajacic M.C., Bolling S.F. Identical tricuspid ring sizing in simultaneous functional tricuspid and mitral valve repair: a simple and effective strategy. J Thorac Cardiovasc Surg. 2014;147:611–614. doi: 10.1016/j.jtcvs.2013.01.027. [DOI] [PubMed] [Google Scholar]
- 14.Sugimoto T., Okada M., Ozaki N., Hatakeyama T., Kawahira T. Long-term evaluation of treatment for functional tricuspid regurgitation with regurgitant volume: characteristic differences based on primary cardiac lesion. J Thorac Cardiovasc Surg. 1999;117:463–471. doi: 10.1016/s0022-5223(99)70325-9. [DOI] [PubMed] [Google Scholar]
- 15.Ghoreishi M., Brown J.M., Stauffer C.E., Young C.A., Byron M.J., Griffith B.P., et al. Undersized tricuspid annuloplasty rings optimally treat functional tricuspid regurgitation. Ann Thorac Surg. 2011;92:89–95. doi: 10.1016/j.athoracsur.2011.03.024. discussion 96. [DOI] [PubMed] [Google Scholar]
- 16.Dreyfus G.D., Raja S.G., John Chan K.M. Tricuspid leaflet augmentation to address severe tethering in functional tricuspid regurgitation. Eur J Cardiothorac Surg. 2008;34:908–910. doi: 10.1016/j.ejcts.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 17.Choi J.B., Kim N.Y., Kim K.H., Kim M.H., Jo J.K. Tricuspid leaflet augmentation to eliminate residual regurgitation in severe functional tricuspid regurgitation. Ann Thorac Surg. 2011;92:e131–e133. doi: 10.1016/j.athoracsur.2011.08.019. [DOI] [PubMed] [Google Scholar]
- 18.Badhwar V., Rankin J.S., He M., Jacobs J.P., Furnary A.P., Fazzalari F.L., et al. Performing concomitant tricuspid valve repair at the time of mitral valve operations is not associated with increased operative mortality. Ann Thorac Surg. 2017;103:587–593. doi: 10.1016/j.athoracsur.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 19.Jokinen J.J., Turpeinen A.K., Pitkänen O., Hippeläinen M.J., Hartikainen J.E.K. Pacemaker therapy after tricuspid valve operations: implications on mortality, morbidity, and quality of life. Ann Thorac Surg. 2009;87:1806–1814. doi: 10.1016/j.athoracsur.2009.03.048. [DOI] [PubMed] [Google Scholar]
- 20.Brescia A.A., Ward S.T., Watt T.M.F., Rosenbloom L.M., Baker M., Khan S., et al. Outcomes of guideline-directed concomitant annuloplasty for functional tricuspid regurgitation. Ann Thorac Surg. 2020;109:1227–1232. doi: 10.1016/j.athoracsur.2019.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Desai R.R., Vargas Abello L.M., Klein A.L., Marwick T.H., Krasuski R.A., Ye Y., et al. Tricuspid regurgitation and right ventricular function after mitral valve surgery with or without concomitant tricuspid valve procedure. J Thorac Cardiovasc Surg. 2013;146:1126–1132.e10. doi: 10.1016/j.jtcvs.2012.08.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sorabella R.A., Mamuyac E., Yerebakan H., Najjar M., Choi V., Takayama H., et al. Residual tricuspid regurgitation following tricuspid valve repair during concomitant valve surgery worsens late survival. Heart Surg Forum. 2015;18:E226–E231. doi: 10.1532/hsf.1469. [DOI] [PubMed] [Google Scholar]
- 23.Axtell A.L., Bhambhani V., Moonsamy P., Healy E.W., Picard M.H., Sundt T.M., et al. Surgery does not improve survival in patients with isolated severe tricuspid regurgitation. J Am Coll Cardiol. 2019;74:715–725. doi: 10.1016/j.jacc.2019.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Watt T.M.F., Brescia A.A., Williams A.M., Bolling S.F. Functional tricuspid regurgitation: indications, techniques, and outcomes. Indian J Thorac Cardiovasc Surg. 2020;36(Suppl 1):131–139. doi: 10.1007/s12055-019-00915-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cetinkaya A., Ganchewa N., Hein S., Bramlage K., Bramlage P., Schonberg M., et al. Long-term outcomes of concomitant tricuspid valve repair in patients undergoing mitral valve surgery. J Cardiothorac Surg. 2020;15:210. doi: 10.1186/s13019-020-01244-6. [DOI] [PMC free article] [PubMed] [Google Scholar]



